Abstract
Objective
To assess the prevalence, correlates, and age of onset of DSM-IV substance use disorders (SUDs) among adult inhalant users.
Methods
Analyses were based on structured psychiatric interviews of a nationally representative sample of 43,093 U.S. adults.
Results
The lifetime prevalence of SUDs among adult inhalant users was 96%. Alcohol (87%), marijuana (68%), nicotine (58%), cocaine (35%), hallucinogen (31%), and stimulant (28%) use disorders were more prevalent than inhalant use disorders (19%). An estimated 62% of inhalant users met criteria for a past-year SUD. Less education, residence in non-metropolitan areas, early onset of inhalant use, and a history of substance abuse treatment were associated with increased odds of having an inhalant use disorder. Inhalant users who were under age 30 or who were members of families with low incomes had increased odds of having nicotine dependence and an alcohol or drug use disorder in the past year. Compared with substance users without a history of inhalant use, inhalant users, on average, initiated use of cigarettes, alcohol, and almost all other drugs at younger ages, and had a higher lifetime prevalence of nicotine, alcohol, and any drug use disorder.
Conclusions
Lifetime and past-year SUDs are prevalent among adults with a history of inhalant use.
Keywords: Comorbidity, Inhalant use, Nicotine dependence, Solvent use, Substance use disorders
1. Introduction
In 2005, approximately 877,000 Americans aged 12 years or older used inhalants for the first time within the past 12 months, 28% of whom were adults aged 18 years or older when they first used inhalants (Substance Abuse and Mental Health Services Administration, 2006). While it is known that inhalant use is associated with cardiac, renal, hepatic, and neurological morbidity and mortality (Anderson and Loomis, 2003), less is known about the prevalence and correlates of substance use disorders (SUDs) among adult inhalant users—the focus of this study.
Studies of inhalant use have typically focused on youth, high-risk subgroups, or convenience samples (Compton et al., 1994; Fendrich et al., 1997; Sakai et al., 2004). These investigations, in general, have identified detrimental health and social conditions associated with inhalant use, including use and abuse of other substances. Wu and Ringwalt (2006) found that 8% of past-year adult inhalant users met criteria for an inhalant use disorder (IUD) and that inhalant use was associated with use of multiple drugs. More recently, Wu and Howard (2007a) examined adult inhalant users in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) and found that, among adults who reported a history of inhalant use, 70% met criteria for one or more lifetime personality, mood, or anxiety disorders, and 38% had experienced a mood or anxiety disorder in the past year.
The present study adds to the findings from prior studies of adult samples (Compton et al., 1994; Wu and Ringwalt, 2006; Wu and Howard, 2007a) by addressing gaps in our knowledge of patterns of SUDs in a representative sample of adult inhalant users. We examined the following questions: Are specific SUDs prevalent among adults with a history of inhalant use? Do inhalant users initiate inhalant use at younger ages than their initiation of other drug use? Do inhalant users start their substance use at younger ages than do substance users without a history of inhalant use? What subgroups of inhalant users have comparatively high odds of experiencing SUDs? Because prior studies indicate sex differences in inhalant use and psychiatric disorders (Wu and Ringwalt, 2006; Wu and Howard, 2007a), we also explored sex variations in SUDs.
2. Methods
2.1. Data source
The NESARC is a longitudinal investigation of a nationally representative sample of 43,093 U.S. adult residents (Grant et al., 2004). It is the largest comorbidity study ever conducted. NESARC’s target population was the civilian, non-institutionalized adult residents of all 50 states and the District of Columbia. Respondents were selected to participate in NESARC using a multistage sampling design. To increase the accuracy of national estimates for subgroups, Hispanics, African Americans, and respondents aged 18–24 years were oversampled. The overall survey response rate was 82%. Detailed designs of the NESARC are reported elsewhere (Grant et al., 2004).
2.2. Study variables
Drug use refers to the use of illicit drugs or the nonmedical use of prescription drugs (use without a doctor’s prescription, in greater amounts, more often, or longer than prescribed). Respondents were asked whether they have ever used each of nine categories of drugs, including sedatives, tranquilizers, opioids, stimulants, marijuana, inhalants, cocaine/crack, hallucinogens, and heroin. Inhalant use was assessed by the question: “Have you EVER used inhalants or solvents, for example amyl nitrite, nitrous oxide, glue, toluene, or gasoline?” Participants who responded affirmatively to this question completed additional inhalant-specific items assessing use in the prior 12 months, recency of use, symptoms of IUD, and age at first use of any inhalant. Age at first use of other drugs was also recorded. Age of first alcohol use was defined as the age when the respondent started drinking, not counting small tastes or sips. For tobacco use (cigarettes, cigars, a pipe, snuff, or chewing tobacco), we examined age of first cigarette use because 94% of tobacco users in NESARC smoked cigarettes.
