Abstract
Introduction
Potential long-term sequelae of hypospadias and its surgical correction include difficulties in voiding, sexual function, psychosexual adjustment and self-appraisal. These difficulties often evolve long after surgical repair as children grow to adulthood. Despite this, patient-driven data on long-term functional outcomes and satisfaction are limited, leaving the true success of hypospadias surgery essentially unknown. The aim of this study was to address these deficiencies.
Methods
We conducted a chart review for all patients operated on by a single urologist from 1981 to 1988. Extensive efforts were made to obtain accurate current address information for patients. A database of patient demographics and pathology, operative details and complications was created. A 22-item questionnaire was mailed to study subjects. Telephone follow-up by an independent research nurse bolstered response rates. Responses from returned questionnaires were pooled and analyzed.
Results
The chart review included 115 patients. Of 100 patients (with address information) who were sent questionnaires, 28 ultimately responded. The chart review group was comparable to groups in other published studies. Despite a slightly higher initial major complication rate (57.2%), respondents reported few long-term complications (11% fistula, 29% persistent chordee and 10% stricture) and excellent urinary and sexual functional results. The most common functional complaints were spraying and hesitancy during micturition. Overall, 86% of patients were satisfied with their surgical result, and 52% wished they had been provided longer follow-up.
Conclusion
Long-term outcomes data are critical to an honest account of success rates for hypospadias surgery. Obtaining these data remains challenging. In this series, despite high initial complication rates, most patients reported excellent long-term functional results and were quite satisfied with their overall outcome.
Introduction
The implications of hypospadias to the affected child include abnormal voiding patterns and inability to void in the standing position, possible sexual dysfunction, the psychological impact of a genital deformity, potential fertility problems and the prospect of 1 or more corrective surgical procedures as a child. Despite these potentially significant medical and psychosexual sequelae, there is very little published in the literature regarding long-term outcomes for hypospadias patients beyond childhood. A common weakness of the existing literature is that most studies have been based on surgeon impressions of outcome, as opposed to patient satisfaction.1,2 In addition, significant contradiction exists in the literature regarding the psychosexual impact of hypospadias and hypospadias repair.3,4,5 Some studies report that sexual development and function are normal,6,7,8 whereas others report less positive results.9,10,11 Some investigators have reported that all patients are satisfied with the cosmetic result,12 whereas others have found that 38% still felt deformed11 or that as many as 72% regarded their penis as abnormal.6 Regardless of their bias, most authors agree that these patients need to be followed into adolescence and adulthood to assess patient satisfaction.4,5,6,11,13,14 To our knowledge, there is no Canadian-based literature on this subject, and there are few studies in the world literature that focus on functional outcomes and patient satisfaction as those with hypospadias grow into adulthood.6,11,14,15
This study aimed to address these deficiencies in current understanding of the long-term outcomes of hypospadias repair during childhood. This will benefit both surgeons (by providing feedback on the anatomic and functional outcomes of their operations) and patients (by providing a better understanding of their long-term satisfaction after hypospadias repair).
Methods
This study was conducted in 5 stages: chart review, address identification, questionnaire mail-out, telephone follow-up and data analysis. The study design was approved by the British Columbia Children's Hospital institutional ethics review board.
Over the course of 6 months in 2003, all charts for patients who underwent hypospadias operations at the British Columbia Children's Hospital by a single pediatric urologist (G.U.C.) from Jan. 1, 1981, to Dec. 31, 1988, were reviewed. These dates were chosen so that the child would be over age 16 years by the time our questionnaire was mailed out. Data retrieved from the charts included patient name, hospital unique number, provincial health care number, birth date, most recent contact address and phone number, initial grade of hypospadias (according to the Barcat classification16), associated anomalies, number of operations (planned and unplanned), date and type of operations, postoperative complications and last known follow-up date. Each patient was assigned a unique identifying number that was used to ensure confidentiality during the data collection phase of the study.
