Abstract
Prior studies have related community violence to depression among children, but few studies have examined this relationship among adults. We hypothesized that victimization, awareness, and fear of neighborhood violence would increase the odds of depression among adult caregivers of children with asthma. We surveyed caregivers in the Baltimore Indoor Environment Study of Asthma in Kids (BIESAK), USA. The primary outcome was screening positive for depression on the Center for Epidemiological Studies Depression index. We assessed victimization, awareness, and fear of neighborhood violence, and conducted spatial analysis identifying subject homes within 500 ft of a homicide to validate survey measures of neighborhood violence. A multilevel logistic model with clustering by neighborhood estimated odds ratios and 95% confidence intervals. Survey responses about fear of neighborhood violence were strongly predicted by having a home within 500 ft of a homicide. Of 150 caregivers of children with asthma, 49% were aware of a neighborhood violent event, 36% were fearful of neighborhood violence, 22% reported victimization, and 27% had a homicide within 500 ft of the home. In our multilevel model, fear of violence increased the odds of depression by 6.7. Victimization was associated with a possible trend towards depression, and awareness of neighborhood violence did not increase the odds of depression. Based on our findings, personal experience with neighborhood violence may be more important than simple awareness. Health care workers should consider screening for depression among patients exposed to community violence.
Keywords: CES-D, Community, Inner-city, Mental health, Survey, USA
Introduction
Violence and homicide have been identified as major public health problems, particularly among minority populations (Centers for Disease Control, 1990). Homicide remains the leading cause of death among black males in the United States aged 15-54 years (Anderson & Smith, 2005). Prior to the 1990s, most research focused on the victims of violence and on homicide victims in particular. Public health research which focuses on immediate physical trauma and mortality among victims of violence, however, may overlook the more insidious health effects of community violence.
In the early 1990s, researchers began to explore the psychological effects of exposure to community violence. Depression and post-traumatic stress disorder became recognized consequences of victimization (Fitzpatrick, 1993). A subsequent study by Freeman, Mokros, and Poznanski (1993) found significantly higher depression scores among adolescents reporting violent experiences. Because depression may increase the propensity to report experience with violence, the relationship between reports of violence and depression has the potential to be biased. The lack of objective measures of violence in most prior work (Sampson, Raudenbush, & Earls, 1997; Wright et al., 2004) remains a weakness in this area of research.
Neighborhood violence may affect children with asthma in many ways. Prior studies have shown a link between proximity to violence, feeling unsafe, and worsened asthma symptoms (Swahn & Bossarte, 2006; Write & Steinbach, 2001). Importantly, neighborhood violence may worsen asthma health as a result of the impact of violence on the mental health of caregivers. Depression among inner-city caregivers of children with asthma has been linked to increased emergency department use (Bartlett et al., 2001) and worsened adherence to therapy (Bartlett et al., 2004). In a study by Wright et al. (2004), exposure to community violence worsened symptom-days among children with asthma. In that study, adjustment for caretaker negative life events, stress, and behaviors like “skipping medicines” partially attenuated the relationship between violence and asthma symptoms, but caregiver depression was not explored.
Despite evidence of the effects of community violence among children with asthma, and the possibility that caregiver depression mediates this relationship, few studies have examined how exposure to community violence impacts caregiver mental health (Sampson et al., 1997; Wright et al., 2004). We hypothesized that victimization, awareness of, and fear of neighborhood violence in the inner-city would worsen feelings of depression among caregivers of children with asthma.
Methods
Participants
We surveyed caregivers of children enrolled in the Baltimore Indoor Environment Study of Asthma in Kids (BIESAK). BIESAK is a cohort study of the relationship between environmental exposures and asthma health in young children. Caregivers of children between 2 and 6 years of age who were residents of 9 contiguous zip codes in inner-city Baltimore, Maryland, were eligible to participate. Potential participants were identified from a random sample of children with a health care encounter for asthma in the previous 12 months at Johns Hopkins Community Physicians or Bayview Pediatrics, the two centers that provide the majority of care to residents in these zip codes. A group of children without asthma were also enrolled, for purposes of comparison. Participants were recruited between September 2001 and December 2003. Recruitment has been further described elsewhere (Hansel et al., 2006). The Johns Hopkins Medical Institutional Review Board approved the study protocol.
