Abstract
We assessed the safety, tolerability and efficacy of the immunomodulatory drug, CC-5013 (REVIMID™), in the treatment of patients with metastatic malignant melanoma and other advanced cancers. A total of 20 heavily pretreated patients received a dose-escalating regimen of oral CC-5013. Maximal tolerated dose, toxicity and clinical responses were evaluated and analysis of peripheral T-cell surface markers and serum for cytokines and proangiogenic factors were performed. CC-5013 was well tolerated. In all, 87% of adverse effects were classified as grade 1 or grade 2 according to Common Toxicity Criteria and there were no serious adverse events attributable to CC-5013 treatment. Six patients failed to complete the study, three because of disease progression, two withdrew consent and one was entered inappropriately and withdrawn from the study. The remaining 14 patients completed treatment without dose reduction, with one patient achieving partial remission. Evidence of T-cell activation was indicated by significantly increased serum levels of sIL-2 receptor, granulocyte–macrophage colony-stimulating factor, interleukin-12 (IL-12), tumour necrosis factor-α and IL-8 in nine patients from whom serum was available. However, levels of proangiogenic factors vascular endothelial growth factor and basic foetal growth factor were not consistently affected. This study demonstrates the safety, tolerability and suggests the clinical activity of CC-5013 in the treatment of refractory malignant melanoma. Furthermore, this is the first report demonstrating T-cell stimulatory activity of this class of compound in patients with advanced cancer.
Keywords: phase I, CC-5013, thalidomide, immunomodulation, cytokines, T-cell activation
CC-5013 is in development for the treatment of a variety of oncological and inflammatory diseases. The first available immunomodulatory drug (IMiD), Thalomid® (thalidomide), is approved for the treatment of the cutaneous manifestations of moderate to severe erythema nodosum leprosum (ENL). Thalidomide has also been shown to be a useful drug in a wide range of other clinical conditions for which there is little other treatment option (Marriott et al, 1999; Raje and Anderson, 1999). These include rheumatoid arthritis (Schuler and Ehninger, 1995), the inflammatory and wasting effects of chronic tuberculosis (Klausner et al, 1996), Behcet’s disease (Hamuryudan et al, 1998), Crohn’s disease (Wettstein and Meagher, 1997; Ehrenpreis et al, 1999; Vasiliauskas et al, 1999) aphthous ulcers (Youle et al, 1989; Alexander and Wilcox, 1997; Jacobson et al, 1997), cachexia (wasting) associated with HIV infection (Sharpstone et al, 1995; Reyes-Teran et al, 1996) and AIDS-related Kaposi’s sarcoma (Fife et al, 1998). There is also a wide body of evidence from large-scale clinical trials showing the effectiveness of thalidomide as a treatment for refractory or relapsed multiple myeloma (MM) (Singhal et al, 1999; Hideshima et al, 2000; Juliusson et al, 2000; Kneller et al, 2000; Zomas et al, 2000), and this extends to the treatment of a number of other tumours (Eisen et al, 2000; Fine et al, 2000; Gutheil and Finucane, 2000; Patt et al, 2000; Tseng et al, 2001; Eisen, 2002).
Immunomodulatory drug analogues are able to costimulate T cells (Haslett et al, 1998; Corral et al, 1999) and are highly antiangiogenic (Dredge et al, 2002a). The ability to costimulate T cells has been associated with an increased Th1-type cytokine response and suggests that in certain clinical settings, IMiD analogues are likely to act as adjuvants to promote T-cell responses, thereby contributing to antitumour activity in vivo. In this regard, IMiDs have been shown to augment antitumour responses in vivo, leading to long-term protection from tumour challenge (Dredge et al, 2002b). Antiangiogenic activity has provided the rationale for the use of this class of compound as anticancer agents and, although unproven, this has often been linked to thalidomide's teratogenicity. However, the lead IMiD, CC-5013, has been shown to be both nonteratogenic and antiangiogenic in animal models.
The clinical development of the IMiDs has been initiated with the use of CC-5013 in MM (Marriott et al, 2001; Richardson et al, 2001; Zangari et al, 2001). This compound has recently completed a phase I clinical trials programme in which it was found to be safe and well tolerated. Furthermore, a report of clinical efficacy of CC-5013 in MM patients has recently been published (Richardson et al, 2002), although T-cell costimulation has not been demonstrated in vivo. We therefore conducted a phase 1 study of CC-5013 in patients with metastatic malignant melanoma with treatment administered according to an accelerated titration design with intrapatient dose escalation (modified from Simon et al, 1997). This disease has a median survival of 6–9 months and current systemic therapy can induce complete durable responses in only a small minority of patients (Atkins, 1997). Current chemotherapeutic options offer a very poor response rate of 14–20% and immunotherapy, for example interleukin (IL)-2 and interferon-α (IFN-α) have produced good responses in only a small number of patients.
In this study, we have assessed the safety, tolerability and clinical effects of CC-5013 during the treatment of 20 patients with metastatic malignant melanoma and other advanced cancers (Table 1 ). We have also sought evidence of immunostimulatory and antiangiogenic effects by assessing multiple serological factors and changes in peripheral blood T-cell markers.
Table 1. Patient details: possible/probable CC-5013-related adverse effects.
