Abstract
Background
The identification of patients' health needs is pivotal in optimising the quality of health care, increasing patient satisfaction and directing resource allocation. Health needs are complex and not so easily evaluated as health-related quality of life (HRQL), which is becoming increasingly accepted as a means of providing a more global, patient-orientated assessment of the outcome of health care interventions than the simple medical model. The potential of HRQL as a surrogate measure of healthcare needs has not been evaluated.
Objectives and method
A generic (Short Form-12; SF-12) and a disease-specific questionnaire (Seattle Angina Questionnaire; SAQ) were tested for their potential to predict health needs in patients with acute coronary disease. A wide range of healthcare needs were determined using a questionnaire specifically developed for this purpose.
Results
With the exception of information needs, healthcare needs were highly correlated with health-related quality of life. Patients with limited enjoyment of personal interests, weak financial situation, greater dependency on others to access health services, and dissatisfaction with accommodation reported poorer HRQL (SF-12: p < 0.001; SAQ: p < 0.01). Difficulties with mobility, aids to daily living and activities requiring assistance from someone else were strongly associated with both generic and disease-specific questionnaires (SF-12: r = 0.46-0.55, p < 0.01; SAQ: r = 0.53-0.65, p < 0.001). Variables relating to quality of care and health services were more highly correlated with SAQ components (r = 0.33-0.59) than with SF-12 (r = 0.07-0.33). Overall, the disease-specific Seattle Angina Questionnaire was superior to the generic Short Form-12 in detecting healthcare needs in patients with coronary disease. Receiver-operator curves supported the sensitivity of HRQL tools in detecting health needs.
Conclusion
Healthcare needs are complex and developing suitable questionnaires to measure these is difficult and time-consuming. Without a satisfactory means of measuring these needs, the extent to which disease impacts on health will continue to be underestimated. Further investigation on larger populations is warranted but HRQL tools appear to be a reasonable proxy for healthcare needs, as they identify the majority of needs in patients with coronary disease, an observation not previously reported in this patient group.
Keywords: Healthcare needs assessment, Coronary artery disease, Health-related quality of life
Introduction
Clinical triallists assess a treatment under evaluation according to specific clinical 'endpoints', typically mortality or morbidity, or some measure of health service utilisation, such as length of hospital stay; similar endpoints have become the standard set in national frameworks [1] and college guidelines [2]. Doctors generally record how successful a medical intervention has been in terms of the extent of symptom relief or the technical success of a procedure. Patients, however, measure the impact of disease in terms of general health status and of quality of life and describe the effectiveness of treatment as the extent to which their health care needs have been met.
Managing population health needs is central to modern healthcare systems [3], regardless of the sophisticated concept and inherent complexity of 'needs'. A well-known definition of needs, which is not without criticism [4], is 'what people could benefit from health services' [5]; this draws attention to the importance of measuring the outcome of a health intervention. Considering a medical intervention as successful if it has a measurable favourable outcome may satisfy a target in one national service framework or another but is of limited importance to an individual since it completely ignores the patient's perspective of his or her needs.
Target-driven standards in areas of health care with a high political profile appear to be replacing the concept of universal provision, which warrants quantifying outcomes of health care. Identifying who might benefit from these health services is equally important if scarce resources are to be fully and appropriately utilised. If the goal of care is optimal health, the key marker of success ought to be to ascertain individual patients' health care needs (HCN) and tailor services accordingly.
Developing a comprehensive, valid and reliable HCN assessment tool is not straightforward, requiring the aggregation of information from a wide variety of sources [6]; this perhaps explains the lack of such tools compared with the more widely accepted quality of life tools such as the Nottingham Health Profile [7] and the Short-Form 36 [8]. Producing a health needs assessment tool involves a qualitative review of professional and patient opinion and all available health service information and a variety of internal checks to achieve validity and reliability.
We hypothesised that there was a direct relationship between health-related quality of life and health needs. If such a relationship were proven, health related quality of life, which is more simply measured, could be assessed in every patient and a more lengthy and detailed analysis of HCN reserved for those with impaired quality of life.
Method
In the absence of an available tool for healthcare needs assessment of patients with coronary heart disease (CHD), we developed our own questionnaire (Nottingham Health Needs Assessment: NHNA), derived from the literature, expert views and information compiled at interview. Following in-hospital testing and amendments, a satisfactory format for the questionnaire was established. The NHNA comprised a wide range of parameters including demographic data, employment, mobility and transport, access to local heath care facilities, information needs and concerns, availability of carers, current health care, accommodation, education, leisure, and social facilities.
