Abstract
Amino acid substitutions widely distributed throughout the influenza hemagglutinin (HA) influence the pH of its membrane fusion activity. We have combined a number of these substitutions in double mutants and determined the effects on the pH of fusion and on the pH at which the refolding of HA required for fusion occurs. By analyzing combinations of mutations in three regions of the metastable neutral-pH HA that are rearranged at fusion pH we obtain evidence for both additive and nonadditive effects and for an apparent order of dominance in the effects of amino acid substitutions in particular regions on the pH of fusion. We conclude that there are at least three components in the structural transition required for membrane fusion activity and consider possible pathways for the transition in relation to the known differences between neutral and fusion pH HA structures.
Infection by influenza viruses involves binding to sialic acid residues of cell surface glycoconjugates, endocytosis, and fusion of viral and endosomal membranes with transfer of the genome–transcriptase complex into the cell. Membrane fusion is activated at endosomal pH, between pH 5.0 and 6.5 depending on the strain of virus, and requires changes in the structure of the fusion glycoprotein, hemagglutinin (HA) (reviewed in ref 1). These changes are specifically induced at the pH of activation and are known from crystallographic and electron microscopic analysis of HA in the neutral and fusion pH conformations to be extensive (2–5). Briefly, they involve de-trimerization of the membrane-distal globular domains that contain the HA receptor-binding sites, and relocation of the “fusion peptide” from its buried position in the native trimer interface to the tip of a newly formed 100-Å triple-stranded α-helical coiled-coil. As a result many residues move 50–100 Å from their original locations.
Among the initial experiments that indicated the extensive nature of these structural changes were those on HA mutants that fuse membranes at different pH from wild-type virus (6–9). The majority of these mutants have an elevated pH of fusion relative to wild-type HA, but one fuses at lower pH. Examination of the molecular locations of the single amino acid substitutions in the mutant HAs indicated their distribution throughout the length of the native trimer. From the x-ray structure of HA in the fusion pH conformation these locations are now known to be in regions reorganized at fusion pH.
In this study we have used combinations of these mutations in double mutants to investigate the refolding processes that are required for the conversion of HA from its metastable neutral pH conformation to its membrane fusion pH conformation. We also attempt to establish an ability to predict the consequences of particular mutations with a view to designing mutants with specific properties especially for use in experiments involving reverse genetics.
Double mutants have been used before (reviewed in ref. 10) in studies of mechanisms of enzyme activity (e.g., ref. 11) and of protein denaturation and folding (e.g., ref. 12). Here we have observed that the effects of amino acid substitutions within distinct regions of the neutral-pH HA structure appear to be additive but not only are the effects of double mutations in separate regions non-additive but also the mutations in one region can dominate those in another. Our results suggest the existence of at least three separate components to the refolding process, one centered in each region examined.
MATERIALS AND METHODS
HA Mutagenesis and Expression.
Oligonucleotide-directed mutagenesis was done either by the method of Kunkel et al. (13) or by PCR using mutant primers. Recombinant vaccinia viruses were used for HA expression under the control of either the 7.5K promoter (14) or the promoter and cis-acting elements of the cowpox p160 gene (15). Recombinants were generated as described previously (16). Methods for expression (9) and purification (17) of bromelain-released HA (BHA) for trypsin susceptibility assays have been reported in detail.
Mutant Influenza Viruses.
The D1122G mutant influenza virus (Asp-112 → Gly in the HA2 chain) was selected by growth of X-31 in the presence of amantadine at 100 μg/ml as described (6). The (D1122G, K582I) double mutant was generated by “reverse genetics” essentially as described by Enami and Palese (18). Influenza virus PR8 was used as the source of viral NP and P proteins. Madin–Darby bovine kidney (MDBK) cells were infected with the influenza virus reassortant X7F1 (H1N2) and subsequently transfected with in vitro assembled ribonucleproteins containing the mutant X31 HA RNA segment. Transfectant viruses containing the X31 HA were selected in Madin–Darby canine kidney (MDCK) cells by neutralization of viruses carrying the helper HA by using a rabbit antiserum to WSN (an H1 subtype virus).
Surface Expression of HA.
