Abstract
Against 300 strains of pneumococci and 100 group A streptococci of differing β-lactam, macrolide, and quinolone resistance phenotypes, AR-709 was very active, with all MICs being ≤2 μg/ml. Furthermore, AR-709 was active against strains that were both susceptible and resistant to trimethoprim-sulfamethoxazole.
Streptococcus pneumoniae strains that are resistant to penicillin G as well as other agents occur worldwide. Most macrolide-resistant pneumococci also are penicillin G resistant, and pneumococcal quinolone resistance also has been reported. Trimethoprim-sulfamethoxazole resistance in pneumococci is high, invalidating its clinical use in infections by these organisms (1, 2, 5, 8-10, 16, 19-22, 25). The problem of drug-resistant pneumococci is exacerbated by their tendency to spread from country to country and also from continent to continent (18). Macrolide resistance also has been reported for Streptococcus pyogenes (4, 6, 13, 22, 26).
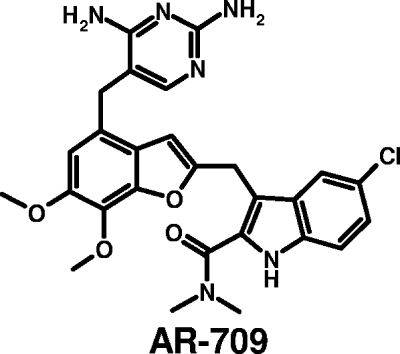
AR-709 is an investigational diaminopyrimidine that inhibits microbial dihydrofolate reductase and is under development by Arpida AG for the therapy of community-acquired upper and lower respiratory tract infections (7, 11, 12, 14, 15, 24). We have compared the in vitro activity of AR-709 (a new diaminopyrimidine antibiotic) (Fig. 1) to those of trimethroprim-sulfamethoxazole, amoxicillin-clavulanate, cefuroxime, azithromycin, ciprofloxacin, and levofloxacin against a spectrum of pneumococci and group A streptococci with differing resistance phenotypes.
FIG. 1.
Chemical structure of AR-709.
Clinical strains of S. pneumoniae included the majority of known resistotypes, of which 101 were penicillin G susceptible (33.6%), 122 were penicillin G intermediate (40.6%), and 77 were fully penicillin G resistant (25.6%). Of these 300 strains, 158 (52.6%) were macrolide resistant [66 had erm(B), 59 mef(A), 1 erm(B) plus mef(A), 4 erm(A), 23 L4, and 4 23S rRNA ribosomal protein mutations]. Twenty-nine (∼10%) pneumococcal strains were quinolone resistant, with defined mutations in the quinolone resistance-determining region. One hundred nine pneumococcal strains were susceptible to trimethoprim-sulfamethoxazole, and the trimethoprim-sulfamethoxazole MICs for 191 strains were intermediate (1 to 2 μg/ml) or resistant (≥4 μg/ml) (3). The 100 S. pyogenes isolates included 61 macrolide-resistant strains [20 had erm(B), 20 erm(A), 20 mef(A), and 1 L4 ribosomal protein mutations]. Organisms were identified by standard methodology and stored at −70°C in double-strength skim milk (Difco Laboratories, Detroit, MI) until use. With the exception of streptococci with ribosomal mutations, all strains were isolated within 8 years of the beginning of the study. Because an effort was made to include as many phenotypes as possible, we decided to include older cultures as well. Regardless of the time of isolation, all phenotypes are similar to those from strains isolated during the past few years and, thus, are representative of strains likely to be encountered clinically at the present time.