Patients admitted to the acute cardiac unit of Queen's Medical Centre, Nottingham with cardiac-sounding chest pain were invited to take part in the study, which had local Ethical Committee approval. All patients participated in a semi-structured interview during the hospital stay.
One month after discharge, patients were sent NHNA and two health-related quality of life (HRQOL) questionnaires (described below) to be completed at home and returned by post. Data from the second test were analysed to compare the needs assessment tool with quality of life questionnaires.
Seattle Angina Questionnaire (SAQ)
This consists of 19 items grouped in five components: physical functioning (SAQ Phys), angina stability (AS), angina frequency (AF), treatment satisfaction (TS), and quality of life perception (SAQ QOL). The SAQ measures broader aspects of CHD effects than other disease-specific tools. SAQ has well-established psychometric properties and can detect physical limitations due to coronary disease, in particular in the presence of when there is co-morbidity [9]. Corresponding well with the Canadian Cardiovascular Society Classification [10].
Short Form 12 (SF-12)
The Short Form 36 (SF-36) [8] has produced consistent results in several European countries and in a diverse range of conditions; the SF-12 is an abridged form of this. It contains 12 questions from which are derived physical and mental component scores (PCS & MCS) which are as precise as the SF-36 [11,12].
Statistical analysis
Data were analysed using SPSS v11. Frequencies, association and correlation, Mann-Whitney test for non-parametric analysis, and comparing means were taken into account. As the majority of variables were in scaling format, Spearman's correlation coefficient was used to detect correlation, considered significant at p < 0.05.
Where major needs variables could be transformed to dichotomous format, as in need for a helper, difficulties in accessing healthcare facilities and satisfaction with health services, receiver operator characteristics (ROC) curves were plotted to establish the sensitivity and specificity of various HRQL domains to detect health needs [13,14].
The y axis (sensitivity) on the ROC curve represented the true positive rate, that is the proportion of patients with a low HRQL score in patients who did require a helper and reflects the ability of the specific HRQL domain to detect this specific need. The x axis represented the false-positive rate (1 minus specificity), that is the proportion of patients with a high HRQL score in patients who did not require a helper. This approach was repeated for the other two major health needs. The area under the curve was calculated to compare the sensitivity of each HRQL domain to differentiate patients in most need. This score varied between 0–1, with 1 indicating maximum sensitivity and 0.50 maximum insensitivity [13].
Results
One patient died soon after hospital discharge and five patients failed to return the questionnaire package despite reminders. Data from the remaining 43 patients (30 male) were available for analysis. Ages ranged from 46 to 88 years with 32% over 75. As a result of their medical problems, 31 patients (73%) had retired, 9 (20%) lost their job, changed to part-time work or were restricted to their home. Main health needs in respect of patients' age are shown in table 1.
Table 1.
Main health needs variables
| Variable | Subgroup | <75 | ≥ 75 | significance |
| Co-morbidity | No | 14 (48) | 4 (29) | P= 0.22 |
| Yes | 15 (52) | 10 (71) | ||
| Difficult access to health services | No | 7 (41) | 16 (61) | P = 0.19 |
| Yes | 10 (59) | 10 (39) | ||
| Factors influencing ease of access | Transport | - | 1 (20) | P < 0.01 |
| Need assistance | 2 (33) | - | ||
| Service availability | 4 (67) | 4 (80) | ||
| Request for home visit | No | 27 (93) | 10 (77) | P = 0.13 |
| Yes | 2 (7) | 3 (23) | ||
| GP periodical visit | Regular | 12 (41) | 5 (36) | P = 0.72 |
| Not regular | 17 (59) | 9 (64) | ||
| Regular medications | High burden | 14 (82) | 19 (76) | P = 0.62 |
| Low burden | 3 (18) | 6 (24) | ||
| GP satisfactory | No | 1 (3) | 1 (7) | P = 0.59 |
| Yes | 28 (97) | 13 (93) | ||
| Care dependence | No | 19 (66) | 2 (14) | P < 0.001 |
| Yes | 10 (34) | 12 (86) | ||
| Helper needed | No | 17 (59) | 4 (29) | P < 0.05 |
| Yes | 12 (41) | 10 (71) |
Mobility
73% (n = 31) had access to a private car and 22% (n = 10) relied exclusively on public transport; two-thirds were completely satisfied with these arrangements. SAQ Physical aspects of quality of life and the SF-12 PCS were strongly correlated with patients' mobility. Those who were pleased with their means of transport had a better HRQL score. (Table 2)
Table 2.