HeLa cell monolayers were dispersed by using 50 mM EDTA (in PBS) 10 h after infection with recombinant vaccinia viruses. Cell suspensions were washed with Eagle’s minimal essential medium and then with PBS containing 3% BSA and 0.2% sodium azide. Cells were incubated on ice with biotinylated monoclonal antibody HC73 for 1 h, washed twice with PBS/BSA/azide, and incubated with fluorescein-conjugated streptavidin, for 1 h on ice. The cells were washed three times with PBS/0.2% sodium azide and expression was assayed immediately by fluorescence-activated cell sorting (FACS). Surface expression as measured by HA0 cleavability was determined as in ref. 19.
Membrane Fusion and Conformational Change Assays.
Heterokaryon formation was assayed using recombinant vaccinia virus-infected baby hamster kidney (BHK) cells as described (9), and virus–liposome fusion assays were done with X-31 wild-type, D1122G single-mutant, and D1122G,K582I double-mutant influenza viruses as in ref. 8. The methods used for assaying the pH of conformational change by trypsin susceptibility (20) and ELISA (21) have also been reported.
RESULTS
The single and double mutants that we have used in this study and their locations in the structure of neutral-pH and fusion-pH HA are shown in Fig. 1. Cell surface expression of the mutant HAs, their membrane fusion activities, and changes in their structures at fusion pH were analyzed as follows.
Figure 1.
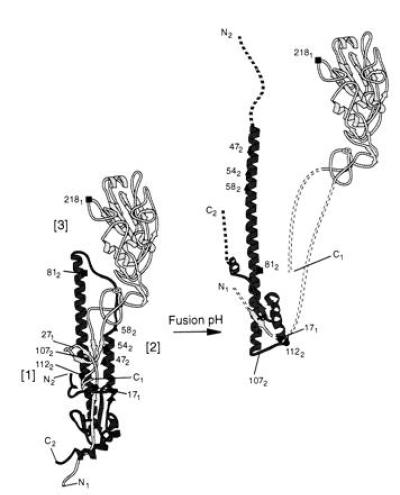
(Left) Diagram of the structure of a subunit of the neutral-pH HA trimer (2) indicating the amino and carboxyl termini of the HA1 and HA2 chains, N1 and C1 and N2 and C2, respectively; the site of HA1 exposed to trypsin digestion at fusion pH, HA1 27 (271); residue 107 of HA2 (1072), the first residue in the turn in HA2 formed at fusion pH; and the three regions of HA in which the amino acid substitutions described here are located; region [1] includes HA1 residue 17 (171) and HA2 residue 112 (1122); region [2] includes HA2 residues 47, 54, and 58; and region [3] includes residues HA1 218 and HA2 81. (Right) The structure of a subunit of the fusion-pH trimer constructed by adding the HA1 28–328 domain structure (4) to the HA2 38–175: HA1 1–27 thermolytic fragment structure (3). The locations of the mutations following the fusion-pH conformational changes are indicated by the residue numbers as in Left. The discontinuous lines indicate components of the structure that are unknown. The HA1 chain is more lightly shaded than HA2.
Estimates of Surface Expression. By FACS.
Cell surface expression of wild-type and mutant HAs was assayed by FACS following infection of HeLa monolayers with recombinant vaccinia viruses. HA-expressing monolayers were overlaid with EDTA to disperse the cells, and the cell suspensions were incubated first with biotinylated monoclonal antibody HC73, which recognizes residue HA1 145, and then fluorescein-conjugated streptavidin for FACS analysis. The data showed that all mutants are expressed on the cell surface and that the percentage of expression compared with wild-type HA ranged from 83% for mutant H171Q,K582I to 112% for mutant G2181E.
By analysis of the susceptibility of HA0 to proteolytic cleavage.
