Abstract
Investigations into the causes of declines in late-life disability have largely focused on the role of contemporaneous factors. Adopting a life-course perspective as a backdrop, in this paper we ask whether there also has been a role for selected early- and mid-life factors in the decline, and if so whether these factors have been operating through changes in the risks of disability onset or recovery. Drawing on five waves from 1995 to 2004 of the US Health and Retirement Study, we found for the 75 and older population in the United States that the prevalence of difficulty with activities of daily living (ADL) declined from 30.2% in 1995 to 26.0% in 2004, whereas the trend in difficulty with instrumental activities of daily living (IADL) was flat. Onset of ADL limitations also was reduced during this period while recovery increased. Changes in the educational composition of the older population were linked to declines in the prevalence of ADL limitations, but there were also modest contributions of changes in mother's education, self-rated childhood health, and lifetime occupation. Declines in late-life vision impairments and increases in wealth also contributed substantially to the downward trend, and had chronic conditions not increased, it would have been even larger. Reductions in the onset of ADL limitations were partly driven by changes in educational attainment of respondents and their mothers and, in late-life, better vision and wealth. In contrast, the recovery trend was not accounted for by changes in early- or mid-life factors. We conclude that early- and mid-life factors have contributed along with late-life factors to U.S. late-life disability trends mainly through their influence on the onset of, rather than recovery from, limitations.
Keywords: USA, disability, aging, trends, life-course
INTRODUCTION
In the United States the prevalence of activity limitations declined dramatically during the 1980s and 1990s for older adults (see, for example, Cutler, 2001; Freedman, Martin & Schoeni, 2002; Manton, Corder, & Stallard, 1997; Spillman, 2004; Wolf, Hunt & Knickman, 2005), and this trend shows no sign of reversing (Manton, Gu & Lamb, 2006; Schoeni, Martin, Andreski, & Freedman, 2005). The U.S. decline initially appeared to be concentrated among those with difficulty in activities required to live independently (known as instrumental activities of daily living, IADLs, such as shopping, cleaning, and using the telephone). During the 1990s, the prevalence of more severe personal care limitations (known as activities of daily living, ADLs, or tasks such as bathing, dressing, and eating) also began to decline (Freedman, Crimmins, Schoeni, Spillman, Aykan, Kramarow et al., 2004).
To promote further declines in U.S. disability levels and gain a better understanding of variation in trends around the world (LaFortune, Balestat, & the Disability Study Expert Group Members, 2007) requires insight into reasons for the recent declines. Thus far, investigations into the causes of trends have been limited to contemporaneous factors measured later in life (Schoeni, Freedman & Martin, 2008). That is, studies have not distinguished among factors that occur early, intermediate, and late in the life course. Increasing evidence of the link between earlier life events and late-life health (e.g., Blackwell, Hayward & Crimmins, 2001; Blane, Higgs, Hyde & Wiggins, 2004; Hayward & Gorman, 2004; Kuh & Ben-Shlomo, 2004; Lawlor, Batty, Morton, Clark, Macintyre, & Leon, 2005; Luo & Waite, 2005) and between occupational risks and late-life disability (e.g., Crimmins & Hayward 2004; Hayward, Grady, Hardy & Sommers,1989; Reville & Schoeni, 2003/2004) suggest that such factors may be particularly ripe for investigation in understanding trends.
Also unclear is whether declines thus far are attributable to shifts in the risks of onset of or recovery from activity limitations. Three U.S. studies point to declines in incidence of limitations during the 1980s and early 1990s (Crimmins, Saito & Reynolds, 1997; Manton, Corder & Stallard, 1993; Wolf, Mendes de Leon & Glass, 2007). The last two suggest that rates of recovery also may have declined. Because of data constraints, early- and mid-life factors have been notably absent from such investigations.
In this paper we use five waves of the Health and Retirement Study (HRS) to explore for the first time the role of early- and mid-life factors in recent U.S. trends in late-life activity limitations. Where we find significant declines and linkages to stages earlier in the life course, we further investigate the extent to which these influences are operating through changes in the risks of onset and recovery.
BACKGROUND
Activity limitations often first appear later in life, but risk factors for such limitations and underlying chronic conditions and impairments may be traced to behaviors and exposures earlier in life. Many demographic predictors of disability onset also reflect influences earlier in the life course. For example, race and ethnicity influence health and socioeconomic outcomes throughout life, and critical educational experiences, which typically are completed by early adulthood, have persisting influences well into late life.
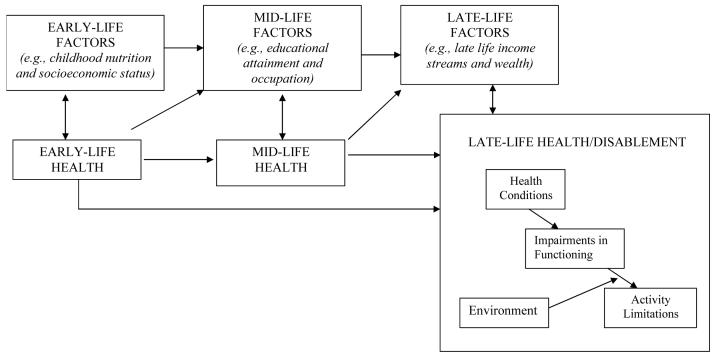
Accordingly, we adopt a life-course perspective as a backdrop to our investigation of trends in late-life activity limitations, as shown in the stylized depiction in Figure 1. On the bottom right, we show the disablement process, in which older individuals with health conditions may develop impairments in functioning, which then, depending on their environments and adoption of accommodations, may lead to limitations in activities (such as ADLs and IADLs). Thus far studies of disability trends have focused on the influence of late-life factors on the disablement process. Here we focus on earlier stages, which we label for convenience sake, “early” and “mid” life. Within each stage there exists the possibility of a bi-directional relationship between risk factors and health. Additional arrows emphasize two distinct pathways through which early- and mid-life factors may influence late-life disablement. The larger solid dark arrows illustrate biological and social “chains of risk” (Kuh & Ben-Shlomo, 2004). For example, it may be that in early life, good nutrition and better childhood socioeconomic status influence education and labor market outcomes in mid-life, which translate into higher income in later life, allowing older adults to purchase services to avoid or accommodate functional decline. The dotted arrow suggests that there also may exist more direct effects of early-life factors on late-life disablement, possibly through biologically “programmed” mechanisms (Power and Hertzman, 1997). Although we do not seek to test these paradigms explicitly, we use them to organize our investigation of how shifting distributions of factors earlier in life influence late-life activity limitation trends.
Figure 1.
Influences of early- and mid-late factors on late-life health/disablement
A number of previously identified late-life factors have been changing over time and have been linked to declines in late-life disability (see Schoeni, Freedman, & Martin, 2008 for a review). Notably, widowhood has declined and socioeconomic status (reflected in income and wealth) has on average increased. Conditions causing activity limitations also have been changing. For example, the percentage of the older population reporting that heart and circulatory, vision, or musculoskeletal conditions cause their activity limitations has declined substantially. Finally, older adults have been increasingly likely to use assistive technology to bridge gaps between functional capacity and the environment.
To date, attention has not explicitly focused on the possible roles of early- and mid-life factors. Therefore, in the following review of prior literature, we highlight these potential influences. We limit consideration to factors that are likely to be associated with late-life disability and whose distribution in the population have been changing over time and thus may possibly influence recent activity limitation trends. For parsimony's sake, we further limit our discussion to indicators available in the HRS.
Race/ethnicity
U.S. Blacks and Hispanics experience greater levels of dependency in late-life than do non-Hispanic whites, and socioeconomic factors do not fully account for such disparities (Carrasquillo, Lantigua, & Shea, 2000; Hayward, Crimmins, Miles & Yang, 2000; Schoeni et al., 2005). In contrast, there appears to be a health and functioning advantage for older Asians, particularly for those born in the United States (Mutchler, Prakash, & Burr, 2007). Over the last few decades, there has been an increase in both the Hispanic and Asian proportions of the older population (U.S. Census Bureau, 2005), suggesting possibly a mixed role for race and ethnicity in late-life disability trends.
