Abstract
Psychotic symptoms are distributed along a continuum that extends from normality to diagnosable psychotic disorders and the presence of psychoticism among individuals in the general population may lead to morbidity and social impairment. This study examined a model in which psychoticism leads to several important psychological consequences. The analysis included 134 African Americans with no psychiatric history who were being seen in medical walk-in clinics for non-emergency medical problems. Psychoticism, perceived hassles, depression, hostility, and hopelessness were measured. The Linear Structural Relations Program (LISREL) was used to test the fit of the data to the proposed model, a trimmed hierarchical version, and two alternative models. The data supported a model in which psychoticism has substantial effects on several important characteristics: perceived daily hassles, depression, and hostility. Depression mediated the association between psychoticism and hopelessness. Goodness-of-fit indices for a final trimmed model that eliminated one path from the initial postulated model revealed good fit to the data, and the two alternative models were found not to fit the data. Like psychosis itself, psychoticism appears to cause meaningful dysfunction even among non-psychiatric individuals from the general population. Additional research is needed to further characterize the detrimental effects of psychoticism or self-reported psychotic symptoms in the general, non-psychiatric population.
Keywords: depression, general population, hostility, perceived hassles, psychoticism
1. Introduction
Psychotic symptoms are distributed along a continuum that extends with increasing severity from normality to diagnosable psychotic disorder (van Os et al., 1999). Variation in the psychosis phenotype is evident from several studies measuring psychotic symptoms in the general population (Peters et al., 1999; van Os et al., 2000; Krabbendam et al., 2005). The Epidemiological Catchment Area study found hallucinations, unrelated to organic causes, to have a lifetime prevalence of 10% in men and 15% in women (Tien, 1991). The National Survey of Psychiatric Morbidity in Great Britain demonstrated 9.1% and 4.2% prevalences of paranoia and hallucinations, respectively (Claridge et al., 1996). Baseline data from the Netherlands Mental Health Survey and Incidence Study revealed a rate of 8.7% for delusions and 6.2% for hallucinations not considered clinically relevant (van Os et al., 2000). Johns et al. (2002) reported similar rates of hallucinations in a large ethnically diverse sample in the United Kingdom.
According to the continuum hypothesis, psychotic symptoms should be present not only in individuals identified as having psychotic disorders, but also in a proportion of individuals in the general population who do not meet clinical criteria for diagnosable psychosis (Verdoux and van Os, 2002). In fact, it has been suggested that paranoid ideation—a complex phenomenon likely to arise from social, cognitive, and biological factors—is almost as common as symptoms of anxiety and depression in the general population (Johns et al., 2004; Freeman et al., 2005). Additionally, experiencing delusions is not associated inevitably with the presence of a functionally-impairing disorder (Stefanis et al., 2002). Taken together, a growing body of evidence suggests that the prevalence of delusional and hallucinatory experiences in the general population is much greater than the prevalence of psychotic disorders, and that a symptomatic continuum exists, extending from subtle features of psychoticism to self-reported psychotic symptoms in individuals from the general population to clinical cases of primary psychotic disorders in mental health care settings (Verdoux and van Os, 2002). Thus, epidemiologic reports of isolated psychotic symptoms are consistent with earlier conceptualizations of the dimensional nature of psychoticism.
Despite the convergence of evidence that psychotic symptoms, or psychoticism, are present in general community samples, very little research has investigated correlates of these experiences, such as perceptions of daily stress, depressive symptoms, and hostility, in the general population. A few studies demonstrate associations between self-reported psychotic symptoms, such as paranoid ideation in general population participants, and stressful life events or perceived stress (Ohayon, 2000; Cohen et al., 2004; Johns et al., 2004). Some investigations involving non-psychiatric participants also have found that expressions of psychotic symptoms, such as delusional ideation, hallucinations, or paranoia, correlate with depression, which often leads to feelings of hopelessness (van Os et al., 2000; Stefanis et al., 2002; Cohen et al., 2004; Hafner et al., 2005; Krabbendam et al., 2005). One study suggested that self-reported positive psychotic symptoms are associated with impulsivity in a sample of low-income, non-psychiatric African Americans (Compton and Kaslow, 2005).
Using a sample of non-psychiatric participants from the general population (seeking treatment in an urban medical setting), the present study used path analysis to examine the role of psychoticism in relation to several important variables—perceived hassles, depression, hopelessness, and hostility. Specification of a path model should be based on theory and results of prior empirical studies (Kline, 2005). Given the aforementioned past findings suggesting that self-reported psychotic symptoms may be associated with perceived stress, depressive symptoms, and impulsivity, a path model was postulated in which psychoticism (an exogenous variable, meaning that its causes are not represented in the model) would lead to perceived hassles, depression, hostility, and hopelessness. In addition, given the recognized association between depression and hopelessness, it was predicted that depression would partially mediate the association between psychoticism and hopelessness.
2. Methods
2.1. Participants
Data for this analysis were obtained from two case-control studies, both of which recruited samples from a large, urban, public-sector, university-affiliated hospital in the southeastern United States that serves a predominantly African American, socially-disadvantaged population. Participants were recruited while obtaining medical treatment in one of three medical walk-in clinics. The two studies from which data were pooled investigated risk and protective factors for suicide attempts among African Americans, and this analysis included only controls who had never attempted suicide. The two studies had focused exclusively on African Americans due to a dearth of research on risk and protective factors in African Americans.
In the first study, participants (n=200) consisted of African American women, aged 18–59 years, who had reported experiencing intimate partner violence within the past year on a revised version of the Universal Violence Prevention Screening Protocol (Dutton et al., 1996; Kaslow et al., 2002; Thompson et al., 2002; Heron et al., 2003). Cases included 100 women who were seen at the hospital after a nonfatal suicide attempt, and controls included 100 women who came to one of three medical walk-in clinics at the same hospital for non-emergency medical problems (Kaslow et al., 2002; Thompson et al., 2002). The second study involved African American men and women aged 18–64 years (n=200). Cases included 50 men and 50 women who were seen by medical or psychiatric services within 24 hours after a suicide attempt, and controls included 50 men and 50 women with no history of suicidal behavior who were seeking medical care in an urgent care clinic within the same hospital (Compton et al., 2004; Kaslow et al., 2004; Kaslow et al., 2005). Exclusionary criteria for both studies are detailed extensively in prior publications (Kaslow et al., 2002; Thompson et al., 2002; Compton et al., 2004; Kaslow et al., 2004; Kaslow et al., 2005).
