Abstract
The intestinal epithelium is anatomically positioned to serve as the critical interface between the lumen and the mucosal immune system. In addition to MHC class I and II antigens, intestinal epithelia constitutively express the nonclassical MHC molecule CD1d, a transmembrane molecule with a short cytoplasmic tail expressed as a β2-microglobulin-associated 48-kDa glycoprotein and novel β2-microglobulin-independent 37-kDa nonglycosylated protein on intestinal epithelia. At present, it is not known whether extracellular ligands can signal intestinal epithelial CD1d. To define signaling of CD1d cytoplasmic tail, retrovirus-mediated gene transfer was used to generate stable cell lines expressing wild-type CD1d or a chimeric molecule (extracellular CD1d and cytoplasmic CD1a), and surface CD1d was triggered by antibody crosslinking. Although wild-type CD1d was readily activated (tyrosine phosphorylation), no demonstrable signal was evident in cell lines expressing the chimeric molecule. Subsequent studies revealed that anti-CD1d crosslinking specifically induces epithelial IL-10 mRNA and protein and is blocked by the tyrosine kinase inhibitor genistein. Further studies addressing epithelial-derived IL-10 revealed that anti-CD1d crosslinking attenuates IFN-γ signaling and that such attenuation is reversed by addition of functionally inhibitory IL-10 antibodies. These results define signaling through surface CD1d, and, importantly, they demonstrate that this pathway may serve to dampen epithelial proinflammatory signals.
Keywords: intestinal disease, inflammation, cytokine, mucosal immunology
The human CD1 gene family is composed of five members, four of which are known to be expressed in vivo—CD1a–d (1). These molecules are most closely related to MHC class I, on the basis of exon–intron organization and the ability to associate with β2-microglobulin. The homology to MHC class I, however, is quite low and suggests a marked divergence in function. In addition, the CD1 family members map outside the HLA locus and have limited polymorphism in the α1 and α2 domains, in contrast to the marked allelic polymorphism displayed by the classic class I MHC molecules. This limited polymorphism suggests that the CD1 molecules may function as unique antigen-presenting molecules for distinct classes of T cells and types of antigens (2). CD1b, for instance, may specifically present nonpeptide lipoglycan mycobacterial antigens to human CD4− CD8− T cells (2–4), and CD1d may present relatively hydrophobic antigens, as suggested by studies with the mouse homolog of this molecule (5, 6).
The cellular localization of the expressed CD1 gene family members further suggests that they perform these functions in specific tissue niches. CD1a, -b, and -c, which share considerable nucleotide homology (1), are constitutively expressed by a majority of thymocytes and certain types of professional antigen-presenting cells (7). The latter include Langerhans cells (8), B cells (9), and monocytes activated by inflammatory cytokines such as granulocyte/macrophage colony-stimulating factor and IL-4 (4, 10). In contrast, human CD1d, which is more homologous to mouse and rat CD1 homologs than to CD1a–c (1, 11, 12), is expressed in thymus and tissues outside the thymus (1, 13, 14). Extrathymic lymphoid expression is primarily limited to B cells (1). Similar to other class I-related molecules in the mouse [CD1 (15), the neonatal MHC class I receptor for IgG (16), and thymus leukemia antigen (17, 18)] and human [MIC or MHC class I chain-related genes (19)], CD1d is expressed on intestinal epithelial cells (IECs) (14, 20). Expression is predominantly localized to the apical and lateral regions of small- and large-intestinal epithelia, with a large subapical intracellular pool evident in cross section (21), placing it in a critical location for interaction with intestinal intraepithelial lymphocytes (iIELs).
The function of CD1d on IECs is poorly understood. It is not known whether CD1d signals through apically localized CD1d. Similar to CD1b and CD1c, the short cytoplasmic tail of CD1d (12 amino acids) contains a putative tyrosine-dependent internalization signal YXXZ (where Y signifies tyrosine, X is any amino acid, and Z is a hydrophobic amino acid) (22). To define the role of the CD1d cytoplasmic tail, and particularly this YXXZ motif, retrovirus-mediated gene transfer was used to generate stable cell lines expressing wild-type CD1d or a chimeric molecule expressing extracellular CD1d and cytoplasmic CD1a (CD1a lacks the YXXZ motif). Antibody crosslinking of extracellular wild-type CD1d, but not the chimeric CD1a/d, resulted in induction of bioactive epithelial IL-10. These results are functionally significant and define a potential autocrine pathway for regulated epithelial barrier function.
Materials and Methods
Cell Culture.
T84 cells were grown and passaged, as previously described (23). Culture conditions for CaCo-2 (24), HT29 (25), and Cl.19A (25) epithelial cells have been described previously. Epithelial cells were split near confluence by incubating in 0.1% trypsin/0.9 mM EDTA in Ca2+- and Mg2+-free PBS for 15–20 min. Cells were diluted in media only or in media containing recombinant human IFN-γ (a gift from Genentech) as indicated.