Region of birth/foreign born
There is evidence that region of birth within the United States matters for some indicators of health in old age, with Southern births often associated with worse outcomes (Kington, Carlisle, McCaffrey, Myers & Allen, 1998). Morbidity also differs between U.S.-born and foreign-born persons, with the latter often in better health possibly due to selection (Dey & Lucas, 2006). Historical data suggest that the geographic distribution of the population ages 5 and under changed in the United States from 1890 to 1930 (U.S. Census Bureau, 1975), with increasing proportions in the Midwest and West, likely reflecting the substantial internal migration that occurred. In the last third of the twentieth century, there also was a dramatic rise in the foreign-born population (U.S. Census Bureau, 2001).
Childhood socioeconomic status
Childhood living situation has long been a key factor in studies of child health and mortality, but only recently has been found to matter for adult health. For example, two studies have shown that low socioeconomic status in childhood – as measured by father's occupation and/or mother's education – predicts chronic disease in later life (Blackwell et al., 2001; Wannamethee, Whincup, Shaper & Walker, 1996). The childhood socioeconomic status of older cohorts in the United States has changed in part as a consequence of the Great Depression from 1929 to 1933 and subsequent recession of 1937-38. Persons ages 75 and over in 1995 were roughly ages 9 and older in 1929, whereas those ages 75 to 84 in 2004 were infants or very small children in 1929 and spent most of their childhoods in difficult economic times.
Childhood health
Chronic diseases and related disability in late life may be influenced by exposure to infectious agents earlier in life (Elo & Preston, 1992; Zimmer, 2001). Indeed, Blackwell and colleagues (2001) found that childhood infectious disease was associated with health in later life, raising the possibility of linkages with later stages of the disablement process. Others have argued that the decline in inflammatory exposure stemming from infectious disease early in life has been a major factor in the decline in old-age mortality (e.g., Crimmins & Finch, 2006). With the growth of childhood immunization and the decline in rates of scarlet fever, tuberculosis, measles, and rheumatic fever since the 1930s, it is possible that improvements in late-life health in part reflect improvements over the last century in childhood health.
Stature
Short stature in adulthood has been interpreted as a proxy for the cumulative effects of adverse living conditions, including early-life malnutrition, disease, and economic and psycho-social deprivation (Peck & Lundberg, 1995; Silventoinen, 2003). A particular focus has been the relationship between height and chronic disease (Fogel, 1994; Hebert, Ajani, Cook, Lee, Chan & Hennekens, 1997; Silventoinen, Zdravkovic, Skytthe, McCarron, Herskind, Koskenvuo, et al., 2006), although results have been mixed. One of the only studies investigating the role of stature in late-life health trends found that increasing height was an important factor in the declining prevalence of chronic disease over the 20th century (Fogel, 1994), suggesting a possible role in disability decline as well. As nutrition and standards of living have increased in the United States, height has increased. For example, the mean measured height of men ages 60 to 74 increased significantly from 67.0 inches in 1960-62 to 68.6 inches in 1999-2002 (Ogden, Fryar, Carroll & Flegal, 2004).
Education
Education is positively associated with health throughout life and through many pathways, for example, via healthful behaviors, access to health care, and ability to navigate the health-care system (Ross & Wu, 1995). Studies suggest education is particularly important in averting the onset of late-life disability, but less so in predicting recovery (see, for example, Melzer, Izmirlian, Leveille, & Guralnik, 2001, and Zimmer & House, 2003). Substantial increases in the educational attainment of the older U.S. population occurred during the 1980s and 1990s, and this change has been identified as a major contributor to declines in late-life disability prevalence. However, Freedman and Martin (1999) predicted that this education bonus might not continue into the future, and more recent evidence suggests that the benefits of increased educational attainment may have leveled off (Freedman, Schoeni, Martin, and Cornman, 2007).
Occupation
Morbidity is often higher in later life among people who have had lower-status occupations (Marmot, Bosma, Hemingway, Brunner & Stansfeld, 1997; Townsend, Davidson & Whitehead, 1988). Both physical and psychosocial demands have been implicated in this connection (Reville & Schoeni, 2003/2004; Theorell, 2000). Manufacturing occupations, which have notably high injury rates, have contracted in the last few decades whereas service industry jobs, which have much lower injury rates (Bureau of Labor Statistics, 2005), have increased, suggesting a potential role for occupation in recent trends. Costa (2000) attributes declines in chronic conditions among white male U.S. veterans from 1910 to 1990 in part to shifts in occupation, but evidence linking such changes to more recent disability trends is lacking.
War experience and military service
There is a considerable literature on the subsequent higher mortality of people, especially men, who were adolescents in World War II (Elo & Preston, 1992). The nature of the association between military service and subsequent disability is less clear, in part because individuals with various health conditions were screened out of the military. In addition to these selection effects, it could be that the stress of war and its aftermath affect subsequent health; alternatively, participation in the military, especially for disadvantaged groups, may increase socioeconomic status, which may have a positive influence on health (Elder, 1986). The number of U.S. veterans ages 75 and older tripled from 1.4 million in 1990 to 4.1 million in 2000 (Federal Interagency Forum on Aging-Related Statistics, 2004).
METHODS
Data
The HRS is an ongoing study of older adults sponsored by the National Institute of Aging and conducted by the University of Michigan. Initially designed as two separate panel studies, the HRS has evolved into a design that represents the full 50-and-over U.S. population, with new cohorts aged into the sample at six-year intervals. The original 1992 sample was based on a multi-stage, clustered area probability design and consisted of individuals born between 1931 and 1941 and their spouses. The second sample of adults born in 1923 or earlier was first interviewed in 1993 and re-interviewed in 1995 as part of the Asset and Health Dynamics among the Oldest Old (AHEAD) study. The AHEAD cohort was based on the HRS sampling frame plus Medicare enrollment files. In 1998, the two studies were merged, and the sample was expanded to include those born 1924-1930 and 1942-1947. Baseline interviews were conducted in person and follow-up interviews generally administered by telephone at two-year intervals. Overall response rates ranged between 86.8 and 89.1 percent across waves.
To facilitate calculation of cross-sectional estimates, HRS sampling weights adjust for non-response and loss to follow-up. Thus, the merged panels can be used to construct comparable cross-sections of U.S. community-dwelling older adults in the years 1993, 1995, 1998, 2000, 2002, and 2004. In 1993, the health and disability questions were substantially different from those in later years, so we omitted that year. Because of initial gaps in the ages covered by the surveys, we focused our analysis on adults ages 75 and older.
To maintain comparability with earlier waves, we omitted respondents living in institutions in later years (approximately 1,774 cases across all years). We have found in analysis of other data sets that the omission of the institutionalized population does not appreciably alter conclusions about U.S. trends in disability prevalence (Schoeni, Freedman & Wallace, 2001; Schoeni et al., 2005). Estimates of disability onset also are unlikely to be biased because most residents in institutional settings have difficulty with daily activities and are therefore not at risk for onset. It is more difficult to assess the likely bias for estimates of recovery from disability. Spillman & Lubitz (2002) suggest that U.S. nursing home residents experienced increasingly shorter stays from 1984 to 1993, but whether this trend has continued for 1995 to 2004 is unclear. If nursing home residents are more likely over time to recover, then their omission is likely to bias downward estimates of trends in recovery.
The final sample size for analysis of prevalence trends was 23,229 (ranging from 4,501 to 4,701 across waves). For analyses of trends of onset and recovery, we used four intervals: 1995-1998, 1998-2000, 2000-2002, and 2002-2004. Respondents who were lost to follow-up or who died by the end of each interval were retained in these analyses, but coded accordingly, making the sample size for onset and recovery analyses 18,552. Average length of time between survey waves was relatively stable (27, 25, 26, and 22 months for the four intervals) in part because of different starting months during the specified years.
Outcomes
In every wave respondents were asked about difficulty with activities of daily living (ADLs) and instrumental activities of daily living (IADLs). (See Table 1.) A respondent who reported having difficulty doing, does not do, or is unable to do one or more of six ADLs was considered to have an ADL limitation. For IADLs, we coded respondents as having a limitation either if they reported difficulty or if they reported that they did not or could not do one of five activities because of a health problem. Respondents who reported that they did not know if they had difficulty or who refused (less than 1% for any given task) were assumed to have no difficulty.