Substance use disorders (SUDs) were assessed with the Alcohol Use Disorders and Associated Disabilities Interview Schedule–Diagnostic and Statistical Manual of Mental Disorders–Fourth Revision (AUDADIS-DSM-IV). We examined alcohol use disorders (AUDs), nicotine dependence (ND), and nine specific drug use disorders (DUDs) (inhalants, marijuana, cocaine, heroin, hallucinogens, opioids, sedatives, stimulants, and tranquilizers). A binary DUD variable was defined to identify respondents who met abuse or dependence criteria for any of the nine DUDs. We also created a variable to summarize the number of the 11 SUDs (AUDs, ND, and nine specific DUDs) that respondents had experienced.
A history of substance abuse treatment was defined as having ever used any treatment or service for alcohol or drug use at any location (Wu and Howard, 2007a). A family history of psychopathology included any self-reported, positive family history of alcohol or drug use problems, depression, or antisocial behavior among any of the respondent’s biological family members (Wu and Howard, 2007a). We also examined respondents’ age, sex, race/ethnicity, education, marital status, annual family income, and area of residence (urbanicity).
2.3. Statistical analysis
Statistical analysis was conducted on the public-use data file of the 2001–2002 NESARC. Sample characteristics are reported in details elsewhere (Grant et al., 2004). Data were weighted and analyzed with SUDAAN software (Research Triangle Institute, 2002). We conducted logistic regression procedures to identify correlates of SUDs among all inhalant users.
3. Results
3.1. SUDs among inhalant users
Of all respondents aged 18–98 years (N = 43,093), 1.7% (N = 664) reported a history of inhalant use (lifetime use). Overall, 96% of lifetime inhalant users met criteria for one SUD, and close to one in five (19%) developed an IUD (Table 1). Sex differences were observed, with men displaying higher lifetime prevalence rates than women of marijuana, cocaine, sedative, and tranquilizer use disorders.
Table 1.
Prevalence of DSM-IV substance use disorders among adult lifetime inhalant users in 2001–2002 NESARC, overall and by sex (N = 664)
| Prevalence, % | Lifetime substance use disorders | Past-year substance use disorders | ||||
|---|---|---|---|---|---|---|
| Overall | Men | Women | Overall | Men | Women | |
| Sample size, N | 664 | 470 | 194 | 664 | 470 | 194 |
|
| ||||||
| Nicotine | 57.8 | 56.3 | 62.2 | 44.5 | 43.5 | 47.4 |
|
| ||||||
| Alcohol | 87.2 | 88.4 | 84.0 | 37.9 | 40.4 | 30.9a |
|
| ||||||
| Any druga | 79.7 | 82.1 | 72.7a | 19.6 | 21.3 | 14.6 |
|
| ||||||
| Any alcohol or drug | 94.4 | 95.2 | 91.9 | 44.4 | 48.1 | 34.0b |
|
| ||||||
| Inhalants | 19.4 | 20.3 | 16.8 | 1.4 | 1.8 | 0.3 |
|
| ||||||
| Marijuana | 67.8 | 72.4 | 54.4b | 15.4 | 17.6 | 9.1a |
|
| ||||||
| Hallucinogens | 30.6 | 31.8 | 27.1 | 2.6 | 2.9 | 1.9 |
|
| ||||||
| Stimulants | 28.1 | 28.0 | 28.5 | 2.4 | 1.6 | 4.7 |
|
| ||||||
| Sedatives | 17.1 | 19.2 | 10.7a | 1.2 | 0.9 | 1.9 |
|
| ||||||
| Tranquilizers | 17.6 | 19.7 | 11.5a | 1.6 | 2.1 | 0.0 |
|
| ||||||
| Opioids | 20.0 | 21.5 | 15.6 | 3.3 | 3.8 | 1.8 |
|
| ||||||
| Cocaine | 35.4 | 38.4 | 26.8a | 5.0 | 5.9 | 2.3 |
|
| ||||||
| Heroin | 4.8 | 5.0 | 4.2 | 0.8 | 0.3 | 2.2 |
|
| ||||||
| Number of substance use disordersb | ||||||
| 0 diagnoses | 4.0 | 3.9 | 4.4 | 38.0 | 37.6 | 39.1 |
| 1–2 | 33.1 | 31.7 | 37.3 | 50.2 | 50.5 | 49.4 |
| 3–5 | 40.1 | 39.1 | 42.8 | 11.8 | 11.9 | 11.5 |
| 6–11 | 22.8 | 25.4 | 15.5 | ….. | ….. | ….. |
|
| ||||||
| Any disorder | 96.0 | 96.1 | 95.6 | 62.0 | 62.4 | 60.9 |
Any drug use disorder included any of the nine drug use disorders: inhalant, marijuana, cocaine, heroin, hallucinogen, opioid, sedative, stimulant, and tranquilizer.
