Abstract
Objective
To update estimates of the associations between mental disorders and earnings from those of Rice et al. for 1985 and Harwood et al. for 1992. Current estimates, for 2002, are based on data from the National Comorbidity Survey Replication (NCS-R).
Methods
The NCS-R is a nationally representative survey of the US household population administered in 2001–03. Following the same basic approach as the prior studies, with some modifications to improve model-fitting, we predicted personal earnings in the 12 months before interview from information about 12-month and lifetime DSM-IV mental disorders among respondents ages 18–64, controlling for socio-demographics and substance disorders. We used conventional demographic rate standardization methods to distinguish predictive effects of mental disorders on amount earned by people with earnings from predictive effects on probability of having any earnings.
Results
Twelve-month DSM-IV serious mental illness (SMI) significantly predicted reduced earnings. Other 12-month and lifetime DSM-IV/CIDI disorders did not. Respondents with SMI had 12-month earnings averaging $16,306 less than other respondents with the same values on control variables ($26,435 among males; $9,302 among females), for a societal-level total of $193.2 billion. Of this total, 75.4% was due to reduced earnings among mentally ill people with any earnings (79.6% males; 69.6% females). The remaining 24.6% was due to reduced probability of having any earnings.
Conclusions
These results add to a growing body of evidence that mental disorders are associated with substantial societal-level impairments that should be taken into consideration in making decisions about the allocation of treatment and research resources.
Keywords: Economic Issues, Social and Political Issues, Burden of mental illness, costs of mental illness, quality of life
This report updates national estimates of the annual lost earnings associated with mental disorders in the US. The first such estimate, $44.1 billion in 1985, was made by Rice et al. (1) in a report commissioned by the US Public Health Service using data from the Epidemiologic Catchment Area (ECA) Study (2). This estimate was subsequently updated to $77 billion for 1992 by Harwood et al. (3) in a report commissioned by NIMH, using data from the National Comorbidity Survey (NCS) (4). The current update is based on data from the National Comorbidity Survey Replication (NCS-R) (5).
Like Rice et al. and Harwood et al., we use regression analysis to predict personal income in the last 12 months from information about DSM mental disorders, controlling socio-demographics and substance disorders. We improve on the earlier analyses, though, in four ways. First, the NCS-R assessed a wider range of disorders than the ECA or NCS. Second, the NCS-R measured personal earnings, whereas the earlier surveys measured the broader category of personal income (including unearned income). Exclusion of unearned income removes a bias in the earlier studies. Third, our estimates are more generalizable than the earlier estimates because the NCS-R is a nationally representative survey of respondents in the age range 18–64, whereas the ECA was a local survey and the NCS was restricted to ages 18–54. Fourth, the statistical analysis used here, as described below, improves on the approaches used in the earlier studies.
METHODS
Sample
The NCS-R is a nationally representative survey carried out between February 2001 and April 2003 of English-speaking householders ages 18 and older. The response rate was 70.9%. Part I of the interview included core diagnoses assessed for all respondents (n = 9282). Part II included questions about correlates and additional disorders assessed for to all respondents with any lifetime Part I disorder plus a probability subsample of other Part I respondents (n = 5692). Earnings were assessed in Part II. The 4,982 Part II respondents (2119 males, 2863 females) aged 18–64 are the focus of analysis. This sample was weighted to adjust for differential probability of selection, differential sampling into Part II, and residual discrepancies between sample and Census population socio-demographic and geographic distributions. More details on NCS-R sampling and weighting are reported elsewhere (6).
Measures
Diagnostic assessment
DSM-IV disorders were assessed with the WHO Composite International Diagnostic Interview (CIDI) Version 3.0 (7), a fully-structured lay-administered research diagnostic interview. The mental disorders assessed include anxiety disorders (panic disorder, GAD, phobias, PTSD, OCD), mood disorders (major depressive disorder, dysthymia, bipolar disorder), impulse-control disorders (oppositional defiant disorder, conduct disorder, intermittent explosive disorder, adult ADHD, eating disorders, pathological gambling disorder), and a screen for non-affective psychosis. Additional assessments were made for alcohol and illicit drug abuse and dependence. A clinical reappraisal study using the DSM-IV Axis I Disorders, Research Version, Non-patient Edition of the Structured Clinical Interview for DSM-IV (SCID) (8) found generally good concordance with CIDI diagnose (9).
We followed Harwood et al. in distinguishing 12-month DSM disorders by severity. Whereas the highest category in the Harwood et al. classification was 12-month Severe-Persistent Mental Illness (SPMI) as defined by the NIMH National Advisory Mental Health Council (10), our highest category was the broader category of Serious Mental Illness (SMI) as defined by the ADAMHA Reorganization Act (11). We used SMI because the number of NCS-R respondents with SPMI (non-affective psychosis, bipolar disorder, and severe major depression and panic disorder) was too small for sensitive analysis. SMI was considerably more prevalent (12). The latter included SPMI plus either: a 12-month suicide attempt with serious lethality intent; an impulse-control disorder with repeated serious violence; or any other disorder that resulted in 30+ days out of role in the year before interview. All other 12-month DSM-IV/CIDI disorders were included in a second category, while other lifetime disorders were a third category. Controls were included for 12-month and other lifetime DSM-IV/CIDI alcohol and illicit drug abuse with or without dependence.