Table 1.
Activity Limitation Outcomes
| Instrumental Activities of Daily Livinga | Activities of Daily Living | |
|---|---|---|
| Introduction | Here are a few other activities which some people have difficulty with because of a physical, mental, emotional, or memory problem. Please tell me whether you have any difficulty with each activity I name. If you don't do the activity at all, just tell me so. Exclude any difficulties that you |
Here are a few more everyday activities. Please tell me if you have any difficulty with these because of a physical, mental, emotional, or memory problem. Again exclude any difficulties you expect to last less than three months. |
| Tasks | (Because of a health or memory problem do you have) any difficulty…? | Because of a health or memory problem do you have any difficulty…? |
| preparing a hot meal | walking across a room | |
| shopping for groceries | dressing, including putting on shoes and socks | |
| making phone calls | bathing or showering | |
| taking medications | eating, such as cutting up your food | |
| managing your money such as paying your bills and keeping track of track of expensess | getting in or out of bed | |
| using the toilet, including getting up and down | ||
| If can't or don't do an activity: | ||
| Is that because of a health or memory problem? | ||
| Criteria | Difficulty or because of a health or memory problem can't or don't do For medications, difficulty or because of a health or memory problem can't do |
Difficulty, can't do, or don't do |
The survey also includes an item on difficulty using a map, which we exclude because it it is not considered a traditional IADL.
We considered various parameterizations of these indicators but ultimately chose to model a hierarchical variable (based upon its distribution, ease of interpretation, and consistency with prior literature) reflecting no limitation, IADL limitation only, and any ADL limitation in each wave. We also created variables reflecting onset and recovery, initially with categories of no limitation, IADL only, any ADL, dead, or lost to follow-up, but later combining the outcomes of no limitation and IADL-only limitation to more fully explore the dynamics of the onset of and recovery from ADL limitations.
Key predictors
Predictors were drawn primarily from the RAND HRS files-version G (St. Claire, Blake, Bugliari, Chien, Hayden, Hurd et al., 2007). The exceptions--age, proxy, height, weight, childhood health, childhood socioeconomic status, and region--were constructed from the final public use files and the 2004 tracker file available from the HRS web site. “Don't know” responses and refusals were recoded to modal values for each variable by year. Demographic factors included in all models were age (75-79, 80-84, 85+), sex, and an indicator that the interview was provided by a proxy respondent (vs. self-report). In addition, we included the following early-, mid-, and late-life factors.
Early-life factors
Measures available to reflect early life were: race/ethnicity (non-Hispanic other, non-Hispanic black, and Hispanic vs. non-Hispanic white); region of birth (Midwest, South, West, and in a U.S. territory/outside the United States vs. Northeast); mother's education (< 8 years and missing vs. 8+ years); childhood socioeconomic status (SES); childhood self-rated health (SRH); and low peak stature. The last three indicators deserve further comment.
Beginning in 1998, respondents were asked to recall their childhood SES and health (SRH). (In subsequent waves this information was collected the first time an individual was interviewed.) Accordingly, information about childhood SES and SRH is missing for 316 respondents in 1995 who did not survive or were lost to follow-up by 1998. We imputed missing values from multinomial logistic regression models for a sample of respondents who were interviewed in 1998 but who died or were lost to follow-up by 2000. In addition, for the small percentage of the sample missing SES/SRH at later interviews (1.2% in 2002 and 3.4% in 2004), we imputed values from model estimates for persons who were not missing SES/SRH in those years. In analyses we contrasted those reporting that their families were well off/about average versus those reporting poor/varied status during childhood. We also included four childhood SRH categories: excellent, very good, good, and fair/poor.
Low peak stature was calculated based on self-reported height, generally collected at the first interview. We made two adjustments. First, because over-reporting of height has been noted in previous studies of both measured and self-reported values, we used data on the relation between the two for different age and sex groups from Kuczmarski and colleagues (2001) to adjust self-reported height for misreporting. Second, because older adults lose height with age, we inflated these estimates of current height to derive an estimate of peak height. These latter adjustments were based on Niewenweg and colleagues' analyses (2003) that take into account sex and the age at which height was reported. Finally, based on visual inspections of continuous peak height distributions and exploratory analyses of the relationship between peak height and disability, we created a dichotomous indicator of whether respondents' peak height was two or more standard deviations below average height for their sex.
Mid-life factors
Three indicators of mid life were examined: education (8 or fewer years, 9-11 years, and high school or general equivalency diploma vs. more than high school); whether the respondent was a veteran; and lifetime occupation. Lifetime occupation was defined as occupation of longest held job and was coded based on a response to a direct question or a detailed employment history. Information on lifetime occupation was not available for those respondents who did not hold a position for more than five consecutive years. For the sake of comparability and statistical power, we collapsed the different HRS and AHEAD lifetime occupation categories into the following five: blue-collar (operators, craftsmen, farmers); pink-collar (clerical and service industry workers); white-collar (professionals, managers, salesmen); those with lifetime occupation not coded; and those who never worked. Finally, for consistency over time, for 188 cases who were in the AHEAD cohort, who were missing occupation, and who died or were lost to follow-up between 1995 and 1998 and did not provide the detailed job history requested in 1998, we imputed occupation based on predictions from multinomial logistic regression models for a sample of respondents who were interviewed in 1998 but who died or were lost to follow-up by 2000.
Late-life factors
Current marital status contrasted three groups: divorced/separated/widowed and never married vs. currently married/has a partner. We considered four regions of residence (Midwest, West, Northeast, vs. South), respondent's (combined with spouse's, if married) income in 2004 dollars (in 6 categories of $10,000 increments up to $50,000+) and assets in 2004 dollars (in 5 categories with more detail at the lower end where we found a stronger gradient with limitations). Current and former smokers were contrasted with those who never smoked. For chronic conditions we relied on respondents' reports about whether a doctor had ever told them that they had high blood pressure, diabetes, cancer, lung disease, heart disease, a stroke, psychiatric disorder, or arthritis. We included a measure of whether the respondent was obese (body mass index at least 30), based on measures of height and weight that were adjusted to take into account misreporting by age and sex (Kuczmarksi et al. 2001). Because height is reported only at first interview, we further adjusted it to account for age-related loss, as previously described. Two sensory measures were included: self-rated vision (fair/poor/legally blind; good; vs. excellent/very good) and hearing (fair/poor; good; vs. excellent/very good).
Statistical Approach
We first examined changes from 1995 to 2004 in the hierarchical indicator (no limitation, IADL only, any ADL) and tested for changes using a multinomial logit specification with year as a linear continuous variable (henceforth, the trend variable). We then examined the prevalence of difficulty with individual ADL and IADL activities, and tested for change using logistic regression with a continuous trend variable. We calculated average annual percent declines in these descriptive analyses by dividing the slope of the line fit through the prevalence estimates (over the period of interest) by the 1995 values. We conducted tests by specifying the trend with categorical variables (e.g., 1998 vs. 1995, 2000 vs. 1995) and found that substantive conclusions were substantially similar (not shown).
Because we found significant changes overall in the prevalence of ADL but not IADL-only limitations, we went on to explore trends in onset of and recovery from ADL limitations. We tested for changes over time in the risks of onset and recovery from ADL limitations using multinomial logit models with a continuous trend variable. Other outcomes in these models were death and loss to follow-up. We also investigated categorical specifications of the trend (e.g., 1998-2000 vs. 1995-1998, 2000-2002 vs. 1995-1998) and found substantive conclusions were robust (not shown).
Finally, we used multinomial logistic regression to model the prevalence of limitations (ADL, IADL only, and none) as a function of early-, mid-, and late-life factors. Base models included year as a continuous trend, age, sex, and an indicator of proxy response. We entered early-, mid-, and late-life factors sequentially both as a block of variables and individually. Our primary interest in these nested models was in the strength, significance, and general direction of the influence of the trend variable. That is, as potential confounders were entered sequentially, we tracked to what extent the trend was attenuated (or enhanced). To facilitate interpretation, we transformed the odds ratios (OR) for the trend variable reported in the tables into average annual percent changes (100*(OR-1)). We also noted changes in the strength and significance of early-and mid-life predictors after controlling for late-life factors. We replicated this approach using ADL onset and recovery outcomes to understand how trends changed as early-, mid-, and late-life factors were taken into account.