Retrovirus-mediated gene transfer of T84 cells with CD1d- and chimeric CD1d-containing vectors (CD1d ectodomain and CD1a cytoplasmic tail construct provided by Steven Balk, Harvard Medical School) was performed by a previously described technique (26). Briefly, CD1d or CD1a/d (27) cDNA was expressed from the viral long terminal repeat, and the dominant selectable marker (conferring resistance to the drug puromycin) was expressed from an internal phosphoglycerol kinase promoter. The PG-13 packaging cell line was used to create stable virus-producing lines after transfection of the retroviral constructs. T84 epithelial cells (106) were plated 24 h before infection. Cells were washed once, and viral supernatant supplemented with 4 μg/ml Polybrene was added to the adherent cells. After 8 h, fresh complete medium was added, and the cells were cultured for 48 h before puromycin selection.
Flow Cytometry.
T84 transfectants were analyzed by flow cytometry, as described in detail in ref. 26. Briefly, cells were trypsinized in a standard manner and stained with primary antibody for 30 min at 4°C in PBS + 0.2% FBS (staining buffer). Cells were washed two times in staining buffer, after which the secondary antibody [rhodamine-conjugated goat anti-mouse (Cappel)] was added for 30 min at 4°C. Cells were washed twice and immediately analyzed on a FACScan flow cytometer (Becton Dickinson). An isotype-matched primary antibody was used to define background staining. All data presented are ungated plots.
Epithelial CD1d Crosslinking/Immunoprecipitation/Western Blotting.
Surface CD1d was activated by standard crosslinking procedures. Briefly, anti-CD1d mAb [10 μg/ml (clone 51.1, a gift from Steven Balk and Steven Porcelli, Harvard Medical School)] was added to the apical surface of confluent epithelia grown on permeable supports (Corning) for 1 h at 37°C. Monolayers were washed, and goat anti-mouse antibody [10 μg/ml (Cappel)] was added as a crosslinker for periods of 0–20 min. Monolayers were washed in cold buffer and lysed (150 mM NaCl/25 mM Tris, pH 8.0/1% Triton X-100/1% Nonidet P-40) in the presence of protease inhibitors. CD1d was precipitated by the addition of 50 μl of preequilibrated protein-G Sepharose (Amersham Pharmacia) with overnight incubation. Washed immunoprecipitates were boiled in nonreducing sample buffer [2.5% SDS/0.38 M Tris (pH 6.8)/20% glycerol/0.1% bromophenol blue], separated by reducing SDS/PAGE, transferred to nitrocellulose, and blocked overnight in blocking buffer. Resultant blots were probed with anti-phosphotyrosine (mAb PY20; Transduction Laboratories, Lexington, KY) and peroxidase-conjugated goat anti-mouse secondary antibody (Cappel). Bands were visualized by enhanced chemiluminescence (ECL; Amersham Pharmacia). To localize CD1d, parallel blots were probed with anti-CD1d mAb (clone D5, provided by Steven Balk) as described above. Resulting bands were quantified from scanned images by using National Institutes of Health image software (Bethesda, MD).
Cytokine ELISAs.
Cytokine [IL-10 and tumor necrosis factor (TNF)] and chemokine (IL-8) levels were quantified by capture ELISA as described previously (28, 29). Preexposure to phorbol 12-myristate 13-acetate (10 ng/ml, 12 h) served as a positive control for induction of IL-8 (28) and TNF (29). In subsets of experiments, as indicated, monolayers were preexposed (30 min, 37°C) to the nonspecific tyrosine kinase inhibitor genistein (Calbiochem) before anti-CD1d crosslinking.
Quantification of IL-10 cDNA by PCR Amplification.
PCR amplification of cDNA was performed as described previously (30). Single-stranded cDNA was synthesized from 1 μg of RNA (DNA Polymerase High Fidelity PCR System, GIBCO). The PCR reaction for human IL-10 contained 1 μM each sense primer (5′-AGCTCAGCACTGCTCTGTTG-3′) and antisense primer (5′-GCATTCTTCACCTGCTGCTCCAC-3′) in a total volume of 50 μl. PCR products were then visualized on a 1% agarose gel containing 5 μg/ml ethidium bromide. A 427-bp fragment corresponding to IL-10 was observed. Human β-actin expression was examined in identical conditions as an internal control [sense primer (5′-TGACGGGGTCACCCACACTGTGCCCATCTA-3′) and antisense primer (5′-CTAGAAGCATTTGCGGTGGACGATGGAGGG-3′)], revealing a 661-bp amplified fragment.
Assessment of Epithelial Barrier Function.
Barrier function was assessed electrically by transepithelial resistance (TER) or by flux of fluorescein-conjugated dextran after CD1d crosslinking [with and without addition of IFN-γ (100 units/ml)] (28, 31). In subsets of experiments, monolayers were coincubated with functionally inhibitory goat anti-human IL-10 polyclonal antibodies (20 μg/ml, R&D Systems). To measure TER, the upper and lower reservoirs were interfaced with pairs of calomel and Ag/AgCl electrodes by 5% agar bridges. Resistance measurements were obtained with a dual-voltage clamp (University of Iowa) as described previously (31). Flux of FITC-labeled dextran [FITC-dextran, 3 kDa (Stokes radius, 17 Å), Molecular Probes] across epithelial monolayers was assayed exactly as described before (28). Samples were read on a fluorescent plate reader [Cytofluor 2300 (Millipore)], and flux rates were calculated from a daily standard curve.
Data Presentation.
Results were analyzed by comparison of means, using Student’s t test (for comparison of individual means) or by ANOVA (for comparison of dose responses and time courses) and are expressed as mean ± SEM for n experiments.
Results
Generation of T84 Epithelial Cell Lines Expressing Wild-Type CD1d and Chimeric CD1a/d.