| Patient no. | Age (years)/sex | Disease | Stagea | Site | Previous treatment | Responseb | Completed/withdrew | Days on study/maximum dose (mg) | Samples for in vitro analysis |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 45/F | Malignant melanoma | IVabc | Right ileoinguinal area | Cancervax trial | PD | Completed | 28/50 | No |
| 2 | 28/F | Malignant melanoma | IVabc | Right thigh | Dacarbazine (three cycles); peptides (melanA, gp100, tyrosinase) and IL-2 | SD; partial response of liver | Completed | 28/50 | No |
| 3 | 58/M | Malignant melanoma | IVabc | Lower abdomen | Dacarbazine; radiotherapy | PD | Progressed | 14/10 | No |
| 4 | 44/F | Malignant melanoma | IVa | Abdomen | Adjuvant interferon | SD; minor response of abdominal nodes | Completed | 28/50 | No |
| 5 | 16/M | Malignant melanoma | IVac | Right temporal region | Adjuvant interferon | PD; minor response of small cutaneous lesion | Completed | 28/50 | No |
| 6 | 56/F | Malignant melanoma | IVabc | Vulva | Chemotherapy; bilateral groin radiotherapy | SD | Completed | 28/50 | No |
| 7 | 31/M | Malignant melanoma | IVabc | Left upper chest | Debulking surgery; peptide (triple) and IL-2; dacarbazine; vindesine X3 | SD; minor response of subcutaneous lesion | Completed | 28/50 | Yes |
| 8 | 80/M | Malignant melanoma | IVab | Right side of neck | Treosulphan (six cycles) | PD | Completed | 28/50 | Yes |
| 9 | 48/M | Malignant melanoma | IVa | Left foot | BCG (two doses) | SD; minor response of cutaneous nodules | Completed | 28/50 | Yes |
| 10 | 56/F | Malignant melanoma | IVac | Breast | Vinflunine; radiotherapy | PD | Completed | 28/50 | No |
| 11 | 23/M | Malignant melanoma | IVabc | Abdomen | Adjuvant interferon; radical radiotherapy | PD | Progressed | 24/50 | Yes |
| 12 | 51/M | Malignant melanoma | IVac | Right thigh | Carboplatin, dacarbazine, vincristine, vinblastine & vindesine | SD | Completed | 28/50 | Yes |
| 13 | 64/M | Malignant melanoma | IVabc | Right chest wall, right lower eyelid, lips | Multiple surgery only | PR, CT & complete subcutaneous response | Completed | 28/50 | Yes |
| 14 | 52/M | Adenocarcinoma of the Pancreas | IV | Pancreas & portal vein | M. vaccae; retinoic acid & gemcitabine | PD; minor response serum CA19.9 | Completed | 28/50 | Yes |
| 15 | 47/M | Carcinoid | IV | Multiple carcinoid tumours | Radiotherapy; 5-fluorouracil & folinic acid; interferon; etoposide & cisplatin; thalidomide | N/E entered inappropriately | Withdrew | 14/10 | No |
| 16 | 34/M | Adenocarcinoma of the Pancreas | IV | Head of pancreas | Gemcitabine & tomudex | PD | Completed | 28/50 | Yes (ELISA only) |
| 17 | 55/F | Renal cell carcinoma | IV | Left kidney | Interferon; bryostatin; thalidomide; radiotherapy | N/E withdrew due to adverse effects | Withdrew | 16/10 | No |
| 18 | 65/F | Ductal carcinoma of the breast | II | Breast | Mitozantrone, methotrexate & mitomycin; cyclophosphomide methotrexate & 5-fluorouracil; megace; 5-fluorouracil, epirubicin & cyclophosphomide; herceptin; tamoxifen; radiotherapy | N/E withdrew due to generalised weakness | Withdrew | 14/10 | No |
| 19 | 66/M | Squamous cell carcinoma of the lung | IV | Right lung | Mitomycin, winblastine sulphate & cisplatin; radiotherapy | PD | Progressed | 26/25 | No |
| 20 | 66/F | Adenocarcinoma of the lung | III | Left lung | Radiotherapy; mitomycin, vinblastine & cisplatin | PD | Completed | 28/50 | Yes |
Staging: a, skin, subcutaneous tissue, lymph node metastases; b, lung and gastrointestinal metastases; c, other sites including liver, bone and brain metastases.
Response: PR=partial response; SD=static disease; PD=progressive disease; N/E=nonevaluable.
MATERIALS AND METHODS
Patient selection
Patients were recruited from a single oncology centre according to the following eligibility criteria: histologically or cytologically proven stage IV metastatic melanoma (n=13), unresectable adenocarcinoma of pancreas (n=2), renal cell carcinoma (n=1), ductal carcinoma of the breast (n=1), squamous cell carcinoma of the lung (n=1), carcinoid (n=1); age over 18 years; clinical or radiological evidence of disease progression in the 3 months prior to trial entry; life expectancy of over 2 months; adequate baseline organ function; and minimum body weight of 50 kg. Previous treatment with chemotherapy or radiotherapy was allowed with the exception of prior radiotherapy to the brain. For all patients, there was no known hypersensitivity to thalidomide or similar drugs and no previous anticancer therapy or experimental treatment for 30 days prior to study entry (for pancreatic patients, no concomitant chemotherapy). Women were excluded from the study if pregnant, lactating or not using adequate contraception. All patients gave written informed consent prior to participation in the study. The study protocol was approved by the local research ethics committee (LREC) and was conducted according to ICH good clinical practice and in accordance with the declaration of Helsinki.
Treatment and assessment
CC-5013 was manufactured by Penn pharmaceuticals (Tredegar, Wales, UK) and supplied by Celgene Corporation (Warren, NJ, USA). Before initiating therapy, patients were subject to a complete medical history, physical examination and baseline evaluation of signs and symptoms, including full blood counts and a detailed neurological examination. These were repeated at weekly intervals during the study period and also at the end of the study. CC-5013 was taken in tablet form each evening and blood samples were collected at approximately the same time of the day at each visit. Therefore, analysis of serum cytokines and T-cell subsets was undertaken at a constant interval relative to the CC-5013 administration.
The treatment was administered according to accelerated titration design with intrapatient dose escalation (modified from Simon et al, 1997). All patients were treated with 5 mg day−1 CC-5013 for 1 week with the dose escalating to 10 mg day−1 at week 2, 25 mg day−1 at week 3 and 50 mg day−1 at week 4. The study treatment was terminated after 4 weeks; however, patients were allowed to continue on the final dose subject to tolerance and response. Treatment beyond 28 days was administered on a named patient basis and patients continued to be regularly assessed for toxicity and response.
The assessment of safety and tolerability of the study drug was based on the evaluations of the clinical laboratory tests, measurements of vital signs and the occurrence of adverse events during the study. The toxicity of the study drug was evaluated by means of the NCI-Common Toxicity Criteria (http://ctep.info.nih.gov/repo rting/ctc.html).
