Abstract
Background:
Although the cardiac biomarker troponin T (cTnT) is strongly related to mortality in end-stage renal disease, the independent association of N-terminal pro-B-type natriuretic peptide (NT-proBNP) and cTnT in predicting outcomes is unknown.
Objective:
To determine factors associated with NT-proBNP and cTnT, and to determine whether these levels are associated with mortality.
Study Design:
Cohort Study
Settings and Participants:
Asymptomatic hemodialysis patients (n=150) in 4 university-affiliated hemodialysis units.
Exposure and Outcomes:
For cross-sectional analysis, echocardiographic variables as exposures and N-terminal proBNP and cardiac troponin T as outcomes; for longitudinal analysis, association of N-terminal proBNP and cardiac troponin T as exposures to all-cause and cardiovascular disease mortality as outcomes.
Results:
In a multivariate regression analysis, low midwall fractional shortening a measure of poor systolic function was an independent correlate of log NT-proBNP (p<0.01), while left ventricular mass index was an independent correlate of cTnT (p<0.01). Over a median follow-up of 24 months, 46 patients died of which, 26 died due to cardiovascular causes. NT-ProBNP had a strong graded relationship with all-cause (Hazard Ratio (HR) 1.54, 4.78 and 4.03 for increasing quartiles, Chi2 32.2, p<0.001) and cardiovascular mortality (HR 2.99, 10.95, 8.54 Chi2 23.66, p<0.01), while cTnT had a weaker relationship with all-cause (HR 1.57, 2.32, 3.39, Chi2 23.09, p<0.01) and cardiovascular mortality (HR 1, 0.81, 2.12, 2.14, Chi2 15.05, p=0.1). The combination of the two biomarkers did not improve the association with all-cause or cardiovascular mortality compared to NT-proBNP alone. NT-proBNP was a marker of mortality even after adjusting for left ventricular mass index and midwall fractional shortening.
Limitations:
Our cohort was predominantly black and of limited sample size.
Conclusion:
NT-proBNP strongly correlates with left ventricular systolic dysfunction and is more strongly associated with mortality than cTnT in asymptomatic hemodialysis patients.
Keywords: NT-proBNP, Troponin T, left ventricular mass, left ventricular function, mortality, hemodialysis
Introduction
It is now well established that chronic kidney disease (CKD) is associated with a markedly increased risk for cardiovascular disease, and the majority of deaths in end stage renal disease (ESRD) are from cardiovascular causes 1. Left ventricular hypertrophy and left ventricular systolic dysfunction are highly prevalent patients with ESRD and are associated with poor cardiovascular outcomes 2;3. Given that cardiac biomarkers may reflect left ventricular structure and function and predict outcomes, there has been an escalating interest in the measurement of such biomarkers in asymptomatic ESRD patients to stratify cardiovascular risk.
Cardiac troponins T and I are released into the circulation in response to myocardial necrosis and are renally cleared. 4 The prognostic value of cardiac troponin t (cTnT) in predicting mortality is well established in ESRD 5-13. B-type natriuretic peptide (BNP) is a hormone that is released in response to wall stretch of the cardiac ventricles. N-terminal proBNP (NT-proBNP) is an inactive fragment that is released along with BNP in a 1:1 ratio, cleared renally, and removed by hemodialysis (HD) to a very small extent 14. The levels of both BNP and NT-proBNP are elevated in the ESRD population 4;14. The prognostic value of BNP or NT-proBNP is less well established in ESRD 15-17.
Very few studies have directly compared the prognostic significance of BNP or NT-proBNP and cTnT in HD patients 18-20. The correlation between cTnT and left ventricular mass and function has been inconsistent in previous studies 7;21;22. Conversely, the relationship between BNP/NT-proBNP and left ventricular mass and systolic function has been more consistent - inverse correlation with left ventricular systolic function and a direct correlation with left ventricular mass 15;16;23-25. Since NT-proBNP has been consistently shown to correlate with poor left ventricular systolic function, it is possible that this biomarker may predict outcomes better than cTnT. Given the paucity of data about the comparative value of these two biomarkers in predicting outcomes and the relationship with left ventricular mass and systolic function, we measured baseline levels of cTnT and NT-proBNP, echocardiographic left ventricular mass and function and followed these patients for all-cause and cardiovascular mortality. The primary objectives of our study were: To determine the presence, nature, and strength of the association of the cardiac biomarkers (NT-proBNP and cTnT) and left ventricular mass and function in asymptomatic hemodialysis patients; and to evaluate the ability of the biomarkers alone and in combination to predict all-cause and cardiovascular mortality in these individuals.
Materials and Methods
Participants
A total of 150 chronic hemodialysis patients were recruited between September 2003 and February 2005. The sample was drawn from 355 patients on thrice-weekly hemodialysis from 4 dialysis units affiliated with Indiana University of which 48% were women, 36% were diabetic and 72% were black. Because there were fewer white patients who were recruited, the racial make up of 126 patients who were screened but who did not participate were analyzed. Of these, 41 were blacks (76%), 12 (22%) whites and 1 (2%) Asian met the recruitment criteria but refused participation. 55 (76%) blacks, 15 whites (21%) and 2 (3%) Asians did not meet one of the inclusion or exclusion criteria. Because 27/126 (21%) whites did not meet eligibility or refused participation, our sample comprised of more black participants that the overall composition from which the sample was derived from. Baseline evaluation was conducted over a two week period with longitudinal follow-up. The study was approved by the Institutional Review Board of Indiana University and Research and Development Committee of the Roudebush VA Medical Center, Indianapolis and all subjects gave written informed consent.
The characteristics of this cohort have been previously reported 26. The inclusion criteria were age >18 years, patients on chronic hemodialysis for ≥ 3 months, compliance with hemodialysis treatments as defined by less than two missed dialysis per month, medically stable in the opinion of the investigator, and willingness to give informed consent. The exclusion criteria were active drug abuse, chronic atrial fibrillation, body mass index ≥ 40 kg/m2, inability to learn or perform home BP monitoring, expected survival <6 months, active cancer or known human immunodeficiency virus positivity, and recent (<2 weeks) change in antihypertensive drugs or dry weight.
Measurements
Biomarkers
All lab measurements were done pre-dialysis and specimen was obtained from the patient's arterio-venous access or tunneled dialysis catheter for hemodialysis. N-terminal proBNP (NT-proBNP) was measured using the Elecsys proBNP immunoassay (Roche Diagnostics, Indianapolis, IN). Cutoffs used were the following: ages< 75 years - 125 pg/ml; ≥ 75 years - 450 pg/ml. Cardiac troponin T (cTnT) was measured using the Elecsys cardiac troponin T assay (Elecsys Troponin T STAT Immunoassay, third generation; Roche Diagnostics). The limit of detection as stated by the manufacturer is <0.01 ng/mL. The 99th percentile of a reference population is 0.01 ng/mL and the threshold for diagnosis of myocardial infarction in 0.1 ng/mL.
