Abstract
This multicentre, randomised phase III study compared docetaxel with 5-fluorouracil+vinorelbine in patients with metastatic breast cancer after failure of neo/adjuvant or one line of palliative anthracycline-based chemotherapy. One hundred and seventy-six metastatic breast cancer patients were randomised to receive docetaxel (100 mg m−2) every 3 weeks or 5-fluorouracil+vinorelbine: 5-fluorouracil (750 mg m−2 per day continuous infusion) D1–5 plus vinorelbine (25 mg m−2) D1 and D5 of each 3-week cycle. Eighty-six patients received 516 cycles of docetaxel; 90 patients received 476 cycles of 5-fluorouracil+vinorelbine. Median time to progression (6.5 vs 5.1 months) and overall survival (16.0 vs 15.0 months) did not differ significantly between the docetaxel and 5-fluorouracil+vinorelbine arms, respectively. Six (7%) complete responses and 31 (36%) partial responses occurred with docetaxel (overall response rate 43%, 95% confidence interval: 32–53%), while 4 (4.4%) complete responses and 31 (34.4%) partial responses occurred with 5-fluorouracil+vinorelbine (overall response rate 38.8%, 95% confidence interval: 29–49%). Main grade 3–4 toxicities were (docetaxel vs 5-fluorouracil+vinorelbine): neutropenia 82% vs 67%; stomatitis 5% vs 40%; febrile neutropenia 13% vs 22%; and infection 2% vs 7%. There was one possible treatment-related death in the docetaxel arm and five with 5-fluorouracil+vinorelbine. In anthracycline-pretreated metastatic breast cancer patients, docetaxel showed comparable efficacy to 5-fluorouracil+vinorelbine, but was less toxic.
British Journal of Cancer (2002) 87, 1210–1215. doi:10.1038/sj.bjc.6600645 www.bjcancer.com
Keywords: metastatic breast cancer, anthracycline, docetaxel, 5-fluorouracil, second-line chemotherapy, vinorelbine
Metastatic breast cancer (MBC) is sensitive to chemotherapy but remains incurable with current therapeutic approaches. Single agents such as doxorubicin or epirubicin, cyclophosphamide, 5-fluorouracil (5-FU) and methotrexate achieve overall response rates (ORRs) ranging from 20 to 50% in this setting (Henderson et al, 1987; Clavel and Catimel, 1993). Combinations of alkylating agents with anthracyclines are extensively used in MBC and yield ORRs ranging from 40 to 60%, with complete response rates <20%, and a median response duration <15 months (The French Epirubicin Study Group, (1991); Brufman et al, 1997; del Mastro et al, 2001).
Use of anthracyclines is associated with problems of cumulative cardiotoxicity and primary or secondary resistance. As a result, there is a limit to the cumulative dose and number of regimens that can be administered to any given patient. Subsequent therapy in case of treatment failure is, therefore, a problem. Single-agent docetaxel has been proposed as an alternative treatment for patients previously treated with anthracycline-based therapy; the efficacy of this drug has been demonstrated in pretreated patients with MBC (Ravdin et al, 1995; Valero et al, 1995; Nabholtz and Crown, 1998; Alexopoulos et al, 1999; Brodowicz et al, 2000).
In patients with anthracycline-resistant MBC, docetaxel (100 mg m−2), infused over 1 h every 3 weeks, induces ORRs ranging from 30 to 69% (Ravdin et al, 1995; Valero et al, 1995; Nabholtz and Crown, 1998; Alexopoulos et al, 1999; Brodowicz et al, 2000).
Single-agent vinorelbine, in second-line or salvage chemotherapy for MBC, has a reported response rate of approximately 16% (Degardin et al, 1994; Gasparini et al, 1994), and the effectiveness of continuous infusion 5-FU in adenocarcinomas is well established (Caballero et al, 1985). A combination of vinorelbine plus 5-FU (FUN) has been administered to patients who have failed anthracycline therapy. In a phase II study, vinorelbine (30 mg m−2 D1) plus 5-FU (350 mg m−2 per day continuous infusion D1–3) in pretreated MBC patients exhibited substantial activity (ORR 43%) and acceptable tolerability, with the main toxic effect being severe neutropenia in 24% of patients (Froudarakis et al, 1998). In another phase II study, first-line administration of FUN (vinorelbine 30 mg m−2 D1 and D5 plus 5-FU 750 mg m−2 per day continuous infusion D1–5) resulted in an ORR of 62% (Dieras et al, 1996). Main grade 3–4 toxicities comprised neutropenia (90%), mucositis (37%) and infection (13%). Nevertheless, the majority of patients received treatment on an outpatient basis. Such results culminated in the use of the FUN regimen in advanced breast cancer in France.