Number of disorders was categorized into three categories for past-year substance use disorders (0, 1–2, 3 or more).
Boldface: χ2 test for sex differences: a: p ≤ 0.05; b: p ≤ 0.01; c: p ≤ 0.001.
3.2. SUDs among non-inhalant users
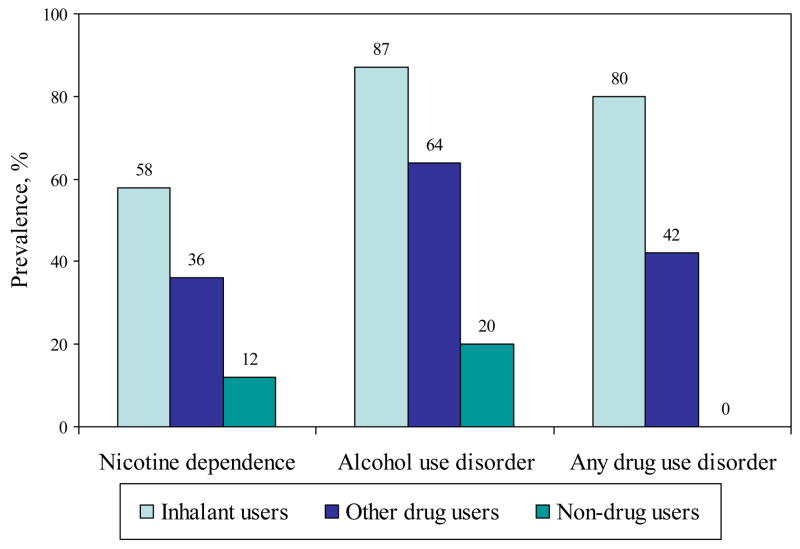
As shown in Fig. 1, lifetime prevalences of SUDs were significantly higher among lifetime inhalant users compared with drug users without a history of inhalant use and respondents without a history of inhalant and other drug use (χ2 test, p < 0.001 for each comparison).
Fig. 1.
Lifetime prevalence of substance use disorders among lifetime inhalant users compared with lifetime drug users without a history of inhalant use (other drug users) and respondents without a history of inhalant and other drug use (non-drug users) in 2001–2002 NESARC (N = 43,093).
3.3. Mean age at first inhalant use and other substance use
Table 2 indicates that inhalant users had an earlier mean age of first use for all the other substances (except heroin) than substance users without a history of inhalant use (t-tests, p < 0.001 for each comparison).
Table 2.