We have shown before that X-31 vaccinia recombinant-infected cells express the precursor HA0 on their surface membranes (19). Incubation of cell monolayers with trypsin results in cleavage of cell surface precursor into HA1 and HA2, and estimates of HA0 cleavability therefore provide additional evidence for surface expression. Duplicate monolayers of HA-expressing cells were incubated with or without trypsin, washed, and harvested, and cell lysates were analyzed by Western blotting as shown in Fig. 2. All mutants except H171Q,D1122G were shown to be cleavable on the cell surface. Residual HA0 in the samples after trypsin treatment is assumed to be intracellular HA0. There is more than one possible explanation for the results obtained with the H171Q,D1122G mutant in this assay. One possibility is that the mutations cause distortion of the structure of the mutant HA0 cleavage site, rendering it resistant to the action of trypsin as reported previously for an insertion mutant at this site (19). Another is that conformational changes in the mutant HA normally associated with fusion occur immediately upon cleavage of HA0 at neutral pH. In this case the HA1 domain would be further digested by trypsin. The residue changes in this mutant are each responsible for increasing the pH of fusion, and the combination of the two could result in a mutant HA for which the characteristic fusion pH structural rearrangements occur at or near neutral pH. This possibility was checked by ELISA using monoclonal antibody HC3, which, like HC73, recognizes antigenic site A in the HA1 membrane-distal domain (22). As shown in Table 1, cells expressing wild-type HA lose very little HC3 reactivity after trypsin treatment, whereas for the cells expressing the mutant HA reactivity is substantially reduced. The loss of reactivity for the mutant HA is therefore most likely due to the trypsin-mediated release of the HA1 domain from the membrane-anchored fragment of the molecule—a property which is characteristic of the fusion-active conformation (20).
Figure 2.
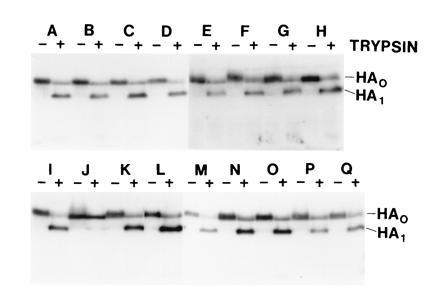
Immunoblot analysis of reducing 12% polyacrylamide gels of lysates from monolayers of HA-expressing CV 1 cells following incubation with (+) or without (-) trypsin, to show cell surface expression of HA. Lane pairs: A, wild type; B, R542E; C, E812G; D, H171Q,G2181E; E, H171Q,K582I; F, R542E,K582I; G, Q472R,K582I; H, E812G,K582I; I, G2181E,K582I; J, H171Q,D1122G; K, wild type; L, D1122G,K582I; M, G2181E; N, K582I; O, D1122G; P, H171Q; and Q, Q472R.
Table 1.
Trypsin release of H171Q,D1122G HA1 membrane-distal domains by ELISA
| Exp. | HA | HA
reactivity, A450
|
|
|---|---|---|---|
| No trypsin | Trypsin | ||
| 1 | Wild type | 1.101 | 1.010 |
| H171Q,D1122G | 1.441 | 0.621 | |
| 2 | Wild type | 1.069 | 1.125 |
| H171Q,D1122G | 1.320 | 0.722 | |
| 3 | Wild type | 0.891 | 0.860 |
| H171Q,D1122G | 0.978 | 0.443 | |
Values represent A450 of HA-expressing HeLa cell monolayers.
Determination of pH of Fusion by Mutant HAs. By heterokaryon formation.
The pH of membrane fusion was assayed by heterokaryon formation of HA-expressing BHK cell monolayers. At 15 h after infection cells were washed, treated with trypsin to cleave HA0 into HA1 and HA2, incubated at the designated pH for 1 min, and neutralized. Monolayers were then incubated in complete medium for 1 h at 37°C, fixed, and stained with 1% toluidine blue. The pH at which heterokaryon formation was observed with cells expressing wild-type HA and the single mutants is shown in Fig. 3. The K582I mutant mediates fusion at pH 0.7 below wild type (9), whereas the other mutations lead to higher pH of fusion (6–8). Fig. 4 shows the results of heterokaryon formation assays with the double mutants. Mutants H171Q,G2181E and H171Q,K582I mediate fusion at pH similar to H171Q alone, and the D1122G,K582I double mutant mediated fusion at pH close to that observed for D1122G. Similarly, the double mutants E812G,K582I and G2181E,K582I mediated heterokaryon formation at the same pH as K582I. The double mutants Q472R,K582I and R542E,K582I, on the other hand, had neither the high-pH nor the low-pH phenotypes observed for the single mutants but mediated fusion at intermediate pH. Mutant H171Q,D1122G did not cause heterokaryon formation at any pH. Under the conditions used heterokaryon formation with BHK cells is negligible with HA-expressing cells not treated with trypsin and with cells infected with wild-type (nonrecombinant) vaccinia virus (9, 21).