In this randomised phase III trial, we compared the efficacy and safety of single-agent docetaxel vs FUN in patients with MBC who had relapsed after anthracycline-based chemotherapy comprising neoadjuvant or adjuvant treatment, or one line of palliative chemotherapy. The schedules used are based on the results of previous studies (Dieras et al, 1996; Froudarakis et al, 1998).
MATERIALS AND METHODS
Patient selection
Patients were eligible for the study if they had histologically confirmed MBC, had been pretreated with one anthracycline-based chemotherapy regimen, were female and were aged >18 years. All patients were required to have measurable or evaluable disease; a World Health Organisation (WHO) performance status (PS) ⩽2; a 4-week wash-out period after any antitumour treatment; and adequate haematological, liver and renal functions. Written informed consent was obtained from each patient before study treatment. The exclusion criteria were: only locally advanced disease; prior therapy with either taxanes or vinorelbine; more than one line of prior palliative chemotherapy; CNS involvement; osteoblastic bone lesions, carcinomatous lymphangitis of the lung or serous effusions as the only sites of disease; sensory neuropathy ⩾grade 2; or any severe concomitant condition, including coronary insufficiency.
As in previous docetaxel studies, patients were classified as anthracycline-sensitive or -resistant/refractory based on the following definitions: refractory (progressive disease during neoadjuvant or adjuvant chemotherapy, or progressive disease as the best response to palliative chemotherapy); resistant (relapse within the 12 months following either adjuvant or neoadjuvant chemotherapy, or disease progression on palliative chemotherapy after initial response); potentially sensitive (relapse more than 12 months after adjuvant chemotherapy or disease progression more than 4 weeks after the end of palliative chemotherapy) (Nabholtz and Crown, 1998).
Drug administration
Patients were randomly assigned on a one-to-one basis to 1 of 2 groups, stratified by accruing centre. Patients received either docetaxel (Taxotere®, Aventis Pharmaceuticals, Paris, France) 100 mg m−2 over a 1-h i.v. infusion every 3 weeks, or 5-FU 750 mg m−2 per day continuous infusion on five consecutive days plus vinorelbine 25 mg m−2 over a 30-min infusion on days 1 and 5 of the 3-week cycle.
Premedication with an oral steroid (prednisolone 50 mg) was administered at 13, 7 and 1 h before each docetaxel infusion and then twice daily for the next 4 days. In both arms, treatment was planned for a maximum of nine cycles, except in the case of disease progression, unacceptable toxicity or consent withdrawal. Where significant toxicity occurred (WHO grade 3–4 non-haematological toxicity, febrile neutropenia or cycle delay >2 weeks) dose reductions were made in subsequent cycles. A maximum of two dose reductions per patient were allowed for both docetaxel (75 mg m−2, then 55 mg m−2) and 5-FU (600 mg m−2, then 500 mg m−2), and only one for vinorelbine (20 mg m−2). Dosing re-escalation was not allowed.
Evaluation
Pretreatment evaluation consisted of a complete medical history and physical examination; complete blood cell count; biochemical profile and urinalysis; ECG; echocardiography or MUGA in case of known heart disease; measurement of all tumour-associated lesions by chest X-ray, abdominal ultrasound and/or computed tomography (CT) scan; and a bone scan complemented by X-ray, CT or magnetic resonance imaging of hot spots. Before each treatment cycle, patients had a physical examination, complete blood cell count, biochemical profile and urinalysis. A complete blood cell count was performed on day 5 of each cycle. Toxicity was evaluated according to WHO criteria (Miller et al, 1981). Antitumour activity was assessed every 3 cycles (after cycles 3, 6 and 9) on all target lesions. On day 28 after the last infusion, patients had a complete tumour evaluation, physical examination and ECG.