Physical and social needs
| Correlation coefficient | ||||||||
| Component | Variable | SAQ Phys | SAQ AS | SAQ AF | SAQ TS | SAQ QOL | SF12 PCS | SF12 MCS |
| Mobility | Physical activity | -.40** | -.18 | -.02 | -.18 | -.44** | -.45** | -.22 |
| Mobility restriction | .65*** | .02 | .51** | .38* | .45** | .55** | .35* | |
| Transport | -.29 | .13 | .03 | -.21 | -.25 | -.39** | -.43** | |
| Need mobility help? | -.52** | .05 | -.25 | -.22 | -.31 | -.38* | -.30 | |
| More physical activity needed? | -.53** | .004 | -.35* | -.48** | -.34 | -.27 | -.45** | |
| Access to health centre | -.43** | -.06 | -.30 | -.20 | -.17 | -.35* | -.36* | |
| Helper | Anybody looks after you? | .41** | .04 | .26 | .18 | .25 | .26 | .16 |
| Need anyone for help? | -.53*** | -.34* | -.36* | -.10 | -.43** | -.46** | -.30* | |
| Helper is happy to continue? | .08 | -.16 | .12 | .10 | -.05 | -.01 | .36* | |
| Physical needs | Anything could be improved? | -.14 | -.19 | -.23 | -.10 | -.43** | -.34* | .04 |
| Equipment for daily activities? | -.62*** | .02 | -.18 | -.38** | -.32* | -.48** | -.25 | |
| Need additional help? | -.37* | .000 | -.12 | -.31* | -.48** | -.32* | -.17 | |
| Social needs | Helpfulness of social services | .17 | -.29 | .02 | .01 | -.05 | .10 | .01 |
| Financial supports needed? | -.43** | -.01 | .06 | -.17 | -.30 | -.29 | -.07 | |
| Cleaning may help? | -.44** | -.33 | -.28 | -.32 | -.28 | -.29 | -.22 | |
| Social worker visit may help? | -.46** | -.16 | -.005 | -.16 | -.57** | -.30 | -.17 | |
| Better housing may help? | -.08 | .18 | -.09 | -.12 | -.13 | -.16 | -.08 | |
| Living alone | .10 | .02 | .15 | .09 | .06 | .08 | .09 | |
| Accommodation | .30 | -.23 | .24 | .22 | .30 | .44*** | .08 | |
| Doing hobbies | .49** | .11 | .28 | .32* | .51** | .57*** | .33* | |
| Frequency of social meetings | -.40** | -.18 | -.02 | -.18 | -.44** | -.45** | -.22 | |
Spearman rho is calculated as correlation coefficient. * indicates significance level (P value) < 0.05, ** < 0.01, and *** < 0.001.
Access to health care services
Problems in accessing local health care services were reported by 20 patients (Table 1), independent of age and co-morbidity. Impairment in physical functioning correlated closely with difficulty in accessing health care services, which was stronger in patients with no significant co-morbidity (n = 16; rho = -0.52, P < 0.05). The SAQ Physical detected this health need better than SF-12. (Table 2)
Information needs
The NHNA covered a wide range of information issues, dealing with health services, social services, treatment, nutrition and daily activities in a Likert scale format. Patients required more information about daily activities (61%), long-term treatment plan (55%) and nutrition (51%), and less frequently about social services (32%). Only one of the components in informational needs had a weak correlation with HRQL (r= 0.4, P < 0.02). (Table 3)
Table 3.
