Abstract
Background
In 2003, US Centers for Disease Control and Prevention (CDC) announced an HIV prevention initiative that emphasized increasing the proportion of persons living with HIV who are aware of their positive serostatus. Previously, CDC set a national HIV prevention goal of reducing new infections by 50% by 2005, with increasing serostatus awareness a central goal. The objectives of this article are to examine the national epidemiologic consequences of increasing serostatus awareness and the important question of how far increasing awareness could lead toward achieving CDC’s goal of a 50% reduction in incident infections.
Methods
Scenario analysis methods were used to project incident HIV infections over 1- and 10-year time horizons at varying levels of HIV seropositivity awareness. Because HIV transmission rates are several times higher for those who are unaware of their HIV seropositivity than for those who are aware, we modeled the effects of increasing awareness via HIV counseling and testing and moving people from the higher to the lower transmission category.
Results
Increasing awareness of HIV seropositivity via HIV counseling and testing in the United States from a baseline 75% to 95% has the potential of reducing new infections by as much as 32% in a single year. Achieving the national goal of 50% reduction seems out of reach, however.
Conclusions
Reduction of new infections by 50% in the United States requires a combination of prevention services to reduce further the already low HIV transmission rate from persons aware of their HIV seropositivity and HIV risk reduction interventions for at-risk persons. Counseling and testing alone seems insufficient to meet the 50% incidence reduction goal.
Keywords: AIDS, awareness, HIV, scenario analysis, serostatus
US Centers for Disease Control (CDC) estimates that the annual HIV incidence in the United States has been approximately 40,000 infections per year since approximately 1990.1,2 In January 2001, CDC set out a national plan with an overarching goal to reduce new infections by 50% by 2005.2 Unfortunately, the annual incidence level has remained stable. A key subgoal of the 2001 CDC plan was to increase to 95% the proportion of persons living with HIV (PLWH) who knew of their infection.2 CDC currently estimates that approximately 75% of PLWH know their serostatus.3,4 In 2003, CDC released its Advancing HIV Prevention Initiative, putting a major emphasis on increasing knowledge of HIV seropositivity via HIV counseling and testing as well as on prevention interventions for PLWH.5
Recent studies have examined the cost-effectiveness of expanding screening for HIV infection to increase the proportion of PLWH who are aware of their serostatus.6,7 One study examined sexual transmission from HIV-seropositive persons aware of their serostatus relative to unaware persons; the study briefly noted the possible impact of perfect awareness over a 1-year time horizon on HIV sexual transmission.8 To our knowledge, however, no study has comprehensively examined the national epidemiologic consequences over a multiyear time horizon of increasing serostatus awareness at various levels or the important question of how far increasing awareness could lead toward achieving CDC’s goal of a 50% reduction in incident infections. These are the issues we examine in this article.
METHODS
The present study used scenario analysis to estimate the number of new HIV infections over 1- and 10-year time horizons at varying levels of HIV seropositivity awareness ranging from the current level of 75% through 100% (paying special attention to CDC’s targeted level of 95%). The epidemiologic impact of increasing serostatus awareness among PLWH depends on the relative proportions of incident infections that are attributable to the transmission risk behaviors of persons who are aware of their serostatus versus those who are unaware.
CDC recently published a model that yields an estimate of the percentage of HIV incident cases attributable to sexual transmission stratified by HIV serostatus awareness of the transmitting partner.8 The model mathematically combines information about the number of persons living with HIV who are aware and unaware of their serostatus, the impact of awareness on HIV-related risk behaviors, the effect of awareness on viral load, and the background prevalence of risk behaviors and HIV seroprevalence.8 CDC authors estimate that transmission from persons living with HIV who are unaware of their serostatus accounts for approximately 54% of the estimated 32,000 sexually acquired HIV infections each year if the number of at-risk unprotected sex partners is the same among those who are aware of their HIV seropositivity as among those who are unaware. Should the ratio of at-risk partners be 2:1 (ie, double the number for persons unaware of their HIV seropositivity relative to persons aware), however, the percentage of new cases of sexual transmission from persons unaware of their seropositivity climbs to 70%. The authors of this study emphasize that little is known about this ratio, and they use 54% as their base case estimate. A previous estimate by CDC suggests that a similar proportion, 55%, of the overall annual total of 40,000 incident infections (including sexually and nonsexually transmitted infections) is the result of transmissions from persons unaware of their serostatus.9 Given the close similarity between CDC’s estimates of 54% and 55%,8,9 we use 55% in our analyses here and assume that this percentage is the same for sexual and drug injection transmission of HIV.
