Abstract
Background:
Recent epidemiological studies suggest that short sleep duration may be associated with the development of obesity from childhood to adulthood.
Objectives:
To assess whether the evidence supports the presence of a relationship between short sleep duration and obesity at different ages, and to obtain an estimate of the risk.
Methods:
We performed a systematic search of publications using MEDLINE (1996-2007 wk 40), EMBASE (from 1988), AMED (from 1985), CINHAL (from 1982) and PsycINFO (from 1985) and manual searches without language restrictions. When necessary, authors were contacted. Criteria for inclusion were: report of duration of sleep as exposure, BMI as continuous outcome and prevalence of obesity as categorical outcome, number of participants, age, and gender. Results were pooled using a random effect model. Sensitivity analysis was performed, heterogeneity and publication bias were also checked. Results are expressed as pooled odds ratios (OR [95% confidence intervals, CIs]) and as pooled regression coefficients (β; 95% CIs).
Results:
Of 696 studies identified, 45 met the inclusion criteria (19 in children and 26 in adults) and 30 (12 and 18, respectively) were pooled in the meta-analysis for a total of 36 population samples. They included 634,511 participants (30,002 children and 604,509 adults) from around the world. Age ranged from 2 to 102 years and included boys, girls, men and women. In children the pooled OR for short duration of sleep and obesity was 1.89 (1.46 to 2.43; P < 0.0001). In adults the pooled OR was 1.55 (1.43 to 1.68; P < 0.0001). There was no evidence of publication bias. In adults, the pooled β for short sleep duration was −0.35 (−0.57 to −0.12) unit change in BMI per hour of sleep change.
Conclusions:
Cross-sectional studies from around the world show a consistent increased risk of obesity amongst short sleepers in children and adults. Causal inference is difficult due to lack of control for important confounders and inconsistent evidence of temporal sequence in prospective studies.
Citation:
Cappuccio FP; Taggart FM; Kandala NB; Currie A; Peile E; Stranges S; Miller MA. Meta-analysis of short sleep duration and obesity in children and adults. SLEEP 2008;31(5):619-626.
Keywords: Sleep duration, obesity, meta-analysis
IN THE LAST FEW DECADES THERE HAS BEEN A SIGNIFICANT INCREASE IN THE PREVALENCE OF OBESITY WORLDWIDE AND THE WORLD HEALTH organization has declared it a global epidemic.1 Obesity in childhood is a cause of psychosocial problems including low self esteem,2 and frequently continues into adulthood3 where it is a cause of major morbidity and mortality including cardiovascular disease and type 2 diabetes. At the same time there has been a reduction in sleep time. National surveys in USA have shown a decline in self-reported sleep duration over the past 50 years by 1.5 to 2 hours.4 This sleep curtailment has been attributed to lifestyle changes.
Several studies have reported associations between duration of sleep (short as well as long) and ill-health, including relationships with self-reported well-being,5 morbidity and mortality,6–12 and with chronic conditions including type 2 diabetes, respiratory disorders, hypertension, and obesity.13–18 The associations between short duration of sleep and obesity, in particular, have stimulated a debate given the potential implications for children19,20 as well as adults.21,22 However, given the variety of studies and the large differences in the target populations, it is difficult to draw immediate conclusions on the consistency of the association, the direction of causality and the likely mechanisms involved. The aims of this article are to (i) systematically review published population-based studies, (ii) to carry out a meta-analysis to assess whether the evidence supports the presence of a relationship between short sleep duration and obesity at different ages, and (iii) to obtain a quantitative estimate of the risk in order to assess the consistency and potential public health relevance
METHODS
Literature Search
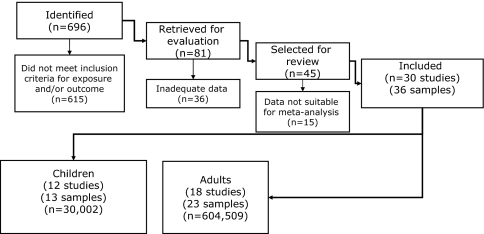
We performed a systematic search for publications using Medline (1996-2007 week 40), EMBASE (from 1988), AMED (from 1985), CINAHL (from 1982) Psychinfo (from 1985). Search strategies used subject headings and key words and did not use language restrictions. We (FMT, N-BK, AC, SS, MAM, and FPC) examined reference lists of the relevant reviews and all identified studies and reviewed the cited literature. Two reviewers (FMT and N-BK) independently extracted the data. Differences about inclusion of studies and interpretation of data were resolved by arbitration (FPC), and consensus was reached after discussion with all authors. Of a total of 696 studies identified from the search (Figure 1), 12 studies in children met the inclusion criteria and provided suitable data on 13 population samples to be included in the pooled analysisw1–w12 (Table 1). Seven studiesw13–w19 were excluded, as they did not provide sufficient data for inclusion (Table 2). In adults 26 studies met the inclusion criteria, and 18 provided suitable data on 23 population samples to be included in the pooled analysisw20–w37 (Table 3). Eight studiesw38–w45 were excluded as they did not provide sufficient data for inclusion (Table 4). Note: All references beginning with a W are available in the website version of this paper on the SLEEP website at www.journalsleep.org
Figure 1.