Earnings
All Part II NCS-R respondents were asked to report “your own personal earnings income in the past 12 months, before taxes.” Respondents were instructed to “count only wages and other stipends from your own employment, not pensions, investments, or other financial assistance or income.” Missing values (among about 5% of respondents) were imputed using regression-based imputation with information on respondent age, sex, marital status, race-ethnicity, education, occupation, average weekly hours worked, and 2000 Census income distribution in the respondent’s Census Tract.
Socio-demographic control variables
Control variables were included for five socio-demographic variables known to predict earnings (13, 14): age at interview, sex, race-ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, Other), Census region (Northeast, Midwest, South, West), and urbanicity (Major Metropolitan Area, other urbanized areas, rural areas). Rice et al. and Harwood et al. also controlled respondent education, marital status, and number of household members. We excluded these variables, though, based on concerns about over-controlling, as previous research has shown that these variables are influenced by mental disorders (15–17).
Analysis methods
Multiple regression analysis was used to predict 12-month personal earnings from mental disorders (separate dummy variables for 12-month SMI, other 12-month DSM-IV/CIDI mental disorders, and other lifetime disorders) with controls for socio-demographics and substance disorders. As in the earlier studies, we allowed coefficients to differ for men and women and added an inflation factor to the outcome for fringe benefits. We used a 42% inflation factor based on evidence that the average fringe benefit in the US was 42% in 2002 (18).
As in earlier studies, our regression model had a nonlinear transformation of the dependent variable and used simulation based on that model to estimate effects of mental disorders on earnings. The major statistical problem in estimating such a model is that the highly skewed distribution of earnings in the US population makes ordinary least squares (OLS) regression analysis both biased and inefficient. Rice et al. addressed this problem by using weighted least squares (WLS) regression analysis. Harwood et al. addressed it by using a two-part model (19), where a Part I logistic regression model (20) predicted having any earnings and a Part II linear regression model (OLS with a logarithmic transformation of the dependent variable) predicted amount earned among respondents with any earnings. Individual-level predictions from these two models were multiplied and transformed with a correction adjustment to predict earnings for each respondent.
We used a different approach. Although two-part models have several desirable features compared to WLS regression, the multiplication and transformation of individual-level estimates is highly sensitive to model misspecification (21). Generalized linear models (GLM) (22) address this problem (23) by using pre-specified nonlinear relationships and suitably specified error structures to estimate one-part models that fit highly skewed earnings data better than two-part models (24). We consequently use GLM rather than two-part models in our analysis.
Simulation generated two estimates of predicted earnings for each respondent from the parameters in our best-fitting model, one based on the actual characteristics of the respondent and the other based on the counter-factual assumption that none of the respondents had SMI. Individual-level differences between these estimates were averaged across all respondents with SMI to estimate the mean individual-level decrease in earnings associated with SMI. This estimate was projected to the societal level by multiplying by the estimated prevalence of SMI and the size of the non-institutionalized civilian US population in the age range 18–64. Demographic rate standardization (25) was then used to decompose the societal-level estimates into components due to the effects of mental disorders on probability of having any earnings and on amount earned by those with any earnings.
Because the NCS-R sample design featured weighting and clustering, all analyses were carried out using the jackknife repeated replications (JRR) method to generate estimates of standard errors (26). In this approach, each of the models and simulations was estimated repeatedly in stratified pseudo-samples drawn from the NCS-R sample. The standard errors were calculated from the empirical distributions of results in these replications. Multivariate significance was estimated using design-adjusted χ2 tests or F tests based on JRR design-corrected coefficient variance-covariance matrices. Statistical significance was consistently evaluated using two-sided .05 level tests.
RESULTS
Variable distributions
The prevalence estimates of DSM-IV mental disorders are 6.5% for 12-month SMI, 22.6% for other 12-month disorders, and 20.3% for other lifetime disorders. (Table 1) SMI and other 12-month disorders are significantly more common among women than men (7.4% vs. 5.6%, t = 2.6, p = .008 SMI; 25.8% vs. 19.2%, t = 4.7, p < .001 other 12-month disorders), but there is no significant sex difference in other lifetime disorders (19.9% vs. 20.7%, t = 0.5, p = .59). Most respondents (86.1%) reported some personal earnings in the year before interview, although more males than females (91.6% vs. 81.1%, t = 6.4, p < .001). Among respondents with any earnings, males had a significantly higher earnings distribution than females (χ23 = 63.6, p < .001). The weighted sample distributions on socio-demographic controls were consistent with the Census population distributions by construction (6). The substance disorder distributions were consistent with those reported previously for the total NCS-R sample (12, 27).
Table 1.