Informational needs and concerns
| SAQ Phys | SAQ AS | SAQ AF | SAQ TS | SAQ QOL | SF12 PCS | SF12 MCS | ||
| Information | Condition | .27 | .21 | .15 | .40** | .19 | .19 | .14 |
| Current treatment | .17 | .22 | -.05 | .19 | .27 | .03 | .16 | |
| Long term plan of treatment | .05 | .14 | -.03 | .18 | .25 | .01 | .04 | |
| Coping after discharge | .25 | .19 | .07 | .16 | .23 | .09 | .11 | |
| Rehabilitation | .15 | .09 | .17 | .27 | .16 | .09 | .20 | |
| Nutritional and diet | -.04 | .11 | .15 | -.10 | -.04 | -.13 | -.05 | |
| Daily Activities | .02 | .07 | .14 | .03 | .07 | -.04 | .00 | |
| Concerns | Any fear about illness? | -.21 | -.21 | -.28 | -.24 | -.34* | -.28 | -.16 |
| Thinking about concerns | .25 | .23 | .31 | .27 | .47** | .28 | .12 | |
| Seek help for concerns | .08 | .16 | .17 | .24 | .14 | .17 | .20 |
Spearman rho is calculated as correlation coefficient. * indicates significance level (P value) < 0.05, ** < 0.01.
Help needs
Eight questions were categorised in this domain to ascertain the extent of any social services input or regular help of another individual; whether the helper had their own needs; whether being a helper posed special difficulties; and any financial and household needs. 51% of the patients were dependent upon another person, particularly older patients (P < 0.001) or those who required regular assistance with daily tasks (Table 1); of these, half felt that their helper was having some difficulty in providing care due to living some distance away or neglecting their other responsibilities. Patients already dependent upon a carer had worse quality of life in physical domains (SAQ phys: rho = 0.41, P < 0.01) but no correlation was found with other components within SAQ and SF-12 (Table 2).
Patients who reported a need for a carer had poor quality of life scores. Co-morbid illness adversely affected HRQL scores (SAQ QOL: rho = -0.76; P = 0.01). The provision of a carer was anticipated to lead to a major improvement in quality of life (rho = -0.33 to -0.53).
Health care needs
Patients were questioned about their satisfaction with various health services including GP, hospital consultants, nurse, rehabilitation services, dietician, home help and social worker. Several components were investigated in this domain, including patients' satisfaction with their medical and nursing care, current treatment and a range of available health care services. Seventeen patients (40%) had been seen by a GP within the preceding two months or less; the better the HRQL score, the less demand was made upon on GPs, best detected by SAQ-AF (rho = 0.51, P < 0.001). SAQ-AF was the only HRQL component which correlated with heart disease, patients with angina having worse HRQL scores (rho = 0.37, P < 0.02).
While 28% were mostly and 30% completely satisfied in their ability to make an appointment to see the doctor or practice nurse, 42% found it hard to get to see the GP. One-fourth were dissatisfied with the care they received and 35% complained that the amount of time available to discuss issues with the GP too limited. Patients' satisfaction with referral to a consultant correlated with SAQ-TS (rho = 0.43, P = 0.01).
Forty four percent were not satisfied with dietetic and 23% with rehabilitation services; no correlation was found with HRQL scores. SAQ-TS detected correlation with health care needs components (Table 4). Mean scores of PCS and MCS in SF-12 were 35.4 and 43.4 in baseline data, which were not statistically different in younger (<65) and older (>65) patients. (Table 5) patients with poorer HRQL scores (MCS less than 50 compared with mean score in normal population) had more health needs; these patients, for example, stated more need to a helper aids, informational needs (p < 0.01), and physical aids (p = 0.01). Similar, but less significant, findings were obtained from PCS analysis.
Table 4.
Healthcare needs
| Healthcare services | SAQ Phys | SAQ AS | SAQ AF | SAQ TS | SAQ QOL | SF12 PCS | SF12 MCS |
| Current treatment | .26 | .01 | .27 | .59*** | .28 | .17 | .32* |
| Referral to consultant | .32* | -.01 | .25 | .43** | .41* | .28 | .17 |
| Hospital service | .17 | .03 | .02 | .33* | .07 | .07 | .05 |
| Rehabilitation service | .29 | .02 | -.07 | .08 | .18 | .22 | .12 |
| Nurse service | .26 | -.06 | .03 | .36* | .28 | .26 | .16 |
| GP service | .22 | .17 | .01 | .34* | .22 | .20 | .06 |
| GP understands needs? | .33* | -.03 | .10 | .15 | .16 | .33* | -.02 |
Spearman rho is calculated as correlation coefficient. • indicates significance level (P value) < 0.05, ** < 0.01, and *** < 0.001.
Table 5.