Evaluation of tumour response was performed following 4 weeks of treatment with CT scan and measurement of visible skin lesions. Response was classified as per WHO criteria.
Analysis of serological factors
Blood was collected into serum separator tubes and left to clot for ∼30 min. Tubes were spun at 950 g for 10 min and serum was collected. Sera were frozen in aliquots at −70°C until assayed for sIL-2 receptor, IL-2, IL-12, tumour necrosis factor-α (TNF-α), IFN-γ, granulocyte–macrophage colony-stimulating factor (GM-CSF), vascular endothelial growth factor (VEGF), IL-8 and basic fibroblast growth factor (b-FGF) by ELISA. Standard absorbance (405 nm) of duplicate wells was used to calculate the concentration of cytokine/receptor levels.
Phenotypic analysis of T cells
Heparinised venous blood was collected into sodium heparin vacutainers and surface stained (for 15 min at room temperature (RT)) with the following fluorochrome-conjugated monoclonal antibodies: anti-CD4 PerCP (Clone SK7; Becton Dickinson Immunocytometry Systems, BDIS, Oxford, UK) or anti-CD8 PerCP (SK1; BDIS) with anti-CD45RA FITC (L48;BDIS) and anti-CD45RO PE (UCHL-1;BDIS) plus appropriate isotype matched and compensation controls. Red blood cells were lysed with 2 ml 1 × FACS Lysing Solution (BDIS; 10 min, RT), samples were spun down (500 g, 5 min) and the cell pellet resuspended in 200 μl CellFix (BDIS) for analysis. PBMC were surface stained (30 min, 4°C) with anti-CD4 or anti-CD8 PerCP FITC (SK11; BDIS) and anti-CD45RO PE plus appropriate isotype matched and compensation controls.
Upon flow cytometric analysis, lymphocytes were gated on forward scatter (FSC) vs side scatter (SSC) properties and PerCP-positive T-cell subsets were displayed as two-colour dotplots. For each sample, 10 000 lymphocytes were acquired on a Becton Dickinson FACScan using CellQuest™ software and analysed using EXPO32™ (Beckman Coulter).
Statistical analysis
Serological and cell surface data comparisons between groups were examined by the Mann–Whitney U-test. The statistics were performed using GraphPad InStat 3 software.
RESULTS
Patient characteristics
The study recruited 20 patients, 13 with stage IV malignant melanoma, two with unresectable adenocarcinoma of the pancreas, one case of renal cell carcinoma, one of ductal carcinoma of the breast, one carcinoid and one patient with squamous cell carcinoma of the lung. (see Table 1 for patient details). In all, 12 patients were male and eight female. Age varied between 16 and 80 years with a median age of 51.5 years. The 16-year-old patient was recruited to the study following thorough discussion and agreement of the patient, his family and study investigators.
In total, 14 patients received the full 28 days of CC-5013 with no need for dose reduction. Three patients developed PD while on the study drug and did not complete treatment. One patient discontinued after 14 days, one after 24 days and one after 26 days. Three patients were nonevaluable due to withdrawal of consent to the study, two after 14 days and one after 16 days.
Toxicity
Seven patients developed serious adverse events, none of them thought to be associated with the study drug. Patient 1 developed anaemia, requiring blood transfusion, as well as chest infection. Anaemia was most likely related to heavy bone marrow infiltration and disseminated disease. Following treatment of the infection, the patient completed the study. Patient 3 developed shortness of breath, which was due to accumulation of pleural effusion followed by chest infection and progressive disease. This patient was withdrawn from the study after 14 days of treatment. Patient 11 suffered dehydration and subsequent renal failure associated with poor performance status and disease progression. The patient was withdrawn from the study after 24 days. Patient 15 had prior spinal disease and was hospitalised due to spinal cord compression. The patient was withdrawn after 14 days and the overall impression was that the patient was entered inappropriately as he was not able to adhere to the study protocol. Patient 17 experienced a series of adverse events, mostly diarrhoea, abdominal pain and paraesthesia; none of those were more than grade 2, but he withdrew his consent to the study drug. Patient 19 was admitted to hospital in an acute confusional state, caused by a collapsed lung and increased dyspnoea. The patient was withdrawn from the study at day 26 and was admitted to a hospice. Patient 20 was hospitalised with worsened haemoptysis and dyspnoea but completed the study.
For 36% of the adverse effects, toxicity was classified as grade 1, 51% as grade 2, 8% as grade 3 and 5% as grade 4. There were several cases of grade 1 and 2 toxicity, some of them possibly associated with CC-5013 (see Table 2 ). The most common were: paraesthesia, altered taste, papular, itchy rash, fatigue, nausea, poor appetite and vomiting. There was no evidence that somnolence is a problem for patients taking CC-5013. Apart from mild paraesthesia, there was no evidence of any neurological defects. Evidence of haematological toxicity included three patients who developed thrombocytopaenia and one who developed neutropaenia while on the study. There was no evidence for any biochemical toxicities in association with CC-5013 treatment.
Table 2. Adverse events reported during CC-5013 treatment.
| Patient | Graded diagnosis | NCI toxicity grade | Causal relationship to REVIMID treatment |
|---|---|---|---|
| 2 | Nausea and Vomiting | Grade 2 | Remote |
| Fatigue | Grade 2 | Possible | |
| Altered taste | Grade 2 | Possible | |
| Hot flushes | Grade 1 | Possible | |
| Occasional cramps | Grade 1 | Possible | |
| 4 | Papular rash | Grade 1 | Possible |
| 6 | Papular rash | Grade 2 | Possible |
| 8 | Cramps | Grade 1 | Possible |
| Fatigue | Grade 2 | Possible | |
| 13 | Altered taste | Grade 1 | Possible – although there is a local lesion |
| 16 | Jaundice | Grade 2 | Remote |
| 17 | Numbness | Grade 2 | Possible |
| 18 | Fatigue | Grade 2 | Possible |
| 20 | Macular rash | Grade 1 | Probable |
Evidence of clinical efficacy
Partial response (PR) was documented in one out of 20 patients (5%). Five patients had stable disease (SD) (25%) and 11 patients developed progressive disease (PD) (60%). There were no complete responses and three patients were not evaluable (patients 17 and 18 withdrew consent and patient 15 was entered inappropriately). Two of the patients developed a mixed response. Patient 2 had a decrease in the size of mediastinal mass and skin lesions but an increase in the size of liver deposit, and patient 14 had stable para-aortic lymphadenopathy but an increase in the number of lung and liver deposits.