HRS has a complex sample design that requires sampling weights to account for stratification, as well as adjustments to standard errors for geographic clustering. Moreover, most respondents appear in more than one wave, and thus observations are not independent. In all analyses, we accounted for the complex design of the survey, including geographic clustering and correlations within primary sampling units (PSU) due to repeat observations, by using STATA's svy commands with sampling weights, strata, and PSU indicators provided in the tracker file (StataCorp, 2005).
FINDINGS
Trends in Prevalence, Onset, and Recovery
The prevalence of reporting any activity limitation declined from 39.3% in 1995 to 36.1% in 2004 (p<.05), implying an annual rate of decline of 0.88% (upper panel Table 2). The prevalence of ADL limitations declined from 30.2% to 26.0% (p<.01), yielding a −1.46 % annual change. In contrast, the prevalence of reporting difficulty with any IADLs and with only IADLs (but not ADLs) did not change significantly. Among specific ADL activities, there were significant declines in difficulty with bathing, dressing, transferring, and toileting. Among IADLs, only difficulty with shopping for groceries decreased significantly.
Table 2.
Trends in ADL and IADL Limitations, 75+ Population, 1995-2004
| Survey Year | ||||||
|---|---|---|---|---|---|---|
| Prevalence | 1995 | 1998 | 2000 | 2002 | 2004 | Annual Percent Change |
| Any ADL or IADL | 39.3 | 37.4 | 35.4 | 36.5 | 36.1 | −0.88% * |
| Any ADL | 30.2 | 28.3 | 27.3 | 27.5 | 26.0 | −1.46% ** |
| IADL only | 9.0 | 9.1 | 8.2 | 9.0 | 10.1 | 1.06% |
| Any IADL | 26.9 | 26.9 | 23.8 | 24.7 | 25.6 | −0.86% |
| Specific ADLs | ||||||
| Bathing | 15.3 | 14.8 | 13.4 | 12.6 | 11.8 | −2.86% ** |
| Dressing | 15.4 | 15.2 | 14.1 | 14.1 | 13.4 | −1.59% * |
| Eating | 6.3 | 6.4 | 5.5 | 5.4 | 5.6 | −1.76% |
| Getting in/out chair/bed | 10.1 | 9.2 | 7.9 | 8.2 | 6.6 | −3.85% ** |
| Walking across room | 13.2 | 12.2 | 11.6 | 12.4 | 11.0 | −1.48% |
| Using toilet | 9.8 | 9.8 | 8.3 | 8.7 | 7.7 | −2.57% * |
| Specific IADLs | ||||||
| Shopping for groceries | 19.2 | 18.0 | 16.3 | 16.7 | 16.6 | −1.62% ** |
| Managing money | 12.8 | 11.9 | 11.3 | 11.8 | 11.1 | −1.33% |
| Preparing meals | 12.5 | 12.2 | 11.5 | 12.2 | 11.4 | −0.84% |
| Using phone | 9.3 | 9.6 | 8.1 | 9.1 | 9.0 | −0.61% |
| Taking medication | 6.2 | 5.7 | 5.5 | 5.7 | 5.8 | −0.68% |
| Survey Interval | ||||||
| Onset of and Recovery from ADL Limitation | 1995-1998 | 1998-2000 | 2000-2002 | 2002-2004 | Annual Percent Change |
|
| Among those with no ADL limitation at start of interval |
||||||
| Onset of ADL limitation | 16.8 | 15.7 | 16.6 | 15.0 | −1.25% * | |
| Death | 10.8 | 8.8 | 10.1 | 8.2 | −2.82% ** | |
| Loss to follow-up | 4.8 | 3.8 | 4.4 | 3.5 | −3.22% * | |
| Among those with ADL limitation at start of interval |
||||||
| Recovery from ADL limitation | 16.9 | 19.0 | 19.9 | 21.0 | 3.63% * | |
| Death | 24.8 | 23.3 | 23.0 | 22.8 | −1.18% | |
| Loss to follow-up | 3.1 | 4.0 | 3.4 | 3.7 | 1.85% | |
| N | 4,501 | 4,676 | 4,701 | 4,674 | 4,677 | |
p<.05
p<.01 based on linear trend
Note: Annual percent change calculated by dividing slope of change by 1995 value.
ADL = Activities of Daily Living IADL = Instrumental Activities of Daily Living
The lower panel of Table 2 indicates that among those without ADL limitations at the start of each interval, there was a significant decline in the onset of such limitations, as well as a significant decline in the risk of dying and in being lost to follow-up. Among those with ADL limitations at the start of each interval, the chances of recovery increased significantly. Note that attrition rates were comparable between those with and without ADL limitations (in the 3-4% range) but decreased only for those without limitations. The resulting bias from such differential attrition is likely to overstate declines in prevalence; however, such effects are likely to be small given the low rates.
Trends in Early-, Mid-, and Late-Life Factors
Between 1995 and 2004, the profile of the older population changed in many ways (Table 3). With respect to early-life factors, older adults in 2004 were more diverse racially and ethnically, were less likely to be born in the South, less like to report mothers having fewer than 8 years of school, more likely to report healthier childhoods, and less likely to have reached a low peak stature. However, they reported lower childhood socioeconomic status, perhaps reflecting exposure to the Depression years. With respect to mid-life factors, older adults in 2004 were increasingly likely to have completed high school, to have worked in a white-collar or pink-collar occupation, and to be a veteran. Contemporaneous factors also shifted, with more older adults living in the Midwest and West and having the highest levels of income and wealth, but fewer being currently married. There was less smoking, increases in reports of all chronic conditions, obesity, and hearing problems, and improvements in self-rated vision.
Table 3.