AR-709 was obtained from Arpida AG, Reinach, Switzerland, and sulfamethoxazole was obtained from Sigma Laboratories, St. Louis, MO. Other drugs were obtained from their respective agents. MIC testing was done by agar dilution methodology using Mueller-Hinton agar (Difco Laboratories) with 5% lysed horse blood for AR-709 and trimethoprim-sulfamethoxazole. All other drugs were tested with 5% added sheep blood. Suspensions with turbidities that were equivalent to a 0.5 McFarland standard were scraped from blood plates and diluted to obtain a final inoculum of 104 CFU/spot. Plates were inoculated and incubated overnight in ambient air at 35°C. Quality control strains recommended by the Clinical Laboratory Standards Institute, including S. pneumoniae ATCC 49619, were included in each run (3).
Results of MIC testing are listed in Tables 1 and 2. As can be seen, AR-709 was very active against all streptococci tested irrespective of resistance phenotypes, with a MIC range against pneumococci of ≤0.008 to 2 μg/ml and of ≤0.008 to 0.125 μg/ml against group A streptococci. In contrast, trimethoprim-sulfamethoxazole MICs against pneumococci ranged between 0.03 and >8 μg/ml. Of all pneumococci, 191 (63.7%) were intermediate or resistant to trimethoprim-sulfamethoxazole; the MIC range for AR-709 against trimethoprim-sulfamethoxazole-intermediate or -resistant strains was ≤0.008 to 2 μg/ml, and against trimethoprim-sulfamethoxazole-susceptible strains it was ≤0.008 to 0.5 μg/ml. Therefore, AR-709 was similarly active against pneumococci that either were susceptible or intermediate/resistant to trimethoprim-sulfamethoxazole. Ninety-three pneumococcal strains (31%) were multidrug resistant (i.e., resistant to three or more different classes of drugs); against these isolates the MIC range for AR-709 was 0.06 to 2 μg/ml. In terms of other comparator agents, the MICs of β-lactams and azithromycin against pneumococci rose with those of penicillin G. Quinolone-susceptible pneumococcal strains had levofloxacin MICs ranging between 0.5 and 2 μg/ml. Furthermore, all group A streptococci were susceptible to β-lactams, trimethoprim-sulfamethoxazole, and quinolones. Against macrolide-resistant group A streptococci, the MICs of AR-709 were within one dilution of those against macrolide-susceptible strains.
TABLE 1.
MICs of AR-709 and other agents against pneumococci
| Drug and strain susceptibility typea | MIC (μg/ml)
|
||
|---|---|---|---|
| Range | 50% | 90% | |
| AR-709 | |||
| Penicillin S | ≤0.008-2 | 0.06 | 0.25 |
| Penicillin I | ≤0.008-1 | 0.25 | 0.5 |
| Penicillin R | 0.016-2 | 0.25 | 1 |
| Macrolide S | ≤0.008-1 | 0.12 | 0.5 |