Figure 3.

Heterokaryon formation by single mutant HA-expressing BHK cells after incubation at the indicated pH. WT, wild type.
Figure 4.

Heterokaryon formation by double-mutant HA-expressing BHK cells after incubation at the indicated pH.
By virus–liposome fusion assays.
For the mutants D1122G and D1122G,K582I we confirmed the above results, using liposome fusion assays with egg-grown influenza virus mutants. The D1122G virus was generated by growth of X-31 virus in the presence of amantadine at millimolar concentrations (6), and the D1122G,K582I double mutant was generated by using reverse genetic techniques (18). Liposome fusion assays were done with these mutants as before (8). Viruses containing D1122G HA were shown to mediate fusion at pH 0.4 above and those containing D1122G,K582I HA at pH 0.3 above the fusion pH of wild-type virus, confirming the results obtained in the heterokaryon formation assays.
Analyses of the pH Dependence of the Structural Changes Required for Fusion by Mutant HAs. By protease susceptibility.
As a result of molecular rearrangements which occur at the pH of fusion, residues 27 and 224 of HA1 become susceptible to digestion with trypsin (20). Wild-type and mutant HAs were purified from the membranes of recombinant vaccinia virus-infected cells, and the pH of conformational change was determined for each by assays of trypsin susceptibility (Fig. 5). The results accurately reflect the coincidence between the pH of structural change and the pH of fusion determined by heterokaryon formation. Mutant G2181E,K582I and E812G,K582I HAs become susceptible to trypsin digestion at pH 4.5, the same pH as K582I HA. The double mutant D1122G,K582I becomes susceptible at pH 5.5, as does D1122G, and the pH of conformational change for the double mutants Q472R,K582I and R542E,K582I fall in between those observed for the individual single mutants.
Figure 5.

Immunoblot analysis of a 12% polyacrylamide gel run under reducing conditions, showing the trypsin susceptibility of HA1 of wild-type and mutant BHAs as a function of pH. (Left) From top to bottom, wild type, E812G, G2181E, D1122G, R542E, and Q472R. (Right) From top to bottom, K582I and double mutants E812G,K582I, G2181E,K582I, R542E,K582I, and Q472R,K582I. The pH of incubation for each BHA was (from left to right) 5.9, 5.7, 5.5, 5.3, 5.1, 4.9, 4.7, 4.5, 4.3, and 4.1.
With the mutants H171Q, H171Q,K582I, and H171Q,G2181E, all three of which formed heterokaryons at a pH significantly above wild-type HA, and for the mutant H171Q,D1122G we were unable to generate sufficient quantities of BHA for this assay. We have had similar difficulties obtaining H171Q BHA from egg-grown influenza virus, and it is likely that such mutants, being more unstable than the others, are more readily degraded during bromelain digestion.
By ELISA using conformation-specific monoclonal antibodies.
The pH of acid-induced conformational change was also determined by ELISA using the monoclonal antibodies HC3, which recognizes both the native and low-pH structures of the HA, and HC67, which reacts with residues near the trimer interface of the globular membrane-distal domains and recognizes only the native structure of the molecule. HA-expressing HeLa cells were treated with trypsin to cleave HA0, the pH was lowered and then brought to neutral, and cells were fixed for ELISA. HC67 to HC3 binding ratios were determined and plotted as a function of pH, and the midpoint of the slope was designated as the pH of conformational change. The results (Table 2, column 4) closely match those obtained from assays of trypsin susceptibility and from assays of the pH of membrane fusion. Substitution of glutamic acid for glycine at residue 218 of HA1 results in a loss of HC67 reactivity and as a consequence, mutants with this change were not analyzed by this assay.
Table 2.