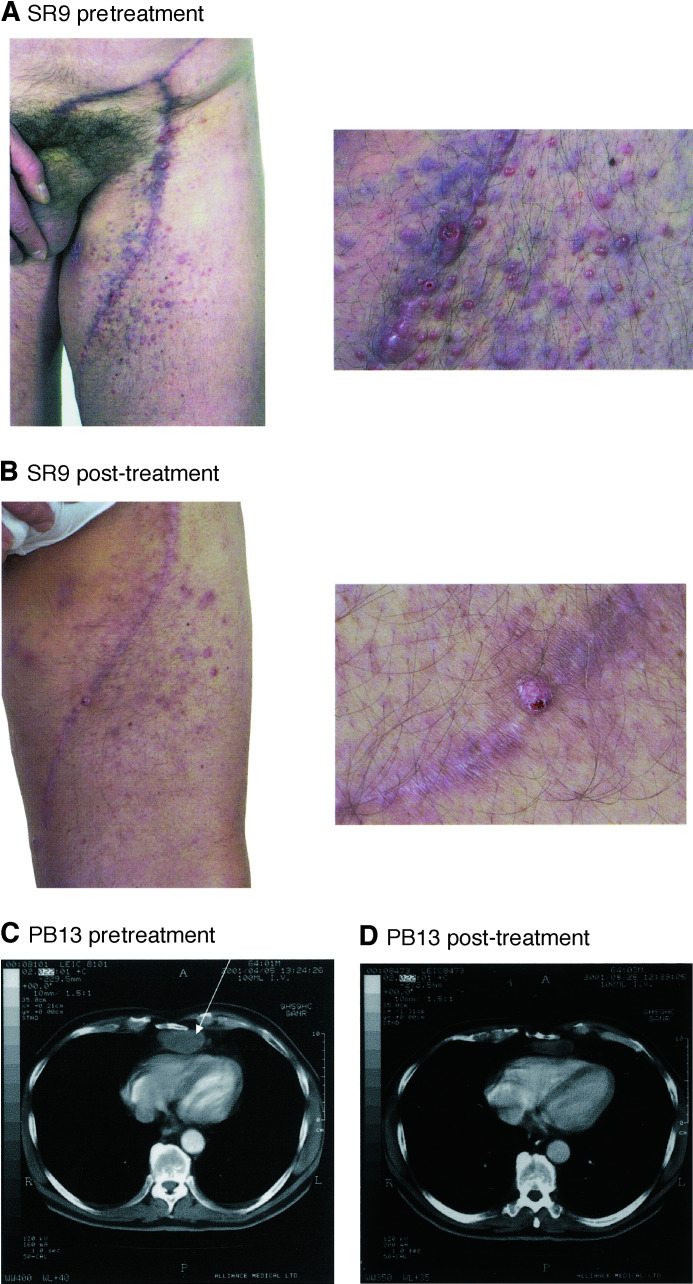
Some patients developed minor responses that did not classify as PR but with a definite decrease in the size of visceral lymph nodes (patient 4), subcutaneous nodules (patient 7) and cutaneous disease (patient 9) (Figure 1). In all, 10 patients continued CC-5013 at the final dose (50 mg) on a named patient basis with static disease and a good quality of life. These patients continued on CC-5013 for a mean of 3.5 months prior to disease progression. One patient continued on CC-5013 at 50 mg for 8 months during which time there was a minor response of pulmonary secondaries.
Figure 1.
Evidence of clinical response during CC-5013 treatment. (A) Patient SR9 exhibited extensive nodular cutaneous disease over his left thigh. Following treatment (B) lesions became flattened and attenuated. (C) Patient PB13 shows mediastinal mass (arrowed) on CT scan which is reduced (D) after treatment.
Effect on immunologic and proangiogenic serum factors
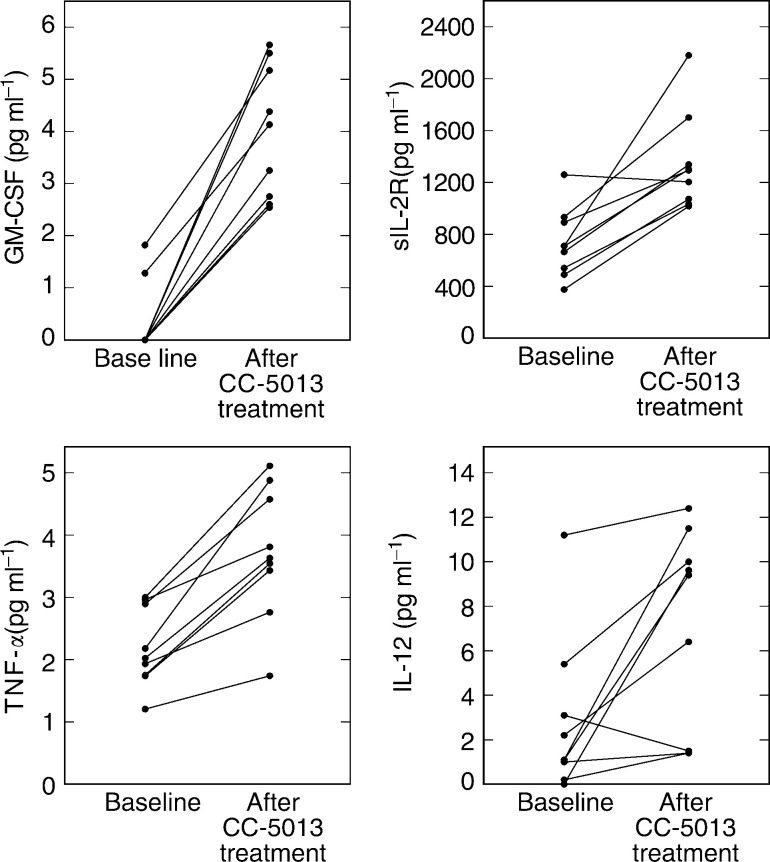
We detected increased levels of GM-CSF, TNF-α (both nine out of nine), sIL-2 receptor (eight out of nine) and IL-12 (seven out of nine) in the serum of patients after CC-5013 treatment compared to pretreatment levels (Figure 2). Available serum samples from nine patients were assessed. Median sIL-2 receptor: baseline, 710 pg ml−1; follow-up, 1294 (*P=0.0005). Median GM-CSF: baseline, 0 pg ml−1; follow-up, 4.13 (*P=<0.0001). Median TNF-α: baseline, 2.02 pg ml−1; follow-up, 3.63 (*P=0.0056). Median IL-12: baseline, 1.1 pg ml−1; follow-up 9.4 (*P=0.032). We were unable to detect IL-2 or IFN-γ in any of the serum samples.