Tumour responses and time-related parameters were assessed according to WHO criteria (Miller et al, 1981). Time to progression (TTP) was calculated from the first treatment infusion to the first objective evidence of tumour progression. All responses documented by imaging were reviewed by an external panel of radiologists.
Statistical methods
The primary endpoint of the study was TTP. In order to reject the null hypothesis of no difference between the two study arms, enrolment of 180 patients (90 per arm) was planned. The sample size provided the study with 85% power to detect a difference in progression free survival (after 9 cycles) of 60% in the docetaxel arm and 40% in the FUN arm, with a type I error of 0.05.
The Kaplan–Meier method was employed to analyse time-related parameters, and comparisons were performed using the non-parametric log rank test. The χ-test was used for non-censored qualitative parameters and Student's t-test for non-censored quantitative parameters. A multivariate analysis for prognostic factors was performed using a Cox proportional hazards model.
RESULTS
Patient characteristics
Between June 1995 and July 1997, 178 patients (docetaxel: 88; FUN: 90) were enrolled into the study in 22 centres. However, two patients in the docetaxel arm did not receive treatment – one due to brain metastases diagnosed after randomisation, and the other due to consent withdrawal – yielding 176 treated patients. (Although the planned total of 180 patients were unavailable for recruitment, the 176 treated patients were sufficient for achieving the statistical hypothesis.) Baseline characteristics of the 176 treated patients (Table 1) were well balanced between the two treatment groups. The median age was 54.8 years, and 81% of patients had a PS⩽1. The median number of organs involved was two. The majority of patients (67%) had liver metastases.
Table 1. 1 Demographics and baseline characteristics of the patients treated in the study.

All patients (except one in the docetaxel group, who was nonetheless considered as eligible without major protocol deviation) had received prior treatment with anthracycline-based chemotherapy; 66% of these patients received prior chemotherapy for advanced disease. According to the definitions for anthracycline sensitivity/resistance, 106 (60%) of the patients were potentially anthracycline-sensitive, including 22% relapsing more than 12 months after the completion of an adjuvant therapy.
Treatment administration
Study treatment comprised 516 cycles of docetaxel (median per patient: 6; range: 1–12) and 476 cycles of FUN (median per patient: 6; range: 1–9). In the docetaxel arm, dose reductions were made in 75 of the 430 cycles in which a reduction was allowed (17%) and in the FUN arm, 171 of the 386 cycles were reduced (44%). Delays longer than 7 days occurred in 17 cycles in the docetaxel arm (3.9%) and 96 cycles in the FUN arm (25%). Consequently, the relative dose intensity of docetaxel was 0.97 while those of 5-FU and vinorelbine were 0.88 and 0.84, respectively.
Efficacy
Results are presented for the intention-to-treat populations, unless otherwise indicated.
Primary endpoint: time to progression
As of 30 November 1998, the median follow up was 30.3 months (range 10.4–45.0 months) with 15 patients (17%) in the docetaxel arm and 22 (24%) in the FUN arm having experienced no disease progression at the cut-off date. The median TTP was 6.5 months (95% CI: 5.5–8.4 months) in the docetaxel arm (15 patients censored) and 5.1 months (95% CI: 4.4–6.9 months) in the FUN arm (22 patients censored; P=0.34; Figure 1). When only the 70 anthracycline-resistant/refractory patients were taken into account, the median TTP was 6.2 months in the docetaxel arm (seven patients censored) and 4.3 months in the FUN arm (eight patients censored; P=0.13; Figure 2).
Figure 1.

Time to tumour progression in the all-treated population.
Figure 2.
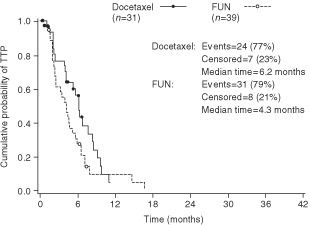
Time to tumour progression in the anthracycline-resistant/ refractory population.
Secondary endpoints
In the docetaxel arm there were six complete responses (CRs) (7%) and 31 partial responses (PRs) (36%), giving an ORR of 43%. In the FUN arm there were four CRs (4.4%) and 31 PRs (34.4%), giving an ORR of 39% (see Table 2). The difference in ORR was not statistically significant (P=0.69). The median duration of objective responses was 8.4 months in the docetaxel arm and 7.8 months in the FUN arm. The ORRs in evaluable patients with liver, bone or lung metastases were 38, 51 and 53%, respectively, in the docetaxel arm; and 49, 44 and 52%, respectively, in the FUN arm.
