Abstract
Individuals with migraine headaches who are obese or overweight may be at elevated risk for experiencing more frequent migraines and for developing chronic migraine. This makes it imperative that clinicians consider including weight management as part of a migraine treatment plan in situations where the patient is overweight or obese. Weight loss and weight maintenance therapy should employ a combination of behavioral strategies, in particular nutritional education, dietary intervention, and exercise counseling, as a first line intervention. Weight loss medications are considered a secondary treatment; however, when weight loss medications are used, it is vital to monitor the influence of the medication on headache. Similarly, a clinician considering migraine prophylaxis needs to consider whether the pharmacologic agent being considered influences weight gain or loss.
Keywords: migraine, obesity, chronic disease management, chronic migraine, transformed migraine
OBESITY
Increased weight has reached epidemic proportions in the United States, where as many as 2 out of every 3 adults is either overweight or obese.1 In fact, the number of overweight (body mass index [BMI] = 25.0–29.9) and obese (BMI ≥ 30.0) Americans has increased nearly 70% in the past 15 years.2 Excess weight can have a severe negative impact on health-related quality of life and is a risk factor for hypertension, metabolic syndrome, diabetes, myocardial infarction, and stroke.3–6 Obesity and its associated health problems have a significant economic impact on the health-care system, accounting for 9.1% of total US medical expenditure in 1998 and reaching as high as $92.6 billion in 2002.7 Obesity is comorbid with a number of chronic pain syndromes and is associated with increased pain severity and treatment refractoriness.8–11 Weight loss, though, is followed by improved physical functioning.
The Clinical Relationship Between Migraine and Obesity
Clinical and empirical observations of headache sufferers have led some to propose a relationship between increased BMI and increased headache days and headache-related disability. This was first identified by Scher et al.12 In a longitudinal 1-year population study,13 3% of individuals with episodic headache progressed to having chronic daily headache (CDH). Among the risk factors for progression, obesity figured prominently. Obese individuals were 5 times more likely to develop CDH relative to those with normal weight (defined as BMI 18.5–24.9) while overweight individuals were 3 times more likely to develop CDH relative to those with normal weight. In the cross-sectional component of the study, obesity was found to be particularly influential in predicting CDH with migraine features (even after adjusting for other comorbidities and demographics), but not CDH without migraine features.13
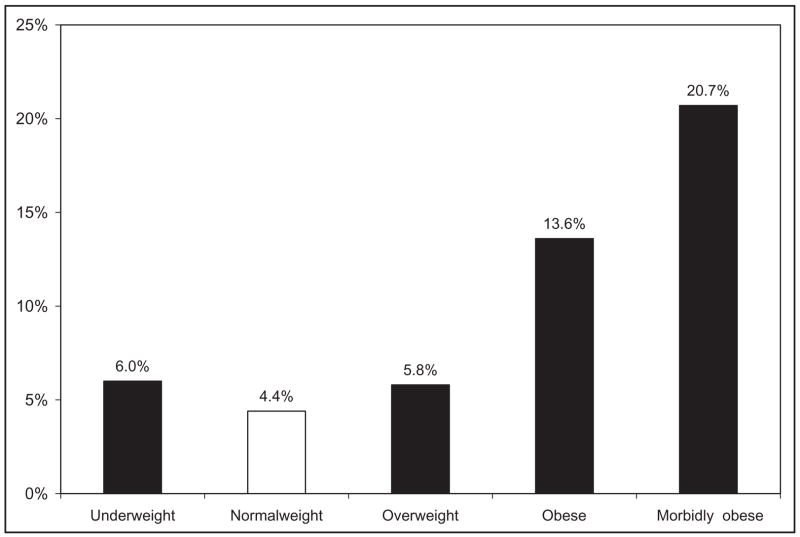
Other studies have continued to investigate the potential relationship between BMI, episodic migraine (EM) and chronic migraine (CM). One study focused on the relationship between BMI and EM.14 A total of 30,215 participants were interviewed, of which 3791 (12.5%) had migraine. Migraine prevalence, frequency of headache attacks, and headache features were modeled as a function of BMI after adjusting for covariates (age, sex, marital status, income, medical treatment, depressive symptoms, medication use). BMI was not associated with the prevalence of migraine. It was, however, associated with the frequency of headache attacks. Particular interest was given to those with 10–14 headache days per month (and thus at higher risk for developing CM). Among those with normal weight, 4.4% had 10–14 headache days per month. The overall rate among those who were overweight (5.8%) was not significantly different (OR = 1.3, 95% CI = 0.6–2.8). However, the rate among those who were obese (13.6%; OR = 2.9, 95% CI = 1.9–4.4) and severely obese (defined as BMI > 35.0;20.7%;OR 5.7, 95% CI = 3.6–8.8) was significantly higher relative to those with normal weight (Fig. 1).