Mean SF-12 scores
| Short Form-12 components | CAD Patients: mean (SD) | Normative data: mean (SD) |
| All (n = 41) | All (n = 2333) [16] | |
| PCS | 35.4 (11) | 50 (10) |
| MCS | 43.4 (9.7) | 50 (10) |
| >65 (n = 25) | >65 (n = 511) [15] | |
| PCS | 36 (11.3) | 39.2 (13.4) |
| MCS | 43.2 (11.3) | 52.6 (10.2) |
Spearman rho is calculated as correlation coefficient. • indicates significance level (P value) < 0.05, ** < 0.01, and *** < 0.001.
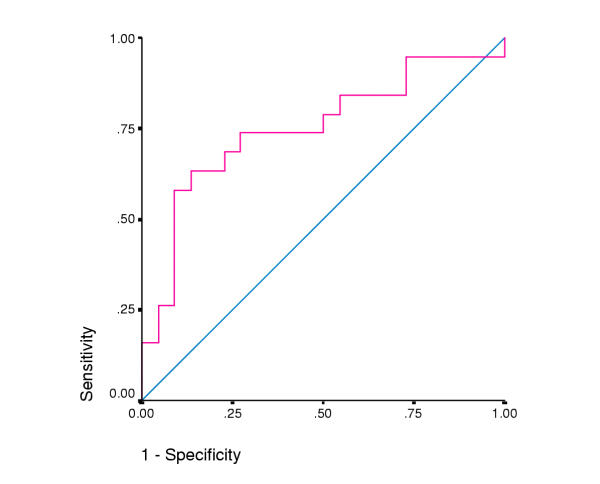
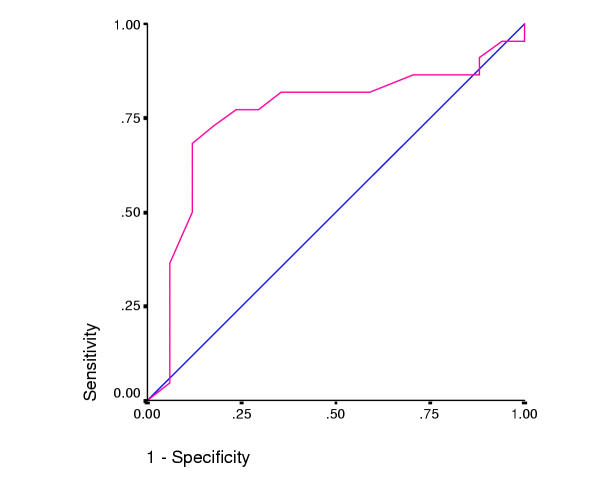
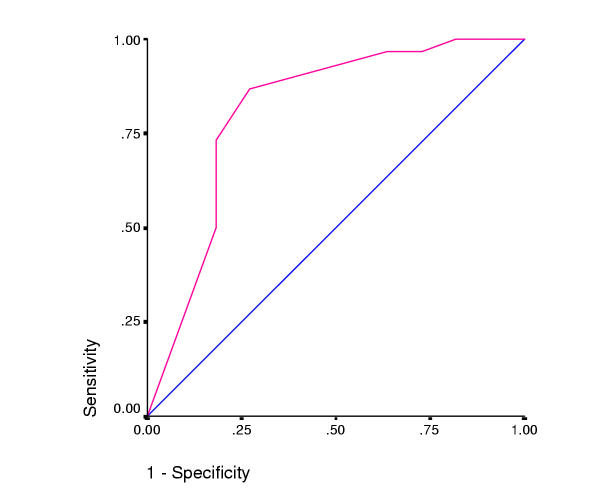
The ROC curves illustrate the sensitivity of various HRQL domains to detect health needs. (Figures 1,2,3). Area under the curve (AUC) scores are shown in table 6. The MCS in SF-12 was the most sensitive domain in detecting the need for a helper variable (0.78), the SAQ Physical domain for 'access to health services' (0.76) and SAQ satisfaction domain for 'satisfaction with health services' (0.81).
Figure 1.
Mental Component Score (SF-12) and need for helper (AUC= 0.78).
Figure 2.
SAQ Physical domain score and difficulties in accessing healthcare services (AUC= 0.76).
Figure 3.
SAQ Treatment satisfaction domain and satisfaction with current treatment in NHNA (AUC= 0.81).
Table 6.