Setting
Baltimore is a mid-Atlantic city with a 2002 population of approximately 670,000. It is highly violent; in 2001, this medium-sized city saw 256 murders and 8500 cases of aggravated assault. The annual expected number of murders in a city the size of Baltimore, calculated using the national prevalence of homicide in 2001, is 38 (Federal Bureau of Investigation, 2005). Subjects for the BIESAK study were recruited from 9 contiguous zip codes in East Baltimore, one of the poorer areas of the city (Baltimore neighborhood indicators alliance, 2005).
Measures
A questionnaire was administered to all caregivers by trained personnel. The questionnaire assessed demographics, three well-studied measures of neighborhood violence (fear, victimization, and awareness of recent violent events) (Sampson et al., 1997; Wright et al., 2004), depression, and social support. Fear was assessed by the question: “Are you afraid you will be hurt by violence in your neighborhood (all/most/some/little/none of the time)?” Because few caregivers reported fear “most of the time,” and because the difference between these categories is conceptually small, answers were dichotomized into having fear (all/more/some of the time) or no fear (little/none of the time). Victimization was measured by the question: “While you have lived in your neighborhood, has anyone ever used violence, such as a fight (hitting, pushing, shoving), against you or any member of your family anywhere in your neighborhood or home (yes/no/don’t know)?” Awareness of violence was assessed by report of any of the following in their neighborhood in the past 6 months: (1) a fight in which a weapon was used, (2) a violent argument between neighbors or friends, (3) a gang fight, (4) a robbery or mugging, (5) a murder.
Depression was assessed by the 11-item Iowa form of the Center for Epidemiological Studies Depression (CES-D) symptoms index. The Iowa form of the CES-D is a validated shortened version of the 20-item CES-D, and has been recommended over other shortened versions of the CES-D (Kohout, Berkman, Evans, & Cornoni-Huntley, 1993). Scores on each item range from 0 to 3, with higher scores representing increased depression. Scores of 8 and above were considered to represent clinically significant levels of depressive symptoms (Bartlett et al., 2001; Carpenter et al., 1998). Sensitivity of the full CES-D for 1-month prevalence of depression is 100%; specificity is 88% (Beekman et al., 1997).
Social support was assessed using the Medical Outcomes Study Social Support Survey (Sherborne & Stewart, 1991). Statements such as “I get love and affection” and “I get useful advice about important things in life” were scaled as most of the time, some of the time, or never. Analyses used both individual questions and total support scores.
For analytic purposes, neighborhoods were defined through consultation with a community representative and using the Baltimore City definitions (Baltimore City Government, 2006).
Reports of neighborhood violence
In order to corroborate survey reports of neighborhood violence, we sought an objective measure of violent events in Baltimore neighborhoods. A Uniform Crime Report coded database was provided by the Baltimore City Police Department Crime Data Analysis Unit. Using ESRI ArcGIS 9.0 geographical reference software (Environmental Systems Research Institute, Incorporated, 2004), locations of homicides for the calendar year of 2001 were geospatially referenced. Home addresses of all subjects enrolled in the study were also geocoded, and a spatial analysis was conducted to identify homes within 500 ft of a homicide (Fig. 1). Because 500 ft equals about one tenth of a mile, or one city block, we felt that homicide within 500 ft would likely represent a highly relevant neighborhood event. Caregivers are likely to have been aware of neighborhood events within a one-block radius of the home, and homicide within 500 ft of the home is more conservative than other potential measures of exposure, such as number of homicides by zip code. We then created a logistic model to determine how well having a homicide within 500 ft of the home related to participant reports of neighborhood violence.
Fig. 1.
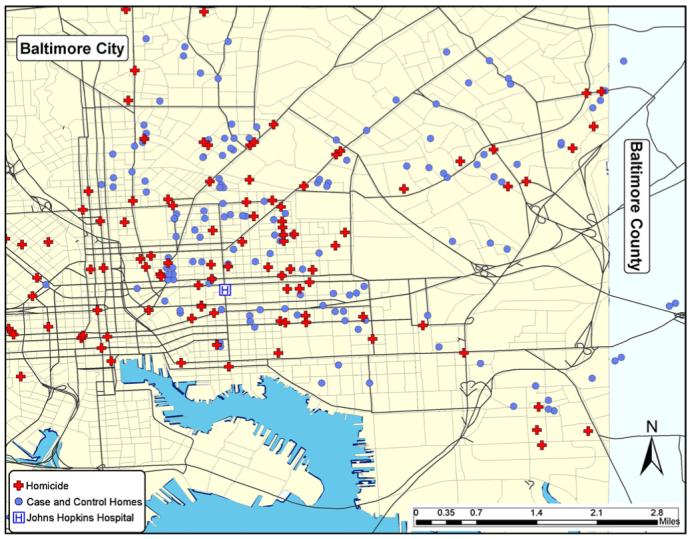
Homicide and proximity to subject homes in Baltimore, Maryland.