Figure 2.
Changes in serum sIL-2 receptor, GM-CSF, TNF-α and IL-12 levels due to CC-5013 treatment. Levels pretreatment (baseline) are compared to levels at follow-up (at 4–5 weeks). sIL-2 receptor; *P=0.0005 (baseline vs follow-up). GM-CSF; *P=<0.0001. TNF-α; *P=0.0056. IL-12; *P=0.032.
We also assayed serum to determine effects on the levels of proangiogenic factors (Figure 3). Median VEGF: baseline, 258 pg ml−1; follow-up, 207 (NS, P=0.566). Median b-FGF: baseline, 1.44 ng ml−1; follow-up, 1.4 (NS, P=0.427). Median IL-8: baseline, 11 pg ml−1; follow-up, 32 (*P=0.047).
Figure 3.
Detection of proangiogenic factors VEGF, IL-8 and b-FGF in the serum of patients is not significantly changed by CC-5013 treatment compared to baseline. VEGF; NS, P=0.566. IL-8; *P=0.047. b-FGF; NS, P=0.427.
Effect on peripheral blood T-cell CD45 isoform expression
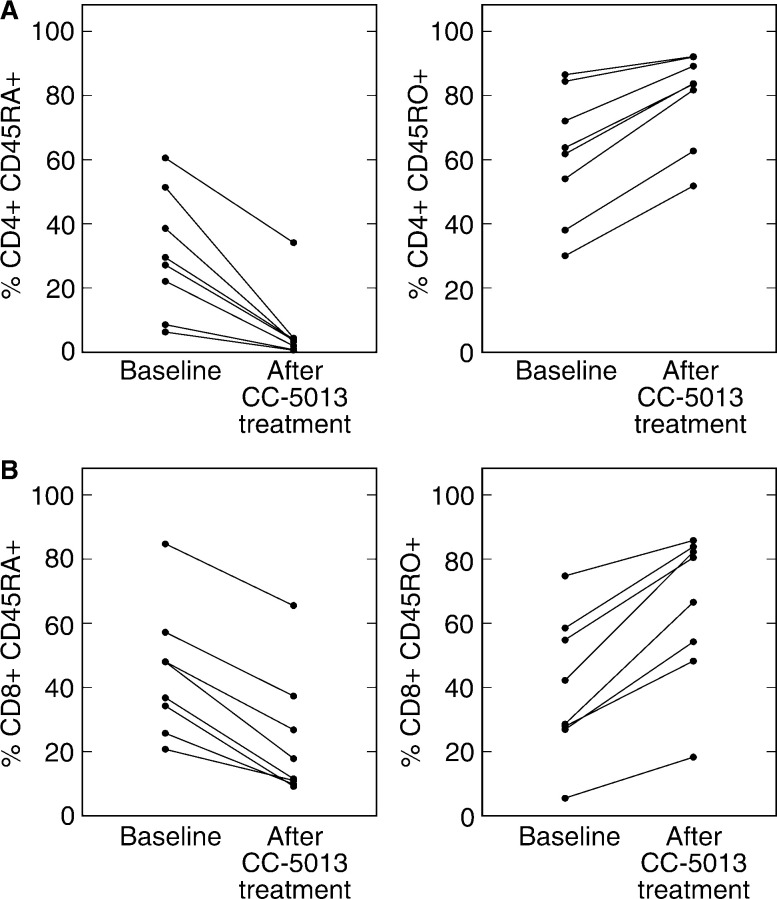
We determined the expression of CD45 isoforms (CD45RA and CD45RO) on peripheral CD4+ and CD8+ T cells before CC-5013 treatment and at follow-up (at weeks 4 and 5). Figure 4 shows clear trends towards decreased CD45RA expression on both T-cell subsets in conjunction with increased expression of CD45RO. However, significance is only reached during analysis of decreased CD45RA expression on CD4+ cells. Median percentage CD45RA expression on CD4+ cells: baseline, 28.4%; follow-up, 3.5% (*P=0.003). Median CD45RO expression: baseline, 62.8%; follow-up, 83.6% (NS, P=0.105). Similar results are seen with CD8+ cells. Median CD45RA expression: baseline, 42.4%; follow-up, 14.7% (*P=0.049). Median CD45RO expression: baseline, 35.4%; follow-up, 73.51% (NS, P=0.065).
Figure 4.
Effect of CC-5013 treatment on the CD4+ and CD8+ T-cell surface expression of CD45 isoforms. Data are expressed as percentage expression on cells’ pretreatment (baseline) and at follow-up (4–5 weeks after starting treatment). For CD4+ cells: CD45RA expression; *P=0.003. CD45RO expression; NS, P=0.105. For CD8+ cells: CD45RA expression; *P=0.049. CD45RO expression; NS, P=0.065.