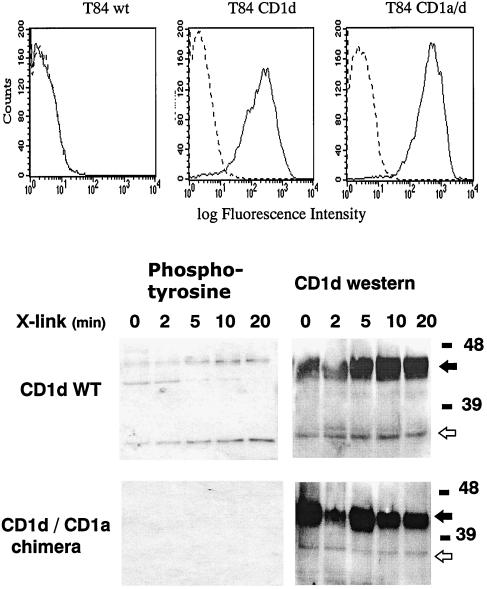
At present, the nature of signaling through epithelial cell surface CD1d is not known. The cytoplasmic tail of human CD1d, but not CD1a, bears a target domain for potential tyrosine kinase activity that consists of a tyrosine endocytic sorting motif (YXXZ) (32). To define these principles, we used retrovirus-mediated gene transfer to develop T84 epithelial cells overexpressing wild-type CD1d or a chimeric CD1d bearing the CD1a cytoplasmic tail (CD1a/d chimera), which lacks the YXXZ motif. Previous studies have shown that CD1d bearing the CD1a cytoplasmic tail is nonfunctional and remains restricted to the cell surface away from endosomes, consistent with the known function of the YXXZ motif. Fig. 1 Upper shows flow cytometric analysis of surface CD1d. This analysis revealed little surface CD1d in wild-type untransfected cells (Fig. 1 Upper Left). These findings are consistent with previous studies, in which CD1d surface expression is most readily detected by confocal microscopy or by surface biotinylation/immunoprecipitation (21). Similar analysis of CD1d and CD1a/d transfectants revealed a >2-log order increase in fluorescence over isotype-matched controls (Fig. 1 Upper Center and Right), confirming our transfection protocol.
Figure 1.
Cell surface staining and tyrosine phosphorylation of retrovirus-mediated overexpression of CD1d and CD1a/d chimera in T84 cells. (Upper) T84 wild-type cells (untransfected, Left) or T84 cells transfected with the wild-type CD1d molecule (Center) or CD1a/d molecule (Right) were stained with a mouse mAb specific for CD1d. Staining was detected with a rhodamine-conjugated secondary antibody specific for mouse IgG. The horizontal axes show the fluorescence intensities on a logarithmic scale and the vertical axes show the relative cell numbers. (Lower) T84 cell CD1d (upper blots) or CD1a/d chimera (lower blots) cell lines were grown to confluence on permeable supports. Apical CD1d was crosslinked with anti-CD1d mAb 51.1 (10 μg/ml) for 0–20 min. CD1d was immunoprecipitated by addition of protein G-Sepharose. Precipitates were resolved by SDS/PAGE, and Western blots were probed with anti-phosphotyrosine (Left). To localize CD1d, parallel blots were probed with anti-CD1d (Right). and indicate 37- and 48-kDa bands, respectively. One of three experiments is shown.
Epithelial CD1d Crosslinking Induces Tyrosine Phosphorylation.
We next determined whether the cytoplasmic tyrosine on CD1d is a substrate for tyrosine kinase(s). Anti-CD1d crosslinking was used to trigger CD1d. Crosslinking was initiated by addition of anti-CD1d (clone 51.1, 10 μg/ml) followed by goat anti-mouse secondary antibody as a crosslinker. Immunoprecipitates were then blotted with anti-phosphotyrosine. As shown in Fig. 1 Lower, anti-CD1d crosslinking resulted in a time-dependent tyrosine phosphorylation of both forms of CD1d described on epithelia (maximal 3.8- and 6.2-fold increases by densitometry for the 48- and 37-kDa forms, respectively). Interestingly, a pattern of dephosphorylation was observed with a protein at ≈45 kDa. The identity of this protein is not known at the present time. As a control for these experiments, crosslinking MHC class I (mAb W6/32, 10 μg/ml) and analysis of tyrosine phosphorylation of CD1d resulted in no observable pattern (data not shown). Moreover, cells expressing the chimeric CD1a/d revealed no observable tyrosine phosphorylation, consistent with a dominant-negative phenotype and indicative that the CD1d cytoplasmic tail is critical for recruitment of tyrosine kinase activity. Similar results of tyrosine phosphorylation induction were observed with wild-type untransfected T84 cells (data not shown), which we have previously shown express both the 37- and 48-kDa forms of CD1d (21). To localize CD1d, parallel blots were probed by Western blot analysis with anti-CD1d (clone D5). Consistent with previous reports, these results revealed a heavily glycosylated 48-kDa and a less glycosylated 37-kDa form of CD1d (21, 33, 34). These data demonstrate that the CD1d cytoplasmic tail serves as a substrate for tyrosine kinase activity and reveal that expression of the chimeric molecule (CD1a/d) functions as a dominant-negative mutant in this system.