After establishing this database, we made every attempt to obtain accurate current address and telephone information for each patient. We used various sources to obtain this information, including telephone contact, online 411 directory assistance (www.canada411.ca), hospital records and provincial health care records.
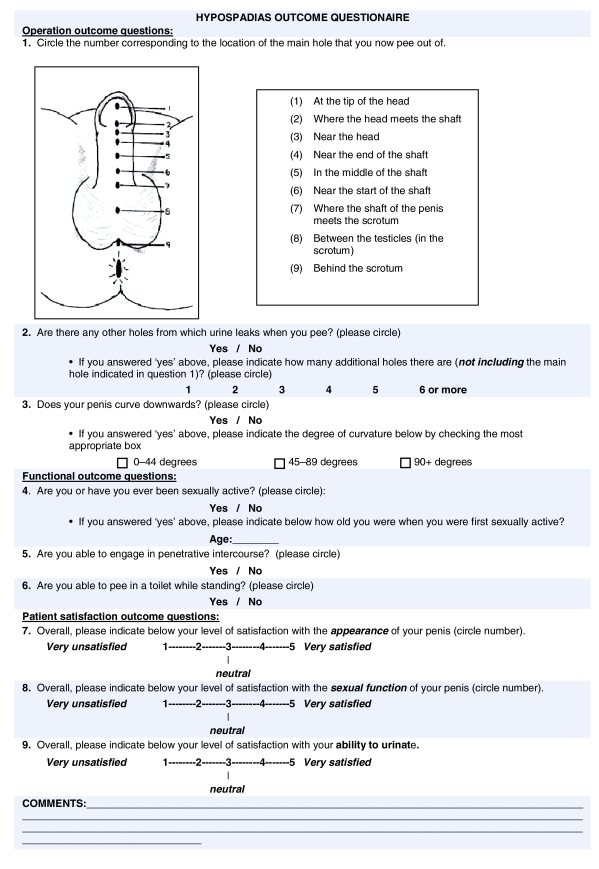
A 22-item questionnaire was devised to address 3 main outcomes: operative or technical success, functional success (voiding and sexual function) and patient satisfaction (see Fig. 1 for abridged version). A combination of categorical questions (e.g., yes or no) and visual analogue scales was used. Patients were provided space for free comment and feedback. We assessed the questionnaire for face validity on a group of 15 urology residents.
Figure 1.
Long-term hypospadias surgery outcome questionnaire (abridged version).
Questionnaires were mailed to all patients for whom address information was obtained. Each package contained a cover letter explaining the study, a consent form, a uniquely numbered questionnaire and 2 separate stamped and addressed return envelopes (one for the consent form and one for the questionnaire). Participants were directed not to print their names or addresses on the return envelopes or questionnaire. The consent forms and questionnaires were to be mailed back separately to maintain confidentiality in the event of lost mail. All questionnaires were mailed to participants in December 2003. Owing to a clerical error, at least 7 subjects received the abridged 9-question version of the questionnaire that included a section for patient comments.
In an attempt to bolster response rates, participants who had not responded were contacted by telephone over the next 6 months by an independent research nurse and asked whether they would be willing to participate in the study. If they agreed, a study package was mailed to them a second time.
After allowing 12 months for participants to respond, we closed the study and analyzed the data. The main database was analyzed to determine average age at first- and second-stage repairs, average age at last follow-up, initial pathology and complication rates. Participant responses were pooled and summarized.