| Macrolide R | ≤0.008-2 | 0.25 | 0.5 |
| Quinolone S | ≤0.008-2 | 0.12 | 0.5 |
| Quinolone R | 0.016-2 | 0.25 | 1 |
| SXT S | ≤0.008-0.5 | 0.06 | 0.12 |
| SXT R | ≤0.008-2 | 0.25 | 0.5 |
| SXT | |||
| Penicillin S | 0.03->8 | 0.25 | 4 |
| Penicillin I | 0.12->8 | 4 | 8 |
| Penicillin R | 0.12->8 | 8 | 8 |
| Macrolide S | 0.03->8 | 0.5 | 8 |
| Macrolide R | 0.12->8 | 4 | 8 |
| Quinolone S | 0.06->8 | 4 | 8 |
| Quinolone R | 0.03->8 | 4 | 8 |
| SXT S | 0.03-0.5 | 0.25 | 0.5 |
| SXT R | 1->8 | 8 | 8 |
| Amoxicillin-clavulanate | |||
| Penicillin S | ≤0.016-0.12 | ≤0.016 | 0.03 |
| Penicillin I | ≤0.016-1 | 0.12 | 1 |
| Penicillin R | 0.25-8 | 2 | 4 |
| Macrolide S | ≤0.016-2 | 0.06 | 1 |
| Macrolide R | ≤0.016-8 | 0.12 | 4 |
| Quinolone S | ≤0.016-8 | 0.12 | 2 |
| Quinolone R | ≤0.016-4 | 0.5 | 2 |
| SXT S | ≤0.016-2 | 0.03 | 0.12 |
| SXT R | ≤0.016-8 | 0.5 | 4 |
| Cefuroxime | |||
| Penicillin S | 0.016-0.5 | 0.03 | 0.12 |
| Penicillin I | 0.03-4 | 0.25 | 4 |
| Penicillin R | 1->64 | 4 | 16 |
| Macrolide S | 0.016-8 | 0.25 | 4 |
| Macrolide R | 0.016->64 | 0.5 | 8 |
| Quinolone S | 0.016->64 | 0.25 | 4 |
| Quinolone R | 0.03-8 | 2 | 8 |
| SXT S | 0.016-16 | 0.03 | 0.5 |
| SXT R | 0.016->64 | 2 | 8 |
| Azithromycin | |||
| Penicillin S | 0.03->64 | 0.12 | >64 |
| Penicillin I | 0.03->64 | 0.12 | >64 |
| Penicillin R | 0.03->64 | 8 | >64 |
| Macrolide S | 0.03-0.25 | 0.12 | 0.12 |
| Macrolide R | 1->64 | >64 | >64 |
| Quinolone S | 0.03->64 | 4 | >64 |
| Quinolone R | 0.03->64 | 0.12 | >64 |
| SXT S | 0.03->64 | 0.12 | >64 |
| SXT R | 0.03->64 | 8 | >64 |
| Ciprofloxacin | |||
| Penicillin S | 0.5->32 | 2 | 16 |
| Penicillin I | 0.5-32 | 1 | 4 |
| Penicillin R | 0.5->32 | 2 | 4 |
| Macrolide S | 0.5->32 | 2 | 16 |
| Macrolide R | 0.5->32 | 1 | 4 |
| Quinolone S | 0.5-32 | 1 | 2 |
| Quinolone R | 4->32 | 32 | >32 |
| SXT S | 0.5->32 | 2 | 8 |
| SXT R | 0.5->32 | 1 | 4 |
| Levofloxacin | |||
| Penicillin S | 0.5-16 | 1 | 8 |
| Penicillin I | 0.5-32 | 1 | 2 |
| Penicillin R | 0.5-16 | 1 | 4 |
| Macrolide S | 0.5-16 | 1 | 8 |
| Macrolide R | 0.5-32 | 1 | 2 |
| Quinolone S | 0.5-2 | 1 | 1 |
| Quinolone R | 4-32 | 16 | 16 |
| SXT S | 0.5-16 | 1 | 2 |
| SXT R | 0.5-32 | 1 | 2 |
| Penicillin G | |||
| Penicillin S | ≤0.008-0.06 | 0.016 | 0.06 |
| Penicillin I | 0.12-1 | 0.25 | 1 |
| Penicillin R | 2-16 | 2 | 4 |
| Macrolide S | 0.016-2 | 0.12 | 2 |
| Macrolide R | ≤0.008-16 | 0.25 | 4 |
| Quinolone S | 0.12-16 | 0.12 | 2 |
| Quinolone R | 0.016-4 | 0.5 | 2 |
| SXT S | ≤0.008-4 | 0.03 | 0.25 |
| SXT R | 0.016-16 | 1 | 4 |
S, susceptible; I, intermediate; R, resistant; and SXT, trimethoprim-sulfamethoxazole (1:19).
TABLE 2.