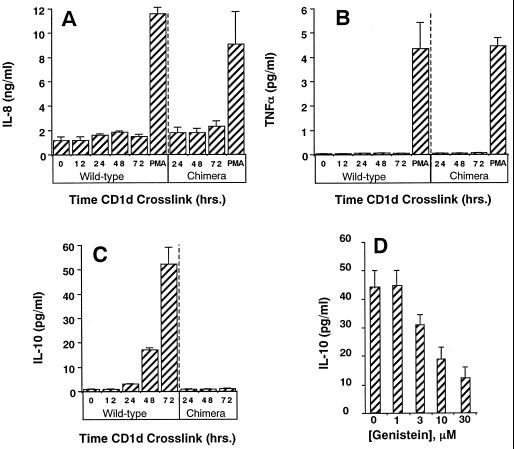
Anti-CD1d Crosslinking Specifically Induces Epithelial IL-10.
We next determined whether induction of CD1d tyrosine phosphorylation was functional. Recent studies have demonstrated that intestinal epithelia are rich sources of both chemokines and cytokines, and therefore we screened epithelial cell supernatants for a representative chemokine (IL-8), proinflammatory cytokine (TNF), and anti-inflammatory cytokine (IL-10) after CD1d crosslinking in wild-type and chimeric CD1a/d cell lines. As shown in Fig. 2, these studies revealed a time-dependent induction of IL-10 (P < 0.01), with a >50-fold induction by 72 h. Neither IL-8 nor TNF was significantly influenced by anti-CD1d crosslinking. Phorbol 12-myristate 13-acetate (10 ng/ml) served as a positive control for both IL-8 and TNF (28, 29) in this analysis. Importantly, induction of IL-10 was not observed in cells expressing the CD1a/d chimeric molecule (P = not significant).
Figure 2.
Anti-CD1d crosslinking induces epithelial release of IL-10; role for the CD1d cytoplasmic tail and tyrosine phosphorylation. T84 cell lines CD1d (wild-type) or CD1a/d chimera (chimeric) cell lines were grown to confluence on permeable supports. Apical CD1d was crosslinked, and soluble cell supernatants were harvested over the indicated periods of time and assayed for IL-8 (A), TNF (B), or IL-10 (C) by ELISA. PMA, phorbol 12-myristate 13-acetate. Results represent the mean ± SEM for 7–10 monolayers in each condition. In D, apical CD1d was crosslinked in the presence of indicated concentrations of genistein, and soluble cell supernatants were harvested 72 h after crosslinking and assayed for IL-10 by ELISA. Results represent the mean ± SEM for 6–8 monolayers in each condition.
To define the precise role of tyrosine phosphorylation in the induction of epithelial IL-10, epithelia were preexposed to the nonspecific tyrosine kinase inhibitor genistein (concentration range, 1–30 μM) and examined for induction of IL-10 at 72 h after anti-CD1d crosslinking. As can be seen in Fig. 2D, genistein blocked epithelial IL-10 release in a concentration-dependent fashion (ANOVA, P < 0.01), with a 72% ± 8% inhibition at 30 μM genistein. These data indicate the likelihood that the cytoplasmic CD1d tyrosine residue is critical for induction of epithelial IL-10 by anti-CD1d crosslinking.
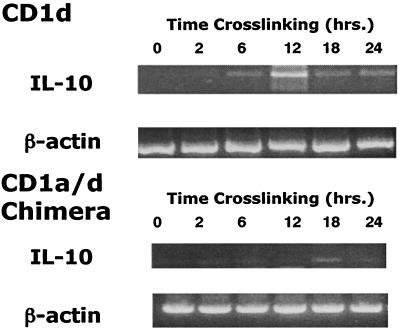
To confirm these observations and to define induction of IL-10 message, reverse transcription–PCR analysis was performed on RNA derived from anti-CD1d-crosslinked T84 cells. As shown in Fig. 3, these studies revealed a time-dependent induction of IL-10 mRNA, with maximal induction at 12 h after CD1d crosslinking. Consistent with our protein findings (see above), similar analysis of the CD1a/d chimeric cell line revealed no significant induction of IL-10 in the CD1a/d chimera.
Figure 3.
Quantification of IL-10 message by PCR amplification. Reverse transcription–PCR was examined in CD1d wild-type (Upper) and CD1a/d chimeric (Lower) cell lines exposed to anti-CD1d crosslinking for indicated periods of time. After crosslinking, total RNA was isolated, treated with DNase I, and amplified by reverse transcription–PCR for IL-10 message or for control β-actin. Data shown represent three experiments.
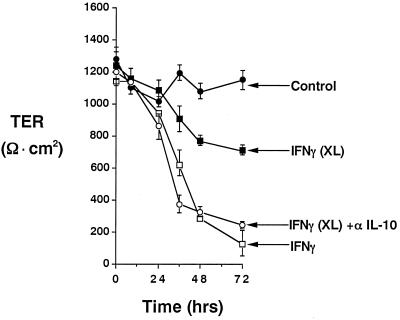
IL-10 Elicited by Anti-CD1d Is Functional.
