Abstract
The lethal toxin produced by Bacillus anthracis is a bipartite toxin in which the first protein, protective antigen (PA), transports the second protein, lethal factor, across the host cell membrane. We have previously shown that CD8+ T-cell epitopes fused to a nontoxic derivative of lethal factor (LFn) are delivered into the host cell cytosol in a PA-dependent manner. Delivery of these antigens targets them to the intracellular major histocompatibility complex (MHC) class I processing and presentation pathway and leads to the stimulation of antigen-specific CD8+ T cells in vivo. In this report, we describe the generation and characterization of LFn fusion proteins that include not only a CD8+ T-cell epitope but also a CD4+ T-cell epitope. We first show that these fusion proteins induce antigen-specific CD4+ T-cell responses following incubation with dendritic cells in vitro or injection into mice. Stimulation of CD4+ T cells by LFn fusion proteins does not require PA but is enhanced by PA in vitro. We also show that a single LFn fusion protein and PA can deliver antigen to both the MHC class II and the MHC class I pathways, resulting in the simultaneous induction of antigen-specific CD4+ T cells and antigen-specific CD8+ T cells in the same mouse. These results suggest that this toxin delivery system is capable of stimulating protective immune responses where effective immunization requires stimulation of both classes of T cells.
CD8+ and CD4+ T lymphocytes are critical mediators of protection against many microbial pathogens (23, 40). CD8+ T cells are stimulated in response to foreign protein antigen present in the host cell cytosol and subsequently degraded by the proteasome (31). The resulting peptides are presented by surface major histocompatibility complex (MHC) class I (MHC-I) molecules to antigen-specific CD8+ T cells (18, 31). In contrast, CD4+ T cells are stimulated in response to exogenous protein antigen engulfed by professional antigen-presenting cells such as dendritic cells (DC) and processed into peptides by proteases along the endocytic pathway (38). These peptides are presented by MHC-II molecules to antigen-specific CD4+ T cells (18). Once primed, CD8+ and CD4+ T cells clonally expand and exert key antimicrobial effector functions. For example, CD8+ T cells can lyse infected target cells and secrete inflammatory cytokines such as gamma interferon (IFN-γ) (19, 40). CD4+ T cells can also secrete cytokines, as well as activate other immune cells, and provide help for a lasting and optimal CD8+ T-cell response (8, 23). Following a contraction phase, a percentage of these antigen-specific CD8+ and CD4+ T cells remains in the host for an extended period of time as memory cells. If a host is subsequently exposed to a pathogen recognized by the memory cells, then the memory cells can rapidly and effectively control the infection.
Because protection against a wide array of pathogens requires the activity of memory CD8+ and CD4+ T cells, there has been much interest in the development of safe vaccines that specifically stimulate these populations. One approach that our laboratory has taken to induce a CD8+ T-cell response is to fuse peptides recognized by CD8+ T cells to a derivative of anthrax lethal toxin (LT) lacking toxic activity (4-6, 14, 25). LT is secreted by Bacillus anthracis as a bipartite toxin consisting of protective antigen (PA) and lethal factor (LF) (30). PA has an inherent ability to transport the enzymatically active LF across a host cell membrane into the cytosol, where it can ultimately lead to host cell death (30). Cellular intoxication is initiated when PA binds one of its ubiquitously expressed cell surface receptors, ANTXR1 (11) or ANTXR2 (33), and oligomerizes on the cell surface (28). The resulting PA heptamer can bind up to three molecules of LF (29), and the entire toxin complex is endocytosed by cells in a receptor- and clathrin-dependent manner (1, 17). Acidification of the endosome triggers a conformational change in PA that leads to formation of a transmembrane pore (9, 24, 27). This pore can facilitate the translocation of catalytic LF molecules from the endosome into the cytosol (30). The first 255 amino acids of LF, termed LFn, retain PA-binding and translocation abilities but are entirely devoid of toxic activity, both in cell culture and in mice (2, 25). Therefore, CD8+ T-cell epitopes fused to LFn are delivered into the host cell cytosol by PA without affecting cell viability. We and others have previously shown that once in the cytosol, the fusion protein gains access to the classical MHC-I antigen processing and presentation pathway (6, 16, 26). We have further shown that the immunization of mice with LFn-antigen fusion proteins and PA results in the induction of antigen-specific, protective CD8+ T cells (5, 14).