Mean age of first use of substances among lifetime inhalant users and substance users without a history of inhalant use in 2001–2002 NESARC, overall and by sex
| Lifetime inhalant users | Lifetime substance users without a history of inhalant use | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean age of first use of each substance (SE) | Sample size | Overall | Men | Women | Sample size | Overall | Men | Women |
| Inhalants | 656a | 17.49 (0.22) | 17.45 (0.26) | 17.59 (0.45) | ……. | ……. | ……. | ……. |
| Cigarettes | 540 | 13.67 (0.18) | 13.70 (0.22) | 13.59 (0.31) | 17216 | 16.17 (0.05) | 15.65 (0.06) | 16.78c (0.06) |
| Alcohol | 658 | 15.62 (0.16) | 15.48 (0.18) | 16.02 (0.33) | 33233 | 19.48 (0.04) | 18.53 (0.05) | 20.46c (0.07) |
| Marijuana | 642 | 15.79 (0.18) | 15.85 (0.20) | 15.61 (0.30) | 7491 | 18.13 (0.06) | 18.12 (0.09) | 18.14 (0.08) |
| Hallucinogens | 477 | 17.73 (0.18) | 17.78 (0.21) | 17.60 (0.38) | 1680 | 18.76 (0.11) | 18.76 (0.14) | 18.75 (0.17) |
| Stimulants | 365 | 17.87 (0.26) | 17.95 (0.28) | 17.63 (0.48) | 1372 | 19.24 (0.14) | 19.47 (0.18) | 18.91 (0.2) |
| Sedatives | 311 | 18.70 (0.36) | 18.68 (0.42) | 18.77 (0.72) | 1260 | 24.22 (0.42) | 23.04 (0.47) | 25.74c (0.65) |
| Tranquilizers | 295 | 19.50 (0.33) | 19.57 (0.39) | 19.24 (0.54) | 977 | 23.69 (0.43) | 22.32 (0.47) | 25.60c (0.70) |
| Opioids | 334 | 19.85 (0.38) | 19.68 (0.44) | 20.35 (0.80) | 1421 | 24.01 (0.35) | 22.97 (0.41) | 25.49c (0.56) |
| Cocaine | 434 | 20.27 (0.28) | 20.35 (0.30) | 19.98 (0.69) | 2072 | 22.11 (0.15) | 22.38 (0.20) | 21.68a (0.21) |
| Heroin | 62 | 21.39 (0.99) | 21.43 (1.05) | 21.27 (2.35) | 88 | 22.07 (0.93) | 22.28 (1.18) | 21.40 (1.02) |
A total of 8 inhalant users had missing data on age of first use. Boldface: T-test for sex differences: a: p ≤ 0.05; c: p ≤ 0.001.
3.4. Correlates of lifetime SUDs among inhalant users
As shown Table 3, less than a high school education, onset of inhalant use before age 18, residence in non-metropolitan areas, and a history of substance abuse treatment were associated with increased odds of having a lifetime IUD.
Table 3.
Adjusted odds ratios (AORs) and 95 percent confidence intervals (CIs) of lifetime substance use disorders among lifetime inhalant users (N = 664)
| Adjusted logistic regression modela | Lifetime inhalant use disorder | Lifetime alcohol use disorder | Lifetime drug use disorderb | Lifetime nicotine dependence |
|---|---|---|---|---|
| Independent variables | AOR (95% CIs) | AOR (95% CIs) | AOR (95% CIs) | AOR (95% CIs) |
| Age group (vs. 45 or older) | ||||
| 18–29 | 0.6 (0.31 1.21) | 1.1 (0.45 2.90) | 1.7 (0.86 3.31) | 1.9 (1.08 3.44) |
| 30–44 | 0.9 (0.49 1.64) | 2.3 (1.18 4.36) | 1.5 (0.86 2.64) | 1.6 (0.95 2.54) |
|
| ||||
| Sex (vs. female) | ||||
| Male | 1.1 (0.58 2.08) | 1.9 (1.05 3.36) | 1.9 (1.22 3.03) | 0.8 (0.52 1.16) |
|
| ||||
| Race/ethnicity (vs. white) | ||||
| African American | 1.0 (0.43 2.34) | 0.6 (0.22 1.38) | 0.5 (0.20 1.44) | 0.6 (0.24 1.30) |
| American Indian/Alaska | 0.9 (0.31 2.46) | 0.7 (0.25 2.10) | 0.5 (0.21 1.18) | 0.8 (0.33 1.71) |
| Native/Asian | ||||
| Hispanic | 1.2 (0.56 2.67) | 1.0 (0.44 2.06) | 1.2 (0.51 2.86) | 0.6 (0.28 1.11) |
|
| ||||
| Education (vs. college) | ||||
| < High school | 2.0 (1.06 3.95) | 0.7 (0.27 1.67) | 1.5 (0.70 3.37) | 1.1 (0.57 1.94) |
| High school | 1.3 (0.76 2.25) | 0.8 (0.44 1.45) | 1.5 (0.83 2.83) | 0.8 (0.46 1.21) |
|
| ||||
| Marital status (vs. married) | ||||
| Widowed/divorced/separated | 1.4 (0.72 2.64) | 0.7 (0.28 1.47) | 0.7 (0.36 1.35) | 1.3 (0.75 2.12) |
| Single | 1.8 (0.89 3.55) | 0.3 (0.11 0.80) | 0.5 (0.27 1.01) | 0.7 (0.37 1.15) |