Table 2. Tumour responses (ITT).

The ORRs in evaluable patients with 1, 2, 3 or >3 organs involved, were 43, 52, 53 and 40%, respectively, in the docetaxel arm; and 57, 48, 31 and 53%, respectively, in the FUN arm. These rates did not differ significantly between the two arms.
There was no difference between the two arms in overall survival (OS). The median OS was 16 months for docetaxel (35 patients censored) and 15 months for FUN (45 patients censored) (Figure 3).
Figure 3.
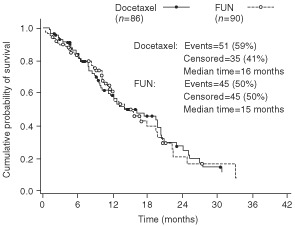
Overall survival in the all-treated population.
When only the 70 anthracycline-resistant/refractory patients were taken into account, docetaxel yielded an ORR of 39% (12/31 patients) vs 23% (9/39 patients) for FUN, and the median survival was 11.5 months in both the docetaxel and FUN arms (Figure 4).
Figure 4.
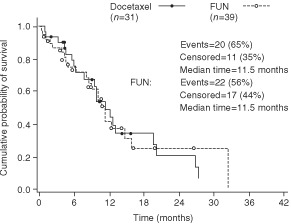
Overall survival in the anthracycline-resistant/refractory population.
Univariate and multivariate analysis
The objective of these analyses was to determine significant prognostic factors for TTP. First, a univariate analysis was performed on 12 factors, and all factors found to have a statistical significance (at the level of P<0.20) were carried forward for a multivariate analysis using a Cox proportional hazards model. Of the 12 prognostic factors included in the univariate analysis, four were found to correlate with TTP. The multivariate stepwise analysis confirmed that two of these four factors (anthracycline sensitivity and the number of organs involved) were significantly correlated with the TTP (Table 3). A patient having ⩾ three organs involved had a 1.72 greater risk of progression than a patient with two or fewer involved organs, and prior anthracycline resistance increased the risk of progression by 1.51.
Table 3. Multivariate analysis of the time to progression (TTP).

Safety
The safety profiles for each treatment arm are summarised in Table 4. The main toxicity (WHO grade 3–4) in both treatment arms was neutropenia. Grade 3–4 neutropenia was significantly more frequent with docetaxel than with FUN (82 vs 67%, respectively; P=0.02), while severe thrombocytopenia and severe stomatitis were significantly more frequent with FUN than with docetaxel (10 vs 1%, respectively; P=0.02 and 40 vs 5%, respectively; P<0.0001). Febrile neutropenia occurred more frequently with FUN than with docetaxel (22 vs 13%, respectively; P=0.10), as did infection (grade 3–4) (7 vs 2%, respectively; P=0.28). Docetaxel led to more alopecia (67 vs 24%; P<0.0001) and sensory neuropathy (grade 1–2) (35 vs 6%; P<0.0001) than FUN. Characteristic cumulative severe dose-related side effects of docetaxel (i.e. fluid retention (peripheral oedema), nail dystrophy and skin reactions) were graded as severe in only 3, 2 and 0% of patients, respectively.
Table 4. Grade 3–4 toxicities (WHO criteria).
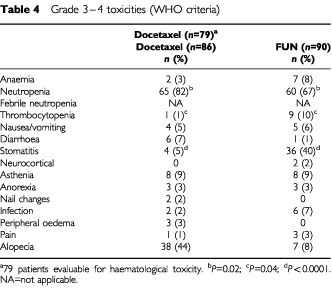
In the docetaxel arm, three patients died during the study: two from progressive disease, which was not considered to be related to treatment, and one from congestive heart failure, possibly related to treatment. In the FUN arm, nine patients died during the study. Five deaths were considered to be probably related to study treatment (three sepsis, one liver failure and one grade 4 diarrhoea and mucositis associated with liver and renal failure). Four deaths were not considered to be related to treatment: two died from disease progression, one from acute pulmonary oedema, one from hepato-cellular insufficiency.