Flowchart indicating the results of the systematic review with inclusions and exclusions.
Table 1.
Description of the Study Populations of Children Included in the Meta-Analyses (n=30,002)
| Author | Year | Country | Sample size (n) | Age (years) |
|---|---|---|---|---|
| Locard w1 | 1992 | France | 1,031 | 5 |
| Ben Slama w2 * | 2002 | Tunisia | 167 | 6–10 |
| Sekine w3 | 2002 | Japan | 8,941 | 2–4 |
| Von Kries w4 | 2002 | Germany | 6,645 | 5–6 |
| Agras w5 | 2004 | USA | 150 | 9.5 |
| (sleep at 3–5) | ||||
| Giugliano w6 | 2004 | Brazil | 165 | 6–10 |
| Padez w7 | 2005 | Portugal | 4,390 | 7–9 |
| Reilly w8 | 2005 | UK | 6,426 | 7 |
| (sleep at 2.5) | ||||
| Chaput (1) w9 | 2006 | Canada | 422 | 5–10 |
| Chen w10 † # | 2006 | Taiwan | 656 | 13–18 |
| Seicean w11 § # | 2007 | USA | 509 | 14–18 |
| Yu (males) w12 ¶ | 2007 | China | 273 | 10–20 |
| Yu (females) w12 ¶ | 2007 | China | 227 | 10–20 |
Short sleep: * <8 h per day; † <6 h per night or <3 h weekday per week; § <5 h on school nights; ¶ average week night sleep in hours # overweight/obesity defined as >85th percentile
Note: All references beginning with a W are available in the website version of this paper on the SLEEP website at www.journalsleep.org
Table 2.
Description of the Studies in Children Excluded from the Meta-Analyses
| Author | Year | Country | Study design and Population | Sample size (n) | Age (yr) | Definition of sleep and obesity | Outcome measures presented | Summary of findings | Reason for exclusion |
|---|---|---|---|---|---|---|---|---|---|
| Gupta w13 | 2002 | USA | Cross-sectional Heartfelt Study | 383 | 11–16 | TST BMI >85th percentile for age and sex and % body fat >25% male or 30% female | Logistic regression | Obesity and TST β = −1.62 (0.28 SE) OR: 0.20 (0.11 to 0.34) | Logistic regression for OR and β only-adolescent study |
| Hui w14 | 2003 | Hong Kong | Selected groups Student Health Service | 343 | 6–7 | Usual no. of h sleep BMI/overweight by HK reference categories | % short sleepers in 3 categories of BMI | Association between short sleep and obesity (% obese increased in short sleepers and decreased in long sleepers) | Case-control analysis Selected by BMI group |
| Knutson w15 | 2005 | USA | National Longitudinal Study of Adolescent Health | 4,555 | grade 7–12 13–18 | BMI and usual no. h sleep | β for sleep duration and BMI | Shorter sleep and obesity boys β= − 0.08 (−0.12 to −0.03) girls β = −0.02 (−0.06 to 0.01) | OR from logistic regression only. |
| Eisenmann w16 | 2006 | Australia | Australian Health and Fitness survey | 6,324 | 7–15 | Sleep time in bed at night. BMI and Waist by sleep duration categories | ORadj for age | Dose response relationship for short sleep and overweight in all age groups (from 7 to 16 yr) significant in boys but not girls. | βadj and ORadj for age |
| Dieu w17 | 2007 | Vietnam | Sample of 20 kindergartens in Ho Chi Minh City | 670 | 4–6 | Obesity by Cole IOTF definition.w45 Night sleep time | Prevalence ratios with CI | Prevalence ratio 0.85 in univariate regression for duration of sleep and overweight. Children with longer nighttime sleep had lower risk of obesity. | No OR or β available |
| Knutson w18 | 2007 | USA | Cross-sectional Child Development supplement of Panel Study of Income Dynamics | 767 boys 779 girls | 10–18 | 2-d time diary and self-reported TST. “Overweight” >95th percentile according to CDC and prevention growth charts | ORadj for self-reported 0.5 to 7 h sleep vs 9.2 to 19.0 h sleep and obesity. | Self reported short sleep duration vs longest sleep ORadj = 0.88 (0.45 to 1.69). However significantly higher risk of overweight with midrange self-reported sleep duration compared to longest sleep. | Reported ORadj. No linear regression. |
| Snell w19 | 2007 | USA | Longitudinal Panel Survey of Income Dynamics | 1,441 | 3–17 | Average nightly sleep, BMI and obesity by Cole et al.w45 | Linear regression BMI, nonlinear (% categories) and sleep and wake timings. | BMI at time 1 sig corr <8 h sleep | No OR for short sleep vs obesity or β for cross sectional analysis. Only mean BMI in sleep duration categories |
TST = Total Sleep Time; SE = standard error; BMI = Body Mass Index; β = regression coefficient; OR = odds ratio; Adj = adjusted; CI = confidence intervals; sd = standard deviation. Note: All references beginning with a W are available in the website version of this paper on the SLEEP website at www.journalsleep.org
Table 3.