Area Under the Curve (AUC) in sensitivity analysis
| Area under the curve (AUC) | |||
| Variable(s) | Need helper | Access to healthcare services | Satisfaction with healthcare |
| SAQ Phys | .76 | .76 | .60 |
| SAQ AS | .51 | .56 | .46 |
| SAQ AF | .67 | .67 | .56 |
| SAQ TS | .76 | .62 | .81 |
| SAQ QOL | .69 | .62 | .55 |
| SF12 PCS | .71 | .71 | .52 |
| SF12 MCS | .78 | .71 | .63 |
Spearman rho is calculated as correlation coefficient. • indicates significance level (P value) < 0.05, ** < 0.01, and *** < 0.001.
Discussion
Determining health needs on a large scale is not straightforward, as each assessment tool requires access to a wide variety of information sources. A range of instruments might be necessary to define patients' health needs across the broad spectrum of ill health, the lack of such tools reflecting the difficulty in designing suitable tools. By contrast, a considerable amount of effort has been devoted to the assessment of quality of life and so there are several readily available, validated, off-the-shelf quality of life instruments.
Our patients had lower HRQL scores compared with age-matched elder population [15] (table 5) and other normative data [16], which indicates vulnerability of these patients. A theoretical relationship between quality of life and health care needs analysis has already been proposed [17,18] and it would not be unreasonable, therefore, to suppose that patients with poor quality of life might have more health (and health care) needs. To date, this has been established in mentally, but not physically, ill patients [19].
In this study, we observed that the generic SF-12 tool not only identified general problems such as mobility, transport, and dependency upon a helper more readily than did the disease-specific Seattle Angina Questionnaire but also identified problems in patients without significant co-morbidity. Generic measures provided an overview of general health status, which is particularly helpful in a socio-economically diverse population [20] or when comparing the outcome of interventions; their generality, however, limits their ability to define specific services [21]. Disease-specific tools may be more sensitive to subtle improvements in health and response to treatment [22] and more helpful in patients with co-morbid conditions. These findings were established later in our main stage of the project [23].
We observed that quality of life tools might have potentials to identify specific and general health needs:
First, some components of the SAQ such as treatment satisfaction and angina frequency were more likely to be associated with specific health care needs. These findings warrant further investigation in larger cohorts to clarify the correlation between generic and specific HRQL and HNA instruments.
Second, although health needs seem to be inadequately covered by either the generic or the disease specific tool when administered singly, the combination of SAQ and SF-12 did provide a comprehensive assessment of need, which suggests that, together, they make a useful proxy for health needs. This has implications for those charged with identifying population health need, since the administration of 'off-the-shelf' quality of life tools afford a rapid screening test to identify both populations (such as geographic areas or the catchment area of a Primary Care Trusts) and individuals who warrant a more detailed health needs assessment.
Weak correlations in this study could be mainly attributable to the limited sample size, therefore to obtain better results it is essential to recruit more patients. Basing health care needs on quality of life scores necessarily incorporates several sources of uncertainty due to factors such as age, sex, social class and individual patient's health status. In addition, quality of life tools may fail to distinguish between health problems and the desire to get professional attention [24].
Any comprehensive evaluation of health care ought to involve assessment of not only outcome but also health needs [17]. If the health service is to optimise the use of allocated resources, identification of the needs of individuals and of the local population, whether through a surrogate such as quality of life or formal needs assessment, is an essential first step. In the absence of alternatives to ascertaining the patients' perspective on the best way to meet their needs, quality of life instruments provide a common currency to compare the effectiveness of health interventions and therefore may be deployed to guide resource allocation among competing health programs [25].
Contributor Information
Mohsen Asadi-Lari, Email: msxma@nottingham.ac.uk.
Chris Packham, Email: Chris.Packham@nottingham.ac.uk.
David Gray, Email: d.gray@nottingham.ac.uk.