Home Blood Pressure Monitoring
Home blood pressure (BP) monitoring was performed over one week using a validated self-inflating automatic oscillometric device (HEM 705 CP, Omron Healthcare).27
Echocardiography
Technique and measurements
Two-dimensional guided M-mode echocardiograms were performed by one technician immediately after a mid-week hemodialysis session with a digital cardiac ultrasound machine (Cypress Acuson, Siemens Medical) as reported previously 28. Left ventricular mass was calculated using these measurements and corrected for height2.7 measured in meters as it corrects for the effects of obesity, correlates better with long-term outcomes in dialysis patients 29 and recent studies have demonstrated that similar thresholds can be used for blacks and whites 30. Left ventricular mass >51 g/m2.7 was taken as evidence of left ventricular hypertrophy.
Midwall fractional shortening
Midwall fractional shortening (mWFS) is a well established marker of systolic ventricular dysfunction in patients with left ventricular hypertrophy and is more sensitive than endocardial fractional shortening in detecting systolic dysfunction. In patients on hemodialysis, mWFS and change in mWFS is reported to be of prognostic importance 31. mWFS was estimated by the elliptic model of left ventricular geometry as described by de Simone et al 32. The third percentile of mWFS is reported as 14.2% 33. Those with <14.2% mWFS were said to have impaired myocardial systolic function. Nine patients did not have satisfactory echocardiograms.
Primary and Secondary End Points
The primary end point was all-cause mortality and the secondary end-point was cardiovascular mortality. Death due to myocardial infarction, stroke, pulmonary edema or sudden cardiac death was classified as cardiovascular mortality. Patients were censored on the date of their last dialysis if they underwent transplantation or left the dialysis unit. The mortality data were gathered by two physicians who had no knowledge of the biomarker levels in the patients.
Statistical Analyses
Patients were stratified into quartiles according to the NT-proBNP and cTnT concentrations. Continuous variables were analyzed using univariate analysis of variance (ANOVA) examining linear contrast. Data were expressed as means ± standard deviation. Categorical variables were expressed as percentages and analyzed using the Pearson's Chi-Square test. We performed multivariate regression analysis to determine the independent determinants of log NT-proBNP and log cTnT using a stepwise approach incorporating the following variables: age, gender, ethnicity, body mass index, years of ESRD, current smoker, etiology of ESRD by diabetes, past cardiovascular disease, antihypertensive medication use, home systolic and diastolic BP, serum albumin, hemoglobin, left ventricular mass index, and mWFS. Cox proportional hazards regression models were used to determine the relationship of the biomarkers and mortality outcomes. Proportional hazards assumption was checked using Schoenfeld residuals and by evaluating the statistical significance of the interaction of the log of time with linear predictor in the Cox model. The Cox model was adjusted for age, race, gender, serum albumin, and diabetes as etiology of ESRD. Cumulative hazard curves were generated by quartiles of the biomarker adjusted for the covariates at their mean values. Hazard ratios and 95 % confidence intervals for all-cause and cardiovascular mortality were obtained for quartiles 2-4 of NT-proBNP and cTnT using quartile 1 as the reference category. The goodness of fit of the Cox model was evaluated by examining the likelihood ratio Chi square statistic. All analyses were conducted using SPSS software version 14.0 (SPSS Inc., Chicago, IL) or Stata 9.0 (College Station, TX). The P values reported are two-sided and significant at < 0.05.
Results
Patient Characteristics
The clinical characteristics of the patients are shown in Table 1. The cohort represented an asymptomatic population on hemodialysis, with a mean age of about 56 years and a mean duration of ESRD of about 5.2 years. The majority were black, representing about 90% of the study population. A previous history of cardiovascular disease defined as a history of myocardial infarction, percutaneous coronary intervention, coronary or peripheral vascular bypass surgeries, stroke, aortic aneurysm, or non-traumatic amputation was present in 47 %. The mean left ventricular mass/height2.7 was about 59 g/m2.7 and mean mWFS about 14.4 % respectively. Left ventricular hypertrophy was present in 67% and left ventricular dysfunction in 44% of the participants. NT-proBNP and cTnT levels were both markedly elevated in our study population with median levels of 3276.5 pg/ml and 0.056 ng/ml respectively. 83 % of our cohort had elevated cTnT levels based on the cut-off 0.01 ng/ml used in the reference population, and 27 % had cTnT levels > 0.1 ng/ml, which is the threshold for diagnosis of myocardial infarction. NT-proBNP was elevated in 100% of our study population based on the normal cut-offs.
Table 1.
Clinical characteristics of the study population by Quartiles of N-Terminal Pro-B-type Natriuretic Peptide
| Clinical Characteristic | Overall | Quartile 1 | Quartile 2 | Quartile 3 | Quartile 4 | p |
|---|---|---|---|---|---|---|
|
N-Terminal Pro-B-type Natriuretic Peptide (pg/mL) |
215-1150.5 |
1150.5- 3276.5 |
3276.5- 7880.5 |
7880.5- ≥ 35000 |
||
| n | 150 | 37 | 38 | 38 | 37 | |
| Age (years) | 55.8 ± 13.5 |
52.6 ± 16.5 | 57.0 ± 12.9 | 56.5 ± 12.6 | 57.0 ± 11.7 | 0.20 |
| Men | 94 (63%) | 23 (62%) | 26 (68%) | 25 (66%) | 20 (54%) | 0.60 |
| Ethnicity | 0.82 | |||||
| White | 13 (9%) | 2 (5%) | 4 (11%) | 3 (8%) | 4 (11%) | |
| Black | 135 (90%) | 35 (95%) | 33 (87%) | 34 (89%) | 33 (89%) | |
| Other | 2 (1%) | 0 | 1 (3%) | 1 (3%) | 0 | |
| Pre-dialysis weight (kg) | 81.8 ± 19.5 |
89.6 ± 21.0 | 85.7 ± 19.2 | 76.3 ± 16.4 | 75.7 ± 18.2 | <0.001 |