Here we investigated whether LFn fusion proteins and PA could also be used to deliver antigen to the MHC-II pathway for the stimulation of antigen-specific CD4+ T cells. To test this, we fused a model CD4+ T-cell epitope from chicken ovalbumin (Ova) to nontoxic LFn and demonstrated that this recombinant protein induced an Ova-specific CD4+ T-cell response both in vitro and in mice. We went on to examine the role of PA in this process. Furthermore, we generated an LFn fusion protein bearing two epitopes from Ova, one restricted by MHC-II and one restricted by MHC-I, and showed that this single LFn fusion protein was capable of stimulating both Ova-specific CD4+ and Ova-specific CD8+ T-cell responses in mice.
MATERIALS AND METHODS
Recombinant anthrax LT proteins.
LFn-Ova323-339 (LFn-Ova323) and LFn-Ova323-339-Ova257-264 (LFn-Ova323-Ova257) were engineered as follows. The antigen tags were generated by annealing single-stranded DNA oligonucleotides (Integrated DNA Technologies, Coralville, IA) to form double-stranded DNA including (from 5′ to 3′) a BglII site, the sequence encoding the appropriate peptide antigen(s), two stop codons, an XhoI site, and a BglII site. This DNA fragment was ligated to pLFn (14), a pET15b vector (Novagen, Madison, WI) with the gene encoding LFn between the NdeI and BamHI sites of the multiple cloning region, which had previously been digested with BamHI. The plasmid encoding LFn-Ova257-264 (LFn-Ova257) was constructed as previously described (6).
Plasmids were transformed into Escherichia coli BL21(DE3) (Novagen) and expressed as previously described (37). The recombinant LFn fusion proteins contain a vector-encoded His6 tag at the amino terminus and were purified by Ni2+ affinity chromatography to greater-than-95% purity as determined by Coomassie staining. Wild-type PA, PAR178A (12), and PAK397D, D425K (35, 36) were generously provided by R. J. Collier (Harvard Medical School, Boston, MA).
Mice and immunizations.
C57BL/6 (CD45.2) and OT-II mice were obtained from the Jackson Laboratory (Bar Harbor, ME). OT-II are transgenic mice that express a Vα2/Vβ5 T-cell receptor (TCR) specific for Ova323 in the context of I-Ab MHC-II molecules (7) and were bred onto a congenic CD45.1 background in a specific-pathogen-free barrier facility at Harvard Medical School. OT-I mice on a CD45.1 background were a gift of C. Benoist (Harvard Medical School) and express a Vα2/Vβ5 TCR specific for Ova257 in the context of Kb MHC-I molecules (20).
Mice were immunized intraperitoneally (i.p.) with 150 pmol of the indicated LFn fusion protein plus or minus 30 pmol of wild-type or mutant PA (unless otherwise indicated) or with 150 pmol of native Ova protein (Sigma, St. Louis, MO), all in 200 μl of phosphate-buffered saline (PBS).
Flow cytometry.
Antibodies specific for CD8α, CD4, CD69, Vα2, and CD45.1 were obtained from BD Biosciences (San Jose, CA). Cells were analyzed on a BD Biosciences FACSCalibur flow cytometer and analyzed using FlowJo software (Tree Star, Ashland, OR).
In vivo T-cell proliferation.
Splenocytes and peripheral lymph nodes were harvested from OT-II or OT-I mice. Erythrocytes were lysed by hypotonic shock using ammonium chloride and potassium. On average, 24% of the cells harvested from OT-II mice were Vα2+ CD4+ and 34% of the cells harvested from OT-I mice were Vα2+ CD8+, as determined by flow cytometry. Cells were labeled with the intracellular fluorescent dye carboxyfluorescein diacetate succimidyl ester (CFSE) by incubation with 5 μM CFSE in PBS with 0.1% bovine serum albumin for 10 min at 37°C. Labeling was stopped by the addition of 5 volumes of cold RP-10 (RPMI 1640 [Invitrogen, Grand Island, NY]-10% fetal bovine serum-l-glutamine-HEPES-50 μM 2-mercaptoethanol-50 U/ml penicillin-50 μg/ml streptomycin). Cells were washed three times with PBS and injected intravenously into the tail veins of recipient C57BL/6 (CD45.2) mice. For cotransfers of OT-II and OT-I, 1 × 106 each of Vα2+ CD4+ OT-II cells and Vα2+ CD8+ OT-I cells were injected, and for transfers of OT-II only, 1 × 106 to 2 × 106 CD4+ Vα2+ OT-II cells were injected. Mice were immunized with the indicated protein(s) 1 day later. After 3 days, single-cell suspensions of spleens or peripheral lymph nodes (superficial cervical, inguinal, axillary, and brachial) pooled from individual mice were prepared, stained, and analyzed by flow cytometry. FlowJo's proliferation platform was used to analyze T cell proliferation, where “percent divided” is defined as the percentage of transgenic T cells in the starting population that divided (assuming that no cells died during the culture) and “proliferation index” is defined as the average number of divisions that those cells that divided (and that were present in the starting population) underwent.