Distributions of study variables
| Total | Male | Female | ||||
|---|---|---|---|---|---|---|
| % | (SD) | % | (SD) | % | (SD) | |
| I. Mental disorders | ||||||
| 12-month DSM-IV/CIDI SMI | 6.5 | (0.06) | 5.6 | (0.05) | 7.4 | (0.07) |
| Other 12-month DSM-IV/CIDI disorders | 22.6 | (0.18) | 19.2 | (0.15) | 25.8 | (0.19) |
| Other lifetime DSM-IV/CIDI disorders | 20.3 | (0.16) | 20.7 | (0.16) | 19.9 | (0.16) |
| II. Outcomes | ||||||
| Any 12-month earnings | 86.1 | (0.12) | 91.6 | (0.08) | 81.1 | (0.15) |
| Low earnings1 | 25.9 | (0.19) | 17.2 | (0.14) | 34.8 | (0.23) |
| Low-average earnings1 | 21.9 | (0.17) | 18.8 | (0.15) | 25.2 | (0.19) |
| High-average earnings1 | 29.2 | (0.21) | 31.4 | (0.22) | 26.9 | (0.20) |
| High earnings1 | 23.0 | (0.18) | 32.6 | (0.22) | 13.0 | (0.11) |
| III. Socio-demographic controls | ||||||
| Sex | ||||||
| Male | 47.9 | (0.25) | ||||
| Female | 52.1 | (0.25) | ||||
| Age | ||||||
| 18–24 | 18.3 | (0.15) | 19.2 | (0.16) | 17.5 | (0.14) |
| 25–39 | 31.8 | (0.22) | 31.7 | (0.22) | 31.9 | (0.22) |
| 40–54 | 36.0 | (0.23) | 36.0 | (0.23) | 36.1 | (0.23) |
| 55–64 | 13.9 | (0.12) | 13.1 | (0.11) | 14.6 | (0.12) |
| Race-ethnicity | ||||||
| Non-Hispanic Black | 13.0 | (0.11) | 11.6 | (0.10) | 14.3 | (0.12) |
| Non-Hispanic White | 70.0 | (0.21) | 71.1 | (0.21) | 69.0 | (0.21) |
| Hispanic | 12.3 | (0.11) | 12.7 | (0.11) | 11.8 | (0.10) |
| Other | 4.8 | (0.05) | 4.6 | (0.04) | 4.9 | (0.05) |
| Region | ||||||
| Northeast | 18.5 | (0.15) | 19.0 | (0.15) | 18.1 | (0.15) |
| Midwest | 23.1 | (0.18) | 24.0 | (0.18) | 22.3 | (0.17) |
| South | 35.7 | (0.23) | 35.2 | (0.23) | 36.2 | (0.23) |
| West | 22.6 | (0.18) | 21.8 | (0.17) | 23.4 | (0.18) |
| Urbanicity | ||||||
| Major Metro Area | 40.9 | (0.24) | 41.0 | (0.24) | 40.8 | (0.24) |
| Other urbanized area | 28.5 | (0.20) | 28.7 | (0.20) | 28.3 | (0.20) |
| Rural area | 30.6 | (0.21) | 30.3 | (0.21) | 30.9 | (0.21) |
| IV. Alcohol disorders2 | ||||||
| 12-month abuse without dependence | 2.1 | (0.02) | 3.1 | (0.03) | 1.2 | (0.01) |
| 12-month dependence | 1.6 | (0.02) | 2.2 | (0.02) | 1.1 | (0.01) |
| Other lifetime abuse without dependence | 6.8 | (0.06) | 9.8 | (0.09) | 4.0 | (0.04) |
| Other lifetime dependence | 4.6 | (0.04) | 6.7 | (0.06) | 2.7 | (0.03) |
| V. Illicit drug disorder controls2 | ||||||
| 12-month abuse without dependence | 1.2 | (0.01) | 1.9 | (0.02) | 0.5 | (0.00) |
| 12-month dependence | 0.5 | (0.00) | 0.6 | (0.01) | 0.4 | (0.00) |
| Other lifetime abuse without dependence | 4.9 | (0.05) | 7.1 | (0.07) | 2.9 | (0.03) |
| Other lifetime dependence | 3.2 | (0.03) | 4.2 | (0.04) | 2.3 | (0.02) |
| (n) | (4982) | (2119) | (2863) | |||
Significant sex difference at the .05 level, two-sided test
Earnings were divided roughly into quartiles in the subsample of respondents who had any earnings to define the earnings categories reported in this table: low earnings (<$12,700), low-average earnings (≥$12,700–<$27,500), high-average earnings (≥$27,500<$42,900) and high earnings (≥$42,900).
The four categories of alcohol disorders are mutually exclusive. The same is true of the four categories of illicit drug disorders. Respondents with a lifetime history of substance dependence who were in partial remission in the 12 months before interview were coded as having 12-month dependence. Only respondents who did not meet criteria for a 12-month disorder were eligible for classification as having a lifetime disorder. In the final models, 12-month alcohol abuse and dependence were collapsed into a single variable based on the lack of significance between the two coefficients. Twelve-month illicit drug abuse and dependence were also collapsed into a single variable, as were lifetime alcohol abuse and dependence and lifetime illicit drug abuse and dependence for the same reason. As a result, there were four rather than eight control variables included in the models for substance disorders.