Descriptive analysis
We used descriptive statistics to characterize the patient sample, using proportions or means with standard deviations. Continuous variables were compared using Student’s two-tailed t test or Kruskall-Wallis test, as appropriate. Differences for categorical variables were evaluated using the Pearson’s Chi-square (χ2) or Fisher’s Exact Test. In order to determine the association between screening positive for depression and neighborhood violence, we used logistic regression to estimate the odds ratio (OR) and 95% confidence intervals using each of the three measures of neighborhood violence as dependent variables. We then performed multivariate logistic regression, adjusting for annual house-hold income, age of caregiver, and race/ethnicity. A high percentage (46%) of respondents did not report annual household income. Respondents who did not report income were more likely to have higher education and to have private insurance, but were otherwise similar to respondents who reported income. Therefore, we included a term for failure to report income, and tested terms for other SES measures (job status, education, and insurance) in our final model. We repeated the analysis among caregivers of children without asthma (control group), and with the combination of cases and controls.
Multilevel model
We tested the effect of neighborhood of residence on the relationship between violence measures and depression with two methods. We created a multilevel regression model with neighborhood-defined clusters. We repeated the analysis using generalized estimating equations (GEE) to test for cluster effects (Zeger & Liang, 1986). Sensitivity analyses were performed to test the effect of outlying influential points; re-calculated odds ratios were unchanged. Analyses were performed using STATA version 9 (Stata Corporation, 2006).
Results
Baseline characteristics
We enrolled 150 caregivers of children with asthma and 150 caregivers of children without asthma. The participants were 90% African-American, and 44% reported an annual household income below $25,000 (Table 1). Caregivers of children without asthma were similar to caregivers of children with asthma. The majority were mothers (87%) with a median age of 28 (data not shown).
Table 1.
Baseline characteristics of caregivers of children with and without asthma in Baltimore, Maryland (n = 300)
| Characteristic | Caregivers of children with asthma | Caregivers of children without asthma |
|---|---|---|
| Percentage (except where indicated) | Percentage (except where indicated) | |
| Relationship with child | ||
| Mother | 87 | 87 |
| Grandmother | 5 | 6 |
| Other caregiver | 8 | 7 |
| Age | ||
| Median (range) | 28 years (14-64 years) | 28 years (17-76 years) |
| Race/ethnicity | ||
| African-American | 91 | 89 |
| White | 5 | 7 |
| Other | 4 | 4 |
| Annual household income | ||
| Less than $25,000 | 42 | 45 |
| Educational attainment | ||
| Less than high school | 38 | 34 |
| High school graduate | 44 | 43 |
| More than high school | 18 | 23 |
Reports of neighborhood violence
Among all 300 study subjects, 67 (22%) had a homicide within 500 ft of their enrollment address in 2001 (Fig. 1). Having a homicide within 500 ft of the home increased the odds of caregiver fear of neighborhood violence [OR (95% CI): 2.2 (1.2, 3.8); p = 0.006] and awareness of a recent violent event in the neighborhood [OR (95% CI): 2.0 (1.1, 3.5); p = 0.015]. More specifically, caregivers who reported awareness of a murder in the neighborhood in the past 6 months were more than twice as likely to have had a homicide within 500 ft of the home [OR (95% CI): 2.4 (1.3, 4.5); p = 0.007]. Nearby homicide also increased the odds of a history of personal or family member victimization, but the result was not significant [OR (95% CI): 1.5 (0.8, 2.8); p = 0.18]. Limiting the analysis to only caregivers of children with asthma did not alter the direction of these findings, though in the smaller sample not all results were statistically significant (not shown).