| Post-dialysis weight (kg) | 79.1 ± 19.0 |
86.9 ± 20.4 | 83.0 ± 18.8 | 73.7 ± 15.8 | 72.9 ± 17.5 | <0.001 |
| Body Mass Index (kg/m2) | 26.7 ± 6.1 | 29.3 ± 6.3 | 27.4 ± 6.1 | 24.9 ± 4.9 | 25.1 ± 6.4 | 0.001 |
| Years of end-stage renal disease | 5.2 ± 5.2 | 5.1 ± 4.0 | 5.3 ± 5.0 | 5.2 ± 6.0 | 5.2 ± 5.6 | 0.94 |
| Current Smoker | 56 (37%) | 5 (16%) | 17 (45%) | 16 (42%) | 18 (49%) | <0.01 |
| Etiology of end-stage renal disease | 0.75 | |||||
| Diabetes Mellitus | 47 (31%) | 11 (30%) | 12 (32%) | 10 (26%) | 14 (38%) | |
| Others | 103 (69%) | 26 (70%) | 26 (68%) | 28 (74%) | 23 (62%) | |
| Past Cardiovascular Disease | 71 (47%) | 15 (41%) | 16 (42%) | 21 (55%) | 19 (51%) | 0.51 |
| Antihypertensive Medications | 124 (83%) | 25 (68%) | 35 (92%) | 33 (87%) | 31 (84%) | 0.03 |
| Mean Home Blood Pressure (mmHg) | ||||||
| Systolic | 142.1± 22.7 |
131.3 ± 24.2 |
142.5 ± 21.6 |
144.6 ± 21.2 |
149.6 ± 21.0 |
0.001 |
| Diastolic | 79.9 ± 13.4 |
75.5 ± 11.4 |
81.8 ± 13.5 |
81.0 ± 12.7 |
81.1 ± 15.5 |
0.13 |
| Urea Reduction Ratio (%) | 73.0 ± 7.6 | 73.0 ± 7.9 | 72.6 ± 7.0 | 72.5 ± 8.4 | 74.2 ± 7.1 | 0.56 |
| Albumin (g/dL) | 3.8 ± 0.4 | 3.9 ± 0.3 | 3.8 ± 0.5 | 3.8 ± 0.3 | 3.8 ± 0.4 | 0.28 |
| Hemoglobin (g/dL) | 12.4 ± 1.5 | 12.5 ± 1.3 | 12.8 ± 1.6 | 12.4 ± 1.2 | 12.0 ± 1.8 | 0.06 |
| Left Ventricular Mass/Ht2.7 (g/m2.7) | 59.0 ± 17.5 |
52.5 ± 18.3 | 59.1 ± 15.3 | 60.6 ± 17.6 | 63.4 ± 17.9 | 0.01 |
| Mid-Wall Fractional Shortening (observed %) | 14.4 ± 2.6 | 15.3 ± 2.1 | 15.0 ± 2.8 | 13.6 ± 2.4 | 13.8 ± 2.6 | <0.01 |
| Cardiac Troponin-T (ng/mL) | 0.082 ± 0.087 |
0.056 ± 0.053 |
0.056 ± 0.059 |
0.091 ± 0.096 |
0.125±0.111 | <0.001 |
± indicates standard deviation. Parenthesis have percent of patients.
Continuous variables p-values computed through Univariate ANOVA examining linear contrast
Categorical variables p-values computed through Pearson's Chi-Square To convert albumin or hemoglobin (g/dL) to g/L, multiply by 10.
NT-proBNP quartile analysis
The characteristics of the study population by quartiles of NT-proBNP are shown in Table 1. A significant association was noted between NT-proBNP quartiles and body mass index, smoking, home systolic blood pressure. Patients with higher quartiles of NT-proBNP had a lower body mass index and higher home systolic blood pressure compared to those with lower quartiles of NT-proBNP (P=0.001 for both). The prevalence of active smokers was significantly higher among those with NT-proBNP in Quartiles 2 - 4 than in Quartile 1 (p=0.007). There was a linear increase in the left ventricular mass/ht2.7 with increasing quartiles of NT-proBNP (p=0.011). NT-proBNP was more significantly associated with mWFS than with left ventricular mass. The mWFS was lower among those with NT-proBNP levels in the higher quartiles of than those with NT-proBNP in the lower quartiles (p=0.003).
Cardiac troponin T quartile analysis
The clinical characteristics of the study population by quartiles of cTnT are shown in Table 2. There was a significant correlation between cTnT quartiles and age, diabetes mellitus, home systolic blood pressure, and serum albumin. Patients with cTnT levels in the higher quartiles were older, had a higher prevalence of diabetes mellitus, higher home systolic BP, and lower serum albumin concentration. Left ventricular mass was higher among those with cTnT levels in quartiles 3-4 compared to those in quartiles 1-2 (P=0.006). However, there was no significant correlation between cTnT and mWFS (p=0.51).
Table 2.
Clinical characteristics of the study population by Quartiles of Cardiac Troponin-T
| Clinical Characteristic | Overall | Quartile 1 | Quartile 2 | Quartile 3 | Quartile 4 | p |
|---|---|---|---|---|---|---|
| Cardiac Troponin-T (ng/mL) | ≤ 0.01 - 0.022 |
0.022 - 0.056 |
0.056 - 0.106 |
0.106 - 0.569 |
||
| N | 150 | 38 | 38 | 37 | 37 | |
| Age (years) | 55.8 ± 13.5 | 47.9 ± 13.5 | 59.5 ± 11.4 | 62.4 ± 13.0 | 53.6 ± 11.8 | 0.03 |
| Men | 94 (63%) | 22 (58%) | 27 (71%) | 22 (59%) | 23 (62%) | 0.64 |
| Ethnicity | 0.72 | |||||
| White | 13 (9%) | 2 (5%) | 5 (13%) | 3 (8%) | 3 (8%) | |
| Black | 135 (90%) | 36 (95%) | 32 (84%) | 33 (89%) | 34 (92%) | |
| Other | 2 (1%) | 0 | 1 (3%) | 1 (3%) | 0 | |
| Pre-dialysis weight (kg) | 81.8 ± 19.5 | 82.0 ± 19.5 | 82.2 ± 18.9 | 77.8 ± 16.8 | 85.3 ± 22.5 | 0.71 |
| Post-dialysis weight (kg) | 79.1 ± 19.0 | 79.3 ± 19.0 | 79.6 ± 18.5 | 75.2 ± 16.3 | 82.4 ± 21.8 | 0.72 |
| Body Mass Index (kg/m2) | 26.7 ± 6.1 | 26.8 ± 6.0 | 25.8 ± 5.9 | 26.8 ± 6.6 | 27.4 ± 6.3 | 0.54 |
| Years of end-stage renal disease | 5.2 ± 5.2 | 5.6 ± 6.7 | 5.4 ± 5.5 | 5.3 ± 4.7 | 4.4 ± 2.6 | 0.38 |
| Current Smoker | 56 (37%) | 14 (37%) | 14 (37%) | 12 (32%) | 16 (43%) | 0.82 |
| Etiology of end-stage renal disease | <.01 | |||||
| Diabetes Mellitus | 47 (31%) | 5 (13%) | 14 (37%) | 10 (27%) | 18 (49%) | |
| Others | 103 (69%) | 33 (87%) | 24 (63%) | 27 (73%) | 19 (51%) | |
| Past Cardiovascular Disease | 71 (47%) | 11 (29%) | 20 (53%) | 20 (54%) | 20 (54%) | 0.07 |
| Antihypertensive Medications | 124 (83%) | 33 (87%) | 33 (87%) | 30 (81%) | 28 (76%) | 0.52 |
| Mean Home Blood Pressure (mmHg) | ||||||
| Systolic | 142.1± 22.7 | 139.1 ± 20.8 |
133.4 ± 24.6 |
147.9 ± 21.8 |
148.3 ± 20.9 |
0.02 |
| Diastolic | 79.9 ± 13.4 | 83.3 ± 12.1 | 74.1 ± 10.7 | 79.7 ± 11.5 | 82.6 ± 17.4 | 0.73 |
| Urea reductuion ratio (%) | 73.0 ± 7.6 | 72.5 ± 8.6 | 73.3 ± 6.2 | 74.0 ± 6.9 | 72.3 ± 8.6 | .99 |
| Albumin (g/dL) | 3.8 ± 0.4 | 4.0 ± 0.3 | 3.8 ± 0.4 | 3.7 ± 0.4 | 3.8 ± 0.4 | 0.04 |
| Hemoglobin (g/dL) | 12.4 ± 1.5 | 12.8 ± 1.3 | 12.5 ± 1.6 | 12.1 ± 1.6 | 12.4 ± 1.5 | 0.20 |
| Left Ventricular Mass/Ht2.7 (g/m2.7) | 59.0 ± 17.5 | 50.8 ± 16.5 | 59.1 ± 15.2 | 65.1 ± 20.1 | 61.0 ± 15.0 | <.01 |
| Mid-Wall Fractional Shortening (observed %) | 14.4 ± 2.6 | 14.7 ± 2.8 | 14.2 ± 2.6 | 14.3 ± 2.7 | 14.3 ± 2.3 | 0.51 |
| NT-proBNP | 6141 ± 7814 | 4095 ± 6197 |
2910 ± 2329 |
7615 ± 6067 |
10090 ± 11714 |
<0.001 |
± indicates standard deviation. Parenthesis have percent of patients.