Fig 1.
Prevalence of high-frequency migraine (migraineurs with 10–14 days of headache per month) according to the body mass index.15
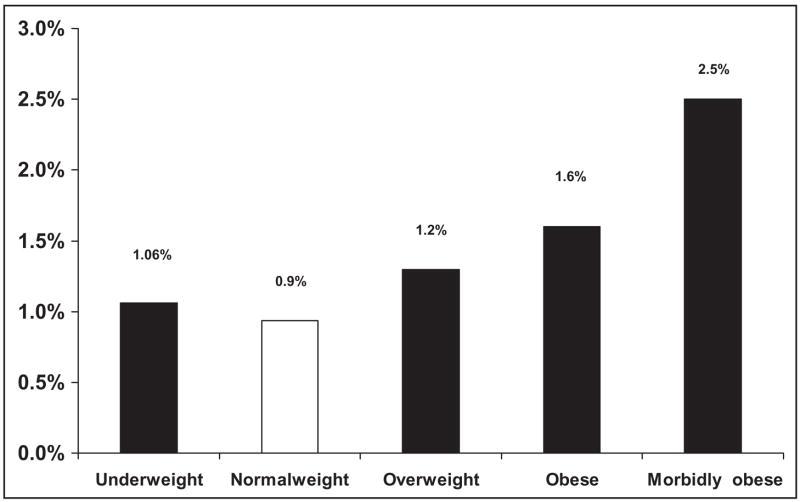
The same group examined the relationship between BMI, CDH and its subtypes, CM and chronic tension-type headache (CTTH).15 The study provided further support for obesity and CDH being comorbid, after adjusting for covariates (use of daily medications, gender, age, symptoms of depression, snoring). The results also found obesity to be a much stronger risk factor for CM than for CTTH. For CM, the prevalence was 0.9% of the normal weighted (reference group). This was significantly different from the overweight group (1.2%; OR = 1.4 [1.1–1.8]), the obese group (1.6%; [OR = 1.7 (1.2–2.43)]), and the severely obese group (2.5%; [OR = 2.2(1.5–3.2)]) (Fig. 2). Among those with CTTH, BMI only influenced prevalence of CTTH relative to normal weight among the severely obese.
Fig 2.
Prevalence of chronic migraine according to the body mass index.15 Analyses adjusted by age, gender, socioeconomic income, and depression. Odds ration and confidence intervals are described in the text.
Following, in the American Migraine Prevalence and Prevention study,16,17 the distribution of very frequent headache (10–14 days/month) was evaluated based on BMI and headache type. For migraine, 6.5% of those with normal weight had 10–14 days of headache. The proportion was not significantly higher among those who were overweight (7.4%), but was significantly higher in the obese (8.2%, P < .001) and severely obese (10.4%, P < .001) groups. For EM and tension-type headache, the differences were not significant. The disability of migraineurs also varied as a function of BMI. Overall, research conducted to date supports the concept that obesity is related to migraine progression but is not an exacerbating factor for headaches overall.
It is important to note that the relationship between BMI and migraine is independent of covariates. A recent study found that presence of depression or anxiety (especially both depression and anxiety) modified the strength of the relationship between BMI and migraine.18 However, it is important to note that the relationship, though modified, continued to exist.
Although a significant number of findings have supported the link between obesity and migraine, to date, a paucity of research has evaluated whether obesity predicts treatment refractoriness or if a reduction in obesity leads to a reduction in headache days. One study19 prospectively assessed the influence of the baseline BMI on the response to headache preventive treatment. The findings indicated that baseline BMI was predictive only of a reduction in the number of days with severe headache, with those being overweight or obese showing greater reduction (P < .01). However, when using logistic regression as a model and adjusting for covariates, BMI did not account for changes in disability, headache frequency, or in the number of days with severe headache per month. Thus, in this one study, obesity at baseline was not predictive of refractoriness to preventive treatment. However, future research needs to not only assess whether individuals response to treatment (both change in headache days and disability) is moderated by baseline BMI or perhaps even mediated by BMI change over time (for a further discussion of moderators and mediators in headache, see Nicholson et al20). Finally, a majority of the patients who have participated in trials looking at the relationship between obesity and CM have come from specialty headache centers. Future research will want to ensure that patients from all clinical settings are included where possible.