Caregivers of children with asthma
As we were primarily interested in the effects of neighborhood violence among caregivers of children with asthma, we performed the remainder of our analyses among this group alone. Almost half (49%) of the caregivers were aware of a recent violent event in their neighborhood (Table 2). The most commonly reported recent violent event was a violent argument between neighbors (41%) and 21% knew of a murder in their neighborhood in the past 6 months (Table 2). Of those who knew of a murder, most (80%) knew of more than one murder in their neighborhood in the past 6 months. We found that 45 (30%) of 150 caregivers of children with asthma screened positive for depression. More than one-third (36%) of caregivers described being afraid that they would be hurt by neighborhood violence, whereas 33 participants (22%) reported that, while living in the neighborhood, someone had used violence against them or a member of their family.
Table 2.
Caregivers of children with asthma: awareness of recent violent events in the neighborhood
| Violent event | Percentage (n = 150) |
|---|---|
| Any violent event | 49 |
| Violent argument between neighbors | 41 |
| Fight using a weapon | 29 |
| Murder | 21 |
| Robbery or mugging | 20 |
| More than one murder | 16 |
| Gang fight | 14 |
Among those who were aware of a neighborhood violent event, 49% were afraid of neighborhood violence, and 32% had been a victim or had a family member who had been a victim of neighborhood violence. Of caregivers of children with asthma who had been victims of violence themselves or who had a family member who had been a victim of violence, 70% were afraid of violence in their neighborhood.
Being afraid of neighborhood violence was strongly associated with screening positive for depression [unadjusted OR (95% CI): 3.8 (1.8, 7.8); p < 0.001] (Table 3). A history of personal or family member victimization also increased the odds of screening positive for depression by 3.0 [unadjusted (95% CI: 1.3, 6.6; p = 0.008)]. In contrast, awareness of a recent violent event in the neighborhood was not significantly associated with screening positive for depression [unadjusted OR (95% CI): 0.9 (0.4, 1.7); p = 0.68]. Age of caregiver, income, and race/ethnicity were not related to screening positive for depression [OR = 1.01 (95% CI: 0.97, 1.05); p = 0.56 for age; OR = 0.91 (95% CI: 0.78, 1.06); p = 0.22 for income; OR = 1.11; (95% CI: 0.34, 3.70); p = 0.86 for race/ethnicity].
Table 3.
Depression and experience with violence among caregivers of children with asthma
| Screen positive for depression | |||
|---|---|---|---|
| Percentage | Unadjusted odds ratio (95% CI) | Multilevel adjusted* odds ratio (95% CI) | |
| Fear of violence (n = 54) | 48 | 3.8 (1.8, 7.8) | 6.7 (3.3, 13.5) |
| History of victimization (n = 33) | 48 | 3.0 (1.3, 6.6) | 2.1 (0.9, 5.0) |
| Awareness of violent event (n = 75) | 28 | 0.9 (0.4, 1.7) | 0.4 (0.1, 1.0) |
Adjusted for age, race, failure to report income, job status, education, insurance, other violence terms, and clustering by neighborhood.
Results of multilevel analysis
After adjusting for individual characteristics and clustering by neighborhood, being afraid of neighborhood violence remained significantly associated with screening positive for depression [OR (95% CI): 6.8 (3.2, 13.5); p < 0.001] (Table 3). History of personal or family victimization was associated with a possible trend towards screening positive for depression [OR (95% CI): 2.1 (0.9, 5.0); p = 0.08] compared to those who had no such history, although the results did not reach statistical significance. Awareness of a recent violent event in the neighborhood did not increase the odds of screening positive for depression [OR (95% CI): 0.4 (0.1, 1.0); p = 0.054].
Model testing
Although prior work has not found interactions between questionnaire-based measures of community violence (Sampson et al., 1997; Wright et al., 2004), it is conceivable that our measures of community violence might covary or interact. Nonetheless, we found no significant interaction or covariance between our measures of community violence. Homicide within 500 ft of enrollment address was not significant in our model and did not alter our results. In addition, increasing the cutoff score for the 11-item CES-D or using categorical outcomes for fear of violence did not change the magnitude or direction of our results, although some statistical power was lost (data not shown). Social support was not related to awareness, victimization, fear of neighborhood violence, or caregiver depression. Further, we found no change in the direction or magnitude of our results when measures of social support were included in the multilevel model (data not shown).
Caregivers of children without asthma
Although our primary objective was to test the effects of neighborhood violence among caregivers of children with a chronic illness, we repeated our analysis among caregivers of children without asthma (control group). Multivariate results were in the same direction and quantitatively similar to results from caregivers of children with asthma, although only the relationship between history of victimization and depression was significant in this population. After controlling for age, race, and failure to report income, fear of neighborhood violence increased the odds of screening positive for depression, although the finding was not significant [OR: 2.31 (95% CI: 0.96, 5.56); p = 0.063]. A history of victimization increased the odds of screening positive for depression [OR: 4.02 (95% CI: 1.67, 9.70); p = 0.02], while awareness of violent events in the neighborhood did not [OR: 0.89 (95% CI: 0.37, 2.14); p = 0.8].