Continuous variables p-values computed through Univariate ANOVA examining linear contrast
Categorical variables p-values computed through Pearson's Chi-Square To convert albumin or hemoglobin (g/dL) to g/L, multiply by 10.
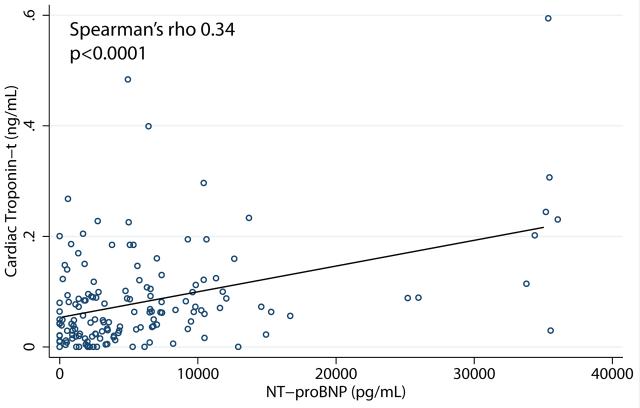
The relationship between cTnT and NT-proBNP is shown in Figure 1. The Spearman's correlation coefficient was 0.34.
Figure 1.
Bivariate relationship between cardiac troponin t (cTnT) and n-terminal pro-B-type natriuretic peptide. The Spearman's correlation coefficient was 0.34 (p<0.001).
Multivariate regression analysis between variables and log NT-proBNP and cTnT
The independent determinants of log NT-proBNP and log cTnT by multivariate regression analysis using a stepwise approach and their β coefficients are shown in Table 3. The independent determinants of log NT-proBNP were current smokers, low hemoglobin, higher home systolic BP, lower home diastolic BP, and low mWFS. The independent determinants of cTnT were older age, male gender, diabetes as ESRD etiology, and high left ventricular mass index.
Table 3.
| Risk Factor | log NT-proBNP | P | log cTnT | P |
|---|---|---|---|---|
| Coefficient (95% CI) | Coefficient (95% CI) | |||
| Age (yrs) | 0.02 (0.00, 0.03) | 0.02 | ||
| Gender (Male) | 0.42 (0.07, 0.77) | 0.1 | ||
| Etiology of ESRD (diabetes) |
0.60 (0.25, 0.95) | <0.01 | ||
| Current Smoker | 0.85 (0.48, 1.21) | <0.001 | ||
| Hemoglobin (g/dL) | −0.15 (−0.27, −0.03) | 0.01 | ||
| Home systolic BP (mm Hg) |
0.02 (0.01, 0.03) | <0.001 | ||
| Home diastolic BP (mm Hg) |
−0.02 (−0.04,0.00) | 0.04 | ||
| Left ventricular Mass index (g/m2.7) |
0.01 (0.00, 0.02) | <0.01 | ||
| Mid wall fractional shortening (%) |
−0.10 (−0.18, −.03) | <.01 | ||
| r2 | 0.31 | 0.19 | ||
| Std. error of estimate | 0.99 | 0.93 |
Beta Coefficients are for 1 unit change
Survival Analysis
The median follow-up was for 24 months. 46 patients died of which, 26 died due to cardiovascular causes. The major cardiovascular cause of death was sudden cardiac death, followed by myocardial infarction, stroke, and pulmonary edema. The crude all-cause and cardiovascular mortality rates were 157 and 89/1000 patient-years respectively.
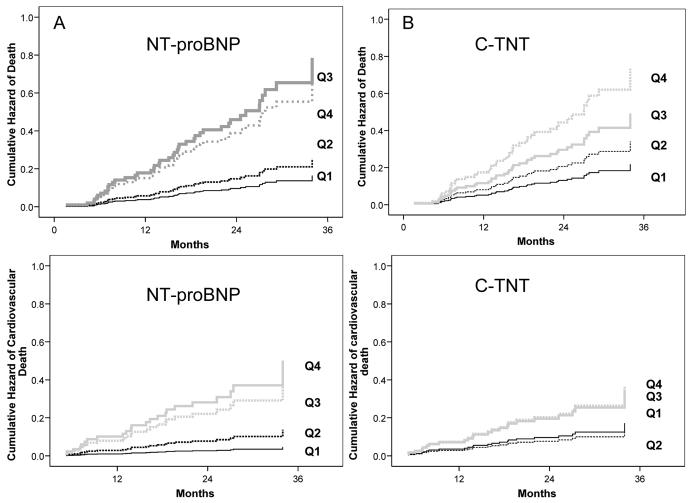
Figure 2a shows the adjusted cumulative hazard curves for quartiles of NT-proBNP. There was a direct relationship between NT-proBNP levels and mortality, with a significantly greater risk of all-cause and cardiovascular mortality among those with NT-proBNP quartiles 2-4 compared to the first quartile. Figure 2b shows the adjusted cumulative hazard curves for quartiles of cTnT. There was an increase in all-cause mortality with the higher quartiles of cTnT levels, but the correlation was not as significant for cardiovascular mortality. Table 4 shows the hazard ratios for total and cardiovascular mortality by quartiles of NT-proBNP and cTnT using quartile 1 as the reference category. The hazard ratios for those with quartiles 3 and 4 compared with quartile 1 of NT-proBNP were 4.78 and 4.03 respectively for all-cause mortality and 10.95 and 8.54 respectively for cardiovascular mortality. The hazard ratios for quartiles 3 and 4 compared with quartile 1 of cTnT were 2.32 (p=0.2) and 3.39 (p=0.04) respectively for all-cause mortality and 2.12 (p=0.3) and 2.14 (p=0.3) respectively for cardiovascular mortality.