Summary of data determined by different assays for ΔpH of conformational change relative to wild-type HA
| HA | ΔpH
|
|||||
|---|---|---|---|---|---|---|
| Heterokaryon formation | Trypsin susceptibility | Liposome fusion | ELISA | Mean | Mean, rounded | |
| Wild type | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| K582I | −0.7 | −0.7 | — | −0.8 | −0.73 | −0.7 |
| H171Q | +0.7 | — | — | +0.7 | +0.70 | +0.7 |
| H171Q,K582I | +0.6 | — | — | +0.6 | +0.60 | +0.6 |
| D1122G | +0.4 | +0.3 | +0.4 | +0.4 | +0.38 | +0.4 |
| D1122G,K582I | +0.3 | +0.3 | +0.3 | +0.3 | +0.30 | +0.3 |
| G2181E | +0.3 | +0.3 | — | — | +0.3 | +0.3 |
| G2181E,K582I | −0.7 | −0.7 | — | — | −0.70 | −0.7 |
| E812G | +0.3 | +0.3 | — | +0.3 | +0.30 | +0.3 |
| E812G,K582I | −0.7 | −0.7 | — | −0.9 | −0.77 | −0.8 |
| Q472R | +0.4 | +0.3 | — | +0.4 | +0.37 | +0.4 |
| Q472R,K582I | −0.3 | −0.1 | — | −0.2 | −0.20 | −0.2 |
| R542E | +0.3 | +0.1 | — | +0.2 | +0.20 | +0.2 |
| R542E,K582I | −0.5 | −0.4 | — | −0.5 | −0.47 | −0.5 |
| H171Q,G2181E | +0.7 | — | — | — | +0.70 | +0.7 |
| H171Q,D1122G Conformational change at neutral pH | ||||||
DISCUSSION
Wild-type X-31 HA is induced at pH 5.2, the pH of fusion, to rearrange extensively into a more stable structure (3, 23). All the mutant HAs containing single amino acid substitutions, expressed here from recombinant vaccinia virus vectors, behaved similarly to the HAs of mutant viruses in which they were initially identified (Table 2; refs. 6–9). All showed similar changes in their pH of fusion to the corresponding mutant virus HAs, and all rearranged structurally at these different pH values, as judged by proteolysis (Fig. 5) and antibody binding experiments (Table 2). Thus, in both virus HA and vaccinia-vector-expressed HA, mutations that influence the pH of fusion equally influence the pH at which the HA structural rearrangements occur. The locations of these mutations in regions of the molecule that change conformation at fusion pH support the interpretation that the observed rearrangements are required for fusion activity.
Differences in the pH of fusion of mutant HAs have been observed previously to be linearly related to differences in the temperatures that will trigger their structural rearrangement at neutral pH (24). Accordingly, although the thermodynamic parameters of the structural transition have not been examined under conditions where refolding is reversible for studies at equilibrium, these observations were interpreted to support the conclusion that individual mutations either increased or decreased the overall stability of the neutral-pH conformation of the mutant HAs relative to wild-type HA. Similarly, site-specific mutations that crosslink the membrane-distal domains through novel disulfide bonds are also found to stabilize the neutral-pH metastable HA and prevent the low-pH structural transition (25).
The amino acid substitutions in the mutants described here are in three regions of the neutral-pH HA structure (Fig. 1): near the amino terminus of HA2, the “fusion peptide,” region [1], residues HA1 17 and HA2 112; in the short α-helix of the HA2 α-helical hairpin, residues HA2 47, 54, and 58, region [2]; and in the interfaces between the membrane-distal HA1 globular domains, residue HA1 218, and between different regions of HA2 near the membrane-distal end of the HA2 α-helical coiled-coil, residue HA2 81, region [3]. The double mutants that we have studied fall into two groups: those in which the two mutations are in the same molecular region, as defined above, and those in which they are in different regions. In general the effects of mutations in the same region appear to be additive–e.g., the mutant HA containing HA2 Q47R and K58I amino acid substitutions that individually modify the pH of fusion by +0.3 and -0.7, respectively, has a fusion pH of -0.2 (Table 2). These results are similar to those reported for numerous double mutants of, for example, T4 lysozyme (26), phage f1 gene V DNA-binding protein (27), λ repressor (28, 29), and subtilisin (30), that have been analyzed for their effects on protein folding and denaturation and the mechanisms of protein activities. By contrast, the properties of the double mutants containing amino acid substitutions in different regions appear to be nonadditive; the HA containing HA2 D112G and K58I substitutions, for example, that individually modify the pH of fusion by +0.4 and -0.7, has a pH of fusion of +0.3. Such nonadditive double mutants have also been observed in other proteins and have been used in attempts to deduce the molecular bases for the observed consequences of individual mutations. For example, the majority of double mutants in staphylococcal nuclease were found to be nonadditive with regard to their effects on enzyme stability (31), providing evidence consistent with a proposal for two core regions in the molecule that interact but individually contribute unequally to the stability of its denatured structure (12). In studies of tyrosine tRNA synthetase, particular additive and nonadditive combinations of substitutions were used to identify interactions between residues in the active site and to propose mechanisms for the modification of enzyme activity by specific mutations (11).