A discussion of potential mechanisms connecting obesity and migraine is beyond the scope of this manuscript. The interested reader is encouraged to read Bigal et al21 for a thorough review of potential mechanisms linking these 2 diseases.
INTERVENTION GUIDELINES AND STRATEGIES FOR WEIGHT MANAGEMENT IN MIGRAINE
Although evidence suggests that obesity is a modifiable risk factor for migraine progression, as discussed, it is still unknown if weight loss is related to decrease in headache frequency. However, it is recommended that all health-care providers communicate with patients who are overweight or obese about the overall health benefits of weight reduction. Thus, any subsequent reduction in headache frequency or headache-related disability will be over and above the health benefits of weight loss.
Weight loss therapy should employ a combination of nutritional education, dietary intervention, and exercise counseling with behavioral strategies22–26 as the first line of intervention. Doing so will help patients acquire the knowledge and develop the skills needed to improve their eating patterns and increase physical activity. Evidence suggests that the best outcomes for weight management will occur when the patient is in regular contact with professionals to promote weight loss and maintenance.27,28 For obese patients, it is recommended that a more intensive (>1 individual or group session per month) for at least the first 3 months of the intervention. A variety of health professionals may effectively deliver these interventions, including physicians, psychologists, dietitians, behavioral therapists, exercise instructors, and multi-disciplinary teams.29
According to the US Preventive Task Force26 and the National Heart, Lung, and Blood Institute’s Obesity Education Initiative (NHLBI-OEI),23 the initial goal of weight loss therapy is to reduce body weight by approximately 10% over a 6-month period. It is vital that a weight maintenance program that continues to emphasize dietary therapy, physical activity, and behavior therapy.
The key to weight loss is eating healthy. NHLBI-OEI recommends achieving this via a low-calorie diet (LCD) (800 to 1500 kcal/day).23,30,31 Increased physical activity can help enhance the effects of an LCD and is crucial for weight loss maintenance.22,32 Moreover, regular exercise may have migraine management benefits as well.33,34 In general, moderate physical activity for 30–45 minutes, 3–5 days per week should be considered a minimum requirement. Working toward moderate physical activity almost all days of the week is a recommended goal for adults.35,36
Behavioral weight management strategies can be an integral part of a lifestyle weight management program. Behavioral strategies can be used to provide the patient skills to address barriers to eating an LCD and engaging in physical activity.23,37–40 These strategies include:
Self-monitoring of eating habits (amount and types of food, calories consumed, and nutrient composition) and physical activity (frequency, intensity, and type).
Using stress management (cognitive coping, relaxation) to keep from engaging in “stress eating.”
Identifying high-risk situations (eg, having high calorie foods in the house, certain places where overeating occurs), planning and implementing a healthier alternative (eg, keeping high-calorie foods out of the house, limiting the times and places of eating, and consciously avoiding situations in which overeating occurs), and evaluating the outcome of making the changes.
Recognizing inaccurate beliefs about weight loss and body image that need to be modified to help change self-defeating thoughts and feelings that undermine weight loss efforts. For example, the thought, “I blew my diet at lunch by eating those french fries and milkshake; today is a waste, so I will eat whatever the rest of the day” is inaccurate; an alternative is “so I ate the fries and milkshake at lunch, I can eat a healthy dinner and be right back on track”; and
Identifying and utilizing a strong social support system (eg, family, friends, work colleagues, a weight reduction support group)
Federal guidelines encourage pharmacologic intervention be considered a secondary source of treatment and used only in conjunction with concomitant lifestyle modification.23,26,35,36 Orlistat and sibutramine, approved for weight loss by the Food and Drug Administration, can produce modest weight loss.40–43 However, it is important to note that these medications, as well as other short-term weight loss medications (typically central nervous system stimulants), often have headache as a side effect. Thus, it is vital that physicians seriously consider whether use of these medications is appropriate for migraine sufferers given the potential for more frequent headaches.