The sample for the present analysis was selected as follows. First, of the 400 participants obtained from the two studies (n=200 from each study), 243 (60.1%) participants were excluded due to a history of suicide attempt or any past psychiatric or substance abuse treatment. From the remaining 157 participants, two were excluded because they did not self-identify as African American, and 21 homeless participants were excluded due to the high prevalence of mental illnesses among individuals who are homeless (Fischer and Breakey, 1991). As a result, the final sample for this analysis (n=134) included African American men (n=30, 22.4%) and women (n=104, 77.6%), aged 18–64 (mean, 32.5±10.7 years), who were not homeless, and who reported no prior history of suicide attempt or any past psychiatric or substance abuse treatment.
In terms of other basic sociodemographic variables, 51 (38.1%) had completed less than 12 years of education, 40 (29.9%) had graduated high school, and 43 (32.1%) had attained more than 12 years of education. Just over half (68, 50.7%) of participants were unemployed, and 70 (52.2%) reported an income of less than $1,000 per month. Over half (72, 53.7%) were single, 30 (22.4%) were married or cohabitating with a partner, and 32 (23.9%) were divorced, separated, or widowed.
2.2. Materials
The Symptom Checklist-90-Revised (SCL-90-R) was used to obtain measures of psychoticism and hostility. The SCL-90-R is a 90-item scale that measures emotional, cognitive and physical symptoms along nine primary symptom dimensions: somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism (Derogatis, 1983). The psychoticism dimension represents a continuum from mild interpersonal alienation to dramatic psychosis (e.g. hallucinations and thought control). The hostility dimension reflects thoughts, feelings, or actions characteristic of anger (such as aggression, irritability, rage, and resentment). Symptom dimensions are scored by summing respective items for participants' ratings of how much discomfort each symptom caused within the last week on a 5-point Likert scale ranging from 0 (“not at all”) to 4 (“extremely”). Cronbach's internal consistency reliability coefficients (α) for the SCL-90-R dimensions have been reported to range from 0.77 for the psychoticism subscale to 0.90 for the depression subscale, and test-retest reliability ranges from 0.78 for hostility to 0.90 for phobic anxiety (Derogatis, 1983). In the sample used for this analysis, the Cronbach's α coefficients were 0.88 and 0.84 for the psychoticism and hostility dimensions, respectively. It should be noted that the SCL-90-R also includes a paranoid ideation dimension, which taps thoughts that others are not trustworthy or are malevolent. However, in the present study, the psychoticism dimension was of more interest than the paranoid ideation dimension because the former captures a broader array of psychotic and psychotic-like experiences, including delusions, hallucinations, and passivity phenomena. Furthermore, because the paranoid ideation dimension and the psychoticism dimension are highly correlated (r=0.77, P<.001 in this sample), additional analyses using the paranoid ideation dimension were deemed unnecessary for the purposes of the study.
The 51-item Survey of Recent Life Experiences (SRLE) measures the extent to which respondents are bothered by various minor and major life events involving six dimensions: social and cultural difficulties, work, time pressures, finances, social acceptability, and social victimization (Kohn and Macdonald, 1992). Respondents are asked to rate, on a 4-point Likert scale (1=“not at all part of my life” to 4=“very much part of my life”), how much they believe each item has been a concern in their lives over the past month. Higher scores indicate higher levels of recent life hassles. The SRLE has adequate psychometric properties and is often used in stress and coping research (DeLongis et al., 1988). In the present sample, the Cronbach's α coefficient for the SRLE was 0.92.
The Beck Depression Inventory-II (BDI-II) is a 21-item version of the original BDI used to measure self-reported depressive symptoms within the past two weeks (Beck et al., 1996). Scores range from 0 to 63, with higher scores indicating more depressive symptoms. Numerous studies have documented the internal consistency, test-retest reliability, and construct validity of the scale in various populations (Al-Musawi, 2001; Coles et al., 2001; Kojima et al., 2002). The BDI-II had an internal consistency Cronbach's α coefficient of 0.92 in the present sample. Although the SCL-90-R includes a depression dimension, the BDI-II was chosen as a measure of depressive symptoms instead of the SCL-90-R depression dimension in order to reduce the influence of shared instrument variance. However, it should be noted that the correlation between the BDI-II total score and the SCL-90-R depression dimension in this sample was quite high (r=0.76, P<.001), which is evidence of concurrent criterion validity.
The 20-item Beck Hopelessness Scale (BHS) is a true-false questionnaire that addresses negative expectancies about the future (Beck et al., 1974). Scores range from 0 to 20, with higher scores indicative of greater hopelessness. The scale has good convergent and criterion validity (Beck et al., 1974). The Cronbach's α coefficient of the BHS was 0.86 in the present sample.
2.3. Design and Procedures
After examination of initial descriptive statistics for the five variables of interest, square-root transformation was conducted for two reasons. First, four of the variables (psychoticism, depression, hostility, and hopelessness) were not normally distributed based on skewness and kurtosis statistics. In each case, a prominent positive skew was apparent, with a relatively high frequency of zero scores. Second, the five variables were ill-scaled for path analysis. Although the perceived hassles variable was approximately normally distributed in its original scale, this variable also was square-root transformed to improve the scaling across all variables (so that variances were more homogeneous). The transformations improved kurtosis and skewness indices and adjusted scaling so that path analysis could be conducted.