Results
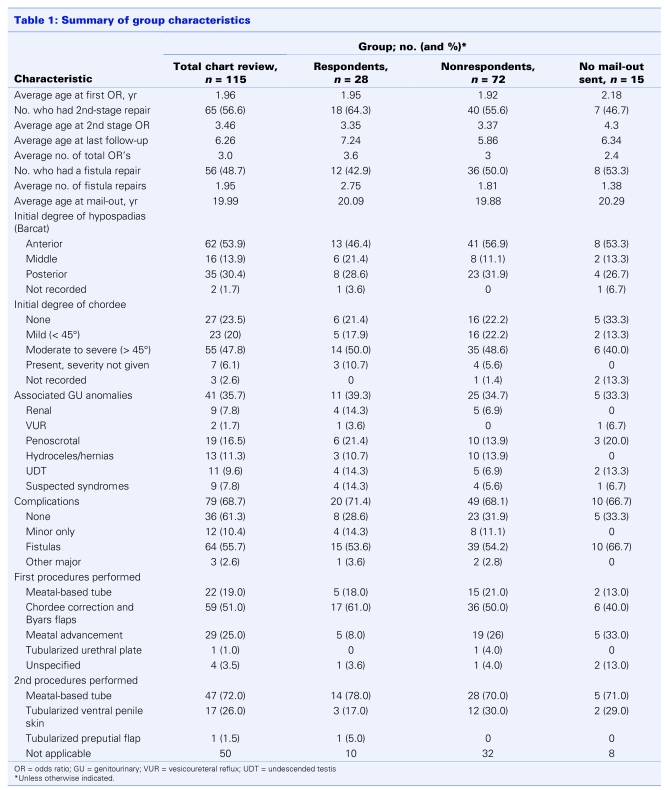
In total, we identified 115 patients as having had hypospadias surgery (performed by G.U.C.) between Jan. 1, 1981, and Dec. 31, 1988. All these charts were retrieved and reviewed. The results of the chart review are summarized in Table 1. The average elapsed time from the date of the last patient follow-up appointment to the time of questionnaire mail-out was 13.7 years. The average patient age at the time of questionnaire mail-out was 20 years (range 16–31 years).
Table 1.
Primary operations were of 3 main types reflecting the commonly used surgical techniques of that era: meatal-based tubes (Mustarde and Broadbent repairs, 19%), first-stage chordee correction and Byars flaps (51%) and meatal advancement (MAGPI repairs, 25%). One tubularized urethral plate (Duplay procedure) was performed as a primary operation, and 4 procedures were unspecified. Second-stage operations consisted of meatal-based tubes (Mustarde and Broadbent repairs, 72%) and tubularized ventral penile skin procedures (Dennis-Brown and Horton-Devine repairs, 26%). One patient was given a tubularized preputial flap as a second-stage operation. Overall 45% of patients had a planned 1-stage procedure, and 53% had a planned 2-stage procedure (information was not available for 2 patients).
It was not possible to obtain complete addresses for 13 patients, and 2 refused to participate when contacted for their address information. Thus questionnaire packages were mailed to 100 potential participants. During the first 4 months after the mail-out, 14 participants consented and returned their completed questionnaires; 11 questionnaires were returned unopened and marked “return to sender.” After the research nurse contacted the nonrespondents by telephone, another 14 consented and returned their completed questionnaires. Thus 15 patients never received packages (either there was no address information for them or they refused consent), while 72 patients never responded and 28 patients consented and returned their completed questionnaires. The characteristics of these 3 groups are summarized in Table 1.