Figure 2.
Figure 2a - Adjusted cumulative hazard curves for quartiles of NT-proBNP for all-cause and cardiovascular mortality. Covariates adjusted for were age, race, gender, serum albumin, and ESRD etiology (diabetes vs non-diabetes) plotted at their mean values. NT-proBNP had a strong graded relationship with all-cause and cardiovascular mortality.
Figure 2b - Adjusted cumulative hazard curves for quartiles of cTnT for all-cause and cardiovascular mortality. Covariates adjusted for were age, race, gender, serum albumin, and ESRD etiology (diabetes vs non-diabetes) plotted at their mean values. cTnT had a strong graded relationship with all-cause mortality, but a weaker relationship with cardiovascular mortality.
Table 4.
Hazard Ratios for all-cause and Cardiovascular Mortality by Quartiles of NT-proBNP and c-TNT
| Biomarker | All-cause mortality | Cardiovascular mortality | |||||
|---|---|---|---|---|---|---|---|
| NT-proBNP | Range (pg/mL) | HR | 95 % CI | p | HR | 95 % CI | p |
| Quartile 1 | 215-1150.5 | 1 | 1 | ||||
| Quartile 2 | 1150.5-3276.5 | 1.54 | 0.46 - 5.19 | 0.5 | 2.99 | 0.33 - 27.40 | 0.32 |
| Quartile 3 | 3276.5-7880.5 | 4.78 | 1.58 - 14.51 | <.01 | 10.95 | 1.38 - 86.73 | 0.02 |
| Quartile 4 | 7880.5- ≥ 35000 | 4.03 | 1.31 - 12.40 | 0.02 | 8.54 | 1.04 - 69.98 | 0.05 |
| LRT | χ2 − 14.9, p <0.01 | χ2 − 12.3, p<0.01 | |||||
| cTnT | Range (ng/mL) | ||||||
| Quartile 1 | ≤ 0.01 - 0.022 | 1 | 1 | ||||
| Quartile 2 | 0.022 - 0.056 | 1.57 | 0.46 - 5.35 | 0.5 | 0.81 | 0.16 - 4.06 | 0.80 |
| Quartile 3 | 0.056 - 0.106 | 2.32 | 0.69 - 7.86 | 0.2 | 2.12 | 0.47 - 9.54 | 0.34 |
| Quartile 4 | 0.106 - 0.569 | 3.39 | 1.04 - 11.07 | 0.04 | 2.14 | 0.48 - 9.60 | 0.32 |
| LRT | χ2 − 5.8, p =0.12 | χ2 − 3.7, p0.30 | |||||
All models are adjusted for age, race, gender, serum albumin, and ESRD etiology (diabetes vs non-diabetes) HR= Hazard Ratio; CI = confidence interval, LRT=Likelihood ratio test comparing the model incorporating biomarker to one containing the covariates only.
Combined analysis of the biomarkers for mortality outcomes
Table 5 shows unadjusted analyses for all-cause mortality using quartiles of NT-proBNP and cTnT separately and when considered together. In the combined model whereas cTnT lost statistical significance, NT-proBNP remained significant for the upper two quartiles. Results were similar for cardiovascular mortality (data not shown).
Table 5.
Hazard Ratios for all-cause mortality by quartiles of NT-proBNP and c-TNT separately and considered together
| Biomarker | All-cause mortality | Adjusted All-cause mortality | |||||
|---|---|---|---|---|---|---|---|
| NT-proBNP | Range (pg/mL) | HR | 95 % CI | p | HR | 95 % CI | p |
| Quartile 1 | 215-1150.5 | 1 | 1 | ||||
| Quartile 2 | 1150.5-3276.5 | 2.09 | 0.63 - 6.95 | 0.2 | 2.01 | 0.61-6.69 | 0.03 |
| Quartile 3 | 3276.5-7880.5 | 5.86 | 1.97-17.4 | 0.001 | 5.21 | 1.73-15.67 | <0.01 |
| Quartile 4 | 7880.5- ≥ 35000 | 4.79 | 1.61-14.23 | <0.01 | 3.72 | 1.18-11.72 | 0.03 |
| LRT | χ2 − 3.42, p=0.33 | ||||||
| cTnT | Range (ng/mL) | ||||||
| Quartile 1 | ≤ 0.01 - 0.022 | 1 | 1 | ||||
| Quartile 2 | 0.022 - 0.056 | 1.95 | 0.67 - 5.71 | 0.2 | 1.95 | 0.66-5.73 | 0.22 |
| Quartile 3 | 0.056 - 0.106 | 3.28 | 1.20 - 8.98 | 0.02 | 2.28 | 0.81-6.46 | 0.12 |
| Quartile 4 | 0.106 - 0.569 | 3.13 | 1.20 - 9.12 | 0.02 | 2.4 | 0.84-6.91 | 0.10 |
| LRT | χ2 − 12.4, p<0.01 | ||||||
Adjusted all-cause mortality for NT-proBNP is adjusted for cTnT. Adjusted all-cause mortality for cTnT is adjusted for NT-proBNP. HR= Hazard Ratio; CI = confidence interval. , LRT=Likelihood ratio test comparing the model incorporating the adjustment to the unadjusted model.
Because of limited sample size we conducted an additional Cox analysis to evaluate the interaction between NT-proBNP and cTnT by splitting the data at the median and evaluating the interaction term for all-cause and cardiovascular mortality. The interaction terms for NT-proBNP × cTnT for all cause mortality (p=0.3) and cardiovascular mortality (p=0.2) were not significant.
Independent effect of biomarkers after adjustment for echocardiography
Table 6 shows unadjusted analyses for all-cause mortality using quartiles of LVMI and mWFS separately and when adjusted for NT-proBNP and cTNT. LVMI was not a determinant of all-cause mortality (Model 1) in contrast to mWFS (Model 2). In bivariate analysis, log cTNT (Model 3) and log NT-proBNP (Model 4) were both determinants of mortality. cTNT retained its value after adjusting for LVMI (Model 5), mWFS (Model 6) or both (Model 7) as a mortality marker. Similarly, NT-proBNP retained its value after adjusting for LVMI (Model 8), mWFS (Model 9) or both (Model 10) as a mortality marker. Results were similar for cardiovascular mortality (data not shown).