|
| ||||
| Family income (vs. $75,000+) | ||||
| $0–$19,999 | 0.9 (0.36 2.05) | 4.3 (1.94 9.41) | 3.3 (1.58 6.70) | 4.9 (2.56 9.29) |
| $20,000–$39,999 | 1.0 (0.41 2.34) | 5.3 (2.01 13.98) | 2.8 (1.35 5.79) | 1.9 (1.03 3.43) |
| $40,000–$74,999 | 0.8 (0.36 1.89) | 2.2 (1.03 4.59) | 1.7 (0.86 3.37) | 2.1 (1.18 3.58) |
|
| ||||
| Urbanicity (vs. metropolitan–in central city) | ||||
| Non-metropolitan | 2.1 (1.04 4.39) | 0.8 (0.36 1.96) | 0.9 (0.45 1.79) | 1.0 (0.49 2.06) |
| Metropolitan–not in central city | 1.7 (0.99 2.84) | 0.9 (0.46 1.74) | 0.8 (0.52 1.30) | 1.1 (0.75 1.67) |
|
| ||||
| Age of first inhalant use(vs. 18) | ||||
| < 13 years | 2.2 (1.01 4.84) | 0.8 (0.32 1.91) | 0.9 (0.46 1.92) | 0.9 (0.44 1.92) |
| 13–17 | 2.0 (1.13 3.41) | 1.1 (0.58 2.01) | 1.7 (1.04 2.64) | 1.7 (1.09 2.65) |
|
| ||||
| Personal history of substance abuse treatment (vs. no) | ||||
| Yes | 5.4 (2.47 11.70) | ……. | 4.9 (0.91 26.73) | 1.9 (0.72 5.12) |
|
| ||||
| Family history of psychopathology (vs. no) | ||||
| Yes | 0.5 (0.24 1.14) | 2.0 (0.83 4.62) | 2.3 (1.04 4.92) | 1.2 (0.76 1.90) |
Each adjusted logistic regression model included all variables listed in the first column.
Drug use disorder included any of the nine drug use disorders: inhalant, marijuana, cocaine, heroin, hallucinogen, opioid, sedative, stimulant, and tranquilizer.
Boldface: p ≤ 0.05.
Not included in the model due to unstable estimates.
Increased odds of lifetime AUD were noted among inhalant users who were aged 30–44 years, male, currently married, and among those with a family income under $75,000. Male sex, low family incomes, early onset of inhalant use (13–17 years), and a family history of psychopathology were associated with increased odds of lifetime DUD. Increased odds of lifetime ND were associated with being aged 18–29 years, having a family income under $75,000, and early onset of inhalant use.
3.5. Correlates of past-year SUDs among inhalant users
Table 4 reports the correlates of past-year SUDs. Young adults and those with low family incomes had increased odds of having a past-year ND, AUD, or DUD. Male sex was associated with greater odds of having a past-year AUD, and high school education was associated with having a DUD. Being white and early inhalant use were associated with increased odds of having a past-year ND.
Table 4.
Adjusted odds ratios (AORs) and 95 percent confidence intervals (CIs) of past-year substance use disorders among lifetime inhalant users (N = 664)
| Adjusted logistic regression modela | Past-year alcohol use disorder | Past-year drug use disorderb | Past-year nicotine dependence |
|---|---|---|---|
| Independent variables | AOR (95% CIs) | AOR (95% CIs) | AOR (95% CIs) |
| Age group (vs. 45 or older) | |||
| 18–29 | 4.6 (2.45 8.77) | 7.8 (3.26 18.47) | 2.1 (1.20 3.74) |
| 30–44 | 2.0 (1.09 3.62) | 1.5 (0.64 3.70) | 1.6 (0.99 2.65) |
|
| |||
| Sex (vs. female) | |||
| Male | 1.9 (1.10 3.10) | 1.7 (0.84 3.42) | 0.9 (0.56 1.30) |
|
| |||
| Race/ethnicity (vs. white) | |||
| African American | 1.1 (0.52 2.24) | 1.9 (0.69 4.94) | 0.7 (0.32 1.73) |
| American Indian/Alaska Native/Asian | 0.9 (0.41 2.06) | 0.7 (0.23 1.85) | 0.9 (0.37 2.20) |
| Hispanic | 0.9 (0.42 1.97) | 0.8 (0.31 1.95) | 0.5 (0.23 0.98) |
|
| |||
| Education (vs. college) | |||
| < high school | 0.8 (0.37 1.68) | 1.5 (0.64 3.49) | 1.5 (0.78 2.77) |
| High school | 0.7 (0.39 1.08) | 2.0 (1.05 3.69) | 0.9 (0.59 1.51) |
|
| |||
| Marital status (vs. married) | |||
| Widowed/divorced/separated | 1.2 (0.67 2.27) | 1.8 (0.78 3.93) | 1.5 (0.91 2.38) |
| Single | 1.3 (0.71 2.33) | 1.8 (0.97 3.52) | 1.1 (0.58 1.96) |