Similarly, in patients with migraine using migraine preventive pharmacotherapy, it is important to note the effects of the medication on weight, since the most frequently used medications are not weight neutral. Among the FDA-approved migraine medications, only topiramate has been shown to promote weight loss.44 Reviews of prophylactic medications in general and those used to prevent migraine both suggest that a majority of prophylactic medications promote weight gain although there are some medications that appear to be weight neutral.45–47 Given that a full review of the weight effects of individual medications is not the purpose of the manuscript, the interested reader is encouraged to consult Maggioni et al46 or Young and Rozen47 for a detailed analysis of the weight effects of various migraine prevention medication. Thus, it is important for any clinician communicating with their migraine patient to note the potential weight change that may result from taking particular preventive. Among those who are overweight or obese, this is especially crucial to consider.
Overall, it appears that obese individuals may be at increased risk for developing CM. However, not nearly enough research has been conducted to date to make definitive statements about the exact nature of this relationship. Almost no prospective trials have examined whether weight reduction decreases the odds of developing CM. Also, there are no trials looking at whether weight gain leads to a subsequent increase in the odds of developing CM.
Given the influence a number of medications have on weight and on headache, it is vital that clinicians not ignore this issue when considering pharmacologic intervention to prevent migraine. The same holds true when clinicians consider utilizing weight loss medications. One of the benefits of behavioral weight management is that the influence it has on headache is significantly minimized. In summary, clinicians need to be cognizant that a patient’s weight may influence the frequency and chronicity of migraine and need to include weight management as part of any migraine treatment plan among overweight and obese individuals.
Footnotes
Conflict of Interest: None
References
- 1.Lethbridge-Cejku M, Rose D, Vickerie J. Summary health statistics for U.S. adults: National Health Interview Survey, 2004. National Center for Health Statistics. Vital Health Stat. 2006;10:1–154. [PubMed] [Google Scholar]
- 2.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 3.Kurth T, Gaziano M, Km R, et al. Prospective study of body mass index and risk of stroke in apparently healthy women. Circulation. 2005;111:1992–1998. doi: 10.1161/01.CIR.0000161822.83163.B6. [DOI] [PubMed] [Google Scholar]
- 4.National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health risk. Arch Int Med. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 5.Pi-Sunyer FX. The medical risks of obesity. Obs Surg. 2002;12(Suppl):6S–11S. doi: 10.1007/BF03342140. [DOI] [PubMed] [Google Scholar]
- 6.Rexrode KM, Hennekens CH, Willett WC, et al. A prospective study of body mass index, weight change, and risk of stroke in women. JAMA. 1997;277:1539–1545. doi: 10.1001/jama.1997.03540430051032. [DOI] [PubMed] [Google Scholar]
- 7.Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: How much, and who’s paying? Health Affairs. 2003;W3:219–226. doi: 10.1377/hlthaff.w3.219. [DOI] [PubMed] [Google Scholar]
- 8.Barofsky I, Fontaine KR, Cheskin LJ. Pain in the obese: Impact on health-related quality-of-life. Ann Behav Med. 1997;19:408–410. doi: 10.1007/BF02895160. [DOI] [PubMed] [Google Scholar]
- 9.Lean ME, Han TS, Seidell JC. Impairment of health and quality of life using new US federal guidelines for the identification of obesity. Arch Int Med. 1999;159:837–843. doi: 10.1001/archinte.159.8.837. [DOI] [PubMed] [Google Scholar]
- 10.Marcus DA. Obesity and the impact of chronic pain. Clin J Pain. 2004;20:186–191. doi: 10.1097/00002508-200405000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Fontaine KR, Cheskin LJ, Barofsky I. Health-related quality of life in obese persons seeking treatment. J Fam Pract. 1996;43:265–270. [PubMed] [Google Scholar]