Description of the Study Populations of Adults Included in the Meta-Analyses (n=604,509)
| Author | Year | Country | Sample size (n) | Age (years) |
|---|---|---|---|---|
| Vioque w20 | 2000 | Spain | 1,772 | 15+ |
| Shigeta w21 * ¶ | 2001 | Japan | 437 | 43–63 |
| Kripke w22 | 2002 | USA | 497,037 | 30–102 |
| Cournot w23 | 2004 | France | 3,127 | 32–62 |
| Hasler w24 | 2004 | Switzerland | 457 | 27 |
| Bjorkelund w25 | 2005 | Sweden | 1,460 | 38–60 |
| Gangwisch (1) w26 | 2005 | USA | 3,682 | 32–49 |
| Gangwisch (2) w26 | 2005 | USA | 3,324 | 50–67 |
| Gangwisch (3) w26 | 2005 | USA | 2,582 | 68–86 |
| Singh w27 | 2005 | USA | 3,158 | 18–65 |
| Moreno w28 § | 2006 | Brazil | 4,878 | Mean 40 |
| Vahtera w29 † ‡ | 2006 | Finland | 26,468 | Mean 45 |
| Watari (men) w30 ‡ | 2006 | Japan | 19,894 | 20–54 |
| Watari (women) w30 ‡ | 2006 | Japan | 5,418 | 20–54 |
| Kohatsu w31 | 2006 | USA | 990 | Mean 48.3 |
| Bjorvatn w32 | 2007 | Norway | 8,860 | 40–45 |
| Chaput (men) w33 * ¶ | 2007 | Canada | 323 | 21–64 |
| Chaput (women) w33 * ¶ | 2007 | Canada | 417 | 21–64 |
| Ko w34 * # | 2007 | Hong Kong | 4,793 | 17–83 |
| Tuomilehto w35 * | 2007 | Finland | 2,770 | 45–74 |
| Fogelholm (men) w36 * | 2007 | Finland | 3,377 | 30+ |
| Fogelholm (women) w36 * | 2007 | Finland | 4,264 | 30+ |
| Stranges w37 | 2008 | UK | 5,021 | 44–69 |
Short sleep: * <6 h or <6 h per day; † <6.5 h or <6.5 h per night; § <8 h per night; Obesity: ¶ BMI >25 kg/m2; # BMI >25 kg/m2 and/or waist >80 cm in women and >90 cm in men; ‡ BMI >27 kg/m2 or >26.4 kg/m2; Note: All references beginning with a W are available in the website version of this paper on the SLEEP website at www.journalsleep.org
Table 4.