Table 6.
Hazard Ratios for all-cause mortality by echocardiographic and biomarker parameters
| Model | Biomarker | Range (g/m2.7) |
HR | 95 % CI | p | LR χ2 |
|---|---|---|---|---|---|---|
| 1 | LVMI | 1.4 | ||||
| Quartile 1 | <48.8 | 1 | ||||
| Quartile 2 | 48.8-58.2 | 0.96 | 0.41 - 2.26 | 0.93 | ||
| Quartile 3 | 58.2-70.2 | 1.2 | 0.54 - 2.68 | 0.65 | ||
| Quartile 4 | >70.2 | 0.72 | 0.30 - 1.74 | 0.47 | ||
| 2 | mWFS | Range (%) | 11.1 | |||
| Quartile 1 | >16.1 | 1 | ||||
| Quartile 2 | 16.1-14.7 | 0.86 | 0.32-2.30 | 0.77 | ||
| Quartile 3 | 12.4-14.7 | 1.05 | 0.39-2.79 | 0.93 | ||
| Quartile 4 | <12.4 | 2.78 | 1.22-6.36 | 0.015 | ||
| 3 | log cTnT | 1.61 | 1.19-2.17 | 0.002 | 10 | |
| 4 | log NT-proBNP | 1.63 | 1.27-2.09 | <0.001 | 15.3 | |
| 5 | LVMI + log cTNT | 11.8 | ||||
| log cTnT | 1.65 | 1.21-2.25 | 0.002 | |||
| 6 | mWFS + log cTNT | 20.9 | ||||
| log cTnT | 1.63 | 1.19-2.22 | 0.002 | |||
| 7 | LVMI + mWFS + log cTnT | 25.6 | ||||
| log cTnT | 1.71 | 1.25-2.34 | 0.001 | |||
| 8 | LVMI + log NT-proBNP | |||||
| log NT-proBNP | 1.71 | 1.30-2.24 | <0.001 | 17.4 | ||
| 9 | mWFS + log NT proBNP | 21.7 | ||||
| log NT-proBNP | 1.57 | 1.18-2.07 | 0.002 | |||
| 10 | LVMI + mWFS + log NT-proBNP | 26.5 | ||||
| log NT-proBNP | 1.65 | 1.24-2.20 | 0.001 |
LVMI= left-ventricular mass index, mWFS= midwall fractional shortening, cTNT = cardiac troponin-t, NT-proBNP = n-terminal pro B-type natriuretic peptide, HR=Hazard ratio, CI=Confidence interval
Discussion
The two biomarkers NT-ProBNP and cTnT appear to measure different aspects of cardiovascular disease. NT-proBNP had an independent correlation with left ventricular systolic dysfunction, while cTnT independently correlated with left ventricular mass index. Left ventricular systolic dysfunction measured by mWFS was a stronger marker of death in contrast to left ventricular mass index. NT-ProBNP had a strong graded relationship with all-cause and cardiovascular mortality, while cTnT had a weaker relationship with all-cause and cardiovascular mortality. Both biomarkers, cTnT and NT-proBNP, were determinants of death independent of echocardiographic findings. The combination of the two biomarkers did not seem to improve the prediction of all-cause or cardiovascular mortality than NT-proBNP alone.
Previous studies have noted higher levels of the biomarkers among those with cardiovascular disease 7;21;34. We did not note such a relationship, although there was a higher prevalence of past cardiovascular disease among those with cTnT in quartiles 2-4 compared to the first quartile (p=0.07). Active smoking, low hemoglobin, high systolic and low diastolic home BP were independent predictors of NT-proBNP. Conversely, older age, male gender, and diabetes as ESRD etiology were independent predictors of cTnT. An independent association between these variables and cTnT has also been noted previously 6;21.
NT-proBNP quartiles had an inverse correlation with left ventricular systolic function and a direct correlation with LVMI in our study. Other studies have also shown similar findings. 16 Most recently, Madsen et al. reported that NT-proBNP correlated inversely with left ventricular ejection fraction and directly with left ventricular hypertrophy 15. cTnT had a direct relationship with LVMI but no correlation with left ventricular systolic function in our study. Studies evaluating the relationship between cTnT and left ventricular parameters have yielded conflicting results. Mallamaci et al. noted that cTnT had a significant correlation with left ventricular mass and left ventricular systolic dysfunction in their cohort of 258 HD patients 6;22. DeFilippi et al. found no significant association between cTnT quartiles and left ventricular hypertrophy (p=0.45), but reduced left ventricular ejection fraction was twice as frequent among those in the higher cTnT quartiles than those with lower cTnT quartiles (p=0.07) 7. In an analysis of 58 HD patients, NT-proBNP correlated with left ventricular mass and left ventricular ejection fraction, but the correlation between cTnT and left ventricular mass was lost when NTpro-BNP was included in the multivariate analysis 19.
Our study was also distinctive in that we performed echocardiography in all of the patients immediately post-dialysis, thereby minimizing any influence of volume on left ventricular measurements. The timing of echocardiography in relation to dialysis was not always consistent in previous studies that evaluated the correlation between biomarkers and left ventricular structure and function. An additional unique feature of our study was that we used mWFS, which is considered to be a more sensitive marker of left ventricular systolic function than left ventricular ejection fraction that has been used in previous studies.
NT-proBNP had a strong predictive value for all-cause and cardiovascular mortality -mortality was higher for those with NT-proBNP levels in quartiles 2-4 compared to those in the first quartile. Zoccali et al. studied 246 patients on HD and peritoneal dialysis and noted that those with BNP levels in the 3rd tertile had a significantly higher risk of death and cardiovascular death. Moreover, BNP remained an independent predictor of death in a Cox model that also included left ventricular ejection fraction and LVMI 16. In the study by Madsen et al. of 109 HD patients, NT-proBNP predicted all-cause mortality. 15 Some studies have also found BNP to be a prognostic indicator despite adjustment for LVMI and left ventricular ejection fraction 16;25. We also found that NT-proBNP was an independent correlate of mortality even after adjusting for LVMI and left ventricular systolic function. Given that BNP is released in response to ventricular stretch and is strongly correlated with left ventricular structure and function, the pathophysiologic mechanisms underlying the independent relationship of BNP with outcomes after accounting for LVMI and left ventricular ejection fraction remains uncertain.
Data regarding the prognostic value of cTnT in ESRD is more robust than that for BNP or NT-proBNP and supported by a meta-analysis 13. Our data extends the prior observations in that cTNT was of prognostic value despite adjusting for LVMI and left ventricular systolic function. The pathophysiologic mechanisms underlying this independent relationship with mortality remains to be elucidated.