MICs of AR-709 and other agents against group A streptococci
| Drug and strain susceptibility typea | MIC (μg/ml)
|
||
|---|---|---|---|
| MIC range | 50% | 90% | |
| AR-709 | |||
| Macrolide S | ≤0.008-0.12 | 0.06 | 0.06 |
| Macrolide R | ≤0.008-0.06 | 0.016 | 0.03 |
| Trimethoprim-sulfamethoxazole (1:19) | |||
| Macrolide S | 0.06-0.5 | 0.12 | 0.25 |
| Macrolide R | ≤0.008-0.5 | 0.06 | 0.25 |
| Amoxicillin-clavulanate | |||
| Macrolide S | ≤0.016-0.03 | ≤0.016 | ≤0.016 |
| Macrolide R | ≤0.016-0.03 | ≤0.016 | ≤0.016 |
| Cefuroxime | |||
| Macrolide S | 0.016-0.016 | 0.016 | 0.016 |
| Macrolide R | 0.016-0.03 | 0.016 | 0.03 |
| Azithromycin | |||
| Macrolide S | 0.06-0.25 | 0.12 | 0.25 |
| Macrolide R | 4->64 | >64 | >64 |
| Ciprofloxacin | |||
| Macrolide S | 0.5-4 | 0.5 | 1 |
| Macrolide R | ≤0.25-2 | 0.5 | 2 |
| Levofloxacin | |||
| Macrolide S | 0.5-2 | 0.5 | 2 |
| Macrolide R | 0.25-2 | 0.5 | 1 |
S, susceptible; and R, resistant.
AR-709 is an experimental diaminopyrimidine that exhibits potent activity against pneumococci and other gram-positive pathogens by inhibiting bacterial dihydrofolate reductase (24). The drug has been shown to have postantibiotic effects for ≥1.1 h against pneumococci, with postantibiotic sub-MIC effects longer than those of postantibiotic + sub-MIC effects (7). AR-709 concentrations remain high in all key compartments of the lung throughout a 12-h experimental period (17) and also exhibited excellent in vivo antipneumococcal activity in mice following intravenous, oral, and intranasal administration (14). Plasma pharmacokinetics suggest a once-daily dosing regimen (15).
In a recent paper (23), Pichichero and Casey reported the emergence in the United States of an otopathogenic strain of pneumococcus type 19A that is not included in the current pneumococcal 7-valent conjugate vaccine and that is resistant to all antibiotics currently approved by the FDA for treating acute otitis media in children. There is a pressing need for new drugs that will be active against such resistant phenotypes. The uniform susceptibility of all trimethoprim-sulfamethoxazole-nonsusceptible pneumococcal strains in the current study to AR-709, together with the pharmacokinetics and administration route of AR-709 mentioned above, makes it a possible alternative drug for the treatment of the above-described resistant pneumococcal infections.
The results of this study show that the MICs of AR-709 were low against all streptococci tested. Similarly, Ressner and coworkers (24) have reported AR-709 MIC ranges of ≤0.008 to 1 μg/ml, with MICs at which 50 and 90% of the isolates tested are inhibited of 0.25 and 0.5 μg/ml, respectively, when tested against 239 recent multiresistant North American isolates of invasive pneumococci. Furthermore, studies by other workers (11, 12) have shown the promising activity of AR-709 against multidrug-resistant pneumococci, including those of erm, mef, and erm plus mef phenotypes. The results for other compounds were similar to those reported in other studies (1, 5, 9, 10, 16, 19-22, 25). Pending human pharmacokinetic/pharmacodynamic, animal efficacy, and toxicology studies, AR-709 shows promise for the future therapy of pneumococcal infections, especially those caused in children by nonvaccine panresistant serotypes such as 19A.
Acknowledgments
This study was supported by a grant from Arpida AG, Reinach, Switzerland.
Footnotes
Published ahead of print on 24 March 2008.