Model-fitting
Seven one-part models and seven two-part models were estimated and compared. Each model included the same predictors: 12-month SMI, other 12-month mental disorders, other lifetime mental disorders, controls for socio-demographics (age, sex, race-ethnicity, region, urbanicity), controls for substance disorders, and interactions between sex and all other model variables to predict past year earnings. Differences among models all involved assumed functional forms and error structures. The seven one-part models, each of which was estimated in the total sample (i.e., including respondents with $0 earnings), included an OLS model, which assumed linear associations between the predictors and the outcome with an independent error structure, and six GLM models. The GLM models assumed one of two nonlinear functional forms of the associations between predictors and outcome (square root, logarithmic) and one of three error structures (independent, error variance proportional to the predicted value, error variance proportional to the square of the predicted value). The seven two-part models used logistic regression in Part I to predict any earnings vs. no earnings and the same set of seven models in Part II to predict amount earned among respondents with any earnings.
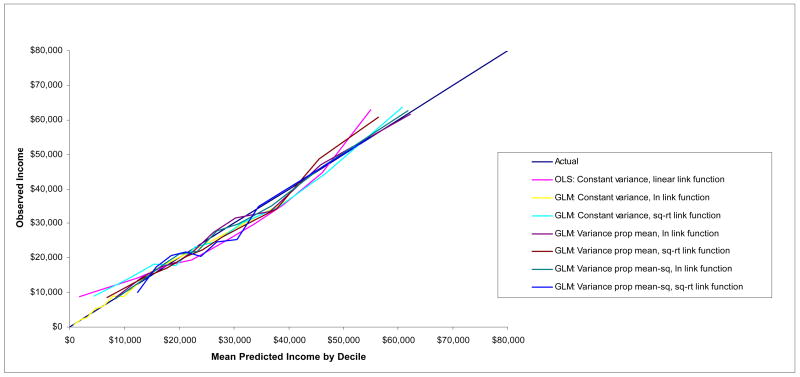
Accuracy of models was evaluated by plotting the associations between predicted mean earnings and observed mean earnings for deciles of predicted earnings. (Figure 1) Only plots for the one-part models are presented because they were clearly better than those for the two-part models. (Two-part results are available on request.) The actual decile means form a 45° line in the figure. Points on the estimator lines above or below this 45° line indicate either overestimation or under-estimation. The figure shows the OLS model does noticeably worse than the GLM models, as OLS over-estimates at both the ends of the distribution and under-estimates in the middle. Several GLM models have predicted means that fall very close to the observed means throughout the range. The best-fitting of these in terms of mean squared error assumes a logarithmic association between the predictors and the outcome and error variance proportional to the predicted value of the outcome. A number of other model-fitting tests proposed in the econometrics literature (28) also showed this to be the best-fitting model (results available on request).
Figure 1.
The associations between predicted and observed earnings (by decile of predicted earnings) based on one-part models in the total sample (n = 4982)
The individual-level predictive effects of mental disorders on earnings
We used the best-fitting GLM specification to compare predictive effects of SMI, other 12-month DSM-IV/CIDI mental disorders, and other lifetime disorders on 12-month earnings. (Table 2) The first model (M1) showed that SMI is significantly associated with reduced earnings among both males and females, while other 12-month and lifetime mental disorders are not statistically significant. Attempts to decompose the measures of other 12-month and lifetime disorders failed to find any specification where subsets of these disorders were significant. A revised model (M2) was consequently estimated that retained SMI but deleted other disorders as predictors. SMI was again significant and negative in M2.
Table 2.
Predictive income models
| Total | Males | Females | ||||
|---|---|---|---|---|---|---|
| Est1 | (95% CI) | Est1 | (95% CI) | Est1 | (95% CI) | |
| I. Model 1: Amount of earnings in the total sample | ||||||
| 12-month DSM-IV/CIDI SMI | −0.35* | (−0.57,−0.14) | −0.70* | (−0.91,−0.48) | −0.36* | (−0.57,−0.15) |
| Other 12-month DSM-IV/CIDI disorders | 0.10 | (−0.02, 0.21) | −0.06 | (−0.18, 0.07) | 0.08 | (−0.02, 0.20) |
| Other lifetime DSM-IV/CIDI disorders | 0.11 | (−0.01, 0.22) | −0.07 | (−0.18, 0.05) | 0.11 | (−0.00, 0.22) |
| II. Model 2: Amount of earnings in the total sample | ||||||
| 12-month DSM-IV/CIDI SMI | −0.40* | (−0.60,−0.20) | −0.66* | (−0.86,−0.46) | −0.42* | (−0.62,−0.22) |
| III. Model 3: Any earnings in the total sample | ||||||
| 12-month DSM-IV/CIDI SMI | 0.35* | (0.25, 0.50) | 0.16* | (0.10, 0.28 | 0.34* | (0.23, 0.51) |
| IV. Model 4: Amount of earnings among respondents with any earnings | ||||||
| 12-month DSM-IV/CIDI SMI | −0.30* | (−0.47,−0.12) | −0.56* | (−0.75,−0.37) | −0.31* | (−0.48,−0.14) |
| (n) | (4982) | (2119) | (2863) | |||
Significant at the .05 level, two-sided test
Coefficient estimates (Est) in Models I, II, and IV are based on GLM multiple linear regression models using a logarithmic link function. Coefficient estimates in Model III are based on multiple logistic regression models.