It was recently reported that IECs, specifically T84 cells, express functional surface receptors for IL-10 (35). Ligation of surface receptors with recombinant cytokine blocks IFN-γ-induced increases in epithelial permeability (36) through down-regulation of the tight junction protein ZO-1 (32). Thus, we determined whether IL-10 elicited by anti-CD1d crosslinking blocks increased T84 monolayer permeability (reflected as a decrease in TER and a concomitant increase in paracellular flux) in response to IFN-γ. As shown in Fig. 4, and consistent with previous studies (36), addition of recombinant IFN-γ (100 units/ml) resulted in a time-dependent decrease in TER (ANOVA, P < 0.001 compared with no IFN-γ) with a 90% ± 7.3% fall in TER at 72 h. Parallel analysis of 3-kDa FITC-dextran flux at 72 h confirmed a significant increase (paracellular flux of 13 ± 2.1 vs. 37 ± 4.3 pM/cm2 per min in the absence and presence of IFN-γ, respectively, P < 0.025). Anti-CD1d crosslinking [conditions that liberate epithelial IL-10 (see Figs. 1 and 2)] 48 h before the addition of recombinant IFN-γ resulted in attenuation of IFN-γ-induced permeability [33% ± 2.7% fall in TER compared with 90% ± 7.3% fall without crosslinking (P < 0.01)]. Addition of anti-IL-10 mAb (10 μg/ml) reversed the attenuation of IFN-γ-induced permeability by crosslinking [80% ± 2.2% fall in TER compared with 33% ± 2.7% fall without anti-IL-10 (P < 0.01)], indicating the likelihood that epithelial-derived IL-10 is bioactive and functionally attenuates IFN-γ signaling in intestinal epithelia.
Figure 4.
Epithelial-cell-derived IL-10 blocks IFN-γ-induced epithelial permeability. T84 cells overexpressing CD1d were grown as monolayers on permeable supports. Some monolayers were anti-CD1d crosslinked (indicated as XL) for 48 h, followed by the addition of IFN-γ (100 units/ml) in the presence and absence of anti-IL-10, as indicated. Monolayer TER was monitored by standard voltage clamp techniques. Results are expressed as the mean ± SD for four individual monolayers in each condition. One of three representative experiments is shown.
Discussion
We demonstrate here that the CD1d cytoplasmic tail signals in response to extracellular activation (antibody crosslinking), resulting in rapid and sustained production of the anti-inflammatory cytokine IL-10, which functionally attenuates IFN-γ signaling. Remarkably, exchange of the short CD1d cytoplasmic tail with that of CD1a (which does not bear a putative tyrosine internalization signal) results in a dominant-negative phenotype. Taken together, these data suggest that ligation of surface CD1d may subserve mucosal immune responses with anti-inflammatory signaling.
The current view of the function of CD1d on IECs is, at best, poorly understood. The present studies with antibody crosslinking to trigger CD1d provide the foundation for better understanding this complex molecule and reveal a number of salient features about CD1d signaling, in particular the YXXZ motif of the cytoplasmic tail. First, mutants that lack the wild-type CD1d cytoplasmic domain manifest as dominant-negative mutants with antibody crosslinking. The YXXZ motif is classically viewed as a tyrosine-dependent internalization domain and, for CD1d, specifically directs internalization but not basolateral sorting (32). Second, the tyrosine residue of the YXXZ motif is critical to induction of IL-10 in response to antibody crosslinking. The tyrosine of the YXXZ motif accounts for the only tyrosine residue in the short cytoplasmic domain of CD1d (22), and CD1d tyrosine phosphorylation was evident in immunoprecipitations. Third, because the nonspecific tyrosine kinase inhibitor genistein substantially inhibited this response, the tyrosine residue appears to orchestrate specific functional responses, including induction of epithelial IL-10. It is important that the amount of IL-10 produced by IECs (picograms per milliliter) in these studies is less than cells conventionally thought to release IL-10 [e.g., T cells, (nanograms per milliliter)]. It is important that the surface area of the intestine covered by epithelial cells is orders of magnitude larger than that covered by T cells, and thus, even with smaller amounts produced per epithelial cell, the total quantity of epithelial-derived cytokine can be quite large and physiologically important in this regard. Additionally, given the architecture of the paracellular space of the intact epithelium (long cylindrical space sealed by the tight junction), it is probable that epithelial cell-derived mediators (growth factors, cytokines, and lipids) concentrate within this space, and, with cytokine delivered directly to the receptor in this fashion (autocrine), the relative bioactivity for these mediators may be enhanced manyfold. This aspect of autocrine signaling has been previously demonstrated for epithelial-cell-derived TNF (29, 37). Taken together, these data define a critical role for the cytoplasmic domain in CD1d functional responses, as has been previously suggested for CD1b (38).
It is not known whether iIELs might functionally crosslink CD1d in the intact intestine and whether such crosslinking might induce epithelial IL-10, in a fashion similar to that in the mouse in vivo (6). Previous studies have suggested that iIELs can recognize CD1d on B cell transfectants in a cytolytic assay, suggesting that CD1d may be a functional ligand in vivo under the appropriate circumstances (39) and that antibodies directed against CD1d block T cell–IEC interactions in modified mixed lymphocyte reactions in vitro (40). To perform such a function, similar signal transduction through lateral CD1d (as opposed to apical CD1d studied here) would be necessary, because iIELs localize to the lateral membrane surface of IECs in vivo. We have not examined lateral membrane CD1d crosslinking and signaling in detail. These studies are complicated by the fact that antibody access to the IEC lateral membrane surface may be limited in confluent, high-resistance monolayers such as those studied here (T84 cells). Additionally, it is not known whether accessory molecules (e.g., glycoprotein 180) (41) might function as costimulators of induction of CD1d tyrosine phosphorylation. As a caveat to this work, recent studies clearly indicate that MHC class I can signal in T cell lines and human endothelial cells, the ligation of which results in induction of cyclin E-associated kinases and concomitant cell proliferation (42). Future studies with iIELs and/or with smaller, more native antigens (e.g., galactosylceramide lipids) will be necessary to define these principles.