REFERENCES
- 1.Appelbaum, P. C. 1992. Antimicrobial resistance in Streptococcus pneumoniae—an overview. Clin. Infect. Dis. 15:77-83. [DOI] [PubMed] [Google Scholar]
- 2.Bozdogan, B., P. C. Appelbaum, L. Ednie, I. N. Grivea, and G. A. Syrogiannopoulos. 2003. Development of macrolide resistance by ribosomal protein L4 mutation in Streptococcus pyogenes during miocamycin treatment of an eight-year-old Greek child with tonsillopharyngitis. Clin. Microbiol. Infect. 9:966-969. [DOI] [PubMed] [Google Scholar]
- 3.Clinical and Laboratory Standards Institute. 2006. Performance standards for antimicrobial susceptibility testing. Approved standard M100-S16. Sixteenth informational supplement. Clinical and Laboratory Standards Institute, Wayne, PA.
- 4.Cornaglia, G., M. Ligozzi, A. Mazzariol, L. Masala, G. L. Cascio, G. Orefici, R. Fontana, et al. 1998. Resistance of Streptococcus pyogenes to erythromycin and related antibiotics in Italy. Clin. Infect. Dis. 27(Suppl. 1):S87-S92. [DOI] [PubMed] [Google Scholar]
- 5.Davies, T. A., L. M. Ednie, D. B. Hoellman, G. A. Pankuch, M. R. Jacobs, and P. C. Appelbaum. 2000. Antipneumococcal activity of ABT-773 compared to those of 10 other agents. Antimicrob. Agents Chemother. 44:1894-1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Azavedo, J. C. S., R. H. Yeung, D. J. Bast, C. L. Duncan, S. B. Borgia, and D. E. Low. 1999. Prevalence and mechanism of macrolide resistance in clinical isolates of group A streptococci from Ontario, Canada. Antimicrob. Agents Chemother. 43:2144-2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hawser, S., L. Weiss, K. Islam, and S. Lociuro. 2007. Postantibiotic effects of AR-709 against pneumococci. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother., abstr. F1-936.
- 8.Hoban, D., K. Waites, and D. Felmingham. 2003. Antimicrobial susceptibility of community-acquired respiratory tract pathogens in North America in 1999-2000: findings of the PROTEKT surveillance study. Diagn. Microbiol. Infect. Dis. 45:251-259. [DOI] [PubMed] [Google Scholar]
- 9.Jacobs, M. R., S. Bajaksouzian, A. Zilles, G. Lin, G. A. Pankuch, and P. C. Appelbaum. 1999. Susceptibilities of Streptococcus pneumoniae and Haemophilus influenzae to 10 oral antimicrobial agents based on pharmacodynamic parameters: 1997 U.S. surveillance study. Antimicrob. Agents Chemother. 43:1901-1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jacobs, M. R., D. Felmingham, P. C. Appelbaum, R. N. Grueneberg, et al. 2003. The Alexander project 1998-2000: susceptibility of pathogens isolated from community-acquired respiratory tract infection to commonly used antimicrobial agents. J. Antimicrob. Chemother. 52:229-246. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs, M. R, C. E. Good, A. Windau, and S. Bajaksouzian. 2006. AR-709, a novel diaminopyrimidine compound: activity against Streptococcus pneumoniae. Abstr. 46th Intersci. Conf. Antimicrob. Agents Chemother., abstr. F1-1956.
- 12.Jansen, W. T. M., A. Verel, J. Verhoef, and D. Milatovic. 2008. In vitro activity of AR-709 against Streptococcus pneumoniae. Antimicrob. Agents Chemother. 52:1182-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaplan, E. L., D. R. Johnson, M. C. del Rosario, and D. L. Horn. 1999. Susceptibility of group A beta-hemolytic streptococci to thirteen antibiotics. Examination of 301 strains isolated in the United States between 1994 and 1997. Pediatr. Infect. Dis. J. 18:1069-1072. [DOI] [PubMed] [Google Scholar]
- 14.Lappin, G., S. Warrington, D. Honeybourne, D. Sanghera, S. Dowen, N. Lister, K. Islam, and S. Lociuro. 2007. Concentrations of AR-709 in plasma and key compartments of the lungs after microdosing. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother., abstr. F1-938.