Discussion
This study of caregivers of children with asthma found that fear of neighborhood violence increased the risk of screening positive for depression, while awareness of neighborhood violent events did not. Victimization was associated with a possible trend towards increased risk of screening positive for depression. We found high levels of depression and experience with violence in our population; 45 of 150 caregivers (30%) in our study screened positive for depression, while about 20% of the population is expected to score at or above this level (Comstock & Helsing, 1976). A large percentage (27%) of asthma subjects had a homicide within 500 ft of their home in 2001. Half (50%) of participants knew of a recent violent event in the neighborhood, and 21% knew of a recent murder. Nonetheless, awareness of a recent event did not increase the risk of screening positive for depression.
Few prior studies have included an objective measure of community violence in their analyses (Sampson et al., 1997; Wright et al., 2004). In 2001, the city of Baltimore experienced 256 homicides, many within a tenth of a mile of the front doors of our subjects. Although nearby homicide was not significant in our final model, it increased fear and awareness of neighborhood violence, as well as awareness of a neighborhood murder in our bivariate analysis. These findings suggest that asking about neighborhood violence strongly corresponds to true neighborhood events, and that community violence, not surprisingly, has concrete effects on fear of violence among adults.
Our findings have important implications for the care of inner-city children with asthma. Caregiver depression may affect ability to manage medication regimens, or to follow asthma recommendations, such as not smoking, as has been found in previous studies. For example, Bartlett et al. (2001) reported that maternal depression increased emergency department use among children with asthma. A separate study found worsened asthma symptoms among children whose caretakers exhibited higher anxiety (Silver, Warman, & Stein, 2005), while a study by Price, Bratton, and Klinnert found that pediatric asthma quality of life decreased with negative affect among caregivers (Price, Bratton, & Klinnert, 2002).
Our results are also consistent with other studies of the effects of violence on mental health among children and adults. Kliewer, Lepore, Oskin, and Johnson (1998) found that exposure to violence in the community of residence was significantly associated with intrusive thinking, anxiety, and depression among 8-12 year old children. A study of violence among sheltered homeless and low-income adult women found that being a victim of recent physical violence, including assault, was associated with a 2.64 times increased risk of symptoms of depression (95% CI: 1.4, 5.0) (Rayburn et al., 2005; Sampson et al., 1997; Wright et al., 2004). Our findings build on prior results by specifically addressing fear and awareness of neighborhood violence as well as recent victimization.
Awareness of a recent neighborhood violent event, including murder and violent argument, did not increase the risk of feeling depressed in our study. Awareness of neighborhood events may represent strong social ties or deep-rooted links to the surrounding community. Although adjusting for measures of social support did not alter our findings, prior studies have demonstrated that social ties decrease the risk of depressive symptoms among mothers (Coiro, 2001; Paarlberg et al., 1996; Panzarine, Slater, & Sharps, 1995; Small, Astbury, Brown, & Lumley, 1994) and among spousal caregivers (Cannuscio et al., 2004). One possible explanation is that caregivers who are aware of violent neighborhood events may have larger social networks, not effectively measured by the Medical Outcomes Study Social Support Survey, so that caregivers learn of violent events in the neighborhood, but are protected from depression by the stress-buffering effects of strong social ties (Kawachi & Berkman, 2001).
Awareness of a violent event may also differ from victimization or fear of violence in that the event is psychologically more distant from the subject. Fitzpatrick found that being a victim of violence but not witnessing violent acts was associated with depression among African-American youths (Fitzpatrick, 1993). We hypothesize that awareness of a violent event becomes important when it is psychologically translated into fear of violence; psychological distance may be one of the factors affecting this translation.