Taking M2 as our preferred model, we next evaluated whether the predictive effect of SMI on earnings varies significantly depending on substance disorders by estimating a model that included interaction terms between SMI and substance disorders. These interactions were not statistically significant either in the total sample (F4,4941 = 0.3, p = .90) or separately among males (F4,4937 = 0.3, p = .90) and females (F4,4937 = 0.4, p = .70). Additive controls for substance disorders were consequently included in the final model. The effect of SMI in M2 was then disaggregated by estimating separate models to predict having any earnings versus no earnings (M3) and to predict amount earned among respondents with any earnings (M4). Both effects were significant both among males and females. SMI was associated with significantly reduced odds of having earnings and, among those with any earnings, significantly lower earnings than among respondents without SMI.
Simulated individual-level effect estimates
Simulated mean expected annual earnings of respondents with SMI in the absence of SMI was estimated at $38,851 compared to mean observed earnings of $22,545. (Table 3) The difference, $16,306, is the estimated mean impact of SMI on earnings. This estimate is higher among males ($26,435) than females ($9,302). The simulation was repeated in the subsample of respondents with any earnings, where the adverse effect of SMI was estimated to be lower than in the total sample ($14,393 vs. $16,306). The same was true separately among males ($23,899 vs. $26,435) and females ($7,820 vs. $9,302). This difference between mean effects in the total sample and subsample reflects the fact SMI is associated not only with lower earnings among people who have earnings but also with decreased odds of having any earnings.
Table 3.
Mean expected1 2002 earnings in the absence of SMI compared to observed earnings among respondents with 12-month DSM-IV/CIDI SMI
| Total | Males | Females | ||||
|---|---|---|---|---|---|---|
| Est ($) | (SD) | Est ($) | (SD) | Est ($) | (SD) | |
| I. All respondents | ||||||
| Expected | 38,851 | (31,486) | 54,505 | (34,189) | 28,026 | (15,548) |
| Observed | 22,545 | (16,239) | 28,070 | (17,608) | 18,724 | (10,387) |
| Mean estimated impact of SMI | 16,306 | (6,846) | 26,435 | (7,175) | 9,302 | (5,547) |
| II. Respondents with earnings | ||||||
| Expected | 40,799 | (31,543) | 57,783 | (34,299) | 30,438 | (16,452) |
| Observed | 26,406 | (18,226) | 31,884 | (19,605) | 22,619 | (12,226) |
| Mean estimated impact of SMI | 14,393 | (7,190) | 23,899 | (7,479) | 7,820 | (5,737) |
| (n) | (4982) | (2119) | (2863) | |||
Based on the coefficients for the control variables in Model 2
Decomposition of the individual-level effect estimates
The lower earnings of respondents with earnings and SMI, when projected to the total sample, equals 75.4% (SD = 9.0) of the overall decrement in earning associated with SMI. This means that the remaining 24.6% is due to the lower probability of people with SMI having any earnings (in conjunction with the fact that, if they had had any earnings, they would have earned significantly less, on average, than people without SMI who were otherwise identical to them on the control variables in the model). The proportion of the total estimated effect of SMI due to lower earnings among those with any earnings is higher among males [79.6% (SD = 8.2)] than females [69.6% (SD = 12.2)].
Simulated societal-level effect estimates
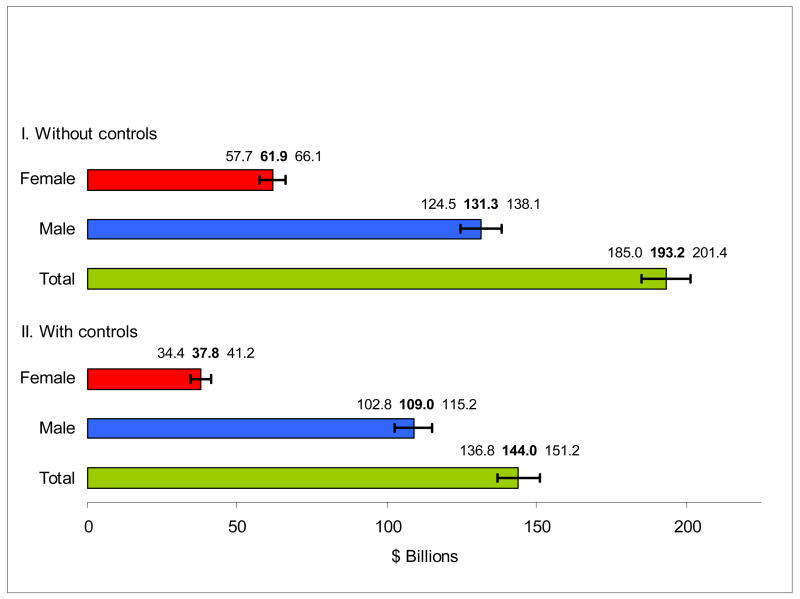
The societal-level effect of SMI was estimated by projecting the individual-level effect to the 179.6 million people ages 18–64 in the non-institutionalized civilian population of the US (29), taking into consideration the estimated prevalence of SMI and the estimated individual-level effect of SMI on earnings. (Figure 2) The estimated societal-level effect is $193.2 (SD = 55.5) billion in the total population, $131.3 (SD = 32.4) billion among males, and $61.9 (SD = 19.7) billion among females.