Trends in Early- , Mid-, and Late-life Factors, 75+ population, 1995-2004
| 1995 | 2004 | 1995 | 2004 | ||
|---|---|---|---|---|---|
| DEMOGRAPHIC VARIABLES | LATE LIFE | ||||
| Age | Marital status | ** | |||
| 75 - 79 | 44.0 | 45.1 | Married/has partner | 47.4 | 46.1 |
| 80 - 84 | 31.8 | 32.2 | Divorced/separated/widowed | 49.8 | 51.7 |
| 85 + | 24.2 | 22.6 | Never married | 2.8 | 2.2 |
| Female | 61.9 | 60.1 * | Region | ||
| Proxy | 11.8 | 9.6 ** | Northeast | 20.9 | 18.6 |
| EARLY LIFE | Midwest | 26.6 | 27.5 | ||
| Race | South | 35.0 | 34.2 | ||
| White, non-Hispanic | 87.7 | 86.6 ** | West | 17.5 | 19.6 |
| Black, non-Hispanic | 7.8 | 7.0 | Couple income (in 2004 $) | ** | |
| Other, non-Hispanic | 1.1 | 2.1 | $0-9,999 | 16.5 | 12.7 |
| Hispanic | 3.4 | 4.4 | $10,000-19,999 | 29.3 | 29.9 |
| Region of birth | * | $20,000-29,999 | 18.3 | 19.7 | |
| Northeast | 23.0 | 22.5 | $30,000-39,999 | 12.0 | 13.2 |
| Midwest | 30.9 | 32.7 | $40,000-49,999 | 7.6 | 7.4 |
| South | 30.0 | 28.4 | $50,000+ | 16.3 | 17.0 |
| West | 6.7 | 8.0 | Total wealth (in 2004 $) | ** | |
| U.S. territory/outside U.S. | 9.5 | 8.5 | <$0 - 1,000 | 9.6 | 9.7 |
| Mother's education | ** | $2,000-49,999 | 19.1 | 15.7 | |
| Fewer than 8 years | 41.5 | 29.3 | $50,000-149,999 | 26.3 | 20.0 |
| 8 or more years | 46.8 | 58.5 | $150,000-299,999 | 20.5 | 19.4 |
| Missing | 11.7 | 12.2 | $300,000+ | 24.5 | 35.3 |
| SES as a child | * | Smoking behavior | ** | ||
| Well off/about average | 33.7 | 63.6 | Never smoked | 50.7 | 46.3 |
| Poor/varied | 33.3 | 36.4 | Quit smoking | 42.8 | 48.1 |
| Self-rated health as child | ** | Still smoking | 6.5 | 5.6 | |
| Excellent | 42.6 | 47.2 | Chronic conditions | ||
| Very good | 28.5 | 27.0 | High blood pressure | 52.1 | 63.6 ** |
| Good | 22.1 | 20.0 | Diabetes | 12.8 | 18.6 ** |
| Fair/poor | 6.8 | 5.8 | Cancer | 16.5 | 20.4 ** |
| Low peak stature | 2.2 | 1.5 * | Lung disease | 11.3 | 11.2 |
| MID LIFE | Heart disease | 35.4 | 38.3 * | ||
| Education | ** | Stroke | 10.0 | 11.0 | |
| 8 or fewer years | 24.6 | 15.3 | Psychiatric disorder | 11.3 | 13.5 ** |
| 9-11 years | 17.0 | 14.1 | Arthritis | 55.3 | 70.6 ** |
| High school diploma/GED | 30.6 | 36.4 | Obese | 16.9 | 22.4 ** |
| More than high school | 27.7 | 34.1 | Self-rated vision | ** | |
| Occupation | ** | Excellent/very good | 26.4 | 29.0 | |
| Blue collar | 24.7 | 22.9 | Good | 37.6 | 42.5 |
| Pink collar | 18.7 | 21.1 | Fair/poor/legally blind | 36.0 | 28.5 |
| White collar | 25.9 | 31.0 | Self-rated hearing | * | |
| Never worked | 7.2 | 5.6 | Excellent/very good | 32.7 | 30.1 |
| Not coded | 23.5 | 19.4 | Good | 36.6 | 36.7 |
| Veteran | 19.1 | 28.9 ** | Fair/poor | 30.8 | 33.2 |
p<.05
p<.01 based on chi-square
Early- and Mid-life Influences on Trends
Disability Prevalence
Base multinomial logit models (controlling for only age, sex, and proxy) show a significant decline in difficulty with ADLs, amounting to 1.8% on average per year (OR=.982; p<.05), but no significant trend in IADL limitations only (Table 4). Controlling for early-life factors resulted in a slight attenuation of the ADL trend (OR for year increased from 0.982 to 0.986, but remained significant). Adding mid-life factors reduced the ADL trend to statistical insignificance (OR=0.992; 0.8% annual decline), suggesting that changes in the prevalence of these factors operated to lower disability prevalence over time.
Table 4.
Odds Ratios for Prevalence of Activity Limitations, 75+ Population, 1995-2004
| Difficulty with ADLs and with only IADLs (vs neither) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Base model | Plus early-life factors | Plus mid-life factors | Plus late-life factors | |||||
| ADL |
IADL only |
ADL |
IADL only |
ADL |
IADL only |
ADL |
IADL only |
|
| Year | 0.982 * | 1.008 | 0.986 * | 1.010 | 0.992 | 1.018 | 0.966 ** | 1.012 |
| Demographic Factors | ||||||||
| Age 80 to 84 | 1.542 ** | 1.535 ** | 1.531 ** | 1.540 ** | 1.514 ** | 1.518 ** | 1.465 ** | 1.422 ** |
| Age 85+ | 3.102 ** | 2.679 ** | 3.111 ** | 2.700 ** | 2.995 ** | 2.579 ** | 2.892 ** | 2.278 ** |
| Female | 1.575 ** | 1.035 | 1.556 ** | 1.024 | 1.454 ** | 0.916 | 1.326 ** | 0.969 |
| Proxy | 4.951 ** | 5.195 ** | 4.666 ** | 4.911 ** | 4.355 ** | 4.472 ** | 4.178 ** | 3.895 ** |
| Early-life Factors | ||||||||
| Black, non-Hispanic | 1.254 * | 1.176 | 1.165 | 1.014 | 0.972 | 0.914 | ||
| Other, non-Hispanic | 1.030 | 1.086 | 0.988 | 1.027 | 0.864 | 0.930 | ||
| Hispanic | 1.109 | 1.089 | 0.901 | 0.819 | 0.772 ** | 0.731 | ||
| Born in Midwest | 1.099 | 1.089 | 1.074 | 1.049 | 1.102 | 1.201 | ||
| Born in South | 1.335 ** | 1.230 * | 1.254 ** | 1.132 | 1.191 | 1.310 * | ||
| Born in West | 1.106 | 1.053 | 1.132 | 1.086 | 1.216 | 1.144 | ||
| Born in U.S. territory/outside U.S. | 0.890 | 1.090 | 0.843 | 1.016 | 0.898 | 1.094 | ||
| Mother's education fewer than 8 years | 1.214 ** | 1.079 | 1.107 * | 0.948 | 1.055 | 0.907 | ||
| Mother's education missing | 1.157 | 1.277 * | 1.030 | 1.086 | 1.040 | 1.070 | ||
| SES as a child poor/varied | 1.185 ** | 1.151 * | 1.148 ** | 1.105 | 1.027 | 1.025 | ||
| Very good self-rated health as a child | 1.104 * | 1.158 * | 1.078 | 1.125 | 0.982 | 1.034 | ||
| Good self-rated health as a child | 1.420 ** | 1.369 ** | 1.359 ** | 1.291 ** | 1.204 * | 1.127 | ||
| Fair/poor self-rated health as a child | 1.799 ** | 1.610 ** | 1.707 ** | 1.502 ** | 1.340 * | 1.176 | ||
| Low peak stature | 1.549 * | 1.200 | 1.486 | 1.142 | 1.397 | 1.190 | ||
| Mid-life Factors | ||||||||
| 8 or fewer years education | 1.641 ** | 1.884 ** | 1.074 | 1.349 * | ||||
| 9-11 years education | 1.201 * | 1.216 * | 0.827 | 0.891 | ||||
| High school diploma/GED | 1.073 | 1.043 | 0.907 | 0.896 | ||||
| Blue-collar lifetime occupation | 1.045 | 1.206 | 0.960 | 1.104 | ||||
| Pink-collar lifetime occupation | 1.011 | 1.351 ** | 0.927 | 1.232 * | ||||
| Never worked | 1.153 | 1.277 | 1.003 | 1.134 | ||||
| Lifetime occupation not coded | 1.360 ** | 1.620 ** | 1.187 * | 1.454 ** | ||||
| Veteran | 0.999 | 0.997 | 1.006 | 0.994 | ||||
| Late-life Factors | ||||||||
| Divorced/separated/widowed | 1.037 | 0.908 | ||||||
| Never married | 1.006 | 0.821 | ||||||
| Lives in the Midwest | 1.180 * | 1.234 * | ||||||
| Lives in the Northeast | 1.105 | 1.422 ** | ||||||
| Lives in the West | 1.108 | 1.311 ** | ||||||
| $0-$9,999 couple income (in 2004 $) | 1.394 ** | 1.701 ** | ||||||
| $10,000-19,999 | 1.213 * | 1.536 ** | ||||||
| $20,000-29,999 | 1.126 | 1.332 * | ||||||
| $30,000-39,999 | 0.972 | 1.269 * | ||||||
| $40,000-49,999 | 0.907 | 1.133 | ||||||
| <$0-1,000 total wealth (in 2004 $) | 1.847 ** | 1.473 ** | ||||||
| $2,000-49,999 | 1.330 ** | 1.254 * | ||||||
| $50,000-149,999 | 1.123 | 1.153 | ||||||
| $150,000-299,999 | 1.115 | 1.059 | ||||||
| Still smoking | 1.235 * | 1.086 | ||||||
| Quit smoking | 1.039 | 1.130 * | ||||||
| High blood pressure | 1.145 ** | 1.042 | ||||||
| Diabetes | 1.328 ** | 1.219 * | ||||||
| Cancer | 1.174 ** | 0.998 | ||||||
| Lung disease | 1.652 ** | 1.334 ** | ||||||
| Heart disease | 1.364 ** | 1.206 * | ||||||
| Stroke | 2.828 ** | 1.856 ** | ||||||
| Psychiatric disorder | 2.126 ** | 2.181 ** | ||||||
| Arthritis | 2.379 ** | 1.162 * | ||||||
| Obese | 1.562 ** | 0.952 | ||||||
| Good vision | 1.122 * | 1.130 | ||||||
| Fair/poor vision | 2.351 ** | 2.215 ** | ||||||
| Good hearing | 1.079 | 1.145 | ||||||
| Fair/poor hearing | 1.435 ** | 1.766 ** | ||||||
p<.05
p<.01
Note: Odds ratios are from weighted multninomial logistic regression models adjusted for complex survey design using STATA's svy procedure. Omitted categories are: White, non-hispanic; born in Northwest; mother's education 8 or more years; excellent self-rated health as a child; more than 12 years education; white collar lifetime occupation; married; lives in the South; $50,000+ couple income; $300,000+ total wealth; never smoked; excellent/very good vision; excellent/very good hearing.