The annual HIV transmission rate in the United States (ie, the number of secondary infections per year per person living with HIV) is approximately 4% (40,000 new infections for 1 million PLWH).8-11 Assuming that 55% or 22,000 of the 40,000 new infections that occur in the United States each year are from persons who are unaware of their serostatus implies an HIV transmission rate of 22,000 per 250,000 (8.8%) for the 250,000 persons who are unaware of their seropositivity and a transmission rate of 18,000 per 750,000 (2.4%) for PLWH who have received HIV counseling and testing and thereby know their serostatus.8-11
This article examines the HIV prevention benefits of increasing provision of voluntary HIV counseling and testing, with the expectation that as persons learn their HIV seropositivity, they move from the higher to the lower transmission rate category. The analyses consider the effects of increasing the serostatus awareness rate for a single year and the long-term impact of this 1-time increase, assuming that serostatus awareness is maintained at the higher level.
One-Year Time Horizon Analysis
We assumed at baseline that there are roughly 40,000 new infections per year in the United States.1,2,8-11 We estimate that there are approximately 1 million PLWH in the United States, approximately 75% of whom know their serostatus.3,4,8-12 We assume that as PLWH become aware of their seropositivity via the receipt of HIV counseling and testing services, they move from the higher to the lower transmission rate category. These parameter values are sufficient to allow an estimate to be made of the number of new HIV infections at any given level of HIV seropositivity awareness: New Infections = TRaware·x·N+TRunaware·(1 - x)·N, where N is the number of persons living with HIV, x is the proportion of PLWH who know their serostatus, and TRaware and TRunaware are the respective HIV transmission rates.
Ten-Year Analysis
Years 2 through 10 of our scenario analysis proceed much as the year 1 analysis with the following additions. At the beginning of each year, we take the number of PLWH from the previous year and then (1) add the number of new infections from the previous year and (2) subtract the number of deaths from the previous year. The annual death rate was estimated using each of 3 different sources: (1) the general population death rate for the year 2000 (0.87%),13 (2) the HIV-specific death rate across the years 2000 through 2002 (1.83%),12 and (3) the sum of these 2 death rates. The general population death rate is likely a lower bound on the actual death rate for this population of PLWH, and the combination death rate is likely an upper bound. These calculations yield a death rate-specific and awareness level-specific estimate of the number of PLWH at the beginning of a given year. Calculations analogous to the year 1 analyses are used to estimate the number of new HIV infections during the course of that year, based on the HIV transmission rates for persons who are aware or unaware of their serostatus.
RESULTS
Year 1 Analysis
Table 1 displays the number of new HIV infection in year 1 at various seropositivity awareness levels and the percentage reduction in new infections at increasingly higher awareness levels. It is seen that raising awareness from the baseline value of 75% to 95% would reduce new infections by 32%. Achievement of a 50% reduction in new infections seems unlikely, however; increasing serostatus awareness to 100% produces only a 40% reduction in incidence.
TABLE 1.
Percentage Reduction in New HIV Infections at Varying Levels of Awareness of HIV Seropositivity: 1-Year Analysis Results
| Level of HIV Seropositivity Awareness | No. New HIV Infections (1 year) | Percentage Reduction |
|---|---|---|
| 75% | 40,000 | Not applicable |
| 80% | 36,800 | 8% |
| 85% | 33,600 | 16% |
| 90% | 30,400 | 24% |
| 95%* | 27,200 | 32% |
| 100% | 24,000 | 40% |
Indicates target level of 95% HIV seropositivity awareness from CDC national HIV prevention plan.