Description of the Studies in Adults Excluded from the Meta-Analyses
| Author | Year | Country | Study design and Population | Sample size (n) | Age (yr) | Definition of sleep and obesity | Outcome measures presented | Summary of findings | Reason for exclusion |
|---|---|---|---|---|---|---|---|---|---|
| Heslop w38 | 2002 | UK | Cross-sectional Employed men | 6,022 | <65 | Self reported TST in 24 h and BMI | Mean BMI for sleep duration categories | Shortest sleepers had higher BMI. [25.4 (25.2-25.6) for <7 h to 25.1(24.7-25.4) for >8 h; P for trend = 0.02]. | No OR for short sleep vs obesity or β |
| Burazeri w39 | 2003 | Israel | Cross-sectional analysis in cohort | 1,842 | 50+ | Night sleep duration >8 h and TST >8 h and obesity | Cross sectional analysis for both long night sleep duration and long total sleep duration and obesity | No significant association between long sleep and obesity - no analysis with short sleep | No report of relation between short sleep and obesity–only looked at 8 h+ vs <8 h |
| Taheri w40 | 2004 | USA | Cross-sectional Employees with oversampling of habitual snorers. | 1,024 | 30–60 | Average nightly sleep from 6-d diary and BMI | βadj for average nightly sleep and BMI. | Mean BMI with se for sleep duration groups | No OR for short sleep vs obesity or β |
| Tamakoshi w41 | 2004 | Japan | Japan Collaborative Cohort Study | 43,852 men 60,158 women | 40–9 | Average sleep duration on weekdays and BMI | BMI (SD) for each of 7 sleep duration categories from <4 h to 10 h+ | No test for trend | No odds ratio for short sleep vs obesity or regression coefficient. Only mean BMI in sleep duration categories |
| Ohayonw42 | 2005 | France | Telephone survey followed by interviews | 1,026 | 60+ | Self-reported sleep duration and height and weight | OR for risk of short sleep (≤4 h30) among obese people (BMI>27) compared to people with normal BMI | Obese people were more likely to have the shortest sleep. OR for risk of short sleep (≤4 h 30) among obese people compared to people with normal BMI. OR = 3.6 (1.0 to 13.1) | OR not comparable because analysis does not include full range of BMI as outcome. |
| Vorona w43 | 2005 | USA | Primary care population | 924 | 18–91 | Self-reported TST in 24 h for weekday and w/end weighted for number of days. Self-reported weight and height | BMI in 4 groups. ANOVA | Obese participants slept less than individuals who were overweight (P = 0.04) or had normal BMI (P = 0.004). | No OR for short sleep vs obesity or β |
| Patel w44 | 2006 | USA | Nurses Health Study | 68,183 | 30–55 | BMI and self-reported h sleep in 24 h | BMI and SE for sleep duration categories | Short sleepers had higher BMI; P for trend <0.000) | No OR for short sleep vs obesity or β. |
| Meisinger w45 | 2007 | Germany | MONICA cohort | 3,508 men 3,388 women | 45–74 | BMI h nighttime sleep | BMI (SD) by 5 sleep duration categories | BMI higher for <5 h sleep and 6 h. | No OR for short sleep vs obesity or β |
*BMI≥ 25 and/or waist ≥80 cm in women or ≥90 cm in men
Note: All references beginning with a W are available in the website version of this paper on the SLEEP website at www.journalsleep.org
Inclusion Criteria
The main objective was to assess the relationship between sleep duration and either obesity or body mass index (BMI). No restriction was placed on populations included. When data were not readily available from the published reports, we wrote to authors to ask for raw data.
Meta-Analysis
Exposure: Sleep Duration
Both the nature and quantity of sleep in children is different from that of adults. There is a gradual change with age and by age 10, sleep is similar to that of adults but the total time is longer (10 h).23 We analyzed the results of studies in children separately from those in adults. For children the definition of “short sleep” was <10 h or <10 h per night unless stated otherwise in Table 1.
In most of the studies in adults, short sleep was defined as either <5 h or <5 h per night for either average total sleep time (TST) in 24 h, nighttime sleep, weekday sleep, or based on a weighted average TST on weekdays and weekends, unless stated otherwise in Table 3. For odds ratios, short sleepers were compared to both middle and long sleepers, although in some studies they were compared to the reference category of either 7 h or 8 h sleep per night.
Outcome: Obesity
Unless stated otherwise (Table 1), obesity in children was defined either as BMI >95th percentile according to local national growth charts or by international growth charts where the thresholds for obesity is defined as the percentile which passes through BMI >30 kg/m2 at age 18 years.w46 Unless stated otherwise (Table 3), obesity in adults was defined as BMI >30 kg/m2.
Confounders
Mean age of the populations, proportion of boys and girls, men and women, and sample size were collected and used in stratified analyses of heterogeneity, publication bias and sensitivity.