|
| |||
| Family income (vs. $75,000+) | |||
| $0–$19,999 | 2.5 (1.16 5.37) | 2.8 (1.09 6.95) | 4.0 (2.01 7.80) |
| $20,000–$39,999 | 2.4 (1.25 4.71) | 1.3 (0.48 3.58) | 1.6 (0.82 3.03) |
| $40,000–$74,999 | 1.5 (0.76 2.77) | 2.2 (0.81 5.88) | 1.2 (0.65 2.15) |
|
| |||
| Urbanicity (vs. metropolitan–in central city) | |||
| Non-metropolitan areas | 1.4 (0.65 2.82) | 0.9 (0.41 2.17) | 1.5 (0.77 3.04) |
| Metropolitan–not in central city | 1.3 (0.80 2.15) | 0.8 (0.42 1.45) | 1.3 (0.85 1.98) |
|
| |||
| Age of onset of inhalant use (vs. 18) | |||
| < 13 years | 0.8 (0.34 1.81) | 1.1 (0.35 3.36) | 0.9 (0.41 1.84) |
| 13–17 | 1.4 (0.92 1.98) | 1.4 (0.80 2.37) | 1.6 (1.02 2.62) |
|
| |||
| Personal history of substance abuse treatment (vs. no) | |||
| Yes | 0.9 (0.33 2.29) | 2.2 (0.79 6.23) | 1.3 (0.55 2.94) |
|
| |||
| Family history of psychopathology (vs. no) | |||
| Yes | 1.2 (0.67 2.11) | 2.0 (0.98 4.22) | 1.3 (0.78 2.05) |
Each adjusted logistic regression model included all variables listed in the first column; past-year inhalant use disorders were not reported due to a small number of respondents with a past-year inhalant use disorder.
Drug use disorder included any of the nine drug use disorders: inhalant, marijuana, cocaine, heroin, hallucinogen, opioid, sedative, stimulant, and tranquilizer.
Boldface: p ≤ 0.05.
4. Discussion
Most (96%) lifetime inhalant users in this adult sample met criteria for at least one lifetime SUD. Nearly two thirds of lifetime inhalant users met criteria for a past-year SUD. These findings suggest that inhalant users have a tendency to use multiple substances and are at risk for developing multiple SUDs (Compton et al., 1994; Dinwiddie et al., 1991).
We found that inhalant users were characterized by early use of cigarettes, alcohol, and marijuana, which might explain the high prevalence of SUDs (e.g., Grant and Dawson, 1998). Early users of substances might have more time to progress from initial use to disorder onset than users who start substance use at a later age. Early substance use also tends to co-occur with multiple risk behaviors (DuRant et al., 1999).
There is a possibility that (a) early individual or environmental risk factors, (b) co-occurrences of substance use with other risk behaviors, and (c) neurotoxic effects of substance use on brain (Rogers and Robbins, 2001) place some inhalant users at risk for using multiple substances and developing SUDs. The vulnerability to SUDs may depend on whether risk characteristics are aggregated (e.g., McGue and Iacono, 2005; Newcomb and Felix-Ortiz, 1992). Although this cross-sectional study cannot determine causality, these findings suggest that a general mechanism of risk might explain the association between inhalant use and multiple SUDs (e.g., McGue and Iacono, 2005). A general propensity to drug use could influence an individual’s risk to use both inhalants and other substances and cause the use of these substances to be correlated.
These findings should be interpreted with caution. First, because of the cross-sectional design, causal inferences are not warranted. Second, some respondents were asked to recall prior drug use over lengthy periods of time, which, due to forgetfulness, may result in distortions in their responses. Third, these findings cannot be generalized to adults who were institutionalized or homeless because they were not covered by the NESARC. A small subgroup of heavy inhalant users might not have been sampled or were unable to participate in a household survey due to neurological or other disability from chronic inhalant use (e.g., Anderson and Loomis, 2003).