- 15.Lappin, G., S. Warrington, D. Sanghera, S. Dowen, N. Lister, K. Islam, and S. Lociuro. 2007. Plasma pharmacokinetics of AR-709 administered to male healthy volunteers as microdoses by the intravenous and oral route. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother., abstr. F1-939.
- 16.Mason, E. O., Jr., L. B. Lamberth, N. L. Kershaw, B. La T. Prosser, A. Zoe, and P. G. Ambrose. 2000. Streptococcus pneumoniae in the USA: in vitro susceptibility and pharmacodynamic analysis. J. Antimicrob. Chemother. 45:623-631. [DOI] [PubMed] [Google Scholar]
- 17.McKenney, D., T. Murphy, S. Little, L. Gordon, K. Islam, and S. Lociuro. 2007. Efficacy of AR-709 in pneumococcal murine pneumonia. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother., abstr. F1-937.
- 18.Munoz, R., J. M. Musser, M. Crain, D. E. Briles, A. Marton, A. J. Parkinson, U. Sorensen, and A. Tomasz. 1992. Geographic distribution of penicillin-resistant clones of Streptococcus pneumoniae: characterization by penicillin-binding protein profile, surface protein A typing, and multilocus enzyme analysis. Clin. Infect. Dis. 15:112-118. [DOI] [PubMed] [Google Scholar]
- 19.Pankuch, G. A., M. R. Jacobs, and P. C. Appelbaum. 1994. Study of comparative antipneumococcal activities of penicillin G, RP 59500, erythromycin, sparfloxacin, ciprofloxacin, and vancomycin by using time-kill methodology. Antimicrob. Agents Chemother. 38:2065-2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pankuch, G. A., S. A. Juenemann, T. A. Davies, M. R. Jacobs, and P. C. Appelbaum. 1998. In vitro selection of resistance to four β-lactams and azithromycin in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 42:2914-2918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pankuch, G. A., M. A. Visalli, M. R. Jacobs, and P. C. Appelbaum. 1998. Susceptibilities of penicillin- and erythromycin-susceptible and -resistant pneumococci to HMR 3647 (RU 66647), a new ketolide, compared with susceptibilities to 17 other agents. Antimicrob. Agents Chemother. 42:624-630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pérez-Trallero, E., C. Fernandez-Mazarrasa, C. Garcia-Rey, E. Bouza, L. Aguiular, J. Garcia-de-Lomas, and F. Baquero. 2001. Antimicrobial susceptibilities of 1,684 Streptococcus pneumoniae and 2,039 Streptococcus pyogenes isolates and their ecological relationships: results of a 1-year (1998-1999) multicenter surveillance study in Spain. Antimicrob. Agents Chemother. 45:3334-3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pichichero, M., and J. R. Casey. 2007. Emergence of a multiresistant serotype 19A pneumococcal strain not included in the 7-valent conjugate vaccine as an otopathogen in children. JAMA 298:1772-1778. [DOI] [PubMed] [Google Scholar]
- 24.Ressner, R., M. Moore, and J. Jorgensen. 2007. Determination of the activity of the diaminopyrimidine AR-709 against recent multidrug-resistant North American isolates of invasive Streptococcus pneumoniae. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother., abstr. E-912. [DOI] [PMC free article] [PubMed]
- 25.Schito, A. M., G. C. Schito, E. Debbia, G. Russo, J. Linares, E. Cercenado, and E. J. Bouza. 2003. Antibacterial resistance in Streptococcus pneumoniae and Haemophilus influenzae from Italy and Spain: data from the PROTEKT surveillance study, 1999-2000. J. Chemother. 15:226-234. [DOI] [PubMed] [Google Scholar]
- 26.York, M., K. L. Gibbs, F. Perdreau-Remington, and G. F. Brooks. 1999. Characterization of antimicrobial resistance in Streptococcus pyogenes isolates from the San Francisco bay area of northern California. J. Clin. Microbiol. 37:1727-1731. [DOI] [PMC free article] [PubMed] [Google Scholar]