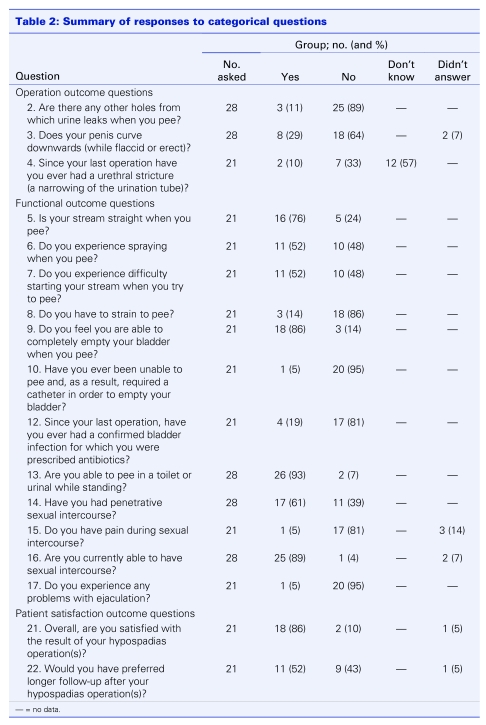
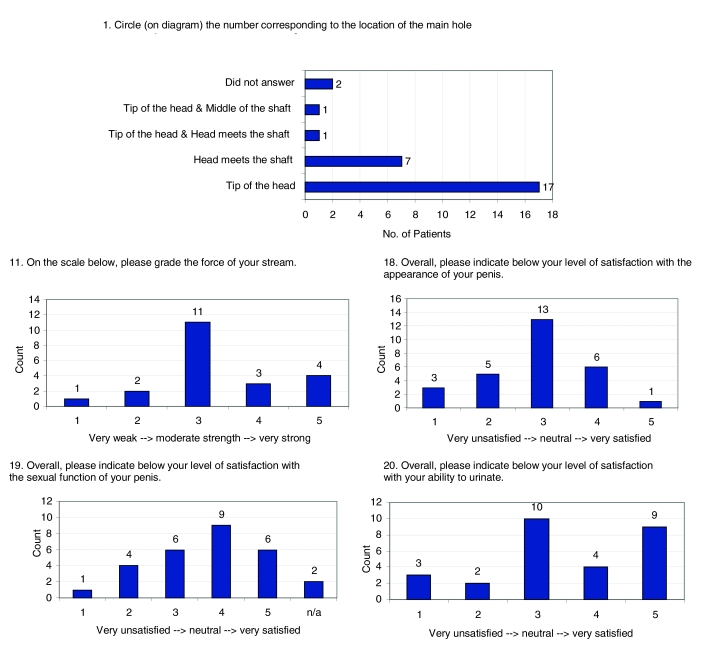
Of the 28 respondents, 7 received an abridged 9-question version of the questionnaire as a result of a clerical error. The responses to each of the questions are summarized in Table 2 and Figure 2. Of those who complained of chordee, 75% indicated that it was minor (< 45°).
Table 2.
Figure 2.
Responses to question 1 and visual analogue questions.
Fourteen respondents provided comments, including 5 of those who received the abridged questionnaire. Three were expressions of gratitude for the care they had received, 3 were clarifications of questionnaire responses, 7 were expressions of angst or frustration with outcomes (spraying, penis size, number of operations, single hair in urethra, scars and embarrassment), and 1, the final comment, was that of a patient's mother who described her son's nightmares of men and women in scrubs for several years after his surgery.
Discussion
Chart review findings
According to our chart review data, our patient population appears to be comparable to populations in the wider hypospadias literature. We found that the distribution of anterior (54%), middle (14%) and posterior (30%) hypospadias was similar to distributions in other authors' series.8,11,15,17,18 The degree of chordee is universally poorly reported in the literature, making comparison of this aspect of initial patient pathology difficult. In our series, the average age at first operation was 2 years, which was early in comparison with other studies of that time period,11,13,15,17,19 but which now falls closer to the accepted optimal time period for initial repair.20 Associated anomalies appeared concordant with other reports.17,21
Reported complication rates from other studies of that time period fall within the range of 50%.11,13,15 We found a slightly higher overall major complication rate in our single-surgeon study (58.3%). Fistula rates (55.7%) were high, although within the range of reported outcomes.6,13,18,22 Minor complications included isolated perioperative urinary infections and balanitis, urethral stent extrusion, patulous meatus and minor excess skin deformity.
Long-term follow-up questionnaire findings
Because of the subject of this study and the significant elapsed time since last follow-up (13.7 yr), we expected from the outset that we would have a low response rate. With telephone follow-up, 28% of subjects who were mailed a questionnaire eventually responded. It is quite likely that, despite our best efforts, a significant proportion of our subject address data was outdated, and this response rate likely underestimates the true response rate for the number of intended subjects who actually did receive the questionnaire package.