Statistical Analysis
To estimate the quantitative relation between short sleep duration and obesity, we obtained an estimate from each study of the unadjusted odds ratio (OR) with 95% confidence intervals (CIs) and the unadjusted regression coefficient β (95% CIs) for BMI as a continuous outcome. Some studies did not report the unadjusted OR and β for the relationship between short sleep duration and obesity. We requested from various authors the unadjusted OR (95% CIs) for <5 h sleep versus >5 h and obesity defined as BMI >30 kg/m2, its standard error (SE), and the exact sample size (N). We also requested the unadjusted β (95% CIs) for BMI (as a continuous outcome) on sleep duration, its standard error (SE), and the exact sample size (N). If the SE of either the OR or β were not supplied, it was algebraically computed from the 95% CIs. We used a random effect model and calculated pooled effects (95% CIs) for both OR and β. A problem which occurs in observational studies is selection bias and confounding. Selection bias is a feature of the study design and the possibility of this can be assessed by examining the methods of the study. Confounding can be due to known or unknown factors involved in the etiology and are related to both exposure and outcome variables. We examined possible sources of heterogeneity between the studies using a meta-regression technique. We performed the Breslow-Day test for homogeneity of ORs, Cochran-Mantel-Haenszel test for the null hypothesis of no effect (OR=1), and the Mantel-Haenszel common OR estimate. We assessed publication bias by using a funnel plot and Begg'sw47 test to find out whether there was a bias towards publication of studies with positive results among the smaller studies. In order to avoid bias in selection of papers, we tried to obtain all population studies which had data on the relationship between sleep duration and obesity which had been published worldwide and conducted the searches in an unbiased way using the main medical databases and reference lists from recent reviews. We also examined the influence of individual studies, in which the meta-analysis estimates are derived omitting one study at a time to see the extent to which inferences depend on a particular study or group of studies.
RESULTS
Children
Thirteen population samples from 12 studies were included in the pooled analysis. They included 30,002 participants from France, Tunisia, Japan, Germany, USA (n = 2), Brazil, Portugal, United Kingdom, Canada, Taiwan, and China. Age ranged from 2 to 20 years and included boys and girls. Sample sizes ranged between 150 and 8,941. Data was extracted from the published articles when available and authors were contacted to request unavailable data or analyses. Details of the studies are summarized in Table 1.
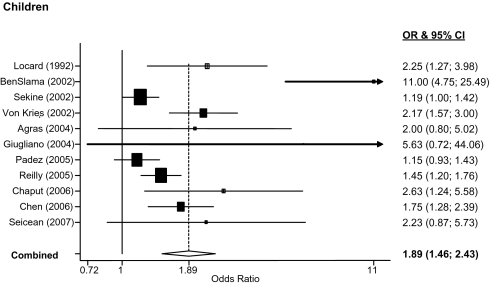
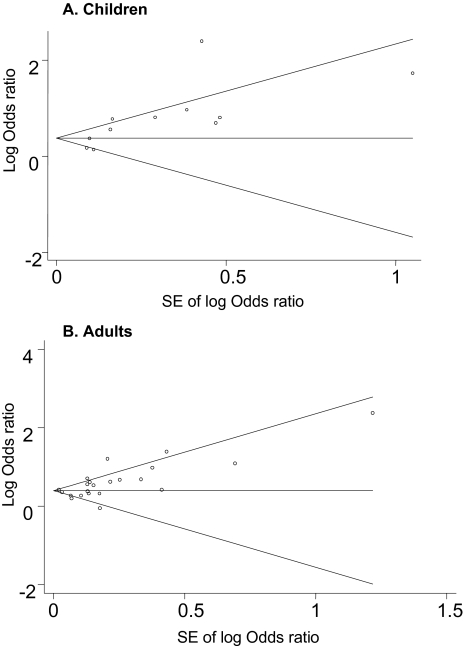
For the meta-analysis sleep exposure was dichotomized for all studies. Figure 2 shows the Forest plot of 11 observational studies of short sleep and obesity involving 29,502 children studied around the world. Seven of 11 studies reported a significant association between short duration of sleep and obesity. The pooled OR was 1.89 (1.46 to 2.43). Publication bias was not detected by the Begg's test (P = 0.12) (Figure 3a). The heterogeneity test was significant (Q = 46.6, df = 10, P < 0.001). The sensitivity analysis indicated that the omission of any of the studies led to changes in estimates between 1.61 (1.33 to 1.96) and 2.07 (1.54 to 2.79) (Appendix 1).
Figure 2.
Forest plot of the associations between short duration of sleep and obesity in studies carried out in children. OR and 95 CI indicate odds ratio and 95% confidence intervals.
Figure 3.
Funnel plot for meta-analysis of studies in children (A: top) and in adults (B: bottom).