We found that when we added each early- and mid-life factor individually to the base model (not shown), shifts in education attenuated by about 40% and eliminated the significance of the trend in ADL limitations. None of the other early- and mid-life variables had such an effect, although inclusion of mother's education, lifetime occupation, and self-rated childhood health status each resulted in attenuations of the trend estimate of at least 10%. Adding these four indicators altogether to a base model resulted in an insignificant odds ratio for year of 0.992 (0.8% annual decline), a change comparable to including all the early- and mid-life factors, as shown in Table 4.
Adding late-life factors to the model with all the early- and mid-life factors resulted in the re-emergence of a significant trend downward in ADL disability (OR=0.966; 3.4% average annual decline), suggesting that had these late-life factors as a group not changed, the prevalence of ADL limitation would have declined at an even faster rate. When we entered late-life factors individually to a base model, we found that the increases in chronic conditions were especially detrimental. Nevertheless, some changes in other factors were beneficial. For example, the addition of vision and wealth indicators attenuated the trend by roughly 50% and 35%, respectively, and in both cases it lost significance. Adding vision and wealth to a base model with education, mother's education, lifetime occupation, and self-rated childhood health status resulted in an odds ratio for the trend of 0.9998, essentially completely accounting for the trend.
Late-life factors were clearly related to early- and mid-life factors, some of which lost statistical significance for predicting ADL limitations once late-life measures were introduced (see, for example, mother's education). However, the disadvantageous effects of good or fair/poor childhood health and not having a lifetime occupation coded persisted in the full model for ADLs, and being Hispanic re-emerged as significant. For IADL limitations only, the negative influences of having fewer than 8 years of education and having a pink-collar or no lifetime occupation coded remained significant in the full model, and being Southern born re-emerged as a predictor.
Onset of and Recovery from ADL Disability
The base model in Table 5 shows a significant decline in the onset of ADL disability over the period (OR=0.977; 2.3% average annual decline). Also significant were declines in death and loss-to-follow up over the period. Once shifts in early-life factors were considered, the implied decline in ADL onset became smaller and non-significant. Adding mid-life factors further attenuated the trend in onset. When we added early- and mid-life factors individually, two factors attenuated by at least 10% the onset trend and eliminated its significance: respondent's education and mother's education. In Table 5, once late-life factors were taken into account, the decline in ADL onset became significant again and was enhanced in size. When we added factors individually, vision and wealth both contributed to the decline in the onset of ADL limitations, whereas increases in chronic conditions were detrimental.
Table 5.
Odds Ratios for Trends in the Onset of and Recovery from ADL Limitations, 75+ population, 1995-2004
| Base model | Plus early-life factors | Plus early- and mid-life factors | Plus early-, mid-, and late-life | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ADL | Death | Lost | ADL | Death | Lost | ADL | Death | Lost | ADL | Death | Lost | |
| Trend in Onset Among those with No ADL Limitation |
0.977 * | 0.958 ** | 0.955 * | 0.980 | 0.957 ** | 0.961 | 0.984 | 0.956 ** | 0.965 | 0.964 ** | 0.951 ** | 0.966 |
| Trend in Recovery Among those with ADL Limitation |
1.041 * | 0.995 | 1.025 | 1.037 * | 0.996 | 1.030 | 1.037 * | 0.996 | 1.032 | 1.042 * | 1.009 | 1.039 |
p<.05
p<.01
Note: Odds ratios are from weighted multninomial logistic regression models adjusted for complex survey design using STATA's svy procedure. Models control for early-, mid-, and late-life factors shown in Table 4.
There also was a significant increase in recovery from ADL disability over the period, but no significant trends in death or loss-to-follow-up among those with an ADL limitation. This increase in recovery remained large and significant even after controlling for early-, mid-, and late-life factors as blocks (shown in Table 5) and individually. When entered singly, none of the early- or mid-life factors resulted in an insignificant recovery trend, nor did any substantially attenuate it. Only inclusion of vision eliminated the significance of the ADL recovery trend, and vision and wealth each attenuated it by at least 10%.
DISCUSSION
This study is the first investigation of the role of early- and mid-life factors in recent late-life disability trends in the United States. We found that from 1995 to 2004 the prevalence of difficulty with ADLs among older U.S. adults declined, whereas IADL limitations did not. Early- and mid-life factors have contributed along with late-life factors to the downward ADL trend. Specifically, changes in the composition of the older population with respect to education, the education level of their mothers, their health during childhood, and lifetime occupation were linked to declines in the prevalence of ADL limitations. Improvements in late-life vision and increases in wealth also contributed substantially to declines, but greater reports of chronic conditions in late-life offset these gains.
We also found that onset of ADL limitations was reduced and that, consistent with Crimmins and colleagues (1997), recovery increased. The downward trend in onset was linked to increases in education among respondents and their mothers and in late life better vision and greater wealth. In contrast, increased recovery was related only to vision and wealth, but not to early- or mid-life factors.
Our finding that limitations in ADLs (but not IADLs) have declined stands in contrast to U.S. studies based on 1980s and 1990s data, which suggested that declines were larger for IADLs than for ADLs (Freedman et al. 2004; Manton et al., 2006; Schoeni et al. 2001). These differences may reflect a new era in trends or differences in question wording across surveys. The HRS does not ask about two prevalent IADLs, namely, going out/getting outside or doing laundry. Further, the HRS asks about difficulty because of a health problem, whereas other surveys ask about the need for help or inability to perform an activity. Additional research is needed to compare these findings with estimates from other surveys of the same period.
Our study has several limitations. The single decade of observation that we analyzed may not be long enough to identify some of the effects of early- and mid-life factors. Also, some of the measures we used were less than ideal. For example, lifetime occupation could not be ascertained for a significant portion of the sample, mostly women who did not work at least five consecutive years at a given job. Moreover, we did not have measures of mid-life health, and our childhood health indicators were limited to a retrospectively reported general self-assessment and a measure of low peak stature.
Despite these limitations, our study has added knowledge to the growing literature on reasons for the disability decline. Like prior studies, we found an important role for shifts in the educational distribution of the older population (Freedman & Martin, 1999; Waidmann & Liu, 2000) and for late-life vision improvements (Freedman et al., 2007). The latter we found related not only to declines in the prevalence of ADL limitations but also to reductions in onset and increases in recovery. Moreover, for the cohorts we examined late-life wealth was a significant factor in trends. We also identified an important, albeit more modest, role for changes in the education levels of the mothers of today's elderly, health in childhood, and lifetime occupation.
Because our focus was on trends we did not investigate structural models to pinpoint the pathways through which these early- and mid-life factors influence late-life disability. Palloni (2006), for example, found important effects of childhood health on adult socioeconomic achievement, which in turn may influence later-life health and functioning. Our finding that in some cases early- and mid-life influences dissipate once late-life factors are considered, are consistent with this study and with the indirect pathway found by Hayward and Gorman (2004) for mortality. We also found, like Cutler and colleagues (2007), that early socioeconomic status does not have a major persistent influence on late-life health outcomes. However, we did find that childhood self-rated health status remained a statistically significant predictor of late-life ADL limitations even after late-life factors were introduced. The latter suggests there may be a more direct, perhaps biologic, pathway at work.