Ten-Year Analysis
Table 2 displays the results of the 10-year analysis. Results are shown at each of the 3 specified death rates and for the baseline 75% awareness level and the target 95% awareness level. Under no scenario is a reduction to 20,000 new infections per year achieved. Over 10 years, if no improvement is made in HIV seropositivity awareness, the number of new infections per year is likely to increase to between 44,931 and 52,787 incident infections. Even ifawareness is increased to 95%, the number of new infections per year does not continue to decline over time; in fact, it increases slightly from the year 1 levels to between 27,249 and 32,079 incident infections by year 10. Figure 1 displays this finding graphically and includes the intermediate awareness level of 85% (this figure assumes an AIDS-specific death rate). As shown, at an 85% awareness level, incidence climbs to greater than 38,500 within 10 years, nearly offsetting the 16% incidence reduction seen in year 1.
TABLE 2.
Ten-Year Projections of New HIV Infections at Baseline (75%) and Target (95%) Levels of Awareness of HIV Seropositivity by Varying Annual Death Rates
| Death Rate | Awareness Level | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Year 6 | Year 7 | Year 8 | Year 9 | Year 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| General population | 75% | 40,000 | 41,252 | 42,543 | 43,875 | 45,248 | 46,664 | 48,125 | 49,631 | 51,185 | 52,787 |
| General population | 95% | 27,200 | 27,703 | 28,216 | 28,738 | 29,269 | 29,811 | 30,362 | 30,924 | 31,496 | 32,079 |
| HIV-specific | 75% | 40,000 | 40,868 | 41,755 | 42,661 | 43,587 | 44,533 | 45,499 | 46,486 | 47,495 | 48,526 |
| HIV-specific | 95% | 27,200 | 27,442 | 27,686 | 27,933 | 28,181 | 28,432 | 28,685 | 28,940 | 29,198 | 29,458 |
| Combined | 75% | 40,000 | 40,520 | 41,047 | 41,580 | 42,121 | 42,669 | 43,223 | 43,785 | 44,354 | 44,931 |
| Combined | 95% | 27,200 | 27,205 | 27,211 | 27,216 | 27,222 | 27,227 | 27,233 | 27,238 | 27,244 | 27,249 |
FIGURE 1.
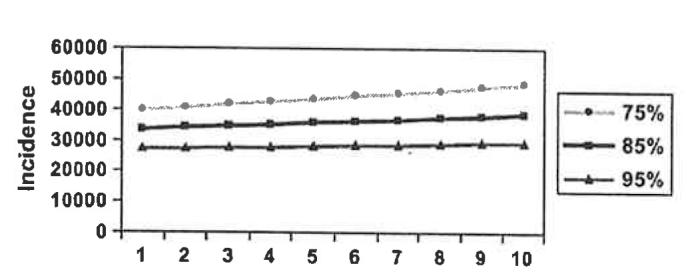
Annual HIV incidence over 10-year time horizon at 75%, 85%, and 95% serostatus awareness levels.
DISCUSSION AND CONCLUSIONS
The scenario analyses presented here indicate that the provision of HIV counseling and testing to increase the awareness of HIV seropositivity may substantially reduce new HIV infections—perhaps by nearly one third if a target level of 95% awareness is achieved. Although impressive, this reduction would not by itself achieve the national goal of reducing new HIV infections by 50% to 20,000 per year. Our estimate of a 40% overall incidence reduction with perfect awareness is slightly larger than CDC’s estimate of a 31% reduction in sexually transmitted HIV infections with perfect awareness.8
Of course, there are limitations to this study. We note that the transmission rate for persons newly learning their HIV seropositivity might not drop to as low as 2.4%. Persons now unaware of their HIV seropositivity seem likely to have less access to the health care system (compared with persons already availing themselves of HIV counseling and testing). We speculate that this lessened access could be a function of higher levels of homelessness, substance use, mental illness, and other factors. Even after someone is made aware of his or her HIV seropositivity, such factors might persist and serve to keep the HIV transmission rate higher than for persons who already have accessed HIV counseling and testing services.
Another limitation of this study is that there is uncertainty in some of the input parameters, including the baseline incidence and prevalence of HIV in the United States. It has been noted elsewhere that much more precise measures of incidence and prevalence are needed.14 CDC’s estimate of the proportion of new infections that are attributable to persons unaware of their HIV seropositivity contains uncertainty.8-11 Additional empiric examination is needed of our assumption that the percentage of transmission from persons unaware that they are living with HIV (relative to persons who are aware) is the same for sexual and drug injection transmission of HIV. We would assert that the precise numbers in our results are not the most important feature of this analysis; rather, the general qualitative conclusions are more important and reliable.