The Linear Structural Relations Program (LISREL version 8.52) was used for path analyses examining the direct and indirect effects of psychoticism on perceived hassles, depression, hostility, and hopelessness. Path analysis involves the estimation of presumed causal relations among observed variables (Kline, 2005), even though they are often measured cross-sectionally. In this analysis, maximum likelihood estimation was used, and only recursive models were considered, meaning that the disturbances (latent variables representing unexplained variability in endogenous variables) were assumed to be uncorrelated and that all causal effects were assigned to be unidirectional (Jöreskog and Sörbom, 1993).
Only overidentified models were assessed, and several model fit indices were selected a priori to assess the fit of the model to the data. First, smaller values of the overall model chi-square (χ2M) indicate goodness-of-fit (P>0.05, indicating that the null hypothesis—that the model fits the data—is not rejected). The normed χ2M also is reported, which reduces the sensitivity of χ2M to sample size (χ2M/dfM). Generally, values <3.0 indicate good fit. Second, the Steiger-Lind root mean square error of approximation (RMSEA) and its 90% confidence interval (CI) provides a correction for model complexity. Small values are desired, and values ≥0.10 indicate poor fit. The 90% CI of the RMSEA generally should not include 0.10. Third, the Bentler comparative fit index (CFI) assesses incremental improvement in fit compared to an independence or null model. Values >0.90 indicate reasonably good fit, though CFI=1.0 only means that χ2M<dfM, not that the model has perfect fit. Fourth, the standardized root mean square residual assesses the mean absolute correlation residual, and values <0.10 are considered acceptable.
To compare hierarchical (nested) models after model trimming, the chi-square difference (χ2D) test was used, in which the χ2M for the trimmed model is subtracted from that of the initial model, and this value is divided by the difference in degrees of freedom (df). A non-significant value indicates approximately equal fit when comparing the two models (suggesting that the trimmed model has not been oversimplified), and the more parsimonious model is preferred. To compare alternative (nonhierarchical) models, the Akaike information criterion (AIC), which favors more parsimonious models, is reported. When comparing two competing models, the one with the lowest value of AIC is preferred.
3. Results
3.1. Frequency of Psychoticism Items and Bivariate Relations among Study Variables
The frequencies of endorsed items within the psychoticism dimension are shown in Table 1. In general, “the idea that something serious is wrong with your body” was the most commonly reported symptom in this dimension (rated as moderately, quite a bit, or extremely by 38, or 28.4%), whereas “hearing voices that other people do not hear” was the least commonly endorsed symptom (rated as moderately, quite a bit, or extremely by 11, or 8.2%). Thought control was reported as moderately, quite a bit, and extremely by 3.7%, 6.0%, and 3.0%, respectively; thought broadcasting was endorsed by 7.5%, 6.0%, and 3.8%; and thought insertion was reported by 5.2%, 4.5%, and 1.5%.
Table 1.
Frequencies of Endorsed Items within the Psychoticism Dimension (n=134)
|
n (%) |
|||
|---|---|---|---|
| SCL-90-R Item | Moderately | Quite a Bit | Extremely |
| 7. The idea that someone else can control your thoughts | 5 (3.7) | 8 (6.0) | 4 (3.0) |
| 16. Hearing voices that other people do not hear | 7 (5.2) | 2 (1.5) | 2 (1.5) |
| 35. Other people being aware of (knowing about) your private thoughts | 10 (7.5) | 8 (6.0) | 5 (3.8) |
| 62. Having thoughts that are not your own | 7 (5.2) | 6 (4.5) | 2 (1.5) |
| 77. Feeling lonely even when you are with people | 11 (8.2) | 13 (9.7) | 8 (6.0) |
| 84. Having thoughts about sex that bother you a lot | 7 (5.2) | 9 (6.7) | 8 (6.0) |
| 85. The idea that you should be punished for your sins | 10 (7.5) | 7 (5.2) | 11 (8.2) |
| 87. The idea that something serious is wrong with your body | 14 (10.4) | 12 (9.0) | 12 (9.0) |
| 88. Never feeling close to another person | 10 (7.5) | 13 (9.7) | 10 (7.5) |
| 90. The idea that something is wrong with your mind | 4 (3.0) | 8 (6.0) | 3 (2.2) |
Pearson product-moment coefficients for correlations between study variables are shown in Table 2. All correlations, which ranged from 0.35 (hopelessness and perceived hassles) to 0.68 (psychoticism and hostility), were statistically significant (P<0.001). Means and standard deviations (SD) for sample scores on each variable also are shown in Table 2, both in the original scale and after square-root transformation.
Table 2.
Correlations between the Five Variables of Interest,* and Means ± Standard Deviations (SD) of Variables in the Original Scale and after Square-Root Transformation
| Psychoticism | Hostility | Hopelessness | Perceived Hassles | Depression | |
|---|---|---|---|---|---|
| Psychoticism | 1 | ||||
| Hostility | 0.68 | 1 | |||
| Hopelessness | 0.42 | 0.41 | 1 | ||
| Perceived Hassles | 0.66 | 0.55 | 0.35 | 1 | |
| Depression | 0.67 | 0.62 | 0.54 | 0.65 | 1 |
| Mean ± SD | |||||
| Original Scale | 6.60 ± 7.70 | 4.69 ± 4.92 | 2.87 ± 3.45 | 90.72 ± 23.46 | 14.57 ± 11.29 |
| Transformed | 2.10 ± 1.49 | 1.76 ± 1.26 | 1.34 ± 1.04 | 9.45 ± 1.23 | 3.47 ± 1.60 |
All correlations are statistically significant, P<0.001.
Because the analysis sample included 77.6% (n=104) African American women, the means, SD, and correlations between the study variables were re-examined restricting the sample to women only, excluding the 30 men. This was done to approximate a control for gender by examining the covariance matrix in a restricted sample; however path analyses described below were not re-run including women only due to sample size concerns. In doing so, the means, SD, and Pearson product-moment correlations were remarkably similar to those reported from the entire sample (women and men) shown in Table 2, suggesting that subsequent path analyses (had a larger sample of women been available) would not have differed substantially from the results presented below.