Only three studies have directly compared the prognostic value of the two biomarkers cTnT and BNP/NT-proBNP in the HD population. In 58 HD patients NT-proBNP level was strongly associated with cTnT and cTnT was the best predictor of death that occurred in 14 patients. 19 In 399 HD patients, cTnT and cTnI, but not NT-proBNP were independent predictors of all-cause mortality. 20 However, this risk was determined based on the normal cut-offs. Given that 99 % of this study cohort had elevated NT-proBNP levels based on the normal cut-off, it is of little surprise that abnormal NT-proBNP was not a marker of mortality. On the other hand, the tertile of either NT-proBNP or cTnT were strong predictors mortality. No head to head comparisons were made. More recently, NT-proBNP and cTnT in 134 HD patients were both found to be independent predictors of the composite end-point of death or cardiovascular events. 18 The survival curves were obtained based on the threshold levels of the biomarkers for hypervolemia. Therefore, whether or not cTnT independently contributed to the survival prediction by NT-proBNP is not clear from this study. In our analysis, although both NT-proBNP and cTnT by themselves were determinants of all-cause and cardiovascular mortality, the relationship was stronger for NT-proBNP than cTnT. More importantly, cTnT had no added value in predicting all-cause mortality when the cohort was divided by the median NT-proBNP levels and the interaction effect was analyzed. This is the first study that demonstrates the superior prognostic value of NT-proBNP over cTnT in asymptomatic HD patients.
The limitations of our study were the relatively small sample size. The study cohort was predominantly black and whether the results of this study can be extrapolated to patients of other ethnicities is unclear. However, our survival analyses were adjusted for ethnicity and current data do not suggest that NT-proBNP levels vary between ethnicities. We also relied on medical records to determine the cause of death that could have resulted in misclassification of the causes of mortality. However, we did not lose any subject during follow-up.
In summary, NT-proBNP was a better predictor of all-cause and cardiovascular mortality than cTnT. Whether or not these biomarkers should be routinely measured in ESRD patients still remains to be answered. Future studies will hopefully address the significance of sequential measurement of these biomarkers in ESRD patients and the effects of therapeutic interventions based on the biomarker levels. Among patients with heart failure, BNP-guided therapy lowered the combined end point of CHF-related death or hospital stay that was mediated primarily through increased use of beta-blockers and angiotensin-converting enzyme inhibitors 35. Whether or not such interventions guided by NT-proBNP in asymptomatic ESRD patients will provide similar impact on outcomes remains to be seen.
Acknowledgement
Supported by a grant from NIH-NIDDK 5RO1-063020-05. Participation of Dialysis Clinics Inc in this study is gratefully acknowledged.
REFERENCES
- 1.Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108:2154–2169. doi: 10.1161/01.CIR.0000095676.90936.80. [DOI] [PubMed] [Google Scholar]
- 2.Foley RN, Parfrey PS, Harnett JD, et al. The prognostic importance of left ventricular geometry in uremic cardiomyopathy. J Am Soc Nephrol. 1995;5:2024–2031. doi: 10.1681/ASN.V5122024. [DOI] [PubMed] [Google Scholar]
- 3.Foley RN, Parfrey PS, Harnett JD, et al. Clinical and echocardiographic disease in patients starting end-stage renal disease therapy. Kidney Int. 1995;47:186–192. doi: 10.1038/ki.1995.22. [DOI] [PubMed] [Google Scholar]
- 4.Roberts MA, Hare DL, Ratnaike S, et al. Cardiovascular biomarkers in CKD: pathophysiology and implications for clinical management of cardiac disease. Am J Kidney Dis. 2006;48:341–360. doi: 10.1053/j.ajkd.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 5.Iliou MC, Fumeron C, Benoit MO, et al. Prognostic value of cardiac markers in ESRD: Chronic Hemodialysis and New Cardiac Markers Evaluation (CHANCE) study. Am J Kidney Dis. 2003;42:513–523. doi: 10.1016/s0272-6386(03)00746-7. [DOI] [PubMed] [Google Scholar]
- 6.Mallamaci F, Zoccali C, Parlongo S, et al. Troponin is related to left ventricular mass and predicts all-cause and cardiovascular mortality in hemodialysis patients. Am J Kidney Dis. 2002;40:68–75. doi: 10.1053/ajkd.2002.33914. [DOI] [PubMed] [Google Scholar]
- 7.DeFilippi C, Wasserman S, Rosanio S, et al. Cardiac troponin T and C-reactive protein for predicting prognosis, coronary atherosclerosis, and cardiomyopathy in patients undergoing long-term hemodialysis. JAMA. 2003;290:353–359. doi: 10.1001/jama.290.3.353. [DOI] [PubMed] [Google Scholar]
- 8.Havekes B, van Manen JG, Krediet RT, et al. Serum troponin T concentration as a predictor of mortality in hemodialysis and peritoneal dialysis patients. Am J Kidney Dis. 2006;47:823–829. doi: 10.1053/j.ajkd.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 9.Kanwar M, Hashem M, Rosman H, et al. Usefulness of clinical evaluation, troponins, and C-reactive protein in predicting mortality among stable hemodialysis patients. Am J Cardiol. 2006;98:1283–1287. doi: 10.1016/j.amjcard.2006.05.064. [DOI] [PubMed] [Google Scholar]
- 10.Dierkes J, Domrose U, Westphal S, et al. Cardiac troponin T predicts mortality in patients with end-stage renal disease. Circulation. 2000;102:1964–1969. doi: 10.1161/01.cir.102.16.1964. [DOI] [PubMed] [Google Scholar]
- 11.Ooi DS, Zimmerman D, Graham J, et al. Cardiac troponin T predicts long-term outcomes in hemodialysis patients. Clin Chem. 2001;47:412–417. [PubMed] [Google Scholar]
- 12.Apple FS, Murakami MM, Pearce LA, et al. Predictive value of cardiac troponin I and T for subsequent death in end-stage renal disease. Circulation. 2002;106:2941–2945. doi: 10.1161/01.cir.0000041254.30637.34. [DOI] [PubMed] [Google Scholar]