Figure 2.
The estimated societal-level effects (+/− two standard errors) of 12-month DSM-IV/CIDI SMI on earnings in 2002 by gender without and with controls for education, marital status, and household size
Sensitivity analysis
We replicated the simulation using three other models shown in Figure 1 to be close to the best-fitting model in reproducing the observed population income distribution: a model with a logarithmic transformation of the outcome and error variance proportional to the square of the predicted value of the outcome and two models that used a square root transformation of the outcome with error variance assumed to be either proportional to the predicted value or proportional to its square. The estimated effect sizes ranged across these models from a low of $178.1 (SD = 49.3) billion (8% lower than in the best-fitting model) to a high of $213.9 (SD = 66.6) billion (11% higher than in the best-fitting model). Roughly comparable ranges were found for estimates among males ($124.3–152.2 billion, between 5% lower and 16% higher than in the best-fitting model) and females ($56.5–65.1 billion, between 9% lower and 5% higher than in the best-fitting model).
We investigated the extent to which the estimated societal-level effect of SMI could be explained by control variables included in the earlier studies but omitted from our models: education, marital status, and household size. The estimated total-population effect of SMI on earnings decreased by approximately 25%, from $193.2 (SD= 55.5) to $144.0 (SD = 48.1) billion. The magnitude of this decrease, though, was substantially larger among females (39%) than males (17%), with the female estimate decreasing from $61.9 (SD = 19.7) billion to $37.8 (SD = 16.6) billion and the male estimate from $131.3 (SD = 32.4) billion to $109.0 (SD = 29.2) billion.
DISCUSSION
SMI was estimated to be associated with a $193.2 billion reduction in personal earnings in the total US in 2002. To put this cost in perspective, it is larger than the $145 billion economic stimulus package proposed by President Bush in January, 2008 to help avoid an economic recession in the US. Our estimate is, on the surface, much higher than the estimates reported by Rice et al. or Harwood et al. These differences can be easily explained, though, by two factors: inflation (i.e., adjusting earlier estimates to 2002 dollars) and controls for education, marital status, and household size. An inflation of the earlier estimates to 2002 dollars using Cost Compensation Trend Data from the US Department of Labor (http://www.bls.gov/ncs/ect/home.htm, accessed 1/08) makes the Rice et al. estimate $83.1 billion and the Harwood et al. estimate $107.7 billion. The Rice et al. estimate becomes higher still, closely approaching the Harwood et al. estimate, when we adjust for Rice et al. not including fringe benefits for paid sick leave or health insurance. Furthermore, when Harwood et al. estimated a revised version model that deleted education, marital status, and household size as controls, the estimated effect of mental disorders increased by a factor of 2.26, making it even larger than our estimate in 2002 dollars ($241 billion).
Irrespective of the reasons for the differences in estimates across studies, all three studies found that mental disorders are associated with massive losses of productive human capital. This finding adds to a growing body of evidence that the impaired functioning associated with mental disorders carries an enormous societal burden (30, 31), although caution is needed in not inferring causation from our associational results. Comparative cost-of-illness studies show that the magnitude of this association is high in relation to most physical disorders. For example, a recent study found that up to one-third of illness-related days out of role in the US are related to mental rather than physical disorders (31). Yet only 6.2% of all US healthcare spending is devoted to treatment of mental disorders (32) even though most people with mental disorders do not get treatment (33) and treatment is much higher for physical than mental disorders with comparable levels of impairment (30). This kind of comparative information about burden and treatment should be integrated with information about comparative treatment effectiveness to develop rational rules to guide decisions about implementation of disorder-specific screening and treatment programs and about federal healthcare research resource allocation (34).
Our results go beyond those of earlier studies in decomposing the association between SMI and low earnings into components due to having no earnings at all and, among those with any earnings, having low earnings. We found that three-fourths of the total association between SMI and earnings in the NCS-R is due to lower earnings among employed people with versus without SMI, while the remaining one-fourth is due to a lower probability of having any earnings among people with versus without SMI. The dominant influence of low earnings among people with earnings raises the possibility that appropriate policy solutions might include increased job training and vocational rehabilitation for workers with SMI and increased enforcement of the Americans with Disabilities Act with regard to corporate practices of promotion and remuneration. More detailed analysis of the data is needed, though, to understand the occupational career dynamics associated with the effects of SMI on earnings among employed people before the relevance of these and other policy implications will become clear. Further analysis is also needed to understand the determinants of the comparatively high unemployment rate among people with SMI. Although such analyses go well beyond the scope of the current report, these analyses need to be the focus of future studies in order to draw out all the policy implications related to the SMI-earnings association documented here.
This study has a number of limitations, including that mental disorders were assessed with fully-structured lay interviews rather than clinical interviews, that earnings were assessed with self-report rather than administrative records, and that a dynamic association was estimated with cross-sectional data. Another limitation is that the productive labor of women in domestic activities was not assigned a monetary value in the analysis even though it has value. As a result of this, the true financial impact of the fact that women with SMI are less likely than other women to have earnings is over-estimated to the extent that the unpaid labor of women without earnings is greater than that of women with earnings.