In conclusion, our analyses indicate that achievement of the national goal of reducing new infections by 50% in the United States requires more than simply increasing awareness of HIV seropositivity via counseling and testing. It also requires a combination of prevention services for the few PLWH at continued risk of transmission, HIV prevention services for high-risk HIV-seronegative persons, the use of biomedical interventions (eg, microbicides) as they become available, and structural interventions to set a context in which effective HIV prevention can occur. The optimal mix of HIV prevention interventions, of course, depends on the relative costs and impact of these services.
Acknowledgments
Partially supported by the Emory University Center for AIDS Research (D. R. Holtgrave) and by National Institute of Mental Health Center grant P30-MH52776 awarded to the Center for AIDS Intervention Research (S. D. Pinkerton).
REFERENCES
- 1.Karon JM, Fleming PL, Steketee RW, et al. HIV in the United States at the turn of the century; an epidemic in transition. Am J Public Health. 2001;91:1060–1068. doi: 10.2105/ajph.91.7.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention . HIV Prevention Strategic Plan Through 2005. CDC, 2001; Atlanta, GA: [Google Scholar]
- 3.Fleming PL, Byers RH, Sweeney PA, et al. HIV prevalence in the United States, 2000; Presented at: Ninth Conference on Retroviruses and Opportunistic Infections; Seattle, WA. Feb 24-28, 2002; [Last accessed December 3, 2006]. Available at: http://www.retroconference.org/2002/Abstract/13996.htm. [Google Scholar]
- 4.Glynn MK, Rhodes P. Estimated HIV prevalence in the United States at the end of 2003 [abstract T1-B1101]; Presented at: 2005 National HIV Prevention Conference; Atlanta. 2005. [Google Scholar]
- 5.Centers for Disease Control and Prevention Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:329–332. [PubMed] [Google Scholar]
- 6.Paltiel AD, Weinstein MC, Kimmel AD, et al. Expanded screening for HIV in the United States—an analysis of cost-effectiveness. N Engl J Med. 2005;352:586–595. doi: 10.1056/NEJMsa042088. [DOI] [PubMed] [Google Scholar]
- 7.Sanders GD, Bayoumi AM, Sundaram V, et al. Cost-effectiveness of screening for HIV in the era of highly active antiretroviral therapy. N Engl J Med. 2005;352:570–585. doi: 10.1056/NEJMsa042657. [DOI] [PubMed] [Google Scholar]
- 8.Marks G, Crepaz N, Janssen RS. Estimating the sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20:1447–1450. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- 9.Cleveland J. Future of HIV prevention; Presented at: National Alliance of State and Territorial AIDS Directors; Washington, DC. 2005. [Google Scholar]
- 10.Holtgrave DR. Estimation of annual HIV transmission rates in the United States, 1978-2000. J Acquir Immune Defic Syndr. 2004;35:89–92. doi: 10.1097/00126334-200401010-00013. [DOI] [PubMed] [Google Scholar]
- 11.Holtgrave DR, Anderson T. Utilizing HIV transmission rates to assist in prioritizing HIV prevention services. Int J STD AIDS. 2004;15:789–792. doi: 10.1258/0956462042563639. [DOI] [PubMed] [Google Scholar]
- 12.Holtgrave DR. Causes of the decline in AIDS deaths, United States, 1995-2002; prevention, treatment or both? Int J STD AIDS. 2005;16:777–781. doi: 10.1258/095646205774988109. [DOI] [PubMed] [Google Scholar]
- 13.US Census Bureau . Statistical Abstract of the United States: 2002. US Census Bureau; Washington, DC: 2002. Table 94: deaths and death rates by sex and race: 1970 to 2000; p. 74. [Google Scholar]
- 14.Institute of Medicine . No Time to Lose: Getting More from HIV Prevention. National Academy Press; Washington, DC: 2001. [PubMed] [Google Scholar]