- 12.Scher AI, Lipton RB, Stewart WF. Risk factors for chronic daily headache. Curr Pain Headache Rep. 2002;6:486–491. doi: 10.1007/s11916-002-0068-8. [DOI] [PubMed] [Google Scholar]
- 13.Scher AI, Stewart WF, Ricci JA, Lipton RB. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003;106:81–89. doi: 10.1016/s0304-3959(03)00293-8. [DOI] [PubMed] [Google Scholar]
- 14.Bigal ME, Liberman JN, Lipton RB. Obesity and migraine. A population study. Neurology. 2006;66:545–550. doi: 10.1212/01.wnl.0000197218.05284.82. [DOI] [PubMed] [Google Scholar]
- 15.Bigal ME, Lipton RB. Obesity is a risk factor for transformed migraine but not chronic-tension-type headache. Neurology. 2006;67:252–257. doi: 10.1212/01.wnl.0000225052.35019.f9. [DOI] [PubMed] [Google Scholar]
- 16.Bigal ME, Gironda M, Tepper SJ, et al. Headache prevention outcome and body mass index. Cephalalgia. 2005;26:445–450. doi: 10.1111/j.1468-2982.2005.01054.x. [DOI] [PubMed] [Google Scholar]
- 17.Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343–349. doi: 10.1212/01.wnl.0000252808.97649.21. [DOI] [PubMed] [Google Scholar]
- 18.Tietjen GE, Peterlin BL, Brandes JL, et al. Depression and anxiety: Effect on the migraine-obesity relationship. Headache. 2007;47:866–875. doi: 10.1111/j.1526-4610.2007.00810.x. [DOI] [PubMed] [Google Scholar]
- 19.Bigal ME, Gironda M, Tepper SJ, et al. Headache prevention outcome and body mass index. Cephalalgia. 2006;26:445–450. doi: 10.1111/j.1468-2982.2005.01054.x. [DOI] [PubMed] [Google Scholar]
- 20.Nicholson RA, Hursey KG, Nash JM. Moderators and mediators of behavioral treatments for headache. Headache. 2005;45:513–519. doi: 10.1111/j.1526-4610.2005.05103.x. [DOI] [PubMed] [Google Scholar]
- 21.Bigal ME, Lipton RB, Holland PR, Goadsby PJ. Obesity, migraine, and chronic migraine: Possible mechanisms of interaction. Neurology. 2007;68:1851–1861. doi: 10.1212/01.wnl.0000262045.11646.b1. [DOI] [PubMed] [Google Scholar]
- 22.Katzel LI, Bleecker ER, Colman EG, Rogus EM, Sorkin JD, Goldberg AP. Effects of weight loss vs aerobic exercise training on risk factors for coronary disease in healthy, obese, middle-aged and older men. A randomized controlled trial. JAMA. 1995;274:1915–1921. doi: 10.1001/jama.1995.03530240025035. [DOI] [PubMed] [Google Scholar]
- 23.NHLBI Obesity Education Initiative. NIH Publication No. 98–4083. Bethesda, MD: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute; 1998. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. [Google Scholar]
- 24.Sheppard L, Kristal AR, Kushi LH. Weight loss in women participating in a randomized trial of low-fat diets. Am J Clin Nutr. 1991;54:821–828. doi: 10.1093/ajcn/54.5.821. [DOI] [PubMed] [Google Scholar]
- 25.Schlundt DG, Hill JO, Pope-Cordle J, Arnold D, Virts KL, Katahn M. Randomized evaluation of a low fat ad libitum carbohydrate diet for weight reduction. Int J Obes Relat Metab Disord. 1993;17:623–629. [PubMed] [Google Scholar]
- 26.U.S. Preventive Services Task Force. Screening for Obesity in Adults: Recommendations and Rationale. Rockville, MD: Agency for Healthcare Research and Quality; 2003. Available at: http://www.ahrq.gov/clinic/3rduspstf/obesity/obesrr.htm. [Google Scholar]
- 27.Perri MG, McAllister DA, Gange JJ, Jordan RC, McAdoo G, Nezu AM. Effects of four maintenance programs on the long-term management of obesity. J Consult Clin Psychol. 1988;56:529–534. doi: 10.1037//0022-006x.56.4.529. [DOI] [PubMed] [Google Scholar]
- 28.Wadden TA, Berkowitz RI, Sarwer DB, Prus-Wisniewski R, Steinberg C. Benefits of lifestyle modification in the pharmacologic treatment of obesity: A randomized trial. Arch Intern Med. 2001;161:218–227. doi: 10.1001/archinte.161.2.218. [DOI] [PubMed] [Google Scholar]
- 29.McTigue K, Harris R, Hemphill MB, et al. Screening and Interventions for Obesity in Adults. Systematic Evidence Review No. 21 (Prepared by the Research Triangle Institute-University of North Carolina Evidence-based Practice Center under Contract 290–97–0011). Rockville, MD: Agency for Health-care Research and Quality; 2003. Available at http://www.ahrq.gov/clinic/serfiles.htm.