3.2. Path Analysis of the Hypothesized Model
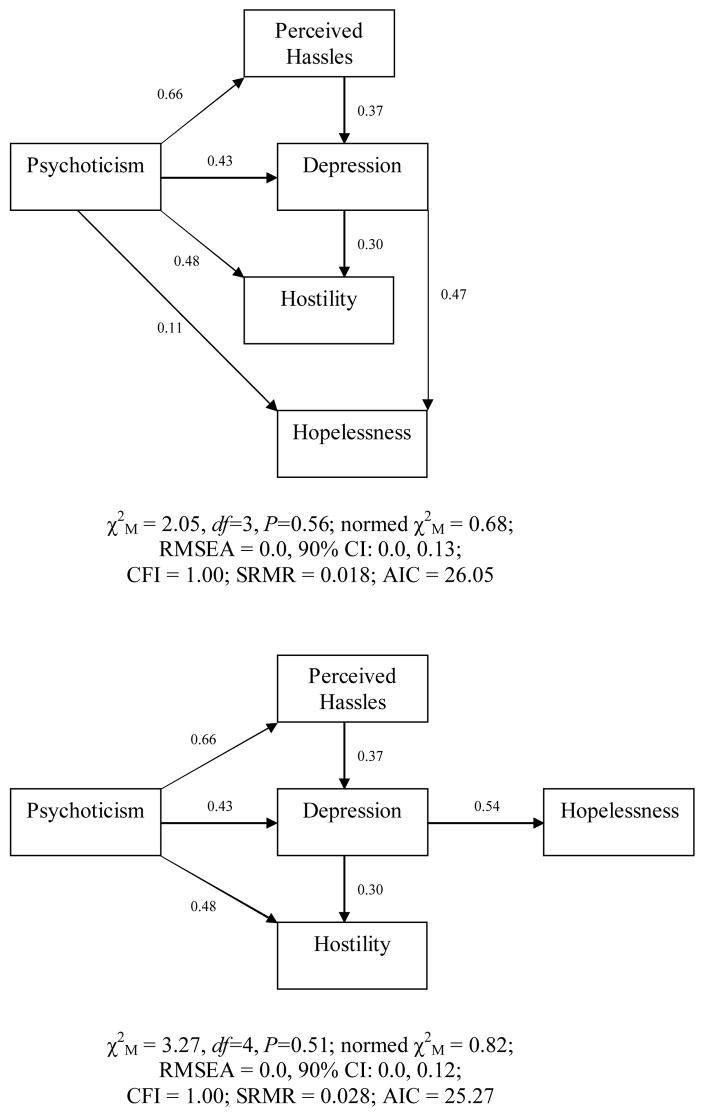
The initial path model, shown in Figure 1, was fitted to a covariance matrix constructed from the correlations and SD shown in Table 2. This model included five variables (and therefore 15 observations in the covariance matrix), and 12 parameters. Thus, this model was overidentified with df=3. All of the path coefficients in this model were statistically significant, except for the direct effect of psychoticism on hopelessness. This finding, a statistically significant indirect effect but not direct effect, suggests mediation (described later). The fit indices for this initial path model were acceptable (shown in Figure 1).
Figure 1.
Initial and Trimmed (Hierarchical) Path Models of the Impact of Psychoticism on Perceived Hassles, Depression, Hostility, and Hopelessness (Standardized Path Coefficients)
The second model, an empirically-trimmed hierarchical version of the first, also is shown in Figure 1. This model included the same five variables, but with only 11 parameters (after the direct effect from psychoticism to hopelessness was fixed to zero). Thus, this model was more parsimonious with df=4. All path coefficients in this model were statistically significant, and the model fit indices remained acceptable. Comparing the two hierarchical models using the χ2D test resulted in a difference that was not statistically significant, leading to a failure to reject the equal-fit hypothesis. This indicates that the two models have roughly equal fit and the trimmed model was not oversimplified.
Conceptually, this model suggests that psychoticism has a significant direct effect on perceived hassles, depression, and hostility. Specifically, a level of psychoticism one full SD above the mean predicts: a level of perceived hassles 0.66 SD above the mean, a level of depression 0.43 SD above the mean, and a level of hostility 0.48 SD above the mean (each controlling for the other variables). The perceived hassles variable has an effect on depression (thus revealing an indirect effect of psychoticism on depression), and depression has an effect on hostility (indicating an indirect effect of psychoticism on hostility). Finally, depression has an effect on hopelessness (such that a level of depression one full SD above the mean predicts a level of hopelessness 0.54 SD above the mean), and mediates any effect that psychoticism has on hopelessness (with no direct effect of psychoticism on hopelessness). All maximum likelihood parameter estimates (direct, indirect, and total effects) for this model, as well as variances and disturbances are shown in Table 3.
Table 3.
Maximum Likelihood Parameter Estimates for the Preferred Path Model
| Path | Unst. | SE | t* | St. |
|---|---|---|---|---|
| Direct Effects | ||||
| Psychoticism → Perceived Hassles | 0.54 | 0.05 | 10.01 | 0.66 |
| Psychoticism → Depression | 0.46 | 0.08 | 5.42 | 0.43 |
| Psychoticism → Hostility | 0.41 | 0.07 | 5.79 | 0.48 |
| Perceived Hassles → Depression | 0.48 | 0.10 | 4.65 | 0.37 |
| Depression → Hopelessness | 0.35 | 0.05 | 7.35 | 0.54 |
| Depression → Hostility | 0.23 | 0.06 | 3.58 | 0.30 |
| Indirect Effects | ||||
| Psychoticism → Perceived Hassles → Depression | 0.26 | 0.06 | 4.22 | 0.24 |
| Psychoticism → Depression → Hopelessness | 0.25 | 0.04 | 6.01 | 0.23 |
| Psychoticism → Depression → Hostility | 0.17 | 0.05 | 3.38 | 0.13 |
| Total Effects | ||||
| Psychoticism → Depression | 0.72 | 0.07 | 10.43 | 0.67 |
| Psychoticism → Hostility | 0.57 | 0.05 | 10.57 | 0.68 |
| Variances and Disturbances | ||||
| Psychoticism (variance) | 2.21 | 0.27 | 8.12 | 1.00 |
| Perceived Hassles (disturbance) | 0.85 | 0.11 | 8.12 | 0.57 |
| Depression (disturbance) | 1.21 | 0.15 | 8.12 | 0.47 |
| Hostility (disturbance) | 0.79 | 0.10 | 8.12 | 0.49 |
| Hopelessness (disturbance) | 0.76 | 0.09 | 8.12 | 0.71 |
Unst. = Unstandardized parameter estimate. SE = Standard error. t = t-test statistic. St. = Standardized parameter estimate.