The fact that we were unable to account for the increases in recovery except through improvements in vision and wealth suggests that factors other than those considered here may be important. The dramatic increase in cataract surgery may well be behind the changes in vision that we report, and medical interventions that reduce the severity of chronic conditions and assistive technologies that enhance functioning may also be implicated (Schoeni et al., 2008). Changes in biologic resiliency and in the use of rehabilitative services also merit further study.
Finally, our analysis permits limited speculation about early- and mid-life factors and the future of late-life disability limitations. Future cohorts of U.S. elderly will likely be even better educated than the elderly of today, as will be their parents; however, rates of change in education among the elderly are diminishing (Freedman & Martin, 1999). Given increases during the last half century in labor force participation rates of U.S. women (Fullerton, 1999), in the future a greater share of women entering old age will have had substantial attachment to the work force. Furthermore, relative to today's elderly, future elderly will be less likely to have spent their working lives in physically demanding occupations. Their jobs may be more cognitively challenging but more sedentary, thus providing both advantages and disadvantages for health in old age. To gain further insight into future trends in disability, it may be fruitful to examine the evidence on trends in childhood health across a wider set of birth cohorts in the United States, including those soon to be entering old age, and to examine trends in earlier life experiences and late-life disability in other countries around the world.
Acknowledgments
This research w as funded by a grant from the U.S. National Institute on Aging (R01-AG021516). The view s expressed are those of the authors alone and do not reflect the view s of the authors' employers or the funding agency.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Vicki A. Freedman, University of Medicine and Dentistry of New Jersey-School of Public Health New Brunswick, NJ UNITED STATES
Linda G Martin, RAND Corporation
Robert F Schoeni, University of Michigan
Jennifer C Cornman, University of Medicine and Dentistry of New Jersey-School of Public Health
REFERENCES
- Blane D, Higgs P, Hyde M, Wiggins RD. Life course influences on quality of life in early old age. Social Science and Medicine. 2004;58(11):2171–2179. doi: 10.1016/j.socscimed.2003.08.028. [DOI] [PubMed] [Google Scholar]
- Blackwell DL, Hayward MD, Crimmins EM. Does childhood health affect chronic morbidity in later life? Social Science and Medicine. 2001;52(8):1269–1284. doi: 10.1016/s0277-9536(00)00230-6. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics Workplace Injuries and Illnesses, 2005. 2005 October 19. 2006. http://www.bls.gov/iif/oshwc/osh/os/osnr0025.pdf.
- Carrasquillo O, Lantigua RA, Shea S. Differences in functional status of Hispanic versus non-Hispanic White elders: data from the Medical Expenditure Panel Survey. Journal of Aging and Health. 2000;12(3):342–361. doi: 10.1177/089826430001200304. [DOI] [PubMed] [Google Scholar]
- Costa D. Understanding the twentieth century decline in chronic conditions among older men. Demography. 2000;37(1):53–72. [PubMed] [Google Scholar]
- Crimmins EM, Hayward MD. Workplace characteristics and work disability onset for men and women. Soz Praventivmed. 2004;49(2):122–131. doi: 10.1007/s00038-004-3105-z. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Finch CE. Infection, inflammation, height, and longevity. Proceedings of the National Academy of Sciences. 2006;103(2):498–503. doi: 10.1073/pnas.0501470103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y, Reynolds SL. Further evidence on recent trends in the prevalence and incidence of disability among older Americans from two sources: the LSOA and the NHIS. Journals of Gerontology B: Social Sciences. 1997;52(2):S59–S71. doi: 10.1093/geronb/52b.2.s59. [DOI] [PubMed] [Google Scholar]
- Cutler DM. Declining disability among the elderly. Health Affairs. 2001;20(6):11–27. doi: 10.1377/hlthaff.20.6.11. [DOI] [PubMed] [Google Scholar]
- Cutler DM, Miller G, Norton DM. Evidence on early-life income and late-life health form America's dust bowl era. Proceedings of the National Academy of Sciences. 2007;104(33):13244–13249. doi: 10.1073/pnas.0700035104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dey AN, Lucas JW. Advance data from vital and health statistics. 369. National Center for Health Statistics; Hyattsville, MD: 2006. Physical and mental health characteristics of U.S.-and foreign-born adults: United States, 1998–2003. [PubMed] [Google Scholar]
- Elder GH., Jr. Military times and turning points in men's lives. Developmental Psychology. 1986;22(2):233–245. [Google Scholar]
- Elo IT, Preston SH. Effects of early-life conditions on adult mortality: A review. Population Index. 1992;58(2):186–212. [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics . Older Americans 2004: Key indicators of well-being. U.S. Government Printing Office; Washington, DC: 2004. [Google Scholar]
- Fogel RW. Economic growth, population theory, and physiology: The bearing of long-term processes on the making of economic policy. American Economic Review. 1994;84(3):369–395. [Google Scholar]
- Freedman VA, Crimmins E, Schoeni RF, Spillman B, Aykan H, Kramarow E, Land K, Lubitz J, Manton K, Martin L, Shinberg D, Waidmann T. Resolving inconsistencies in trends in old-age disability: Report from a technical working group. Demography. 2004;41(3):417–441. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Martin LG. The role of education in explaining and forecasting trends in functional limitations among older Americans. Demography. 1999;36(4):461–473. [PubMed] [Google Scholar]
- Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: A systematic review. Journal of the American Medical Association. 2002;288(24):3137–3146. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Schoeni RF, Martin LG, Cornman JC. Chronic conditions and the decline in late-life disability. Demography. 2007;44(3):459–477. doi: 10.1353/dem.2007.0026. [DOI] [PubMed] [Google Scholar]
- Fullerton HN. Labor force participation: 75 years of change, 1950–98 and 1998–2025. Monthly Labor Review. 1999;122(12):3–12. [Google Scholar]
- Hayward MD, Grady WR, Hardy MA, Sommers D. Occupational influences on retirement, disability, and death. Demography. 1989;26(3):393–409. [PubMed] [Google Scholar]
- Hayward MD, Gorman BK. The long arm of childhood: The influence of early-life social conditions on men's mortality. Demography. 2004;41(1):87–107. doi: 10.1353/dem.2004.0005. [DOI] [PubMed] [Google Scholar]
- Hayward MD, Crimmins EM, Miles TP, Yang Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. American Sociological Review. 2000;65(6):910–930. [Google Scholar]
- Health and Retirement Study . 1993-2004 public use datasets. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740); Ann Arbor, MI: 2006. [Google Scholar]
- Hebert PR, Ajani U, Cook NR, Lee IM, Chan KS, Hennekens CH. Adult height and incidence of cancer in male physicians. Cancer Causes Control. 1997;8(4):591–597. doi: 10.1023/a:1018442329319. [DOI] [PubMed] [Google Scholar]
- Kington R, Carlisle D, McCaffrey D, Myers H, Allen W. Racial differences in functional status among elderly U.S. migrants from the South. Social Science and Medicine. 1998;47(6):831–840. doi: 10.1016/s0277-9536(98)00145-2. [DOI] [PubMed] [Google Scholar]
- Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: Findings from the third Nutritional Health and Nutrition Examination Survey, 1988-1994. Journal of the American Dietetic Association. 2001;101(1):28–33. doi: 10.1016/S0002-8223(01)00008-6. [DOI] [PubMed] [Google Scholar]
- Kuh D, Ben-Shlomo Y, editors. A life course approach to chronic disease epidemiology. Oxford University Press; Oxford: 2004. [PubMed] [Google Scholar]