- 30.VanItallie TB, Yang M-U. Current concepts in nutrition: Diets and weight loss. N Engl J Med. 1977;297:1158–1161. doi: 10.1056/NEJM197711242972106. [DOI] [PubMed] [Google Scholar]
- 31.Yang M, VanItallie TB. Effect of energy restriction on body composition and nitrogen balance in obese individuals. In: Wadden TA, VanItallie TB, editors. Treatment of the Seriously Obese Patient. New York: Guilford Press; 1992. pp. 83–106. [Google Scholar]
- 32.Stefanick ML, Mackey S, Sheehan M, Ellsworth N, Haskell WL, Wood PD. Effects of the NCEP Step 2 diet and exercise on lipoprotein in postmenopausal women and men with low HDL-cholesterol and high LDL-cholesterol. N Engl J Med. 1998;339:12–20. doi: 10.1056/NEJM199807023390103. [DOI] [PubMed] [Google Scholar]
- 33.Köseoglu E, Akboyraz A, Soyuer A, Ersoy A. Aerobic exercise and plasma beta endorphin levels in patients with migrainous headache without aura. Cephalalgia. 2003;23:972–976. doi: 10.1046/j.1468-2982.2003.00624.x. [DOI] [PubMed] [Google Scholar]
- 34.Lockett DC, Campbell JF. The effects of aerobic exercise on migraine. Headache. 1992;32:50–54. doi: 10.1111/j.1526-4610.1992.hed3201050.x. [DOI] [PubMed] [Google Scholar]
- 35.NIH Consensus Conference. Physical activity and cardiovascular health. JAMA. 1996;276:241–246. [PubMed] [Google Scholar]
- 36.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 37.Douketis JD, Feightner JW, Attia J, Feldman WF. Periodic health examination, 1999 update: 1. Detection, prevention and treatment of obesity. Canadian Task Force on Preventive Health Care. CMAJ. 1999;160:513–525. Available at: http://www.cmaj.ca/cgi/reprint/160/4/513.pdf (retrieved July 7, 2007) [PMC free article] [PubMed] [Google Scholar]
- 38.NHS Center for Reviews and Dissemination University of York. The prevention and treatment of obesity. Eff Health Care. 1997;3:1–12. [Google Scholar]
- 39.Wadden TA, Foster GD. Behavioral assessment and treatment of markedly obese patients. In: Wadden TA, VanItallie TB, editors. Treatment of the Seriously Obese Patient. New York: Guilford Press; 1992. pp. 290–330. [Google Scholar]
- 40.Wadden TA, Berkowitz RI, Womble LG, et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. N Engl J Med. 2005;353:2111–2120. doi: 10.1056/NEJMoa050156. [DOI] [PubMed] [Google Scholar]
- 41.Arterburn D, Noel PH. Effects of drug treatment for obesity in adults. BMJ Clin Evid. 2001;322:412–419. [Google Scholar]
- 42.Sidhaye A, Cheskin LJ. Pharmacologic treatment of obesity. Adv Psychsom Med. 2006;27:42–52. doi: 10.1159/000090962. [DOI] [PubMed] [Google Scholar]
- 43.Snow V, Barry P, Fitterman N, Qaseem A, Weiss K. Pharmacologic and surgical management of obesity in primary care: A clinical practice guideline from the American College of Physicians. Ann Int Med. 2005;142:525–531. doi: 10.7326/0003-4819-142-7-200504050-00011. [DOI] [PubMed] [Google Scholar]
- 44.Silberstein SD. Topiramate in migraine prevention. Headache. 2005;45(Suppl 1):S57–S65. doi: 10.1111/j.1526-4610.2005.4501005.x. [DOI] [PubMed] [Google Scholar]
- 45.Leslie WS, Hankey CR, Lean MEJ. Weight gain as an adverse effect of some commonly prescribed drugs: A systematic review. QJM. 2007;100:395–404. doi: 10.1093/qjmed/hcm044. [DOI] [PubMed] [Google Scholar]
- 46.Maggioni F, Ruffatti S, Dainese F, Mainardi F, Zanchin G. Weight variations in the prophylactic therapy of primary headaches: 6-month follow-up. J Headache Pain. 2005;6:322–324. doi: 10.1007/s10194-005-0221-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Young WB, Rozen TD. Preventive treatment of migraine: Effect on weight. Cephalalgia. 2005;25:1–11. doi: 10.1111/j.1468-2982.2004.00819.x. [DOI] [PubMed] [Google Scholar]