P<0.05.
3.3. Consideration of Alternative Models
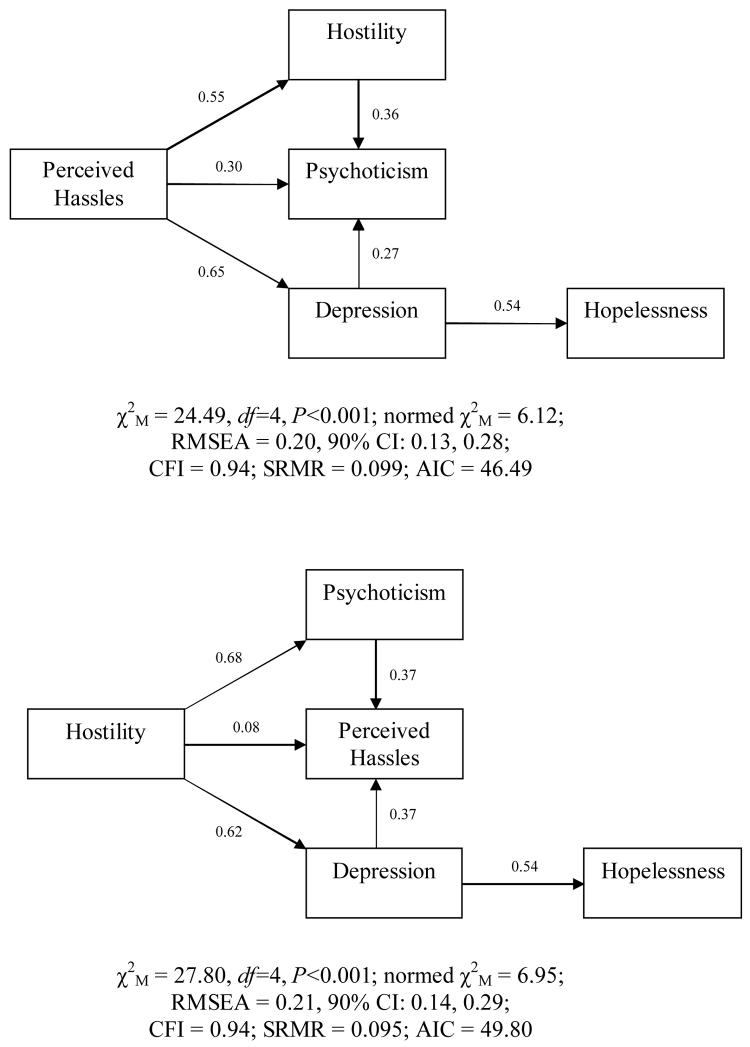
Because path analysis does not preclude the possibility that very different models may fit the data equally well, two a priori alternative models were considered. In both cases, these alternative models had 11 parameters and therefore, df=4. In the first, perceived hassles was assigned as the exogenous variable, with direct effects on hostility, psychoticism, and depression. Additionally, in this model psychoticism would be influenced by hostility and depression. As in the trimmed model described above, hopelessness would be driven by depression (and indirectly by perceived hassles). As shown in Figure 2, the fit indices for this model were not acceptable. Furthermore, the AIC was much higher for this model than for the well-fitting trimmed model.
Figure 2.
Two Alternative Path Models That Do Not Provide Good Fit to the Data (Standardized Path Coefficients)
In the second alternative model (also shown in Figure 2), hostility was the exogenous variable, with direct effects on psychoticism, perceived hassles, and depression. In this model, perceived hassles would be influenced by both psychoticism and depression. Again, hopelessness would be driven by depression (and indirectly by hostility). However, the fit statistics again revealed poor fit to the data. The AIC was again much higher for this model than for the well-fitting model described above. The assessment of these two alternative models—neither of which provided good fit to the data—offers a statistical basis for choosing the previously described model in which psychoticism impacts the other four variables. However, as discussed further below, additional alternative models could be investigated.
4. Discussion
In this study involving 134 African Americans without histories of psychiatric treatment, the data supported our postulated model in which psychoticism impacted subsequential stresses and psychological symptoms—psychoticism led to greater perceptions of daily hassles, depressive symptoms, and hostility. This is not altogether surprising given the fact that some of the psychoticism items pertain to, for example, thought control, thought broadcasting, and thought insertion (which would seemingly inevitably lead to perceived daily stressors and hostility), as well as ideas that something is wrong with one's body or mind (cognitive schemas that clearly could lead to depressive feelings). Rejection of the two alternative models provided further support for (but not proof of) the directionality associated with the postulated model. Yung and colleagues (Yung et al., 2006) studied 140 young people reporting psychotic-like experiences in a youth psychiatric service designed for early intervention during the prodrome of psychotic disorders. In that study, two domains of psychotic-like symptoms (bizarre experiences and persecutory ideas) were associated with distress, depression, and poor functioning. This finding, together with the results reported here, suggests that like psychosis itself, self-reported psychotic or subthreshold psychotic symptoms cause meaningful dysfunction even among non-psychiatric individuals from the general population.