Adults
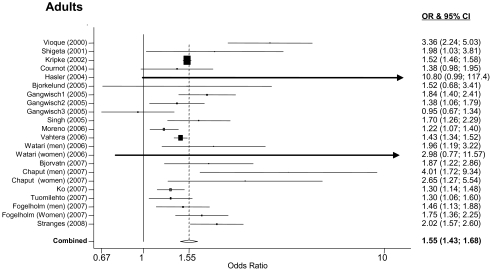
Twenty-two population samples from 17 studies met the inclusion criteria and provided suitable data for pooled analyses. They included 604,509 participants from Spain, Japan (n = 2), USA (n = 5), France, Switzerland, Sweden, Brazil, Finland (n = 3), Norway, Canada, Hong Kong, and United Kingdom. Age ranged from 15 to 102 years and included men and women. Sample sizes ranged between 437 and 497,037. Data were extracted from the published articles when available and authors were contacted to request unavailable data or analyses. Details of the studies included in the meta-analysis are summarized in Table 3. For the meta-analysis sleep exposure was used in two ways: as dichotomized variable and as continuous variable regressed over BMI used as continuous variable. Figure 4 shows the forest plot of 22 population samples from 17 observational studies of short sleep and obesity involving 603,519 adults studied around the world. Seventeen population samples showed a significant association between short duration of sleep and obesity. The pooled OR was 1.55 (1.43 to 1.68). There was no evidence of publication bias (Begg's test P = 0.09) (Figure 3b). The heterogeneity test was significant (Q = 64.0, df = 21, P < 0.001). The sensitivity analysis indicated that the omission of any of the studies led to changes in estimates between 1.50 (1.39 to 1.61) and 1.59 (1.44 to 1.76) (Appendix 2).
Figure 4.
Forest plot of the associations between short duration of sleep and obesity in studies carried out in adults. OR and 95 CI indicate odds ratio and 95% confidence intervals.
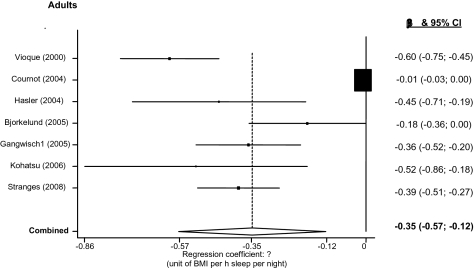
Figure 5 shows the Forest plot of 7 studies in adults including 16,509 participants and reporting regression coefficients (β) between hours of sleep per night and BMI. Unlike studies in children, all studies in adults showed a consistent and significant negative association between hours of sleep and BMI. The pooled β was −0.35 (−0.57 to −0.12) unit of change in BMI per hour of sleep (P = 0.002; heterogeneity P < 0.001). The sensitivity analysis indicated that the omission of any of the studies led to changes in estimates between −0.30 (−0.51 to −0.09) and −0.41 (−0.53 to −0.28) (Appendix 3).
Figure 5.
Forest plot of the associations between duration of sleep and body mass index in studies carried out in adults. β and 95 CI indicate regression coefficient and 95% confidence intervals.
DISCUSSION
This study provides for the first time a systematic review of the literature and quantitative estimates of the cross-sectional associations between duration of sleep and obesity (or measures of obesity) in population-based studies of children and adults around the world. It shows a consistent pattern of increased odds of being short sleeper if you are obese, both in childhood and in adulthood. A pooled regression analysis in adults also suggests that a reduction in one hour of sleep per day would be associated with a 0.35 kg/m2 increase in BMI. For a person approximately 178 cm tall it would be equivalent to approximately 1.4 kg in weight.
These results are of interest for several reasons. First, the association is consistent in different populations. Although the meta-analysis detected significant heterogeneity between studies, further sensitivity analyses and the exclusion of publication bias are in favor of a similar effect across the populations. Second, they indicate an effect size consistent across ages. The 60% to 80% increase in the odds of being short sleeper amongst obese was seen in both children and adults, even after some attenuation following sensitivity analyses. Third, the categorical results were corroborated by the meta-analysis of regression coefficients, at least in adults.
There are some limitations. First, the quality of the data cannot go beyond the quality of the individual studies included. Second a meta-analysis of observational studies is open to important fallacies in that it cannot directly control for confounding and therefore may be open to biased estimates. Third, the results can only be representative of the studies that have been included and are unable to provide a representative inference of all studies published. Nevertheless, these results are important in guiding the assessment of current evidence and the definition of future research strategies.
The pooled studies are cross-sectional and cannot, therefore, determine temporal sequence, hence, causality. They also cannot examine changes in sleeping habits with time. Moreover, all studies used sleep questionnaires to determine self-reported sleep duration within their populations. Self-reported duration of sleep has been validated against actigraphy.24
The variety of methods for analyzing weight and obesity reflects our current poor understanding of what the most effective measuring scheme is. Many different methods were used to determine obesity, particularly in children, making the various studies more difficult to reconcile.