DISCUSSION
Prior to widespread taxane use, several second-line chemotherapy regimens were used after the failure of anthracycline-based regimens. These included vinorelbine plus mitomycin C (Vici et al, 1996), vinorelbine combined with cisplatin (Ray-Coquard et al, 1998), and 5-FU as single agent or combined with vinorelbine (Cany et al, 1996; Dieras et al, 1996; Froudarakis et al, 1998). The approval of docetaxel as a single agent in this setting, based on high response rates in phase II studies (Ravdin et al, 1995; Valero et al, 1995; Marty et al, 1997), prompted this randomised trial in which the efficacy and safety of docetaxel was compared with that of the FUN regimen, a popular treatment for advanced breast cancer patients in France.
The patient characteristics in this trial were representative of those for the general population of patients with MBC. Interestingly, 60% of the patients in this study were considered to be potentially sensitive to anthracycline according to available operational definitions. There was no evidence of any imbalance in baseline characteristics between the two groups.
In terms of efficacy, there were no significant differences in TTP, response rate, response duration or OS between the two treatments. There was, however, a trend towards both a higher ORR, particularly in anthracycline-resistant tumours, and a longer TTP with docetaxel. The response rate in anthracycline-resistant/refractory patients was 39% with docetaxel vs 23% with FUN. The small sample size of this sub-group (31 for docetaxel, 39 for FUN), does not allow pertinent statistical analysis of the two treatments.
The ORRs observed in both arms of the study are similar to those seen in other studies. The ORR of 43% for docetaxel reported in our study is similar to the ORR of 48% observed by Chan in a phase III study of MBC patients who had failed alkylating agent therapy (Chan et al, 1999). The ORR of 39% observed for the FUN regimen in the current study is similar to the 43% ORR reported by Froudarakis et al (1998) in patients with MBC who had all been pretreated, mainly with anthracyclines.
Interestingly, the ORR of 43% for docetaxel (for all patients pretreated with anthracyclines) observed in this study is better than the ORR of 30% observed by Nabholtz et al (1999), who compared docetaxel as a single agent against vinblastine and mitomycin C (VMC) in patients who had failed anthracycline therapy. However, patients who relapsed more than 12 months after adjuvant chemotherapy were not accepted, and 43% of patients considered not to be resistant had progressive disease more than 30 days after the completion of palliative chemotherapy. VMC was found to be better tolerated than docetaxel, but docetaxel led to a significantly improved response rate. Median TTP was significantly longer in the docetaxel arm than in the VMC arm (19 weeks vs 11 weeks; P=0.001), as was median OS (11.4 months vs 8.7 months in all randomised patients; P=0.01). The cohort enrolled in the Nabholtz study had a higher rate of anthracycline resistance and a poorer prognostic profile than the patients in our study, as is supported by their shorter TTP and survival. The Nabholtz study also enrolled 392 patients, including 220 (56%) true anthracycline-resistant patients, as opposed to 70 (40%) anthracycline-resistant patients in our study.
The safety profiles of the two treatments differed. Docetaxel induced higher incidence of alopecia, grade 1–2 peripheral neuropathy, fluid retention, skin and nail disorders and grade 3–4 neutropenia, whereas FUN was responsible for more grade 3–4 stomatitis and thrombocytopenia. Despite the lower incidence of severe neutropenia with FUN, patients receiving this therapy experienced more febrile neutropenia and neutropenic infections than patients receiving docetaxel. Sepsis was responsible for three deaths in the FUN group, whereas no patients died from a neutropenia-related complication in the docetaxel group. This striking mortality difference is probably due to the association of febrile neutropenia and stomatitis with the FUN regimen.
The feasibility of the FUN regimen in this trial was compromised by poor compliance. There were more frequent dose reductions and dose delays, which were responsible for lower relative dose intensities of 5-FU and vinorelbine than docetaxel. The FUN regimen chosen was based on the results of studies carried out before this trial was started (Dieras et al, 1996; Froudarakis et al, 1998). However, more recent trials indicate that other FUN regimens may be less toxic (Lombardi et al, 2000; Zambetti et al, 2000).