Importantly, the sample for this study was comprised of individuals with no prior psychiatric treatment history. Although their levels of psychotic-like symptoms would likely not meet a diagnostic threshold, these symptoms nonetheless could potentially result in clinically significant psychological morbidity. Recent studies show associations between psychoticism and panic attacks (Goodwin et al., 2004) and impulsivity (Compton and Kaslow, 2005). The results of this investigation expand the range of correlates with psychoticism and reinforce the possibility that meaningful psychological impairment may be associated with subsyndromal levels of psychotic symptoms. The effects of psychoticism on perceived hassles, depression, and hostility provide avenues through which psychoticism may detrimentally affect functioning. Each of these variables, in turn, has been linked with significant morbidity in a variety of domains. For example, research implicates hostility in impairments in health (Brydon et al., 2006), employment (Timothy et al., 2006), and quality of life (Shen et al., 2006). Subsyndromal depressive symptoms have, likewise, been correlated with poorer functioning (Goldney et al., 2004; Backenstrss et al., 2005). A recent study found that both psychoticism and depressive symptoms are associated with earlier age of onset for coronary artery disease, and this relation remains even after excluding individuals with major depression (Kettner et al., 2006).
Given that the individuals in this study had never received psychiatric care, identifying persons with detrimental levels of psychoticism for early intervention or treatment would be challenging. It is possible that a subset of these individuals would obtain psychiatric care if depressive symptoms were to become significant enough to meet diagnostic criteria. In that case, however, it might still be valuable to address psychoticism due to its potential effects upon adherence with treatment because individuals with significant psychoticism may be more difficult to engage and maintain in treatment. Furthermore, research suggests a negative association between psychoticism and response to antidepressant therapy and treatments for sleep disturbance (Rasmussen et al., 2005). Assessing psychoticism could alert clinicians to individuals who may need enhanced treatment regimens to attain adequate symptom remission. In such cases, it would be important to watch for the emergence of psychotic features that may require treatment with antipsychotic medication. Additionally, psychotherapy might be useful in addressing maladaptive approaches to situations and individuals that result from psychoticism.
Because this analysis sought to examine the impact of psychoticism on perceived hassles, depression, hostility, and hopelessness in a non-psychiatric sample of African Americans (i.e., individuals not currently or previously engaged in psychiatric treatment), any participants who reported a history of past suicide attempt, any past psychiatric or substance abuse treatment, or homelessness were excluded. These proxy measures likely successfully restricted the sample to a non-psychiatric group. It was not, however, the aim of this analysis to exclude participants with potentially undiagnosed or untreated mental disorders or serious symptoms. The prominent problem of under-recognition and under-treatment of mental disorders is widely known (Hirschfeld et al., 1997; Kessler et al., 2001; Wang et al., 2002), and if people with past or present undiagnosed/untreated psychiatric syndromes had been excluded from the analysis, then the sample would have been overly “purified” and not at all generalizable to the non-psychiatric population.
Several methodological limitations should be considered, the first and most important of which relates to generalizability of the sample and potential biases that may have been introduced due to the sample characteristics, in terms of (1) socioeconomic characteristics, (2) race/ethnicity, (3) the particular setting from which participants were recruited, and (4) the fact that the women from the first of the two studies from which data were obtained had a history of intimate partner violence. Regarding the first of these issues, it could be that this sample experienced a higher likelihood of being hassled, depressed, hostile, or hopeless by virtue of socioeconomic characteristics. Means of variables and correlations between them cannot be extrapolated to dissimilar socioeconomic groups. With regard to race/ethnicity, the ways in which restricting the study to only African Americans might have biased the results (e.g., stronger correlations between some study variables than may be seen in other ethnic groups) are not known. However, internal validity is enhanced by the relatively homogenous sample that included urban, African American, non-psychiatric participants. That participants were recruited from a medical center poses obvious limitations in terms of generalizability to the broader general population. For example, the fact that the most commonly endorsed symptom was “the idea that something serious is wrong with your body” is not surprising, given that the participants were recruited from medical clinics. Equally importantly, participants were involved in the first case-control study by virtue of having reported a history of intimate partner violence, which further limits generalizability and may introduce bias.
A second limitation relates to the fact that correlation does not imply causation, though path analysis seeks to understand potential causal relations among variables. Failure to reject a path model based on its fit indices does not prove that its hypotheses about causality are necessarily correct (Kline, 2005). Yet, the trimmed postulated model clearly fit the data whereas the two alternative models did not. Although these two a priori alternative models did not fit the data, it should be noted that a host of other alternative models could be tested. Moreover, due to sample size limitations and very limited research in this area, the present study aimed to keep the path analyses relatively simple, and therefore only recursive models with unidirectional effects were considered. Further research utilizing larger samples should study more complex models with bidirectional effects. A third potential weakness pertains to the fact that although the number of cases has no impact on whether or not a path model is identified, results derived from larger samples have less sampling error than results from smaller samples (Kline, 2005). A generally acceptable ratio for the number of cases to free parameters is 10:1, and our final trimmed model and the two alternative models had 11 parameters, meaning that the ratio was 12.2:1. Although this sample size is acceptable, larger studies may provide more precise parameter estimates. A fourth limitation is that two of the five variables of interest in this study (psychoticism and hostility) were measured with subscales of the SCL-90-R. Analyzing the effects of one scale on another scale from the same questionnaire introduces shared instrument variance, which undoubtedly contributes to the correlation between these two measures. However, the remaining variables were measured using different instruments.
In summary, psychoticism has important associations with other variables that are clearly associated with stress and impairment. Thus, individuals reporting isolated psychotic symptoms or demonstrating significant levels of psychoticism are at risk in at least two ways. In the long-term, such individuals are likely to have an elevated risk for the development of psychiatric illnesses, such as mood or psychotic disorders. More immediately, however, those experiencing elevated levels of psychoticism are at risk for greater perceived hassles in everyday life, more depressive symptoms, and increased hostility. Each of these, in turn, may be associated with a host of psychological and social disturbances. Future research should be directed at further characterization of the untoward effects of psychoticism or self-reported psychotic symptoms among individuals not already engaged in mental health treatment.