DISCUSSION
Disseminated malignant melanoma is a chemoresistant tumour with very poor prognosis. However, immunotherapy in advanced disease can offer durable responses and a greater understanding of the immune mechanisms involved may in the future offer better treatment for a wider group of patients. This study is the first to show the use of CC-5013 in patients with solid tumours, which include 13 patients with advanced melanoma. Despite the fact that clinical response was not the primary end point of the study and that the patients had not responded to prior therapy, we found clear evidence of drug activity in rapidly progressing malignant melanoma with one PR and two minor responses of visceral disease. Responses were noted in small volume cutaneous and subcutaneous disease. However, there was no correlation between clinical response and disease volume; the one PR occurred in a patient with relatively high volume visceral disease. It was also noted that patients subjectively felt better after commencing treatment. There was no therapeutic effect in other solid tumours treated, although three out of six patients were nonevaluable due to withdrawal or disease progression. Overall, it would appear that CC-5013 is capable of inducing antitumour activity at the doses tested and that static disease can be maintained even if only a minor response has been achieved.
Unfortunately, due to the small numbers of patients for whom immunological parameters could be measured, it was impossible to correlate the data with clinical response. However, we have found that irrespective of clinical response, there is strong evidence of immunological activation in all nine patients from whom samples were available for analysis. We assessed serum cytokine levels for evidence of immune activation. While serum levels of IL-2 and IFN-γ remained beneath the detection limit of the assays employed in the study, there were significant and consistently increased levels of sIL-2 receptor (in eight out of nine patients), providing evidence of T-cell activation. The strong induction of GM-CSF production by CC-5013 in all nine patients is further evidence of immune activation and is likely to lead to the stimulation and increased functional capacity of monocytes/macrophages and dendritic cells (Armitage, 1998), thereby potentially boosting the presentation of tumour antigens. The clinical use of recombinant GM-CSF as a cancer immunotherapy has led to reports demonstrating its benefits in the treatment of patients with melanoma (Armitage, 1998; Spitler et al, 2000).
The induction of GM-CSF may explain the significantly increased levels of TNF-α and IL-12 in these patients. These observations are consistent even in the serum of patients with rapidly progressing disease that did not respond clinically to CC-5013. Increased production of TNF-α and IL-12 by antigen-presenting cells is likely to drive Th1-type immune responses and enhance antitumour immunity. We have previously shown that the strong induction of TNF-α in ex vivo cultures correlates with a better prognosis in patients with colorectal cancer (Heriot et al, 2000).
Immunological activation was also assessed by the analysis of surface expression of CD45 isoforms on CD4+ and CD8+ T cells. The CD45RA+ T-cell phenotype represents nonactivated and mainly naïve cells. Upon activation, truncation of the CD45RA isoform exposes the CD45RO epitope. Our results show that there is a remarkably consistent and extensive shift in T-cell expression of CD45RA at baseline to CD45RO during treatment with CC-5013 (Figure 3). However, due to limited patient numbers, only the decrease in CD45RA expression reaches statistical significance. This apparent T-cell activation is evident on both CD4+ and CD8+ populations, supporting previous in vitro data showing that IMiDs are able to costimulate both T-cell subsets (Marriott et al, 2001). The total lymphocyte counts were generally increased in this patient group (data not shown), indicating that apoptosis of CD45RA+ cells is unlikely to account for the relative decrease in this population.
Our data suggest that CC-5013 is able to boost Th1-type cellular immunity and provide an environment for the generation of an antitumour response. Support for this concept has been obtained in a vaccination model of colorectal cancer in which another IMiD was shown to generate a protective and long-lasting antitumour response in vivo (Dredge et al, 2002b).
The serological changes observed in our study indicate that low-dose therapy is able to provide a significant immunological stimulus. In the context of tumour immunity, this may help to overcome the anergy associated with advanced cancer patients and boost cellular immune responses. It is worth noting that the progressive nature of disease in this patient group means that while immunological activation is seen in all patients, it is remarkable to also observe clinical responses and static disease in some patients. In this regard, it is possible that a correlation between immunological and clinical responses may become apparent during the treatment of patients with less advanced disease. The possibility that CC-5013 may boost previously induced immunity is suggested by the fact that five patients with minor responses and static disease had previously been given some form of immunotherapy, such as melanoma peptides or IL-2.
We have observed that CC-5013 is antiangiogenic using in vitro assay systems (Dredge et al, 2002a). Therefore, it is possible that this compound may also act in vivo to reduce the formation of new blood vessels, thereby inhibiting metastasis and preventing tumour growth. During our assessment of serum proangiogenic factors, we found that although levels of the neutrophil chemoattractant IL-8 were increased, VEGF and b-FGF were relatively unchanged. Interestingly, thalidomide has also been shown to have no effect on serum VEGF and b-FGF during the effective treatment of patients with multiple myeloma (Neben et al, 2001). Although other factors may also be important during angiogenesis, these results suggest that the T-cell costimulatory activity of CC-5013 (and perhaps thalidomide) may be of greater importance during the advanced cancer setting. Other evidence in MM patients suggests that natural killer (NK) cell activity may be important (Davies et al, 2001) and we have noted increased NK cell numbers in some patients after CC-5013 treatment (unpublished observation).
The possibility that CC-5013 can enhance the effect of prior or subsequent treatments cannot be ruled out. Prior immunotherapy, whether successful or not, may contribute to the immunostimulatory properties of CC-5013 and its antiangiogenic properties may enhance responses to radiotherapy and chemotherapy. Future studies will need to take these potential interactions into account. In conclusion, CC-5013 is safe, well tolerated and has some clinical benefit and immunological effects in the treatment of patients with refractory malignant melanoma and supports the continuing clinical development of this exciting class of compounds.
Acknowledgments
The clinical data were compiled by Harrison Clinical Research, Ely, UK. We thank Nneka Belonwu and Joe Diffley for monitoring of patients and acquisition of trial data. This work was supported by Celgene Corporation, NJ, USA.