- 13.Khan NA, Hemmelgarn BR, Tonelli M, et al. Prognostic value of troponin T and I among asymptomatic patients with end-stage renal disease: a meta-analysis. Circulation. 2005;112:3088–3096. doi: 10.1161/CIRCULATIONAHA.105.560128. [DOI] [PubMed] [Google Scholar]
- 14.Rosner MH. Measuring risk in end-stage renal disease: is N-terminal pro brain natriuretic peptide a useful marker? Kidney Int. 2007;71:481–483. doi: 10.1038/sj.ki.5002140. [DOI] [PubMed] [Google Scholar]
- 15.Madsen LH, Ladefoged S, Corell P, et al. N-terminal pro brain natriuretic peptide predicts mortality in patients with end-stage renal disease in hemodialysis. Kidney Int. 2007;71:548–554. doi: 10.1038/sj.ki.5002087. [DOI] [PubMed] [Google Scholar]
- 16.Zoccali C, Mallamaci F, Benedetto FA, et al. Cardiac natriuretic peptides are related to left ventricular mass and function and predict mortality in dialysis patients. J Am Soc Nephrol. 2001;12:1508–1515. doi: 10.1681/ASN.V1271508. [DOI] [PubMed] [Google Scholar]
- 17.Naganuma T, Sugimura K, Wada S, et al. The prognostic role of brain natriuretic peptides in hemodialysis patients. Am J Nephrol. 2002;22:437–444. doi: 10.1159/000065272. [DOI] [PubMed] [Google Scholar]
- 18.Sommerer C, Beimler J, Schwenger V, et al. Cardiac biomarkers and survival in haemodialysis patients. Eur J Clin Invest. 2007;37:350–356. doi: 10.1111/j.1365-2362.2007.01785.x. [DOI] [PubMed] [Google Scholar]
- 19.Fernandez-Reyes MJ, Mon C, Heras M, et al. Predictive value of troponin T levels for ischemic heart disease and mortality in patients on hemodialysis. J Nephrol. 2004;17:721–727. [PubMed] [Google Scholar]
- 20.Apple FS, Murakami MM, Pearce LA, et al. Multi-biomarker risk stratification of N-terminal pro-B-type natriuretic peptide, high-sensitivity C-reactive protein, and cardiac troponin T and I in end-stage renal disease for all-cause death. Clin Chem. 2004;50:2279–2285. doi: 10.1373/clinchem.2004.035741. [DOI] [PubMed] [Google Scholar]
- 21.Iliou MC, Fumeron C, Benoit MO, et al. Factors associated with increased serum levels of cardiac troponins T and I in chronic haemodialysis patients: Chronic Haemodialysis And New Cardiac Markers Evaluation (CHANCE) study. Nephrol Dial Transplant. 2001;16:1452–1458. doi: 10.1093/ndt/16.7.1452. [DOI] [PubMed] [Google Scholar]
- 22.Mallamaci F, Zoccali C, Parlongo S, et al. Diagnostic value of troponin T for alterations in left ventricular mass and function in dialysis patients. Kidney Int. 2002;62:1884–1890. doi: 10.1046/j.1523-1755.2002.00641.x. [DOI] [PubMed] [Google Scholar]
- 23.Nishikimi T, Futoo Y, Tamano K, et al. Plasma brain natriuretic peptide levels in chronic hemodialysis patients: influence of coronary artery disease. Am J Kidney Dis. 2001;37:1201–1208. doi: 10.1053/ajkd.2001.24523. [DOI] [PubMed] [Google Scholar]
- 24.Zeng C, Wei T, Jin L, et al. Value of B-type natriuretic peptide in diagnosing left ventricular dysfunction in dialysis-dependent patients. Intern Med J. 2006;36:552–557. doi: 10.1111/j.1445-5994.2006.01136.x. [DOI] [PubMed] [Google Scholar]
- 25.Cataliotti A, Malatino LS, Jougasaki M, et al. Circulating natriuretic peptide concentrations in patients with end-stage renal disease: role of brain natriuretic peptide as a biomarker for ventricular remodeling. Mayo Clin Proc. 2001;76:1111–1119. doi: 10.4065/76.11.1111. [DOI] [PubMed] [Google Scholar]
- 26.Agarwal R, Andersen MJ, Bishu K, et al. Home blood pressure monitoring improves the diagnosis of hypertension in hemodialysis patients. Kidney Int. 2006;69:900–906. doi: 10.1038/sj.ki.5000145. [DOI] [PubMed] [Google Scholar]
- 27.Agarwal R, Andersen MJ, Bishu K, et al. Home blood pressure monitoring improves the diagnosis of hypertension in hemodialysis patients. Kidney Int. 2006;69:900–906. doi: 10.1038/sj.ki.5000145. [DOI] [PubMed] [Google Scholar]
- 28.Agarwal R, Brim NJ, Mahenthiran J, et al. Out-of-hemodialysis-unit blood pressure is a superior determinant of left ventricular hypertrophy. Hypertension. 2006;47:62–68. doi: 10.1161/01.HYP.0000196279.29758.f4. [DOI] [PubMed] [Google Scholar]
- 29.Zoccali C, Benedetto FA, Mallamaci F, et al. Prognostic impact of the indexation of left ventricular mass in patients undergoing dialysis. J Am Soc Nephrol. 2001;12:2768–2774. doi: 10.1681/ASN.V12122768. [DOI] [PubMed] [Google Scholar]
- 30.Nunez E, Arnett DK, Benjamin EJ, et al. Optimal threshold value for left ventricular hypertrophy in blacks: the Atherosclerosis Risk in Communities study. Hypertension. 2005;45:58–63. doi: 10.1161/01.HYP.0000149951.70491.4c. [DOI] [PubMed] [Google Scholar]
- 31.Zoccali C, Benedetto FA, Tripepi G, et al. Left ventricular systolic function monitoring in asymptomatic dialysis patients: a prospective cohort study. J Am Soc Nephrol. 2006;17:1460–1465. doi: 10.1681/ASN.2005111240. [DOI] [PubMed] [Google Scholar]
- 32.de Simone G, Devereux RB, Roman MJ, et al. Assessment of left ventricular function by the midwall fractional shortening/end-systolic stress relation in human hypertension. J Am Coll Cardiol. 1994;23:1444–1451. doi: 10.1016/0735-1097(94)90390-5. [DOI] [PubMed] [Google Scholar]
- 33.Devereux RB, Roman MJ, Palmieri V, et al. Left ventricular wall stresses and wall stress-mass-heart rate products in hypertensive patients with electrocardiographic left ventricular hypertrophy: the LIFE study. Losartan Intervention For Endpoint reduction in hypertension. J Hypertens. 2000;18:1129–1138. doi: 10.1097/00004872-200018080-00019. [DOI] [PubMed] [Google Scholar]
- 34.Osajima A, Okazaki M, Tamura M, et al. Comparison of plasma levels of mature adrenomedullin and natriuretic peptide as markers of cardiac function in hemodialysis patients with coronary artery disease. Nephron. 2002;92:832–839. doi: 10.1159/000065459. [DOI] [PubMed] [Google Scholar]
- 35.Jourdain P, Jondeau G, Funck F, et al. Plasma brain natriuretic peptide-guided therapy to improve outcome in heart failure: the STARS-BNP Multicenter Study. J Am Coll Cardiol. 2007;49:1733–1739. doi: 10.1016/j.jacc.2006.10.081. [DOI] [PubMed] [Google Scholar]