Acknowledgements
This study was funded by a grant entitled “Black Suicide Attempters: Risk Factors and Sex Differences” from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Support for analyses was provided to the first author from a grant from the National Institute of Mental Health (K23 MH067589).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Al-Musawi N. Psychometric properties of the Beck Depression Inventory-II with university students in Bahrain. Journal of Personality Assessment. 2001;77:568–579. doi: 10.1207/S15327752JPA7703_13. [DOI] [PubMed] [Google Scholar]
- Backenstrss M, Frank A, Joset K, Hingmann S, Mundt C, Kronmuller KT. A comparative study of nonspecific depressive symptoms and minor depression regarding functional impairment and associated characteristics in primary care. Comprehensive Psychiatry. 2005;47:35–41. doi: 10.1016/j.comppsych.2005.04.007. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory Manual. 2nd ed. Psychological Corporation; San Antonio, Texas: 1996. [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Brydon L, Magid K, Steptoe A. Platelets, coronary heart disease, and stress. Brain, Behavior, and Immunity. 2006;20:113–119. doi: 10.1016/j.bbi.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Claridge G, McCreery C, Msaon O, Bentall R, Boyle G, Slade P, Popplewell D. The factor structure of ‘schizotypal’ traits: A large replication study. British Journal of Psychology. 1996;35:103–115. doi: 10.1111/j.2044-8260.1996.tb01166.x. [DOI] [PubMed] [Google Scholar]
- Cohen CJ, Magai C, Yaffee R, Walcott-Brown L. Racial differences in paranoid ideation and psychoses in an older urban population. American Journal of Psychiatry. 2004;161:864–871. doi: 10.1176/appi.ajp.161.5.864. [DOI] [PubMed] [Google Scholar]
- Coles ME, Gibb BE, Heimberg RG. Psychometric evaluation of the Beck Depression Inventory in adults with social anxiety disorder. Depression and Anxiety. 2001;14:145–148. doi: 10.1002/da.1057. [DOI] [PubMed] [Google Scholar]
- Compton MT, Kaslow NJ. Self-reported psychotic symptoms predict impulsivity among African-American patients in an urban non-psychiatric medical setting. Psychiatry Research. 2005;135:35–44. doi: 10.1016/j.psychres.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Compton MT, Thompson NT, Kaslow NJ. Social environment factors associated with suicide attempt among low-income African Americans: The protective role of family relationships and social support. Social Psychiatry Psychiatric Epidemiology. 2004;40:175–185. doi: 10.1007/s00127-005-0865-6. [DOI] [PubMed] [Google Scholar]
- DeLongis A, Folkman S, Lazarus R. The impact of daily stress on health and mood: Psychological and social resources as mediators. American Journal of Psychiatry. 1988;151:1132–1136. doi: 10.1037//0022-3514.54.3.486. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90-R. Administration, scoring & procedures manual. Clinical Psychometric Research; Baltimore, Maryland: 1983. [Google Scholar]
- Dutton MA, Mitchell B, Haywood Y. The emergency department as a violence prevention center. Journal of the American Medical Women's Association. 1996;51:92–96. [PubMed] [Google Scholar]
- Fischer PJ, Breakey WR. The epidemiology of alcohol, drug and mental disorders among homeless persons. American Psychologist. 1991;46:1115–1128. doi: 10.1037//0003-066x.46.11.1115. [DOI] [PubMed] [Google Scholar]
- Freeman D, Garety PA, Bebbington PE, Smith B, Rollinson R, Fowler D, Kuipers E, Ray K, Dunn G. Psychological investigation of the structure of paranoia in a non-clinical population. British Journal of Psychiatry. 2005;186:427–435. doi: 10.1192/bjp.186.5.427. [DOI] [PubMed] [Google Scholar]
- Goldney RD, Fisher LJ, Dal Grande E, Taylor W. Subsyndromal depression: Prevalence, use of health services and quality of life in an Australian population. Social Psychiatry and Psychiatric Epidemiology. 2004;39:293–298. doi: 10.1007/s00127-004-0745-5. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Fergusson DM, Horwood JL. Panic attacks and psychoticism. American Journal of Psychiatry. 2004;161:88–92. doi: 10.1176/appi.ajp.161.1.88. [DOI] [PubMed] [Google Scholar]
- Hafner H, Maurer K, Trendler G, an der Heiden W, Schmidt M. The early course of schizophrenia and depression. European Archives of Psychiatry and Clinical Neuroscience. 2005;255:167–173. doi: 10.1007/s00406-005-0584-8. [DOI] [PubMed] [Google Scholar]
- Heron SL, Thompson MP, Jackson E, Kaslow NJ. Do responses from an intimate partner violence screen predict scores on a comprehensive measure of intimate partner violence in low-income black women? Annals of Emergency Medicine. 2003;42:483–491. doi: 10.1067/s0196-0644(03)00718-2. [DOI] [PubMed] [Google Scholar]
- Hirschfeld R,M, Keller MB, Panico S, Arons BS, Barlow D, Davidoff F, Endicott J, Froom J, Goldstein M, Gorman JM, Marek RG, Maurer TA, Meyer R, Phillips K, Ross J, Schwenk TL, Sharfstein SS, Thase ME, Wyatt RJ. The National Depressive and Manic-Depressive Association consensus statement on the undertreatment of depression. Journal of the American Medical Association. 1997;277:333–40. [PubMed] [Google Scholar]
- Johns LC, Cannon M, Singleton N, Murray RM, Farrell M, Brugha T, Bebbington P, Jenkins R, Meltzer H. Prevalence and correlates of self-reported psychotic symptoms in the British population. British Journal of Psychiatry. 2004;185:298–305. doi: 10.1192/bjp.185.4.298. [DOI] [PubMed] [Google Scholar]
- Johns LC, Nazroo JY, Bebbington P, Kuipers E. Occurrence of hallucinatory experiences in a community sample and ethnic variations. British Journal of Psychiatry. 2002;180:174–178. doi: 10.1192/bjp.180.2.174. [DOI] [PubMed] [Google Scholar]