This study of neighborhood violence has a few relevant weaknesses. Since our study was conducted entirely in an urban setting, we cannot be sure if a similar effect of violence would be found in other residential settings or other countries. We have focused on the violent urban setting, however, because of the generally unexplained asthma disparities there (Sampson et al., 1997; Wright et al., 2004). Knowledge of one’s neighbors is generally lower in urban settings (Fischer, 1973), and social ties with neighbors are strongest among rural residents (Geis & Ross, 1998). Additionally, because our population is primarily African-American, we are unable to determine the independent impact of race/ethnicity on the effects of neighborhood violence in this study. Nonetheless, our findings are highly relevant to urban dwelling African-Americans, who are markedly affected by asthma in the United States (Mannino et al., 2002). Finally, it is important to note that depression is a complex and multifactorial illness. While we tested for the contribution of social support and other demographic factors, we were unable to include such potential contributors as stressful life events or substance use as they were not measured in our questionnaire.
In conclusion, fear of neighborhood violence increased the risk of screening positive for depression, while history of victimization was associated with a possible trend towards screening positive for depression, in this population of primarily African-American caregivers of children with asthma. Awareness of a recent violent event in the neighborhood, which may indicate strong social ties and knowledge of community events, did not increase the risk of screening positive for depression. Our findings suggest the personal experience of violence in or around the home can have a profound psychological impact on caregivers, which, based the results of prior studies, may interfere with the needed care of young children with asthma. Health care providers of urban children with asthma should be aware of these possible deleterious effects of neighborhood violence and consider asking caregivers about their own experiences, and making referrals for screening and management of caregiver depression.
Acknowledgments
The authors would like to thank Officers Troy Harris and James H. Green of the Baltimore City Police Department for their help with acquiring crime data.
References
- Anderson RN, Smith BL. Leading causes for 2002. National Vital Statistics Reports. 2005;53(17):1–90. [PubMed] [Google Scholar]
- Baltimore City Government 2006 Retrieved 24.07.06 from: Neighborhoods http://www.baltimorecity.gov/neighborhoods>.
- Baltimore neighborhood indicators alliance 2005 Retrieved er 23.10.06 from: http://www.bnia.org/about/index.html.
- Bartlett SJ, Kolodner K, Butz AM, Eggleston P, Malveaux FJ, Rand CS. Maternal depressive symptoms and emergency department use among inner-city children with asthma. Archives of Pediatrics & Adolescent Medicine. 2001;155(3):347–353. doi: 10.1001/archpedi.155.3.347. [DOI] [PubMed] [Google Scholar]
- Bartlett SJ, Krishnan JA, Riekert KA, Butz AM, Malveaux FJ, Rand CS. Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics. 2004;113(2):229–237. doi: 10.1542/peds.113.2.229. [DOI] [PubMed] [Google Scholar]
- Beekman AT, Deeg DJ, Van Limbeek J, Braam AW, De Vries MZ, Van Tilburg W. Criterion validity of the center for epidemiologic studies depression scale (CES-D): results from a community-based sample of older subjects in the Netherlands. Psychological Medicine. 1997;27(1):231–235. doi: 10.1017/s0033291796003510. [DOI] [PubMed] [Google Scholar]
- Cannuscio CC, Colditz GA, Rimm EB, Berkman LF, Jones CP, Kawachi I. Employment status, social ties, and caregivers’ mental health. Social Science & Medicine. 2004;58(7):1247–1256. doi: 10.1016/S0277-9536(03)00317-4. [DOI] [PubMed] [Google Scholar]
- Carpenter JS, Andrykowski MA, Wilson J, Hall LA, Rayens MK, Sachs B, et al. Psychometrics for two short forms of the center for epidemiologic studies - depression scale. Issues in Mental Health Nursing. 1998;19(5):481–494. doi: 10.1080/016128498248917. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control Homicide among young black males - United States, 1978-1987. Morbidity and Mortality Weekly Report. 1990;37:543–545. [PubMed] [Google Scholar]
- Coiro MJ. Depressive symptoms among women receiving welfare. Women Health. 2001;32(12):1–23. doi: 10.1300/J013v32n01_01. [DOI] [PubMed] [Google Scholar]
- Comstock GW, Helsing KJ. Symptoms of depression in two communities. Psychological Medicine. 1976;6(4):551–563. doi: 10.1017/s0033291700018171. [DOI] [PubMed] [Google Scholar]
- Environmental Systems Research Institute, Incorporated . ArcGIS 9.0. Redwood; California: 2004. [Google Scholar]
- Federal Bureau of Investigation 2005 Uniform crime reports. Retrieved 14.10.06 from: http://www.fbi.gov/ucr/ucr.htm.