References
- National Service Framework for Coronary Heart Disease, Modern standards and service models. London, Department of Health; 2000. [Google Scholar]
- de Bono D and Hopkins A, editor. Management of stable angina. London, Royal College of Physicians of London; 1994. [Google Scholar]
- House-of-Commons . National Health Service and Community Care Act. London, HMSO; 1990. [Google Scholar]
- Asadi-Lari M, Packham C, Gray D. Need for redefining needs. Health Qual Life Outcomes. 2003;1:34. doi: 10.1186/1477-7525-1-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens A, Gillam S. Health needs assessment - Needs assessment: from theory to practice. British Medical Journal. 1998;316:1448–1452. doi: 10.1136/bmj.316.7142.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickin C, St Leger S. Assessing health need using the life cycle framework. Buckingham, Open University Press; 1993. [Google Scholar]
- Hunt SM, McKenna SP, McEwen J, Backett EM, Williams J, Papp E. A quantitative approach to perceived health status: a validation study. J Epidemiol Community Health. 1980;34:281–286. doi: 10.1136/jech.34.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazier JE, Harper R, Jones NM, O'Cathain A, Thomas KJ, Usherwood T, Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. Bmj. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Fihn SD. Monitoring the quality of life in patients with coronary artery disease. Am J Cardiol. 1994;74:1240–1244. doi: 10.1016/0002-9149(94)90555-x. [DOI] [PubMed] [Google Scholar]
- Dougherty CM, Dewhurst T, Nichol WP, Spertus J. Comparison of three quality of life instruments in stable angina pectoris: Seattle Angina Questionnaire, Short Form Health Survey (SF-36), and Quality of Life Index-Cardiac Version III. J Clin Epidemiol. 1998;51:569–575. doi: 10.1016/S0895-4356(98)00028-6. [DOI] [PubMed] [Google Scholar]
- Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–1178. doi: 10.1016/S0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- Jenkinson C, Layte R, Jenkinson D, Lawrence K, Petersen S, Paice C, Stradling J. A shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? J Public Health Med. 1997;19:179–186. doi: 10.1093/oxfordjournals.pubmed.a024606. [DOI] [PubMed] [Google Scholar]
- Kirkwood BR, Sterne JAC. Essential medical statistics. 2nd. Malden, Massachusetts, Blackwell Science; 2003. [Google Scholar]
- Stucki G, Liang MH, Fossel AH, Katz JN. Relative responsiveness of condition-specific and generic health status measures in degenerative lumbar spinal stenosis. J Clin Epidemiol. 1995;48:1369–1378. doi: 10.1016/0895-4356(95)00054-2. [DOI] [PubMed] [Google Scholar]
- Pettit T, Livingston G, Manela M, Kitchen G, Katona C, Bowling A. Validation and normative data of health status measures in older people: the Islington study. Int J Geriatr Psychiatry. 2001;16:1061–1070. doi: 10.1002/gps.479. [DOI] [PubMed] [Google Scholar]
- Ware J., Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- van den Bos GA, Triemstra AH. Quality of life as an instrument for need assessment and outcome assessment of health care in chronic patients. Qual Health Care. 1999;8:247–252. doi: 10.1136/qshc.8.4.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donabedian A. Aspects of medical care administration: specifying requirements for health care. Cambridge (Ma), Harvard University Press; 1973. [Google Scholar]
- Wiersma D, van Busschbach J. Are needs and satisfaction of care associated with quality of life? An epidemiological survey among the severely mentally ill in the Netherlands. Eur Arch Psychiatry Clin Neurosci. 2001;251:239–246. doi: 10.1007/s004060170033. [DOI] [PubMed] [Google Scholar]
- Patrick DL, Deyo RA. Generic and disease-specific measures in assessing health status and quality of life. Med Care. 1989;27:S217–32. doi: 10.1097/00005650-198903001-00018. [DOI] [PubMed] [Google Scholar]
- Donovan JL, Frankel SJ, Eyles JD. Assessing the need for health status measures. J Epidemiol Community Health. 1993;47:158–162. doi: 10.1136/jech.47.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kremer B, Klimek L, Bullinger M, Mosges R. Generic or disease-specific quality of life scales to characterize health status in allergic rhinitis? Allergy. 2001;56:957–963. doi: 10.1034/j.1398-9995.2001.00919.x. [DOI] [PubMed] [Google Scholar]
- Asadi-Lari M, Packham C, Gray D. Unmet health needs in patients with coronary heart disease: implications and potential for improvement in caring services. Health Qual Life Outcomes. 2003;1:26. doi: 10.1186/1477-7525-1-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osse BH, Vernooij-Dassen MJ, de Vree BP, Schade E, Grol RP. Assessment of the need for palliative care as perceived by individual cancer patients and their families: a review of instruments for improving patient participation in palliative care. Cancer. 2000;88:900–911. doi: 10.1002/(SICI)1097-0142(20000215)88:4<900::AID-CNCR22>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Spiegelhalter DJ, Gore SM, Fitzpatrick R, Fletcher AE, Jones DR, Cox DR. Quality of life measures in health care. III: Resource allocation. Bmj. 1992;305:1205–1209. doi: 10.1136/bmj.305.6863.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]