These limitations aside, this study demonstrates a high prevalence of SUDs among adults who report a history of inhalant use. Given that young inhalant users may be at risk for injection drug use and developing multiple SUDs (Wu and Howard, 2007b; Wu et al., 2005), additional studies are needed to advance our understanding of the progression from inhalant use to drug use disorders, and to develop effective interventions targeting inhalant users.
Acknowledgments
NESARC was sponsored by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health, US Department of Health and Human Services, with supplemental support from the National Institute on Drug Abuse. This work was supported by a grant award from the National Institute on Drug Abuse (DA015938) to Li-Tzy Wu. The opinions expressed in this paper are solely those of the authors. We thank Tzy-May Kuo for assistance with some of the data analyses and Amanda McMillan for proofreading the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anderson CE, Loomis GA. Recognition and prevention of inhalant abuse. American Family Physician. 2003;68:869–874. [PubMed] [Google Scholar]
- Compton WM, Cottler LB, Dinwiddie SH, Spitznagel EL, Mager DE, Asmus G. Inhalant use: Characteristics and predictors. The American Journal on Addictions. 1994;3:263–272. [Google Scholar]
- Dinwiddie SH, Reich T, Cloninger CR. The relationship of solvent use to other substance use. The American Journal of Drug and Alcohol Abuse. 1991;17:173–186. doi: 10.3109/00952999108992820. [DOI] [PubMed] [Google Scholar]
- DuRant RH, Smith JA, Kreiter SR, Krowchuk DP. The relationship between early age of onset of initial substance use and engaging in multiple health risk behaviors among young adolescents. Archives of Pediatric and Adolescent Medicine. 1999;153:286–291. doi: 10.1001/archpedi.153.3.286. [DOI] [PubMed] [Google Scholar]
- Fendrich M, Mackesy-Amiti ME, Wislar JS, Goldstein PJ. Childhood abuse and the use of inhalants: differences by degree of use. American Journal of Public Health. 1997;87:765–769. doi: 10.2105/ajph.87.5.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age of onset of drug use and its association with DSM-IV drug abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1998;10:163–173. doi: 10.1016/s0899-3289(99)80131-x. [DOI] [PubMed] [Google Scholar]
- McGue M, Iacono WG. The association of early adolescent problem behavior with adult psychopathology. The American Journal of Psychiatry. 2005;162:1118–1124. doi: 10.1176/appi.ajp.162.6.1118. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, Felix-Ortiz M. Multiple protective and risk factors for drug use and abuse: cross-sectional and prospective findings. Journal of Personality and Social Psychology. 1992;63:280–296. doi: 10.1037//0022-3514.63.2.280. [DOI] [PubMed] [Google Scholar]
- Research Triangle Institute. SUDAAN user’s manual: Release 8.0. Research Triangle Park, NC: Research Triangle Institute; 2002. [Google Scholar]
- Rogers RD, Robbins TW. Investigating the neurocognitive deficits associated with chronic drug misuse. Current Opinion in Neurobiology. 2001;11(2):250–257. doi: 10.1016/s0959-4388(00)00204-x. [DOI] [PubMed] [Google Scholar]
- Sakai JT, Mikulich-Gilbertson SK, Crowley TJ. Inhalant use, abuse, and dependence among adolescent patients: commonly comorbid problems. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:1080–1088. doi: 10.1097/01.chi.0000132813.44664.64. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2005 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies, Substance Abuse and Mental Health Services Administration; 2006. [Google Scholar]
- Wu LT, Howard MO. Psychiatric disorders in inhalant users: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2007a;88:146–155. doi: 10.1016/j.drugalcdep.2006.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Howard MO. Is inhalant use a risk factor for heroin and injection drug use among adolescents in the United States? Addictive Behaviors. 2007b;32:265–281. doi: 10.1016/j.addbeh.2006.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Ringwalt CL. Inhalant use and disorders among adults in the United States. Drug and Alcohol Dependence. 2006;85:1–11. doi: 10.1016/j.drugalcdep.2006.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Pilowsky DJ, Schlenger WE. High prevalence of substance use disorders among adolescents who use marijuana and inhalants. Drug and Alcohol Dependence. 2005;78:23–32. doi: 10.1016/j.drugalcdep.2004.08.025. [DOI] [PubMed] [Google Scholar]