Footnotes
JB Bartlett was previously known as JB Marriott
References
- Alexander LN, Wilcox CM (1997) A prospective trial of thalidomide for the treatment of HIV-associated idiopathic esophageal ulcers. AIDS Res Hum Retroviruses 13: 301–304 [DOI] [PubMed] [Google Scholar]
- Armitage JO (1998) Emerging applications of recombinant human granulocyte–macrophage colony-stimulating factor. Blood 92: 4491–4508 [PubMed] [Google Scholar]
- Atkins MB (1997) The treatment of metastatic melanoma with chemotherapy and biologics. Curr Opin Oncol 9: 205–213 [DOI] [PubMed] [Google Scholar]
- Corral LG, Haslett PA, Muller GW, Chen R, Wong LM, Ocampo CJ, Patterson RT, Stirling DI, Kaplan G (1999) Differential cytokine modulation and T cell activation by two distinct classes of thalidomide analogues that are potent inhibitors of TNF-α. J Immunol 163: 380–386 [PubMed] [Google Scholar]
- Davies FE, Raje N, Hideshima T, Lentzsch S, Young G, Tai YT, Lin B, Podar K, Gupta D, Chauhan D, Treon SP, Richardson PG, Schlossman RL, Morgan GJ, Muller GW, Stirling DI, Anderson KC (2001) Thalidomide and immunomodulatory derivatives augment natural killer cell cytotoxicity in multiple myeloma. Blood 98: 210–216 [DOI] [PubMed] [Google Scholar]
- Dredge K, Marriott JB, Macdonald CD, Man H-W, Chen R, Muller GW, Stirling D, Dalgleish AG (2002a) Novel thalidomide analogues display anti-angiogenic activity independently of immunomodulatory effects. Br J Cancer 87: 1166–1172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dredge K, Marriott JB, Todryk SM, Muller GW, Chen R, Stirling DI, Dalgleish AG (2002b) Protective anti-tumour immunity induced by a costimulatory thalidomide analog in conjunction with whole tumour cell vaccination is mediated by increased Th1-type immunity. J Immunol 168: 4914–4919 [DOI] [PubMed] [Google Scholar]
- Ehrenpreis ED, Kane SV, Cohen LB, Cohen RD, Hanauer SB (1999) Thalidomide therapy for patients with refractory Crohn's disease: an open-label trial. Gastroenterology 117: 1271–1277 [DOI] [PubMed] [Google Scholar]
- Eisen T, Boshoff C, Mak I, Sapunar F, Vaughan MM, Pyle L, Johnston SR, Ahern R, Smith IE, Gore ME (2000) Continuous low dose thalidomide: a phase II study in advanced melanoma, renal cell, ovarian and breast cancer. Br J Cancer 82: 812–817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen T (2002) Thalidomide in solid malignancies. J Clin Oncol 20: 2607–2608 [DOI] [PubMed] [Google Scholar]
- Fife K, Howard MR, Gracie F, Phillips RH, Bower M (1998) Activity of thalidomide in AIDS-related Kaposi's sarcoma and correlation with HHV8 titre. Int J STD AIDS 9: 751–755 [DOI] [PubMed] [Google Scholar]
- Fine HA, Figg WD, Jaeckle K, Wen PY, Kyritsis AP, Loeffler JS, Levin VA, Black PM, Kaplan R, Pluda JM, Yung WK (2000) Phase II trial of the antiangiogenic agent thalidomide in patients with recurrent high-grade gliomas. J Clin Oncol 18: 708–715 [DOI] [PubMed] [Google Scholar]
- Gutheil J, Finucane D (2000) Thalidomide therapy in refractory solid tumour patients. Br J Haematol 110: 754. [DOI] [PubMed] [Google Scholar]
- Hamuryudan V, Mat C, Saip S, Ozyazgan Y, Silva A, Yurdakal S, Zwingenberger K, Yazici H (1998) Thalidomide in the treatment of the mucocutaneous lesions of the Behcet syndrome. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 128: 443–450 [DOI] [PubMed] [Google Scholar]
- Haslett PA, Corral LG, Albert M, Kaplan G (1998) Thalidomide costimulates primary human T lymphocytes, preferentially inducing proliferation, cytokine production, and cytotoxic responses in the CD8+ subset. J Exp Med 187: 1885–1892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heriot AG, Marriott JB, Cookson S, Kumar D, Dalgleish AG (2000) Reduction in cytokine production in colorectal cancer patients: association with stage and reversal by resection. Br J Cancer 82: 1009–1012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hideshima T, Chauhan D, Shima Y, Raje N, Davies FE, Tai YT, Treon SP, Lin B, Schlossman RL, Richardson P, Muller G, Stirling D, Anderson KC (2000) Thalidomide and its analogs overcome drug resistance of human multiple myeloma cells to conventional therapy. Blood 96: 2943–2950 [PubMed] [Google Scholar]
- Jacobson JM, Greenspan JS, Spritzler J, Ketter N, Fahey JL, Jackson JB, Fox L, Chernoff M., Wu AW, MacPhail LA, Vasquez GJ, Wohl DA (1997) Thalidomide for the treatment of oral aphthous ulcers in patients with human immunodeficiency virus infection. N Engl J Med 336: 1487–1493 [DOI] [PubMed] [Google Scholar]
- Juliusson G, Celsing F, Turesson I, Lenhoff S, Adriansson M, Malm C (2000) Frequent good partial remissions from thalidomide including best response ever in patients with advanced refractory and relapsed myeloma. Br J Haematol 109: 89–96 [DOI] [PubMed] [Google Scholar]
- Klausner JD, Makonkawkeyoon S, Akarasewi P, Nakata K, Kasinrerk W, Corral L, Dewar RL, Lane HC, Freedman VH, Kaplan G (1996) The effect of thalidomide on the pathogenesis of human immunodeficiency virus type 1 and M. tuberculosis infection. J AIDS 11: 247–257 [DOI] [PubMed] [Google Scholar]