To define whether epithelial-cell-derived IL-10 is functional in this model system, we used IFN-γ signaling as a readout. Multiple functional endpoints have been studied in IECs in response to IFN-γ, and we have proposed that IFN-γ induces a “phenotype switch” on IECs from one exhibiting classical epithelial functions (vectorial fluid and electrolyte transport barrier function) to one exhibiting significant immune accessory function [regulated MHC class I and II and CD1d expression, expression of neutrophil/intraepithelial lymphocyte ligands, and cytokine and chemokine production (31, 43–46)]. Others have demonstrated that these IFN-γ-elicited signaling pathways (specifically increased permeability) are dampened by recombinant IL-10 (35). Our studies confirm these previous findings and further define that epithelia are a source of IL-10 in response to anti-CD1d crosslinking in vitro. At present, it is not clear how IL-10 modulates IFN-γ bioactivity in this model epithelium. Although we have not directly addressed this issue, it was recently demonstrated that IL-10 specifically suppresses tyrosine phosphorylation of signal transducer and activator of transcription-1 (STAT-1), a component of the IFN-γ-induced DNA complex (47).
The in vivo correlates of IL-10 and CD1d revealed by using this model system need to be identified. CD1d is constitutively expressed by IECs of the small and large human intestine in vivo (14, 20, 21) and may be up-regulated by intestinal inflammation in vivo (14). It is important that CD1d exists in a prime location for direct modulation of iIEL-epithelial interactions (along the lateral membrane surface). The studies presented here support an active role for epithelial CD1d in down-regulation of responses to luminal antigens. In particular, epithelial cells are demonstrated sources of IL-10 (48, 49), and significant evidence exists that IL-10 contributes to the development of mucosal tolerance. For instance, IL-10-deficient mice develop an inflammatory bowel disease-like condition, administration of IL-10 restores tolerance to indigenous flora in mice with inflammatory bowel disease, and IL-10 accompanies the induction of IL-4 in animals that have become tolerant of low-dose antigen (50). Given the further role of IL-10 in regulating important subsets of T cells dedicated to IL-10 production and down-regulation of colitis, IEC responses to either luminal or T cell stimuli may directly regulate this important population of cells (46). In support of this idea, it was recently shown that glycosphingolipids induce T cell IL-10 production and that such induction parallels our findings with tyrosine kinase dependency (51). These studies, taken together with the proposed role of CD1d in lipid binding and processing, unveil the unique possibility that CD1d contributes significantly to the regulation of IFN-γ-mediated epithelial responses (barrier function, ion transport, MHC molecule expression, etc.) and potentially to oral tolerance directed toward lipid antigens in the intestine.
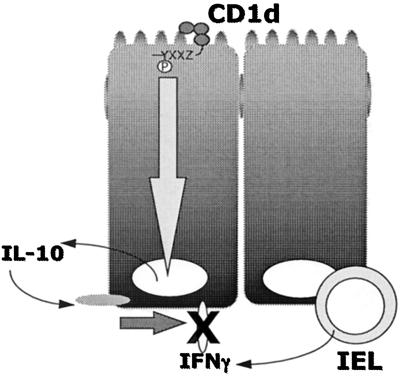
In summary, these results define a signal transduction pathway through surface activation of epithelial CD1d that defines a potential pathway to dampen proinflammatory signals at the level of mucosal epithelia. Fig. 5 depicts a proposed model of CD1d signaling in polarized IECs. We speculate that signaling through apical CD1d regulates inflammatory processes (e.g., those provided by IFN-γ) through the autocrine actions of epithelial-derived IL-10.
Figure 5.
Proposed model of CD1d signaling in polarized intestinal epithelia. Results from these studies define a signal transduction pathway through surface activation of epithelial CD1d and illustrate that this pathway may serve to dampen proinflammatory signals at the level of mucosal epithelia through the autocrine actions of epithelial-cell-derived IL-10.
Acknowledgments
This work was supported by National Institutes of Health research grants DK50189 and HL60569 to S.P.C.; DK44319, DK53056, and DK51362 to R.S.B., and DK02564 to G.T.F. and by a grant from the Crohn’s and Colitis Foundation of America.
Abbreviations
- IEC
intestinal epithelial cell
- iIEL
intestinal intraepithelial lymphocyte
- TNF
tumor necrosis factor
- TER
transepithelial resistance
Footnotes
This paper was submitted directly (Track II) to the PNAS office.