The studies varied in the degree of control for confounders such as age, gender, ethnic background, socioeconomic status, degree of energy intake, energy expenditure, frequency of snacking, and other health-related behaviors and nutritional habits. A confounding factor in the relationship between sleep duration and obesity in adults is psychiatric comorbidity, particularly depression.25–27 Chronic illness, physical disability, use of hypnotics, etc., would also be important confounders to consider. In the pooled analysis we used exclusively unadjusted estimates from the individual studies. The consistency of the pooled associations between children and adults suggests that it is unlikely that a differential bias due to common unaccounted confounders might have occurred in the two age categories.
The results of prospective studies do not provide consistency in support of the view that short sleep duration predicts the future development of obesity,22,28–31 with the exception of a very large study (n >60,000), carried out in women only, which shows a small effect (hazard ratio of 1.15 and 1.06 for those sleeping <5 h and <6 h per night, respectively).32 The relationship may be confounded by comorbidity, such as chronic mental illness, causing a decrease in the levels of physical activity and a reduction in sleep, or by physical illnesses associated with pain—hence disrupted sleep—and severe limitation in energy expenditure through limited physical activity. More recent studies have adjusted for these potential confounders and found no prospective association.22
Our study does not allow us to study mechanism. However, it has been suggested that short sleep may lead to obesity through the activation of hormonal responses33 leading to an increase in appetite and caloric intake. Short sleep is associated to reciprocal changes in leptin and ghrelin.33 This in turn would increase appetite and contribute to the development of obesity. The evidence in humans comes from short-lived severe sleep deprivation experiments35,36 that cannot be extrapolated to long term effects in the population.
Activation of inflammatory pathways by short sleep may also be implicated in the development of obesity.37 Finally, it is not inconceivable that short sleep is just a marker of unfavorable health status and of lifestyle characteristics.38,39
The potential public health implications of a causal relationship between short duration of sleep and obesity have already been widely disseminated in the media. The findings of our analysis suggest that whilst sustained sleep curtailment and ensuing excessive daytime sleepiness are undoubtedly cause for concern, the link to obesity is of interest but still to be proven as a causal link. Many questions still need an answer to determine causality. Prospective studies in which weight, height, waist measurements. and adiposity are measured at baseline and again at subsequent data collection times together with more accurate objective measurement of sleep duration (including naps) and confounding factors or mediators such as depression are needed.
Further prospective studies with improved assessment of long-term exposure (repeated self-reported sleep duration or repeated actigraphy), more specific outcomes (including measures of adiposity) and better control for confounders are needed before causality can be determined.
ACKNOWLEDGMENTS
We thank Drs. Agras, Bjorkelund, Chaput, Chen, Cournot, Gangwisch, Giugliano, Hasler, Kripke, Locard, Sekine and Vioque for supplying additional data or analyses not available in the published article. This work is part of the Programme ‘Sleep, Health & Society’ of the University of Warwick.
Footnotes
Disclosure Statement
This was not an industry supported study. Dr. Peile has received research support from Cephalon. The other authors have indicated no financial conflicts of interest.
Authors' Contribution
FPC conceived the study aims and design, contributed to the data extraction, planned the analysis, interpreted the results and drafted the final version of the paper. FMT carried out the systematic review and contributed to data extraction and analysis. N-BK contributed to data extraction and carried out the statistical analysis. AC, SS and MAM contributed to the systematic review, analysis and interpretation. EP contributed to interpretation of results. All authors contributed to the revision of the manuscript.