- Kneller A, Raanani P, Hardan I, Avigdor A, Levi I, Berkowicz M, Ben-Bassat I (2000) Therapy with thalidomide in refractory multiple myeloma patients – the revival of an old drug. Br J Haematol 108: 391–393 [DOI] [PubMed] [Google Scholar]
- Marriott JB, Muller G, Dalgleish AG (1999) Thalidomide as an emerging immunotherapeutic agent. Immunol Today 583: 538–540 [DOI] [PubMed] [Google Scholar]
- Marriott JB, Muller GW, Stirling D, Dalgleish AG (2001) Immunotherapeutic and anti-tumour potential of thalidomide analogues. Exp Opin Biol Ther 1: 675–682 [DOI] [PubMed] [Google Scholar]
- Neben K, Moehler T, Kraemer A, Benner A, Egerer G, Ho AD, Goldschmidt H (2001) Response to thalidomide in progressive multiple myeloma is not mediated by inhibition of angiogenic cytokine secretion. Br J Haematol 115: 605–608 [DOI] [PubMed] [Google Scholar]
- Patt YZ, Hassan MM, Lozano RD, Ellis LM, Petersson JA, Waugh KA (2000) Durable clinical response of refractory hepatocellular carcinoma to orally administered thalidomide. Am J Clin Oncol 23: 319–321 [DOI] [PubMed] [Google Scholar]
- Raje N, Anderson K (1999) Thalidomide – a revival story. N Engl J Med 341: 1606–1609 [DOI] [PubMed] [Google Scholar]
- Reyes-Teran G, Sierra-Madero JG, Martinez Del Cerro V, Arroyo-Figueroa H, Pasquetti A, Calva JJ, Ruiz-Palacios GM (1996) Effects of thalidomide on HIV-associated wasting syndrome: a randomized, double-blind, placebo-controlled clinical trial. AIDS 10: 1501–1507 [DOI] [PubMed] [Google Scholar]
- Richardson PG, Schlossman RL, Hideshima T, Davies F, Le Blanc R, Catley L, Doss D, Kelly KA, McKennev M, Mechlowicz J, Freeman A, Deocampo R, Rich R, Ryoo J, Chauhan D, Munshi N, Weller E, Thomas S, Zeldis J, Anderson KC (2001) A phase 1 study of oral CC-5013, an immunomodulatory thalidomide derivative, in patients with relapsed and refractory multiple myeloma. Presented at the American Society of Hematology 43rd Annual Meeting, Orlando, FL, 7–11 December
- Richardson PG, Schlossman RL, Weller E, Hideshima T, Mitsiades C, Davies F, LeBlanc R, Catley L, Doss D, Kelly KA, McKenney M, Mechlowicz J, Freeman A, Deocampo R, Rich R, Ryoo J, Chauhan D, Balinski K, Zeldis J, Anderson KC (2002) Immunomodulatory drug CC-5013 overcomes drug resistance and is well tolerated in patients with relapsed multiple myeloma. Blood 100: 3063–3067 [DOI] [PubMed] [Google Scholar]
- Schuler U, Ehninger G (1995) Thalidomide: rationale for renewed use in immunological disorders. Drug Saf 12: 364–369 [DOI] [PubMed] [Google Scholar]
- Sharpstone D, Rowbottom A, Nelson M, Gazzard B (1995) The treatment of microsporidial diarrhoea with thalidomide. AIDS 9: 658–659 [DOI] [PubMed] [Google Scholar]
- Simon R, Freidlin B, Rubinstein L, Arbuck SG, Collins J, Christian MC (1997) Accelerated titration designs for phase I clinical trials in oncology. J Natl Cancer Inst 89: 1138–1147 [DOI] [PubMed] [Google Scholar]
- Singhal S, Mehta J, Desikan R, Ayers D, Roberson P, Eddleman P, Munshi N, Anaissie E, Wilson C, Dhodapkar M, Zeldis J, Barlogie B (1999) Antitumour activity of thalidomide in refractory multiple myeloma. N Engl J Med 341: 1565–1571 [DOI] [PubMed] [Google Scholar]
- Spitler LE, Grossbard ML, Ernstoff MS, Silver G, Jacobs M, Hayes FA, Soong SJ (2000) Adjuvant therapy of stage III and IV malignant melanoma using granulocyte–macrophage colony-stimulating factor. J Clin Oncol 18: 1614–1621 [DOI] [PubMed] [Google Scholar]
- Tseng JE, Glisson BS, Khuri FR, Shin DM, Myers JN, El-Naggar AK, Roach JS, Ginsberg LE, Thall PF, Wang X, Teddy S, Lawhorn KN, Zentgraf RE, Steinhaus GD, Pluda JM, Abbruzzese JL, Hong WK, Herbst RS (2001) Phase II study of the antiangiogenesis agent thalidomide in recurrent or metastatic squamous cell carcinoma of the head and neck. Cancer 92: 2364–2373 [DOI] [PubMed] [Google Scholar]
- Vasiliauskas EA, Kam LY, Abreu-Martin MT, Hassard PV, Papadakis KA, Yang H, Zeldis JB, Targan IR (1999) An open-label pilot study of low-dose thalidomide in chronically active, steroid-dependent Crohn’s disease. Gastroenterology 117: 1278–1287 [DOI] [PubMed] [Google Scholar]
- Wettstein AR, Meagher AP (1997) Thalidomide in Crohn’s disease. Lancet 350: 1445–1446 [DOI] [PubMed] [Google Scholar]
- Youle M, Clarbour J, Farthing C, Connolly M, Hawkins D, Staughton R, Gazzard B (1989) Treatment of resistant aphthous ulceration with thalidomide in patients positive for HIV antibody. BMJ 298: 432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zangari M, Tricot G, Zeldis J, Eddlemon P, Saghafifar F, Barlogie B (2001) Results of phase 1 study of CC-5013 for the treatment of multiple myeloma patients who relapse after high dose chemotherapy. Presented at the American Society of Hematology 43rd Annual Meeting, Orlando, FL, 7–11 December
- Zomas A, Anagnostopoulos N, Dimopoulos MA (2000) Successful treatment of multiple myeloma relapsing after high-dose therapy and autologous transplantation with thalidomide as a single agent. Bone Marrow Transplant 25: 1319–1320 [DOI] [PubMed] [Google Scholar]