References
- 1.Calabi F, Bradbury A. Tissue Antigens. 1991;37:1–9. doi: 10.1111/j.1399-0039.1991.tb01836.x. [DOI] [PubMed] [Google Scholar]
- 2.Shawar S M, Vyas J M, Rodgers J R, Rich R R. Annu Rev Immunol. 1994;12:839–880. doi: 10.1146/annurev.iy.12.040194.004203. [DOI] [PubMed] [Google Scholar]
- 3.Sieling P A, Chatterjee D, Porcelli S A, Prigozy T I, Mazzaccaro R J, Soriano T, Bloom B R, Brenner M B, Kronenberg M, Brennan P J, Modlin R L. Science. 1995;269:227–230. doi: 10.1126/science.7542404. [DOI] [PubMed] [Google Scholar]
- 4.Porcelli S, Morita C T, Brenner M B. Nature (London) 1992;360:593–598. doi: 10.1038/360593a0. [DOI] [PubMed] [Google Scholar]
- 5.Castano A R, Tangri S, Miller J E, Holcombe H R, Jackson M R, Huse W D, Kronenberg M, Peterson P A. Science. 1995;269:223–226. doi: 10.1126/science.7542403. [DOI] [PubMed] [Google Scholar]
- 6.Bendelac A, Rivera M N, Park S H, Roark J H. Annu Rev Immunol. 1997;15:535–562. doi: 10.1146/annurev.immunol.15.1.535. [DOI] [PubMed] [Google Scholar]
- 7.Reinherz E L, Kung P C, Goldstein G, Levey R H, Schlossman S F. Proc Natl Acad Sci USA. 1980;77:1588–1592. doi: 10.1073/pnas.77.3.1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fithian E, Kung G, Goldstein G, Rubenfeld M, Fenoglio C, Edelson R L. Proc Natl Acad Sci USA. 1981;78:2541–2544. doi: 10.1073/pnas.78.4.2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Small T N, Knowles R W, Keever C, Kernan N A, Collins N, O’Reilly R J, Dupont B, Flomenberg N. J Immunol. 1987;138:2864–2870. [PubMed] [Google Scholar]
- 10.Kasinrerk W, Baumruker T, Majdic O, Knapp W, Stockinger H. J Immunol. 1993;150:579–584. [PubMed] [Google Scholar]
- 11.Balk S P, Bleicher P A, Terhorst C. J Immunol. 1991;146:768–774. [PubMed] [Google Scholar]
- 12.Ichimiya S, Kikuchi K, Matsuura A. J Immunol. 1994;153:1112–1120. [PubMed] [Google Scholar]
- 13.Bradbury A, Belt K T, Neri T M, Milstein C, Calabi F. EMBO J. 1988;7:3081–3086. doi: 10.1002/j.1460-2075.1988.tb03173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Canchis P W, Bhan A K, Landau S B, Yang L, Balk S P, Blumberg R S. Immunology. 1993;80:561–565. [PMC free article] [PubMed] [Google Scholar]
- 15.Bleicher P A, Balk S P, Hagen S J, Blumberg R S, Flotte T J, Terhorst C. Science. 1990;250:679–682. doi: 10.1126/science.1700477. [DOI] [PubMed] [Google Scholar]
- 16.Simister N E, Mostov K E. Nature (London) 1989;337:184–187. doi: 10.1038/337184a0. [DOI] [PubMed] [Google Scholar]
- 17.Wu M, VanKaer L, Itohara S, Tonegawa S. J Exp Med. 1991;174:213–218. doi: 10.1084/jem.174.1.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hershberg R, Eghtesady P, Sydora B, Brorson K, Cheroutre H, Modlin R, Kronenberg M. Proc Natl Acad Sci USA. 1990;87:9727–9731. doi: 10.1073/pnas.87.24.9727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bahram S, Bresnahan M, Geraghty D E, Spies T. Proc Natl Acad Sci USA. 1994;91:6259–6263. doi: 10.1073/pnas.91.14.6259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blumberg R S, Terhorst C, Bleicher P, McDermott F V, Allan C H, Landau S B, Trier J S, Balk S P. J Immunol. 1991;147:2518–2524. [PubMed] [Google Scholar]
- 21.Somnay-Wadgaonkar K, Nusrat A, Kim H S, Canchis W P, Balk S P, Colgan S P, Blumberg R S. Int Immunol. 1999;11:383–392. doi: 10.1093/intimm/11.3.383. [DOI] [PubMed] [Google Scholar]
- 22.Balk S P, Bleicher P A, Terhorst C. Proc Natl Acad Sci USA. 1989;86:252–256. doi: 10.1073/pnas.86.1.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dharmsathaphorn K, Mandel K G, McRoberts J, Tisdale L D, Masui H. Am J Physiol. 1984;246:G204–G208. doi: 10.1152/ajpgi.1984.246.2.G204. [DOI] [PubMed] [Google Scholar]
- 24.Grasset E, Bernabeu J, Pinto M. Am J Physiol. 1985;89:C339–C349. doi: 10.1152/ajpcell.1985.248.5.C410. [DOI] [PubMed] [Google Scholar]
- 25.Morris A P, Cunningham S A, Benos D J, Frizzell R A. J Biol Chem. 1992;267:5575–5583. [PubMed] [Google Scholar]