A technical limitation is that we applied a flat fringe benefit rate of 42% to all workers. It could be argued that the average fringe benefit rate of workers with SMI is lower than this national average because the lower paying jobs of people with SMI probably also have lower than average fringe benefit rates. We were unable to assign differentiated fringe benefits to individual NCS-R respondents because no nationally representative administrative data file exists that would allow us to do this. It should be noted, though, that the assumption of constant fringe benefits leads to a conservative bias in our estimates due to the fact that we presumably over-estimated the total compensation to workers with SMI.
Perhaps the most significant limitation of the analysis is that we were unable to adjust for the reciprocal effect of low earnings on risk of mental disorder. There is good reason to believe that such an effect exists (35). Because of this limitation, while we can state that SMI is associated with low earnings we cannot say how much of this association is due to SMI causing low earnings. Earlier studies and, indeed, virtually all cost-of-illness studies (36) have the same limitation. There is no way to correct this limitation definitively with non-experimental data. Controlling for mediating variables, such as education and marital status, which might themselves be reciprocally related to mental disorder, is not a corrective, as this can lead to over-correction. Longitudinal analysis can sometimes help. For example, a five-year longitudinal follow-up of 5000 initially employed respondents ages 18–30 in the Cardia study in four US cities found that high baseline CES-D scores significantly predicted subsequent unemployment and decreases in income even after controlling for baseline education, marital status, and history of prior unemployment (37). Even here, though, high baseline CES-D scores could have been influenced by knowledge of job insecurity that turned out to predict subsequent job loss. Sophisticated econometric models can sometimes be useful in resolving such uncertainty if information is available on third variables that influence one but not the other variable in a reciprocal pair (38), but such models are highly sensitive to misspecification (39).
Although not a limitation per se, it is also worth noting that we purposely restricted the analysis to only one component of the societal costs of mental disorder: the impact on earnings. We did not consider such other societal costs as the impact of mental illness on welfare and SSI or the workplace effects of mental illness on lost productivity. The results reported here should consequently not be considered a comprehensive estimate of all the societal costs of mental illness, but only the estimate of one component of these costs, with the caveat noted above that the $193.2 billion decrement in earnings should be seen as associated with mental illness rather than necessarily caused by mental illness.
Experimental interventions are ultimately the only reliable way to resolve this uncertainty and document causal effects of mental disorders on earnings or other indicators of role performance (40). Such interventions are comparatively rare and almost always include only relatively short-term follow-up. It is consequently important for future treatment effectiveness studies to include measures of functioning (such as measures of employment status, work productivity, and earnings) as secondary outcomes and for these studies to follow participants as long as possible in order to document long-term effects of mental disorders on functional outcomes. It is also important to note that some interventions, based on a social skills training model or an occupational rehabilitation model, might be effective in decreasing unemployment and improving job performance among people with SMI without decreasing symptoms of mental illness. It is important that interventions of this type, aimed directly at addressing the problem of low earnings, be implemented and evaluated. Controlled studies of these sorts, when combined with information about the prevalence and course of illness from epidemiological studies, are our greatest hope of obtaining more definitive data than presented here about the effects of mental disorders of earnings and other aspects of functioning.
Footnotes
Disclosure: Professor Kessler has been a consultant for Astra Zeneca, BristolMyersSquibb, Eli Lilly and Co, GlaxoSmithKline, Pfizer, Sanofi-Aventis, and Wyeth and has had research support for his epidemiological studies from BristolMyersSquibb, Eli Lilly and Company, Ortho-McNeil, Pfizer, and the Pfizer Foundation. The remaining authors report no competing interest.