In conclusion, single-agent docetaxel (100 mg m−2) is as effective as, and less haematologically toxic than, the chosen FUN regimen. Furthermore, the single 1-h docetaxel infusion is more convenient than the 5-day FUN regimen. Our results, together with those of another controlled trial (Nabholtz et al, 1999), demonstrate that docetaxel as a single agent is an important and easy-to-use treatment option in MBC after anthracycline failure.
Acknowledgments
This study was supported by a grant from Laboratoires Aventis, Paris, France. The authors wish to thank the following physicians for their participation in the trial: S Culine, M Rios, D Serin, JC Eymard, N Tubiana-Mathieu, D Lepille, L Mauriac, R Schaerer, F Boué, L Mignot, M Krulik, B Leduc, JP Malhaire, F Morvan, C Lejeune and P Chollet.
References
- AlexopoulosCGRigatosGEfremidisAPPapacharalambousAAlexopoulosAVassilomanolakisMPatilaE1999A phase II study of the effectiveness of docetaxel (Taxotere) in women with advanced breast cancer previously treated with polychemotherapy. Hellenic Cooperative Interhospital Group in Oncology Cancer Chemother Pharmacol 44253258 [DOI] [PubMed] [Google Scholar]
- BrodowiczTKoestlerWJTomekSVaclavikIHerscoviciVWiltschkeCStegerGGZielinskiCC2000Monotherapy with docetaxel in second- or third-line treatment of anthracycline-resistant metastatic breast cancer Anticancer Drugs 11149153 [DOI] [PubMed] [Google Scholar]
- BrufmanGColajoriEGhilezanNLassusMMartoniAPerevodchikovaNToselloCViaroDZielinskiC1997Doubling epirubicin dose intensity (100 mg/m2 versus 50 mg/m2) in the FEC regimen significantly increases response rates. An international randomised phase III study in metastatic breast cancerThe Epirubicin High Dose (HEPI 010) Study GroupAnn Oncol 8155162 [DOI] [PubMed] [Google Scholar]
- CaballeroGAAismanRKQuebbemanEJ1985Long-term, ambulatory continuous IV infusion of 5-FU for the treatment of advanced adenocarcinomas Cancer Treat Rep 691315 [PubMed] [Google Scholar]
- CanyLToulouseCRavaudADurandMMauriacL1996Vinorelbine/5-FU combination in metastatic breast cancer chemotherapy. A retrospective study of 63 cases Eur J Cancer 32A370371 [DOI] [PubMed] [Google Scholar]
- ChanSFriedrichsKNoelDPinterTVan BelleSVorobiofDDuarteRGilGMBodrogiIMurrayEYelleLvon MinckwitzGKorecSSimmondsPBuzziFGonzalezMRRichardsonGWalpoleERonzoniMMurawskyMAlaklMRivaA1999Prospective randomized trial of docetaxel versus doxorubicin in patients with metastatic breast cancer. The 303 Study Group J Clin Oncol 1723412354 [DOI] [PubMed] [Google Scholar]
- ClavelMCatimelG1993Breast cancer: chemotherapy in the treatment of advanced disease Eur J Cancer 29A598604 [DOI] [PubMed] [Google Scholar]
- DegardinMBonneterreJHecquetBPionJMAdenisAHornerDDemailleA1994Vinorelbine (navelbine) as a salvage treatment for advanced breast cancer Ann Oncol 5423426 [DOI] [PubMed] [Google Scholar]
- Del MastroLVenturiniMLionettoRCarninoFGuarneriDGalloLContuAPronzatoPVesentiniLBergaglioMComisSRossoR2001Accelerated-intensified cyclophosphamide, epirubicin, and fluorouracil (CEF) compared with standard CEF in metastatic breast cancer patients: results of a multicenter, randomized phase III study of the Italian Gruppo Oncologico Nord-Ouest-Mammella Inter Gruppo Group J Clin Oncol 1922132221 [DOI] [PubMed] [Google Scholar]
- DierasVExtraJMBellissantEEspieMMorvanFPiergaJYMignotLTrescaPMartyM1996Efficacy and tolerance of vinorelbine and fluorouracil combination as first-line chemotherapy of advanced breast cancer: results of a phase II study using a sequential group method J Clin Oncol 1430973104 [DOI] [PubMed] [Google Scholar]