- 26.Hershberg R M, Framson P E, Cho D H, Lee L Y, Kovats S, Beitz J, Blum J S, Nepom G T. J Clin Invest. 1997;100:204–215. doi: 10.1172/JCI119514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Exley M, Porcelli S, Furman M, Garcia J, Balk S. J Exp Med. 1998;188:867–876. doi: 10.1084/jem.188.5.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colgan S P, Dzus A L, Parkos C A. J Exp Med. 1996;184:1003–1015. doi: 10.1084/jem.184.3.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor C T, Dzus A L, Colgan S P. Gastroenterology. 1998;114:657–668. doi: 10.1016/s0016-5085(98)70579-7. [DOI] [PubMed] [Google Scholar]
- 30.Colgan S P, Morales V M, Madara J L, Balk S P, Blumberg R S. Am J Physiol. 1996;271:C276–C283. doi: 10.1152/ajpcell.1996.271.1.C276. [DOI] [PubMed] [Google Scholar]
- 31.Colgan S P, Parkos C A, Matthews J B, D’Andrea L, Awtrey C S, Lichtman A, Delp C, Madara J L. Am J Physiol. 1994;267:C402–C410. doi: 10.1152/ajpcell.1994.267.2.C402. [DOI] [PubMed] [Google Scholar]
- 32.Youakim A, Ahdiel M. Am J Physiol. 1999;276:G1279–G1288. doi: 10.1152/ajpgi.1999.276.5.G1279. [DOI] [PubMed] [Google Scholar]
- 33.Kim H S, Garcia J, Exley M, Johnson K W, Balk S P, Blumberg R S. J Biol Chem. 1999;274:9289–9295. doi: 10.1074/jbc.274.14.9289. [DOI] [PubMed] [Google Scholar]
- 34.Balk S P, Burke S, Polischuk J E, Frantz M E, Yang L, Porcelli S, Colgan S P, Blumberg R S. Science. 1994;265:259–262. doi: 10.1126/science.7517575. [DOI] [PubMed] [Google Scholar]
- 35.Madsen K L, Lewis S A, Taverini M N, Hibbard J, Fedorak R N. Gastroenterology. 1997;113:151–159. doi: 10.1016/s0016-5085(97)70090-8. [DOI] [PubMed] [Google Scholar]
- 36.Madara J L, Stafford J. J Clin Invest. 1989;83:724–727. doi: 10.1172/JCI113938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taylor C T, Fueki N, Agah A, Hershberg R M, Colgan S P. J Biol Chem. 1999;274:19447–19450. doi: 10.1074/jbc.274.27.19447. [DOI] [PubMed] [Google Scholar]
- 38.Jackman R M, Stenger S, Lee A, Moody D R, Rogers R A, Niazi K R, Sugita M, Modlin R L, Peters P J, Porcelli S A. Immunity. 1998;8:341–351. doi: 10.1016/s1074-7613(00)80539-7. [DOI] [PubMed] [Google Scholar]
- 39.Balk S P, Ebert E C, Blumenthal R L, McDermott F V, Wucherpfenning K W, Landau S B, Blumberg R S. Science. 1991;253:1411–1415. doi: 10.1126/science.1716785. [DOI] [PubMed] [Google Scholar]
- 40.Panja A, Blumberg R S, Balk S P, Mayer L. J Exp Med. 1993;178:1115–1119. doi: 10.1084/jem.178.3.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yio X Y, Mayer L. J Biol Chem. 1997;272:12786–12792. doi: 10.1074/jbc.272.19.12786. [DOI] [PubMed] [Google Scholar]
- 42.Nath N, Bian H, Reed E F, Chellappan S P. J Immunol. 1999;162:5351–5358. [PubMed] [Google Scholar]
- 43.Colgan S P, Resnick M B, Parkos C A, Delp-Archer C, Bacarra A E, Weller P F, Madara J L. J Immunol. 1994;153:2122–2129. [PubMed] [Google Scholar]
- 44.Holmgren J, Fryklund J, Larsson H. Scand J Immunol. 1989;30:499–503. doi: 10.1111/j.1365-3083.1989.tb02456.x. [DOI] [PubMed] [Google Scholar]
- 45.Kaoutzani P, Colgan S P, Cepek K L, Grant Burkhard P, Carlson S, Delp-Archer C, Brenner M B, Madara J L. J Clin Invest. 1994;94:788–796. doi: 10.1172/JCI117398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mayer L, Eisenhardt D, Salomon P, Bauer W, Plous R, Piccinini L. Gastroenterology. 1991;100:3–12. doi: 10.1016/0016-5085(91)90575-6. [DOI] [PubMed] [Google Scholar]
- 47.Ito S, Ansari P, Sakatsume M, Dickensheets H, Vazquez N, Donnelly R P, Larner A C, Finbloom D S. Blood. 1999;93:1456–1463. [PubMed] [Google Scholar]
- 48.Eckmann L, Jung H C, Schurer-Maly C, Panja A, Morzycka-Wroblewska E, Kagnoff M F. Gastroenterology. 1993;105:1689–1697. doi: 10.1016/0016-5085(93)91064-o. [DOI] [PubMed] [Google Scholar]
- 49.Galliaerde V, Desvignes C, Peyron E, Kaiserlian D. Eur J Immunol. 1995;25:1385–1390. doi: 10.1002/eji.1830250537. [DOI] [PubMed] [Google Scholar]
- 50.Mowat A M, Weiner H L. In: Mucosal Immunology. Ogra P, Mestecky J, Lamm M E, Strober W, Bienenstock J, McGhee J R, editors. Vol. 2. San Diego: Academic; 1999. pp. 587–618. [Google Scholar]
- 51.Kanda N. Biochem Biophys Res Commun. 1999;256:41–44. doi: 10.1006/bbrc.1999.0281. [DOI] [PubMed] [Google Scholar]