References
- 1.Rice DP, Kelman S, Miller LS, Dunmeyer S. The Economic Costs of Alcohol and Drug Abuse and Mental Illness: 1985. Rockville, MD: National Institute on Drug Abuse; 1990. [Google Scholar]
- 2.Robins LN, Regier DA, editors. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, NY: The Free Press; 1991. [Google Scholar]
- 3.Harwood H, Ameen A, Denmead G, Englert E, Fountain D, Livermore G. Report to National Institute of Mental Health. Falls Church, VA: Lewin Group; 2000. The Economic Cost of Mental Illness, 1992. [Google Scholar]
- 4.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13:60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, Jin R, Pennell BE, Walters EE, Zaslavsky A, Zheng H. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 9.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, Lepine JP, Mazzi F, Reneses B, Vilagut G, Sampson NA, Kessler RC. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006;15:167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Advisory Mental Health Council. Health care reform for Americans with severe mental illnesses: report of the National Advisory Mental Health Council. Am J Psychiatry. 1993;150:1447–1465. doi: 10.1176/ajp.150.10.1447. [DOI] [PubMed] [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration. Final notice establishing definitions for (1) children with a serious emotional disturbance, and (2) adults with a serious mental illness. Fed Regist. 1993;58:29422–29425. [Google Scholar]
- 12.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bowles S, Gintis H, Osborne M. The determinants of earnings: a behavioral approach. J Econ Lit. 2001;39:1137–1176. [Google Scholar]
- 14.Goldsmith AH, Veum JR, Darity JW. The impact of psychological and human capital on wages. Econ Inq. 1997;35:815–829. [Google Scholar]
- 15.Forthofer MS, Kessler RC, Story AL, Gotlib IH. The effects of psychiatric disorders on the probability and timing of first marriage. J Health Soc Behav. 1996;37:121–132. [PubMed] [Google Scholar]
- 16.Kessler RC, Foster CL, Saunders WB, Stang PE. Social consequences of psychiatric disorders, I: Educational attainment. Am J Psychiatry. 1995;152:1026–1032. doi: 10.1176/ajp.152.7.1026. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, Walters EE, Forthofer MS. The social consequences of psychiatric disorders, III: probability of marital stability. Am J Psychiatry. 1998;155:1092–1096. doi: 10.1176/ajp.155.8.1092. [DOI] [PubMed] [Google Scholar]
- 18.Bureau of Labor Statistics. 2005 Employer costs for employee compensation – March 2005. United States Department of Labor News; Washington, DC: 2005. [Google Scholar]
- 19.Duan N, Manning WG, Morris CN, Newhouse JP. Choosing between the sample-selection model and the multi-part model. J Bus Econ Stat. 1984;2:283–289. [Google Scholar]
- 20.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2. New York, NY: Wiley & Son; 2001. [Google Scholar]
- 21.Manning WG. The logged dependent variable, heteroscedasticity, and the retransformation problem. J Health Econ. 1998;17:283–295. doi: 10.1016/s0167-6296(98)00025-3. [DOI] [PubMed] [Google Scholar]
- 22.McCullagh P, Nelder JA. Generalized Linear Models. 2. London: Chapman and Hall; 1989. [Google Scholar]
- 23.Mullahy J. Much ado about two: reconsidering the two-part model in health econometrics. J Health Econ. 1998;17:247–281. doi: 10.1016/s0167-6296(98)00030-7. [DOI] [PubMed] [Google Scholar]
- 24.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 25.Schempf A, Becker S. On the application of decomposition methods. Am J Public Health. 2006;96:1899. doi: 10.2105/AJPH.2006.094789. author reply 1899–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wolter KM. Introduction to Variance Estimation. New York: Springer-Verlag; 1985. [Google Scholar]
- 27.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 28.Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. 2004;23:525–542. doi: 10.1016/j.jhealeco.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Census Bureau. Table 2: Annual Estimates of the Population by Selected Age Groups and Sex for the United States: April 1, 2000 to July 1, 2006. Washington, DC: U.S. Census Bureau; 2006. [Google Scholar]
- 30.Druss BG, Hwang I, Petukhova M, Sampson NA, Wang PS, Kessler RC. Impairment in role functioning in mental and chronic medical disorders in the United States: results from the National Comorbidity Survey Replication. Mol Psychiatry. doi: 10.1038/mp.2008.13. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Merikangas KR, Ames M, Cui L, Stang PE, Ustun TB, Von Korff M, Kessler RC. The impact of comorbidity of mental and physical conditions on role disability in the US adult household population. Arch Gen Psychiatry. 2007;64:1180–1188. doi: 10.1001/archpsyc.64.10.1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.U.S. Department of Health and Human Services. National Expenditures for Mental Health Services and Substance Abuse Treatment, 1993–2003. Washington, DC: Substance Abuse and Mental Health Services Administration; 2007. [Google Scholar]
- 33.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 34.Wilson EC, Rees J, Fordham RJ. Developing a prioritisation framework in an English Primary Care Trust. Cost Eff Resour Alloc. 2006;4:3. doi: 10.1186/1478-7547-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Costello EJ, Compton SN, Keeler G, Angold A. Relationships between poverty and psychopathology: a natural experiment. JAMA. 2003;290:2023–2029. doi: 10.1001/jama.290.15.2023. [DOI] [PubMed] [Google Scholar]
- 36.Hu TW. Perspectives: an international review of the national cost estimates of mental illness, 1990–2003. J Ment Health Policy Econ. 2006;9:3–13. [PubMed] [Google Scholar]
- 37.Whooley MA, Kiefe CI, Chesney MA, Markovitz JH, Matthews K, Hulley SB. Depressive symptoms, unemployment, and loss of income: The CARDIA Study. Arch Intern Med. 2002;162:2614–2620. doi: 10.1001/archinte.162.22.2614. [DOI] [PubMed] [Google Scholar]
- 38.Ettner SL, Frank RG, Kessler RC. The impact of psychiatric disorders on labor market outcomes. Ind Labor Relat Rev. 1997;51:64–81. [Google Scholar]
- 39.Bound J, Jaeger DA, Baker RM. Problems with instrumental variables estimation when the correlation between the instruments and the endogenous explanatory variables is weak. J Am Stat Assoc. 1995;90:443–450. [Google Scholar]
- 40.Wang PS, Simon GE, Avorn J, Azocar F, Ludman EJ, McCulloch J, Petukhova MZ, Kessler RC. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA. 2007;298:1401–1411. doi: 10.1001/jama.298.12.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]