- Fischer CS. On urban alienations and anomie: powerlessness and social isolation. American Sociological Review. 1973;38(3):311–326. [PubMed] [Google Scholar]
- Fitzpatrick KM. Exposure to violence and presence of depression among low-income, African-American youth. Journal of Consulting and Clinical Psychology. 1993;61(3):528–531. doi: 10.1037//0022-006x.61.3.528. [DOI] [PubMed] [Google Scholar]
- Freeman LN, Mokros H, Poznanski EO. Violent events reported by normal urban school-aged children: characteristics and depression correlates. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32(2):419–423. doi: 10.1097/00004583-199303000-00025. [DOI] [PubMed] [Google Scholar]
- Geis KJ, Ross CE. A new look at urban alienation: the effect of neighborhood disorder on perceived powerlessness. Social Psycholology Quarterly. 1998;61(3):232–246. [Google Scholar]
- Hansel NH, Rand CS, Krishnan JA, Okelo S, Breysse PN, Eggleston PA, et al. Influence of caregivers’ health beliefs and experiences on their use of environmental control practices in homes of pre-school children with asthma. Pediatric Asthma, Allergy, and Immunology. 2006;19(4):231–242. [Google Scholar]
- Kawachi I, Berkman LF. Social ties and mental health. Journal of Urban Health. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kliewer W, Lepore SJ, Oskin D, Johnson PD. The role of social and cognitive processes in children’s adjustment to community violence. Journal of Consulting and Clinical Psychology. 1998;66(1):199–209. doi: 10.1037//0022-006x.66.1.199. [DOI] [PubMed] [Google Scholar]
- Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (center for epidemiological studies depression) depression symptoms index. Journal of Aging & Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma - United States, 1980-1999. CDC Surveillance Summaries. Morbidity and Mortality Weekly Report. 2002;51(1):1–13. [PubMed] [Google Scholar]
- Paarlberg KM, Vingerhoets AJ, Passchier J, Heinen AG, Dekker GA, van Geijn HP. Psychosocial factors as predictors of maternal well-being and pregnancy-related complaints. Journal of Psychosomatic Obstetrics and Gynecology. 1996;17(2):93–102. doi: 10.3109/01674829609025669. [DOI] [PubMed] [Google Scholar]
- Panzarine S, Slater E, Sharps P. Coping, social support, and depressive symptoms in adolescent mothers. Journal of Adolescent Health. 1995;17(2):113–119. doi: 10.1016/1054-139X(95)00064-Y. [DOI] [PubMed] [Google Scholar]
- Price MR, Bratton DL, Klinnert MD. Caregiver negative affect is a primary determinant of caregiver report of pediatric asthma quality of life. Annals of Allergy, Asthma & Immunology. 2002;89:572–577. doi: 10.1016/S1081-1206(10)62104-7. [DOI] [PubMed] [Google Scholar]
- Rayburn NR, Wenzel SL, Elliott MN, Hambarsoomians K, Marshall GN, Tucker JS. Trauma, depression, coping, and mental health service seeking among impoverished women. Journal of Consulting and Clinical Psychology. 2005;73(4):667–677. doi: 10.1037/0022-006X.73.4.667. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sherborne CD, Stewart AL. The MOS social support survey. Social Science & Medicine. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Silver EJ, Warman KL, Stein REK. The relationship of caretaker anxiety to children’s asthma morbidity and acute care utilization. Journal of Asthma. 2005;42:379–383. doi: 10.1081/JAS-62999. [DOI] [PubMed] [Google Scholar]
- Small R, Astbury J, Brown S, Lumley J. Depression after child-birth: does social context matter? Medical Journal of Australia. 1994;161(8):473–477. doi: 10.5694/j.1326-5377.1994.tb127559.x. [DOI] [PubMed] [Google Scholar]
- Stata Corporation . Stata version 9. College Station; Texas: 2006. [Google Scholar]
- Swahn MH, Bossarte RM. The associations between victimization, feeling unsafe, and asthma episodes among US high-school students. American Journal of Public Health. 2006;96(5):802–804. doi: 10.2105/AJPH.2005.066514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, et al. Community violence and asthma morbidity: the inner-city asthma study. American Journal of Public Health. 2004;94(4):625–632. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RJ, Steinbach SF. Violence: an unrecognized environmental exposure that may contribute to greater asthma morbidity in high risk inner-city populations. Environmental Health Perspectives. 2001;109(10):1085–1089. doi: 10.1289/ehp.011091085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]