Examination of the phenotypes of the double mutants containing amino acid substitutions in different regions of HA also indicates that the consequences of substitutions near the fusion peptide, region [1] (Fig. 1), apparently override those of mutations in the other two regions and, in turn, that the substitutions in the short α-helix, region [2], apparently override mutations in the membrane-distal region [3]. This apparent order of dominance is reminiscent of a proposal (32) for an ordering of the structural changes induced at fusion pH that was based on the acquisition of anti-peptide antibody reactivities by HA as a function of time after incubation at fusion pH. However, although our observations can be interpreted as evidence for the existence of at least three components in the HA refolding process, they do not indicate the order in which they occur, nor do they establish whether refolding follows only a single pathway each time or a number of pathways simultaneously. A comparison of the neutral-pH HA conformation with the fusion-pH conformation indicates at least five major structural differences: (i) the HA1 membrane-distal domains of the neutral-pH trimer are dissociated from each other and from HA2 at fusion pH (Fig. 1); (ii) the HA2 amino-terminal “fusion peptide” is expelled at fusion pH from its buried position in the neutral-pH trimer interface; (iii) the α-helical coiled-coil region of the central fibrous HA2 domain is extended at fusion pH toward the “fusion peptide,” displacing it more than 100 Å; (iv) a central portion of the long α-helix carboxyl terminal to the coiled-coil region (near HA2 residue 107) is refolded to form a 180° turn and the neutral-pH membrane-proximal domain of each subunit is folded back against the coiled-coil; and (v) residues near the carboxyl terminus of bromelain-released HA2 appear to become disordered, possibly creating a flexible link to the viral membrane. This comparison suggests more than one plausible refolding pathway. For example, an initiating event that led to the dissociation of the HA1 membrane-distal domains could destabilize the interactions between HA1 and the extended chain region of HA2 that links the two α-helices in the neutral-pH structure. Removal of HA1 in this way could allow refolding of HA2 into the extended α-helical coiled-coil that its sequence prefers, as shown by sequence-based structure prediction (33), synthetic peptide studies (34), x-ray crystallography (3), and structural analyses of HA2 expressed alone in Escherichia coli (35). Alternatively, the structural transition could initially involve expulsion of the “fusion peptide.” Since the amino terminus of the “fusion peptide” is adjacent to residue HA2 112 in the long central α-helix (Fig. 1), to residues near HA2 107 in the α-helix that refold at fusion pH to form the turn, and to a loop in HA1 containing HA1 27 that becomes sensitive to proteases at fusion pH (4, 20), a triggering event in this cluster that released the “fusion peptide” could simultaneously destabilize the adjacent α-helix so that it unfolded into a bend and began dissociation of HA1 from HA2 near HA1 residue 27 in the membrane-proximal stem region of the neutral-pH structure. Selecting between such alternatives, the majority of refolding molecules would take the path with the lowest energy barrier against refolding. Raising the energy barrier on such a preferred pathway by mutation or decreasing the barrier on a disfavored pathway could alter the predominant mechanism by which HA refolds; our observations may reflect such alterations.
Experiments are in progress which may detect such alternatives, but whatever the mechanistic explanations of the double-mutant phenotypes they provide information essential for attempts to manipulate X-31 HA stability and function by specific mutations. They have also allowed the construction of an infectious X-31 mutant containing the K582I substitution that in a single mutant would prevent infection by requiring lower than endosomal pH to trigger its fusion activity, by using the double mutant D1122G,K582I. High-yield growth of this double mutant and crystallization of the mutant HA will provide information on the structure of this region of the molecule, which is poorly defined in the x-ray structure of X-31 HA (36). However, one of the consequences of our observations is that the effects of particular amino acid substitutions in wild-type HA cannot be extrapolated to HAs that have already been modified by other mutations. This finding appears to preclude prediction of the effects of similar mutations in different HA backgrounds—e.g., in HAs of other antigenic subtypes, irrespective of the degree of local structural conservation in the region of HA to be modified.