Few published studies have followed hypospadias patients into adulthood. Only 4 have focused (to a greater or lesser degree) on patient-reported long-term functional outcomes and satisfaction,11,14,15,19 whereas most others have focused on surgeon-assessed outcomes. Patient response rates range from 23.4%8 to 87%,10 and many authors comment on the logistical difficulty of tracking these patients to early adulthood. Our response rate of 28% falls within the low end of this range. Contributing factors to the difficulty with follow-up that are unique to our study included length of time to follow-up, the huge catchment area served by the BC Children's Hospital (the entire province of 365 000 square miles and 4.3 million residents), the geographical remoteness of most of the communities served and the inherent mobile nature of the youth in this province (to find employment or pursue further education).
We believe that the best judge of the long-term success of hypospadias repairs is the patient himself, who can best assess functional outcomes and satisfaction. It has been demonstrated that surgeon and patient impressions of outcome are often discordant.3 Despite the higher initial complication rate indicated by our chart review data (57.2% of respondents had major complications), our questionnaire respondents faired remarkably well over the long term. Of 26 respondents, 24 stated that their main meatus was at the corona or glans, 11% reported an ongoing fistula, and 10% recollected having had a urethral stricture. The most common operational outcome complaint among respondents was some degree of persistent chordee (29%), most (6 of 8) of which was minor (< 45°). The other 2 respondents indicated an intermediate degree of chordee (45–90°). A similar long-term follow-up study reported a 20% rate of residual chordee > 30°,11 which is within the range of our findings. Interestingly, in the same study, only 30% of those patients found degree of chordee to be a major physical handicap.11 In our study, all patients with residual chordee had been sexually active (5) or felt that they were capable of sexual activity (3), and only 1 of these subjects (who had a minor degree of residual chordee) experienced pain with intercourse. One of the 2 patients with intermediate chordee had been sexually active without reported pain.
Functional outcomes in terms of micturition were also encouraging. Most study subjects voided with a moderate or strong stream, had no deviation of their stream, were able to void without straining and felt that they emptied their bladders well; 93% were able to void in the standing position. Strangely, although few obstructive lower urinary tract symptoms were reported, 52% of subjects reported difficulty starting their streams when voiding. Without interviewing subjects further, it is difficult to explain this finding, although identical findings of hesitancy in the absence of anatomic obstruction were reported by van der Werff and Ultee.14 The most common micturition complaint was spraying (52%) which is consistent with other long-term outcome studies.6,10,11,15 A minority of respondents (5/28) indicated overall dissatisfaction with their ability to void.
The average age of respondents was 20 years, and 61% had had sexual intercourse at some point before receiving our questionnaire, which is consistent with the findings in similar studies of hypospadias patients as young adults.6,8,11 Multiple studies have demonstrated that those with hypospadias have delayed sexual milestones (emotional intimacy, physical intimacy and sexual intercourse).4,5,7,10,23,24 However, they do not appear to differ significantly from normal men in terms of sexual functioning (erection quality, ejaculation, satisfaction and pain).4,8,10 These findings also appear to be reflected in our study, in which all but 1 respondent denied difficulty or pain with sexual intercourse or ejaculation and most (15/28, with 6 others being “neutral”) indicated satisfaction with their sexual functioning. Finally, most respondents were “neutral” about their satisfaction regarding the appearance of their penis. This variation in genital appraisal is reflected elsewhere in the literature.6,11,12 Further, the low positive genital appraisal may explain their apparently delayed sexual debut, as suggested by Mureau and colleagues.4,5 Two of our respondents who provided comments corroborated this suggestion by indicating that anxiety over the appearance of their penis had delayed their first sexual experience.