- Jöreskog K, Sörbom D. LISREL 8: Structural Equation Modeling with the SIMPLIS Command Language. Scientific Software International Incorporated; Lincolnwood, Illinois: 1993. [Google Scholar]
- Kaslow NJ, Price AW, Wyckoff S, Bender GM, Sherry A, Young S, Scholl L, Millington UV, Rashid A, Jackson EB, Bethea K. Person factors associated with suicidal behavior among African American women and men. Cultural Diversity and Ethnic Minority Psychology. 2004;10:5–22. doi: 10.1037/1099-9809.10.1.5. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Sherry A, Bethea K, Wyckoff S, Compton MT, Bender Grall M, Scholl L, Webb Price A, Kellermann A, Thompson N, Parker R. Social risk and protective factors for suicide attempts in low income African American men and women. Suicide and Life-Threatening Behavior. 2005;35:400–412. doi: 10.1521/suli.2005.35.4.400. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Thompson MP, Okun A, Price A, Young S, Bender M, Wyckoff S, Twomey H, Goldin J. Risk and protective factors for suicidal behavior in abused African American women. Journal of Consulting and Clinical Psychology. 2002;70:311–319. doi: 10.1037//0022-006x.70.2.311. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch JR. The prevalence and correlates of untreated serious mental illness. Health Services Research. 2001;36:987–1007. [PMC free article] [PubMed] [Google Scholar]
- Kettner MW, Wulsin L, Cao JJ, Schairer J, Hakim A, Hudson M, Keteyian SJ, Khanal S, Clark V, Weaver D. “Major” depressive disorder, coronary heart disease, and the DSM-IV threshold problem. Psychosomatics. 2006;47:50–55. doi: 10.1176/appi.psy.47.1.50. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. The Guilford Press; New York, New York: 2005. [Google Scholar]
- Kohn PM, Macdonald JE. The Survey of Recent Life Experiences: A decontaminated hassles scale for adults. Journal of Behavioral Medicine. 1992;15:221–236. doi: 10.1007/BF00848327. [DOI] [PubMed] [Google Scholar]
- Kojima M, Furukawa TA, Takahashi H, Kawai M, Nagaya T, Tokudome S. Cross-cultural validation of the Beck Depression Inventory-II in Japan. Psychiatry Research. 2002;110:291–299. doi: 10.1016/s0165-1781(02)00106-3. [DOI] [PubMed] [Google Scholar]
- Krabbendam L, Myin-Germeys I, Bak M, Van Os J. Explaining transitions over the hypothesized psychosis continuum. Australian and New Zealand Journal of Psychiatry. 2005;39:180–186. doi: 10.1080/j.1440-1614.2005.01541.x. [DOI] [PubMed] [Google Scholar]
- Ohayon MM. Prevalence of hallucinations and their pathological associations in the general population. Psychiatry Research. 2000;97:153–164. doi: 10.1016/s0165-1781(00)00227-4. [DOI] [PubMed] [Google Scholar]
- Peters ER, Joseph SA, Garety PA. Measurement of delusional ideation in the normal population: Introducing the PDI (Peters et al. Delusions Inventory) Schizophrenia Bulletin. 1999;25:553–576. doi: 10.1093/oxfordjournals.schbul.a033401. [DOI] [PubMed] [Google Scholar]
- Rasmussen N-A, Schroder P, Olsen LR, Brodsgaard M, Uden M, Bech P. Modafinil augmentation in depressed patients with partial response to antidepressants: A pilot on self-reported symptoms covered by the Major Depression Inventory (MDI) and the Symptom Checklist (SCL-92) Nordic Journal of Psychiatry. 2005;59:173–178. [PubMed] [Google Scholar]
- Shen B-J, Myers HF, McCreary CP. Psychological predictors of cardiac rehabilitation quality of life outcomes. Psychosomatic Research. 2006;60:3–11. doi: 10.1016/j.jpsychores.2005.06.069. [DOI] [PubMed] [Google Scholar]
- Stefanis NC, Hanssen M, Smirnis NK, Avramopoulous DA, Evdokimidis IK, Stefanis CN, Verdoux H, van Os J. Evidence that three dimensions of psychosis have a distribution in the general population. Psychological Medicine. 2002;32:347–358. doi: 10.1017/s0033291701005141. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Kaslow NJ, Short LM, Wyckoff S. The mediating roles of perceived social support and resources in the self-efficacy-suicide attempts relation among African American abused women. Journal of Consulting and Clinical Psychology. 2002;70:942–949. doi: 10.1037//0022-006x.70.4.942. [DOI] [PubMed] [Google Scholar]
- Tien AY. Distributions of hallucinations in the population. Social Psychiatry and Psychiatric Epidemiology. 1991;26:287–292. doi: 10.1007/BF00789221. [DOI] [PubMed] [Google Scholar]
- Timothy JA, Brent A, Ilies R. Hostility, job attitudes, and workplace deviance: Test of a multilevel model. Journal of Applied Psychology. 2006;91:126–138. doi: 10.1037/0021-9010.91.1.126. [DOI] [PubMed] [Google Scholar]
- van Os J, Hanssen M, Bijl RV, Ravelli A. Straus (1969) revisited: A psychosis continuum in the general population? Schizophrenia Research. 2000;45:11–20. doi: 10.1016/s0920-9964(99)00224-8. [DOI] [PubMed] [Google Scholar]
- van Os J, Verdoux H, Maurice-Tison S, Gay B, Liraud F, Salamon R, Bourgeois M. Self-reported psychosis-like symptoms and the continuum of psychosis. Social Psychiatry and Psychiatric Epidemiology. 1999;34:359–463. doi: 10.1007/s001270050220. [DOI] [PubMed] [Google Scholar]
- Verdoux H, van Os J. Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophrenia Research. 2002;54:59–65. doi: 10.1016/s0920-9964(01)00352-8. [DOI] [PubMed] [Google Scholar]
- Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. American Journal of Public Health. 2002;92:92–98. doi: 10.2105/ajph.92.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yung AR, Buckby JA, Cotton SM, Cosgrave EM, Killackey EJ, Stanford C, Godfrey K, McGorry PD. Psychotic-like experiences in nonpsychotic help-seekers: Associations with distress, depression, and disability. Schizophrenia Bulletin. 2006;32:352–359. doi: 10.1093/schbul/sbj018. [DOI] [PMC free article] [PubMed] [Google Scholar]