Acknowledgments
We acknowledge the assistance of David Stevens, Rose Gonsalves, and Carol Newman and helpful discussions with Alan Jasanoff. This work was supported by a National Institutes of Health grant (D.C.W.) and the MRC (J.J.S.). D.C.W. is an investigator of the Howard Hughes Medical Institute.
Footnotes
Abbreviations: HA, hemagglutinin; BHA, bromelain-released HA.
References
- 1.Skehel J J, Bizebard T, Bullough P A, Hughson F M, Knossow M, Steinhauer D A, Wharton S A, Wiley D C. Cold Spring Harbor Symp Quant Biol. 1995;60:573–580. doi: 10.1101/sqb.1995.060.01.061. [DOI] [PubMed] [Google Scholar]
- 2.Wilson I A, Skehel J J, Wiley D C. Nature (London) 1981;289:366–373. doi: 10.1038/289366a0. [DOI] [PubMed] [Google Scholar]
- 3.Bullough P A, Hughson F M, Skehel J J, Wiley D C. Nature (London) 1994;371:37–43. doi: 10.1038/371037a0. [DOI] [PubMed] [Google Scholar]
- 4.Bizebard T, Gigant B, Rigolet P, Rasmussen B, Diat O, Boseck P, Wharton S A, Skehel J J, Knossow M. Nature (London) 1995;376:92–94. doi: 10.1038/376092a0. [DOI] [PubMed] [Google Scholar]
- 5.Wharton S A, Calder L J, Ruigrok R W H, Skehel J J, Steinhauer D A, Wiley D C. EMBO J. 1995;14:240–246. doi: 10.1002/j.1460-2075.1995.tb06997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daniels R S, Downie J C, Hay A J, Knossow M, Skehel J J, Wang M L, Wiley D C. Cell. 1985;40:431–439. doi: 10.1016/0092-8674(85)90157-6. [DOI] [PubMed] [Google Scholar]
- 7.Daniels R S, Jeffries S, Yates P, Schild G C, Rogers G N, Paulson J C, Wharton S A, Douglas A R, Skehel J J, Wiley D C. EMBO J. 1987;6:1459–1465. doi: 10.1002/j.1460-2075.1987.tb02387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wharton S A, Skehel J J, Wiley D C. Virology. 1986;149:27–35. doi: 10.1016/0042-6822(86)90083-8. [DOI] [PubMed] [Google Scholar]
- 9.Steinhauer D A, Wharton S A, Skehel J J, Wiley D C, Hay A J. Proc Natl Acad Sci USA. 1991;88:11525–11529. doi: 10.1073/pnas.88.24.11525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wells J A. Biochemistry. 1990;29:8509–8517. doi: 10.1021/bi00489a001. [DOI] [PubMed] [Google Scholar]
- 11.Carter P J, Winter G, Wilkinson A J, Fersht A R. Cell. 1984;38:835–840. doi: 10.1016/0092-8674(84)90278-2. [DOI] [PubMed] [Google Scholar]
- 12.Shortle D. Adv Protein Chem. 1995;46:217–247. doi: 10.1016/s0065-3233(08)60336-8. [DOI] [PubMed] [Google Scholar]
- 13.Kunkel T A, Roberts J D, Zakour R A. Methods Enzymol. 1987;159:367–382. doi: 10.1016/0076-6879(87)54085-x. [DOI] [PubMed] [Google Scholar]
- 14.Venkatesan S, Baroudy B M, Moss B. Cell. 1981;25:805–813. doi: 10.1016/0092-8674(81)90188-4. [DOI] [PubMed] [Google Scholar]
- 15.Patel D D, Ray C A, Druker R P, Pickup D J. Proc Natl Acad Sci USA. 1988;85:9431–9435. doi: 10.1073/pnas.85.24.9431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mackett M, Smith G L, Moss B. J Virol. 1984;49:857–864. doi: 10.1128/jvi.49.3.857-864.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brand C M, Skehel J J. Nature (London) New Biol. 1972;238:145–147. doi: 10.1038/newbio238145a0. [DOI] [PubMed] [Google Scholar]