- French Epirubicin Study Group1991A prospective randomized trial comparing epirubicin monochemotherapy to two fluorouracil, cyclophosphamide, and epirubicin regimens differing in epirubicin dose in advanced breast cancer patients J Clin Oncol 9305312 [DOI] [PubMed] [Google Scholar]
- FroudarakisMECatimelGGuastallaJPRebattuPClavelM1998Phase II trial of navelbine and fluorouracil as second-line chemotherapy in metastatic breast carcinoma Oncology 558788 [DOI] [PubMed] [Google Scholar]
- GaspariniGCaffoOBarniSFrontiniLTestolinAGuglielmiRBAmbrosiniG1994Vinorelbine is an active antiproliferative agent in pretreated advanced breast cancer patients: a phase II study J Clin Oncol 1220942101 [DOI] [PubMed] [Google Scholar]
- HendersonICHayesDFComeSHarrisJRCanellosG1987New agents and new medical treatments for advanced breast cancer Semin Oncol 143464 [PubMed] [Google Scholar]
- LombardiDMagriMDCrivellariDSpazzapanSPaolelloCDe CiccoMDi LauroVScuderiCVeronesiA2000Combination chemotherapy with navelbine and continuous infusion of 5-fluorouracil in metastatic, chemotherapy refractory breast cancer Ann Oncol 1110411043 [DOI] [PubMed] [Google Scholar]
- MartyMExtraJMCottuPHEspieM1997Prospects with docetaxel in the treatment of patients with breast cancer Eur J Cancer 33Suppl 7S26S29 [DOI] [PubMed] [Google Scholar]
- MillerABHoogstratenBStaquetMWinklerA1981Reporting results of cancer treatment Cancer 47207214 [DOI] [PubMed] [Google Scholar]
- NabholtzJMCrownJ1998Phase III studies of single-agent docetaxel in patients with metastatic breast cancer who have progressed despite previous chemotherapy regimens: preliminary results Semin Oncol 2549 [PubMed] [Google Scholar]
- NabholtzJMSennHJBezwodaWRMelnychukDDeschenesLDoumaJVandenbergTARapoportBRossoRTrillet-LenoirVDrbalJMolinoANortierJWRichelDJNagykalnaiTSiedleckiPWilkingNGenotJYHupperetsPSPannutiFSkarlosDTomiakEMMurawskyMAlaklMRivaAAaproM1999Prospective randomized trial of docetaxel versus mitomycin plus vinblastine in patients with metastatic breast cancer progressing despite previous anthracycline-containing chemotherapy. 304 Study Group J Clin Oncol 1714131424 [DOI] [PubMed] [Google Scholar]
- RavdinPMBurrisIIIHACookGEisenbergPKaneMBiermanWAMortimerJGenevoisEBelletRE1995Phase II trial of docetaxel in advanced anthracycline-resistant or anthracenedione-resistant breast cancer J Clin Oncol 1328792885 [DOI] [PubMed] [Google Scholar]
- Ray-CoquardIBironPBachelotTGuastallaJPCatimelGMerroucheYDrozJPChauvinFBlayJY1998Vinorelbine and cisplatin (CIVIC regimen) for the treatment of metastatic breast carcinoma after failure of anthracycline- and/or paclitaxel-containing regimens Cancer 82134140 [PubMed] [Google Scholar]
- ValeroVHolmesFAWaltersRSTheriaultRLEsparzaLFraschiniGFonsecaGABelletREBuzdarAUHortobagyiGN1995Phase II trial of docetaxel: a new, highly effective antineoplastic agent in the management of patients with anthracycline-resistant metastatic breast cancer J Clin Oncol 1328862894 [DOI] [PubMed] [Google Scholar]
- ViciPDi LauroLCarpanoSAmodioAPignattiFCasaliAContiFLopezM1996Vinorelbine and mitomycin C in anthracycline-pretreated patients with advanced breast cancer Oncology 531618 [DOI] [PubMed] [Google Scholar]
- ZambettiMMarianiGDemicheliRVerderioPPotepanPGarbagnatiF2000Five-day infusion fluorouracil plus vinorelbine in women with breast cancer previously treated with anthracyclines and paclitaxel Breast Cancer Res Treat 62135139 [DOI] [PubMed] [Google Scholar]