- Lafortune G, Balestat G, the Disability Study Expert Group Members Trends in Severe Disability Among Elderly People: Assessing the Evidence in 12 OECD Countries and the Future Implications. Health Working Paper. 2007;26 [Google Scholar]
- Lawlor DA, Batty GD, Morton SM, Clark H, Macintyre S, Leon DA. Childhood socioeconomic position, educational attainment, and adult cardiovascular risk factors: the Aberdeen children of the 1950s cohort study. American Journal of Public Health. 2005;95(7):1245–1251. doi: 10.2105/AJPH.2004.041129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y, Waite LJ. The impact of childhood and adult SES on physical, mental, and cognitive well-being on later life. Journal of Gerontology B: Social Sciences. 2005;60(2):S93–101. doi: 10.1093/geronb/60.2.s93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton KG, Corder LS, Stallard E. Estimates of change in chronic disability and institutional incidence and prevalence rates in the U.S. elderly population from the 1982, 1984, and 1989 National Long Term Care Survey. Journals of Gerontology. 1993;48(4):S153–S166. doi: 10.1093/geronj/48.4.s153. [DOI] [PubMed] [Google Scholar]
- Manton KG, Corder LS, Stallard E. Chronic disability trends in elderly United States populations: 1982-1994. Proceedings of the National Academy of Sciences. 1997;94(6):2593–2598. doi: 10.1073/pnas.94.6.2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton KG, Gu X, Lamb V. Change in chronic disability from 1982 to 2004-2005 as measured by long-term changes in function and health in the U.S. elderly population. Proceedings of the National Academy of Sciences. 2006;103(48):18374–18379. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M, Bosma H, Hemingway H, Brunner EJ, Stansfeld SA. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet. 1997;350(9073):235–239. doi: 10.1016/s0140-6736(97)04244-x. [DOI] [PubMed] [Google Scholar]
- Melzer D, Izmirlian G, Leveille SG, Guralnik JM. Educational differences in the prevalence of mobility disability in old age: the dynamics of incidence, mortality, and recovery. Journals of Gerontology B: Social Sciences. 2001;56(5):S294–301. doi: 10.1093/geronb/56.5.s294. [DOI] [PubMed] [Google Scholar]
- Mutchler JE, Prakash A, Burr JA. The demography of disability and the effects of immigrant history: older Asians in the United States. Demography. 2007;44(2):251–263. doi: 10.1353/dem.2007.0015. [DOI] [PubMed] [Google Scholar]
- Niewenweg R, Smit ML, Walenkamp MJE, Wit JM. Adult height corrected for shrinking and secular trend. Annals of Human Biology. 2003;30(5):563–569. doi: 10.1080/0301446032000112661. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Fryar CD, Carroll MD, Flegal KM. Mean body weight, height, and body mass index, United States 1960-2002. Advance Data from Vital and Health Statistics. 2004;347:1–18. [PubMed] [Google Scholar]
- Palloni A. Reproducing inequalities: luck, wallets, and the enduring effects of childhood health. Demography. 2006;43(4):587–615. doi: 10.1353/dem.2006.0036. [DOI] [PubMed] [Google Scholar]
- Peck MN, Lundberg O. Short stature as an effect of economic and social conditions in childhood. Social Science and Medicine. 1995;41(5):733–738. doi: 10.1016/0277-9536(94)00379-8. [DOI] [PubMed] [Google Scholar]
- Power C, Hertzman C. Social and biological pathways linking early life and adult disease. Royal Society of Medicine Press Limited/British Medical Bulletin. In: Marmot M, Wadsworth MEJ, editors. Fetal and early childhood environment: Long-term health implications. Vol. 53. London: 1997. pp. 210–222. [DOI] [PubMed] [Google Scholar]
- Reville R, Schoeni R. The fraction of disability caused at work. Social Security Bulletin. 20032004;65(4):31–37. [PubMed] [Google Scholar]
- Ross CE, Wu CL. The links between education and health. American Sociological Review. 1995;60(5):719–745. [Google Scholar]
- Schoeni R, Freedman VA, Wallace R. Persistent, consistent, widespread, and robust? Another look at recent trends in old-age disability. Journal of Gerontology B: Social Sciences. 2001;56(4):S206–S218. doi: 10.1093/geronb/56.4.s206. [DOI] [PubMed] [Google Scholar]
- Schoeni R, Martin L, Andreski P, Freedman VA. Persistent and growing socioeconomic disparities in disability among the elderly: 1982-2002. American Journal of Public Health. 2005;95(11):2065–2070. doi: 10.2105/AJPH.2004.048744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoeni RF, Freedman VA, Martin LG. Why is late-life disability declining? Under Review. Milbank Quarterly. 2008;86(1):47–89. doi: 10.1111/j.1468-0009.2007.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silventoinen K. Determinants of variation in adult body height. Journal of Biosocial Science. 2003;35(2):263–85. doi: 10.1017/s0021932003002633. [DOI] [PubMed] [Google Scholar]
- Silventoinen K, Zdravkovic S, Skytthe A, McCarron P, Herskind AM, Koskenvuo M, de Faire U, Pedersen N, Christensen K, Kaprio J. Association between height and coronary heart disease mortality: A prospective study of 35,000 twin pairs. American Journal of Epidemiology. 2006;163(7):615–621. doi: 10.1093/aje/kwj081. for the GenomEUtwin Project. [DOI] [PubMed] [Google Scholar]
- Spillman BC. Changes in elderly disability rates and the implications for health care utilization and cost. Milbank Quarterly. 2004;82(1):157–94. doi: 10.1111/j.0887-378X.2004.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillman BC, Lubitz J. New estimates of lifetime nursing home use: have patterns of use changed? Medical Care. 2002;40(10):965–75. doi: 10.1097/00005650-200210000-00013. [DOI] [PubMed] [Google Scholar]
- StataCorp. STATA Survey Data Reference Manual, Release 9. Stata Press; College Station, Texas: 2005. [Google Scholar]
- Clair P, Blake D, Bugliari D, Chien S, Hayden O, Hurd M, Ilchuk S, Kung F-Y, Miu A, Panis C, Pantoja P, Rastegar A, Rohwedder S, Roth E, Wedell J, Zissimopoulos J. RAND HRS data documentation-Version G. RAND Corporation; Santa Monica: 2007. [Google Scholar]
- Theorell T. Working conditions and health. In: Berkman L, Kawachi I I, editors. Social epidemiology. Oxford University Press; New York: 2000. pp. 95–117. [Google Scholar]
- Townsend P, Davidson N, Whitehead M. Inequalities in health. Penguin; London: 1988. [Google Scholar]
- U.S. Census Bureau . Historical statistics of the United States, colonial times to 1970, bicentennial edition. Part 2. Government Printing Office; Washington, D.C: 1975. [Google Scholar]
- U.S. Census Bureau . Profile of the foreign-born population in the United States: 2000. U.S. Government Printing Office; Washington DC: 2001. [Google Scholar]
- U.S. Census Bureau . 65+ in the U.S., 2005. U.S. Government Printing Office; Washington, DC:: 2005. [Google Scholar]
- Waidmann T, Liu K. Disability trends among the elderly and implications for the future. Journal of Gerontology B: Social Sciences. 2000;55(5):S298–S307. doi: 10.1093/geronb/55.5.s298. [DOI] [PubMed] [Google Scholar]
- Wannamethee SG, Whincup PH, Shaper G, Walker M. Influence of fathers' social class on cardiovascular disease in middle-aged men. Lancet. 1996;348(9037):1259–1263. doi: 10.1016/S0140-6736(96)02465-8. [DOI] [PubMed] [Google Scholar]
- Wolf DA, Hunt K, Knickman J. Perspectives on the recent decline in disability at older ages. Milbank Quarterly. 2005;83(3):365–95. doi: 10.1111/j.1468-0009.2005.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf D, Mendes de Leon C, Glass T. Trends in rates of onset of and recovery from disability at older ages: 1982–1994. Journal of Gerontology B: Social Sciences. 2007;62(1):S3–S10. doi: 10.1093/geronb/62.1.s3. [DOI] [PubMed] [Google Scholar]
- Zimmer C. Do chronic diseases have an infectious root? Science. 2001;293(5537):1974–1977. doi: 10.1126/science.293.5537.1974. [DOI] [PubMed] [Google Scholar]
- Zimmer Z, House JS. Education, income, and functional limitation transitions among American adults: Contrasting onset and progression. International Journal of Epidemiology. 2003;32(6):1089–1097. doi: 10.1093/ije/dyg254. [DOI] [PubMed] [Google Scholar]