- 18.Enami M, Palese P. J Virol. 1991;65:2711–2713. doi: 10.1128/jvi.65.5.2711-2713.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steinhauer D A, Wharton S A, Skehel J J, Wiley D C. J Virol. 1995;69:6643–6651. doi: 10.1128/jvi.69.11.6643-6651.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skehel J J, Bayley P M, Brown E B, Martin S R, Waterfield M D, White J M, Wilson I A, Wiley D C. Proc Natl Acad Sci USA. 1982;79:968–972. doi: 10.1073/pnas.79.4.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steinhauer D A, Wharton S A, Wiley D C, Skehel J J. Virology. 1991;183:445–448. doi: 10.1016/0042-6822(91)90867-b. [DOI] [PubMed] [Google Scholar]
- 22.Daniels R S, Douglas A R, Skehel J J, Wiley D C. J Gen Virol. 1983;64:1657–1662. doi: 10.1099/0022-1317-64-8-1657. [DOI] [PubMed] [Google Scholar]
- 23.Ruigrok R W H, Aitken A, Calder L J, Martin S R, Skehel J J, Wharton S A, Weis W, Wiley D C. J Gen Virol. 1988;69:2785–2795. doi: 10.1099/0022-1317-69-11-2785. [DOI] [PubMed] [Google Scholar]
- 24.Ruigrok R W H, Martin S R, Wharton S A, Skehel J J, Bayley P M, Wiley D C. Virology. 1986;155:484–497. doi: 10.1016/0042-6822(86)90210-2. [DOI] [PubMed] [Google Scholar]
- 25.Godley L, Pfeifer J, Steinhauer D, Ely B, Shaw G, Kaufmann R, Suchanek E, Pabo C, Skehel J J, Wiley D C, Wharton S A. Cell. 1992;68:635–645. doi: 10.1016/0092-8674(92)90140-8. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Z-J, Baase W A, Matthews B W. Biochemistry. 1991;30:2012–2017. doi: 10.1021/bi00222a001. [DOI] [PubMed] [Google Scholar]
- 27.Sandberg W S, Terwilliger T C. Proc Natl Acad Sci USA. 1993;90:8367–8371. doi: 10.1073/pnas.90.18.8367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hecht M H, Sturtevant J M, Sauer R T. Proteins. 1986;1:43–46. doi: 10.1002/prot.340010108. [DOI] [PubMed] [Google Scholar]
- 29.Stearman R S, Frankel A D, Freire E, Liu B, Pabo C O. Biochemistry. 1988;27:7571–7574. doi: 10.1021/bi00419a059. [DOI] [PubMed] [Google Scholar]
- 30.Cunningham B C, Wells J A. Protein Eng. 1987;1:319–325. doi: 10.1093/protein/1.4.319. [DOI] [PubMed] [Google Scholar]
- 31.Green S M, Shortle D. Biochemistry. 1993;32:10131–10139. doi: 10.1021/bi00089a032. [DOI] [PubMed] [Google Scholar]
- 32.White J M, Wilson I A. J Cell Biol. 1987;105:2887–2896. doi: 10.1083/jcb.105.6.2887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ward C W, Dopheide T A A. Aust J Biol Sci. 1980;33:441–447. doi: 10.1071/bi9800441. [DOI] [PubMed] [Google Scholar]
- 34.Carr C M, Kim P S. Cell. 1993;73:823–832. doi: 10.1016/0092-8674(93)90260-w. [DOI] [PubMed] [Google Scholar]
- 35.Chen J, Wharton S A, Weissenhorn W, Calder L J, Hughson F M, Skehel J J, Wiley D C. Proc Natl Acad Sci USA. 1995;92:12205–12209. doi: 10.1073/pnas.92.26.12205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weis W I, Brünger A T, Skehel J J, Wiley D C. J Mol Biol. 1990;212:737–761. doi: 10.1016/0022-2836(90)90234-D. [DOI] [PubMed] [Google Scholar]