REFERENCES
- 1.WHO Europe. Diet and Physical Activity for Health; WHO European Ministerial Conference on Counteracting Obesity; 1–9; 2006. EUR/06/5062700/9. [Google Scholar]
- 2.Strauss RS. Childhood obesity and self-esteem. Pediatrics. 2000;105:e15. doi: 10.1542/peds.105.1.e15. [DOI] [PubMed] [Google Scholar]
- 3.Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002;76:653–8. doi: 10.1093/ajcn/76.3.653. [DOI] [PubMed] [Google Scholar]
- 4.National Sleep Foundation. Sleep in America Poll. Washington DC: 2005. [Google Scholar]
- 5.Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;166:1689–92. doi: 10.1001/archinte.166.16.1689. [DOI] [PubMed] [Google Scholar]
- 6.Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6:102–7. doi: 10.1093/sleep/6.2.102. [DOI] [PubMed] [Google Scholar]
- 7.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 8.Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27:51–4. [PubMed] [Google Scholar]
- 9.Patel SR, Ayas NT, Malhotra MR, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–4. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 10.Kojima M, Wakai K, Kawamura T, et al. Sleep patterns and total mortality: a 12-year follow-up study in Japan. J Epidemiol. 2000;10:87–93. doi: 10.2188/jea.10.87. [DOI] [PubMed] [Google Scholar]
- 11.Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: the effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002;3:305–14. doi: 10.1016/s1389-9457(02)00016-3. [DOI] [PubMed] [Google Scholar]
- 12.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30:1659–66. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 14.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–9. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 15.Cappuccio FP, Stranges S, Kandala N-B, et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension. The Whitehall II study. Hypertension. 2007;50:694–701. doi: 10.1161/HYPERTENSIONAHA.107.095471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayas NT, White DP, Al-Delaimy WK, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–4. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 17.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29:657–61. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 18.Knutson KL, Ryden AM, Mander BA, Van Cauter E. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med. 2006;166:1768–74. doi: 10.1001/archinte.166.16.1768. [DOI] [PubMed] [Google Scholar]
- 19.Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch Dis Child. 2006;91:881–4. doi: 10.1136/adc.2005.093013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Currie A, Cappuccio FP. Sleep in children and adolescents: a worrying scenario. Can we understand the sleep deprivation–obesity epidemic? Nutr Metab Cardiovasc Dis. 2007;17:230–2. doi: 10.1016/j.numecd.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 21.Cizza G, Skarulis M, Mignot E. A link between short sleep and obesity: building the evidence for causation. Sleep. 2005;28:1217–20. doi: 10.1093/sleep/28.10.1217. [DOI] [PubMed] [Google Scholar]
- 22.Stranges S, Cappuccio FP, Kandala N-B, et al. Cross-sectional versus prospective associations of sleep duration with changes in relative weight and body fat distribution: the Whitehall II study. Am J Epidemiol. 2008;167:321–9. doi: 10.1093/aje/kwm302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302–7. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 24.Lockley SW, Skene DJ, Arendt J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res. 1999;8:175–83. doi: 10.1046/j.1365-2869.1999.00155.x. [DOI] [PubMed] [Google Scholar]
- 25.Pfaffenberger RSJ, Lee IM, Leung R. Physical activity and personal characteristics associated with depression and suicide in American college men. Acta Psychiatr Scand. 1994;377:16–22. doi: 10.1111/j.1600-0447.1994.tb05796.x. [DOI] [PubMed] [Google Scholar]
- 26.Chang PP, Ford DE, Mead LA, Cooper-Patrick L, Klag MJ. Insomnia in young men and subsequent depression. The Johns Hopkins precursors study. Am J Epidemiol. 1997;146:105, 14. doi: 10.1093/oxfordjournals.aje.a009241. [DOI] [PubMed] [Google Scholar]
- 27.Foley DJ, Monjan AA, Izmirlian G, Hays JC, Blazer DG. Incidence and remission of insomnia among elderly adults in a biracial cohort. Sleep. 1999;22(Suppl 2):S373–8. [PubMed] [Google Scholar]
- 28.Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 2007;78:309–23. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 29.Hasler G, Buysse DJ, Klaghofer R, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27:661–6. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 30.Bjorkelund C, Bondyr-Carlsson D, Lapidus L, et al. Sleep disturbances in midlife unrelated to 32-year diabetes incidence: the prospective population study of women in Gothenburg. Diabetes Care. 2005;28:2739–44. doi: 10.2337/diacare.28.11.2739. [DOI] [PubMed] [Google Scholar]
- 31.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28:1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 32.Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006;164:947–54. doi: 10.1093/aje/kwj280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vgontzas AN, Bixler EO, Chrousos GP. Metabolic disturbances in obesity versus sleep apnoea: the importance of visceral obesity and insulin resistance. J Intern Med. 2003;254:32–44. doi: 10.1046/j.1365-2796.2003.01177.x. [DOI] [PubMed] [Google Scholar]
- 34.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spiegel K, Tasali E, Penev P, Van Cauter E. Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 36.Spiegel K, Leproult R, L'hermite-Baleriaux M, Copinschi G, Penev PD, Van Cauter E. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89:5762–71. doi: 10.1210/jc.2004-1003. [DOI] [PubMed] [Google Scholar]
- 37.Miller MA, Cappuccio FP. Inflammation, sleep, obesity and cardiovascular disease. Curr Vasc Pharmacol. 2007;5:93–102. doi: 10.2174/157016107780368280. [DOI] [PubMed] [Google Scholar]
- 38.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29:883–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Knutson KL, Turek FW. The U-shaped association between sleep and health: the 2 peaks do not mean the same thing. Sleep. 2006;29:881–2. doi: 10.1093/sleep/29.7.878. [DOI] [PubMed] [Google Scholar]