Overall, most respondents (86%) were satisfied with the result of their hypospadias surgery. Respondents who received the abridged questionnaire were not asked about their “overall” satisfaction; however, they were asked about their level of satisfaction in the specific realms of ability to urinate, sexual function and cosmesis. Of these 7 respondents, 3 responded with scores of 1 or 2 on the visual analogue scales for these individual facets of satisfaction. Three of these patients also provided comments indicating frustration with their outcomes, particularly in the realm of urination and self-consciousness. It is impossible to say how these 7 respondents would have answered the “overall” satisfaction question, but extrapolating from the data available (that 3 were dissatisfied) still yields an overall satisfaction rate of 79% (22/28).
Despite the favourable overall satisfaction rates, many (52%) wished they had had longer follow-up. This desire for longer follow-up through adolescence has been documented by several other authors3,15,23 citing delayed complications, increased adolescent anxiety, poor body image and patients' misunderstanding of their medical history.6,11 Patients have been shown to be reluctant to seek further medical advice despite significant distress.11 Several authors have therefore recommended routine surgeon-initiated follow-up until age 15 years or later.4,5,6,11,13,14 We echo this recommendation; in the impending era of electronic medical records (with automated follow-up routines), initiating these follow-up appointments 10–15 years postrepair will become increasingly feasible.
One of the potential limitations of this study is response bias. It is possible that patients' outcomes (positive or negative) affected their likelihood of responding to our questionnaire. Another limitation of this study is the possibility of subjective misinterpretation of the questionnaire by study participants. For example, the query regarding chordee in both the flaccid and erect states could have been misinterpreted by some respondents. Finally, the inherent difficulty in interpretating long-term hypospadias studies is the applicability of the findings to today's operations. As in all other long-term studies, the operations performed on our study subjects are outmoded and have been replaced by newer techniques that are thought to be superior but have yet to stand the rigorous test of time. Nonetheless, long-term studies (especially those based on patient response) are critically important to highlighting the key outcome issues that continue to hamper or dissatisfy hypospadias patients into adulthood.
Conclusion
Long-term follow-up data are limited for adult hypospadias patients who had reparative surgery in childhood, particularly with regard to patient-reported functional outcomes and satisfaction. Patient-reported outcomes are of paramount importance (outweighing surgeon-assessed outcomes) in assessing the success of hypospadias surgeries. Many patients report hesitancy in seeking medical attention as they mature through adolescence, despite significant distress, making surgeon-initiated long-term follow-up critically important. Our series has demonstrated positive long-term outcomes in adult hypospadias patients repaired as children. Patients were satisfied with their overall surgical result and function and appeared to be experiencing minimal long-term voiding and sexual sequelae. The most common functional complaints were hesitancy and spraying during micturition. Because hypospadias surgery is a constantly evolving art, long-term studies (into adulthood) will continue to be important and will need to be repeated for each new procedure developed if surgeons are to continue to provide an honest and meaningful account of their results.
Acknowledgments
Acknowledgement: Statistical analysis by AnalysisWorks Inc., Vancouver, BC.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
References
- 1.Jayanthi VR, McLorie GA, Khoury AE, et al. Functional characteristics of the reconstructed neourethra after island flap urethroplasty. J Urol 1995;153:1657-9. [PubMed] [Google Scholar]
- 2.Garibay JT, Reid C, Gonzalez R. Functional evaluation of the results of hypospadias surgery with uroflowmetry. J Urol 1995;154:835-6. [DOI] [PubMed] [Google Scholar]
- 3.Mureau MA, Slijper FM, Slob AK, et al. Satisfaction with penile appearance after hypospadias surgery: the patient and surgeon view. J Urol 1996;155:703-6. [PubMed] [Google Scholar]
- 4.Mureau MA, Slijper FM, van der Meulen JC, et al. Psychosexual adjustment of men who underwent hypospadias repair: a norm-related study. J Urol 1995;154:1351-5. [PubMed] [Google Scholar]
- 5.Mureau MA, Slijper FM, Nijman RJ, et al. Psychosexual adjustment of children and adolescents after different types of hypospadias surgery: a norm-related study. J Urol 1995; 154: 1902-7. [PubMed] [Google Scholar]
- 6.Sommerlad BC. A long-term follow-up of hypospadias patients. Br J Plast Surg 1975;28:324-30. [DOI] [PubMed] [Google Scholar]
- 7.Avellan L. The development of puberty, the sexual debut and sexual function in hypospadiacs. Scand J Plast Reconstr Surg 1976;10:29-44. [DOI] [PubMed] [Google Scholar]
- 8.Kenawi MM. Sexual function in hypospadiacs. Br J Urol 1975;47:883-90. [DOI] [PubMed] [Google Scholar]
- 9.Farkas LG, Hynie J. Aftereffects of hypospadias repair in childhood. Postgrad Med 1970; 47: 103-5. [DOI] [PubMed] [Google Scholar]
- 10.Berg R, Svensson J, Astrom G. Social and sexual adjustment of men operated for hypospadias during childhood: a controlled study. J Urol 1981;125:313-7. [DOI] [PubMed] [Google Scholar]
- 11.Bracka A. A long-term view of hypospadias. Br J Plast Surg 1989;42:251-5. [DOI] [PubMed] [Google Scholar]
- 12.Maier WA, Tewes G. Sexual function after operations for hypospadias according to Ombredanne. Prog Pediatr Surg 1984;17:79-82. [PubMed] [Google Scholar]
- 13.Nuininga JE. DE Gier RP, Verschuren R, et al. Long-term outcome of different types of 1-stage hypospadias repair. J Urol 2005;174:1544-8; discussion 1548. [DOI] [PubMed] [Google Scholar]
- 14.van der Werff JF, Ultee J. Long-term follow-up of hypospadias repair. Br J Plast Surg 2000; 53:588-92. [DOI] [PubMed] [Google Scholar]
- 15.Aho MO, Tammela OK, Tammela TL. Aspects of adult satisfaction with the result of surgery for hypospadias performed in childhood. Eur Urol 1997;32:218-22. [PubMed] [Google Scholar]
- 16.Barcat J. Current concepts in treatment. In: Horton CE, editor. Plastic and reconstructive surgery of the genital area. Boston: Little, Brown;1973, p. 249-63. [Google Scholar]
- 17.Wu WH, Chuang JH, Ting YC, et al. Developmental anomalies and disabilities associated with hypospadias. J Urol 2002;168:229-32. [PubMed] [Google Scholar]
- 18.Marrocco G, Vallasciani S, Fiocca G, et al. Hypospadias surgery: a 10-year review. Pediatr Surg Int 2004;20:200-3. [DOI] [PubMed] [Google Scholar]
- 19.Lam PN, Greenfield SP, Williot P. 2-stage repair in infancy for severe hypospadias with chordee: long-term results after puberty. J Urol 2005;174:1567-72; discussion 1572. [DOI] [PubMed] [Google Scholar]
- 20.Timing of elective surgery on the genitalia of male children with particular reference to the risks, benefits, and psychological effects of surgery and anesthesia. American Academy of Pediatrics. Pediatrics 1996;97:590-4. [PubMed] [Google Scholar]
- 21.Retik AB, Borer JG. Hypospadias, In: Retik AB, Vaughan ED, Wein AJ, et al., editors. Campbell's urology. 8th ed. Philadelphia: Saunders; 2002. p. 2291. [Google Scholar]
- 22.Nelson CP, Bloom DA, Kinast R, et al. Long-term patient reported outcome and satisfaction after oral mucosa graft urethroplasty for hypospadias. J Urol 2005;174:1075-8. [DOI] [PubMed] [Google Scholar]
- 23.Aho MO, Tammela OK, Somppi EM, et al. Sexual and social life of men operated in childhood for hypospadias and phimosis. A comparative study. Eur Urol 2000;37:95-100; discussion 101. [DOI] [PubMed] [Google Scholar]
- 24.Svensson J, Berg R, Berg G. Operated hypospadiacs: late follow-up. Social, sexual, and psychological adaptation. J Pediatr Surg 1981;16:134-5. [DOI] [PubMed] [Google Scholar]