Intracellular cytokine staining (ICCS).
Cells were stimulated for 6 h with 4 μM Ova323 peptide or 100 nM Ova257 peptide in the presence of GolgiPlug (BD Biosciences). Cells were surface stained, fixed, and permeabilized using the Cytofix/Cytoperm Plus kit (BD Biosciences) and stained intracellularly with anti-interleukin-2 (IL-2) or anti-IFN-γ antibody (BD Biosciences) as indicated. To determine the percentage of IFN-γ+ Ova257-specific T cells out of the total CD8+ T cells, the percentage of IFN-γ+ T cells from parallel unstimulated samples (no peptide) was subtracted from the peptide-stimulated value from the same mouse.
IFN-γ enzyme-linked immunospot (ELISPOT) analysis.
Spleens from experimental mice were harvested and erythrocytes were lysed. Serial dilutions of splenocytes were added to nitrocellulose-backed 96-well plates previously coated with rat anti-mouse IFN-γ antibody (BD Biosciences). Each well also contained 1 × 105 irradiated, Ova257 peptide-pulsed (1 μM), EL-4 (H-2b) thymoma cells. Plates were incubated for 24 h, washed, and treated with biotinylated rat anti-mouse IFN-γ antibody (BD Biosciences). After an additional 18 h, plates were washed and streptavidin-horseradish peroxidase (BD Biosciences) was added. The plates were developed with 1 mg/ml 3,3′-diaminobenzidine tetrahydrochloride dyhydrate (Bio-Rad, Hercules, CA) in 50 mM Tris (pH 7.9). The number of Ova257-specific T cells was determined by subtracting the number of spots in the presence of EL-4 cells alone from the number of spots when the T cells were incubated with peptide-pulsed EL-4 cells.
In vitro T-cell activation assay.
DC were cultured from the bone marrow of C57BL/6 mice as previously described (37). Cells were harvested after 6 days in culture and purified using anti-CD11c-conjugated MACS microbeads and magnetic separation columns (Miltenyi Biotec, Auburn, CA) (approximately 95% CD11c+ by flow cytometry). DC (5 × 105) were treated with the indicated concentrations of LFn fusion protein, wild-type or mutant PA, Ova protein, and/or Ova323 peptide in 1 ml of RP-10 for 2.5 h. Splenocytes and peripheral lymph node cells were isolated from OT-II mice as described above and enriched for T cells in anti-CD90.2-conjugated MACS microbeads and magnetic separation columns (Miltenyi Biotec). A total of 5 × 105 Vα2+ CD4+ OT-II cells in 500 μl of RP-10 were added to treated DC. T cells were analyzed approximately 16 h later by flow cytometry for CD69 expression.
Statistical analysis.
Data are expressed as means ± standard deviations. Statistical significance of differences was analyzed using a two-tailed Student's t test for paired samples (Fig. 1; also see Fig. 3 below) or independent samples (see Fig. 4 below). In all cases, a P value of <0.05 was considered statistically significant.
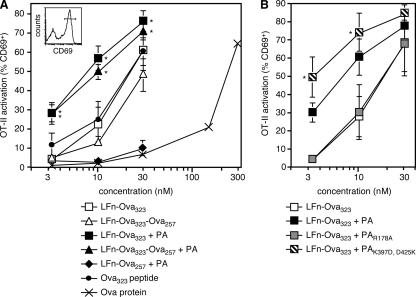
FIG. 1.
DC treated with LFn fused to Ova323 activate Ova-specific CD4+ T cells by both PA-independent and PA-dependent mechanisms. Bone marrow-derived DC were treated with the indicated concentrations of each protein (1:1 ratio of LFn fusion protein:PA when both added) or peptide. PAR178A cannot bind LFn and PAK397D, D425K is a translocation mutant. Ova-specific CD4+ OT-II T cells were added to treated DC and the percentage of OT-II cells (Vα2+ CD4+) that were activated (CD69+) was determined by flow cytometry 16 h later. Cells were determined to be CD69+ if they fell within the gate shown in the inset histogram, which is a representative plot of OT-II cells that were incubated with DC treated with 30 nM of LFn-Ova323. Graphs indicate the average percentage of activated OT-II for each treatment condition. (A) Results are the average of five independent experiments, except for the Ova protein-treated group, for which the plotted data are representative of two independent experiments. *, P < 0.05 versus treatment with the same concentration of the same LFn fusion protein, but without PA. (B) Results are the average of three independent experiments. *, P < 0.05 versus treatment with the same concentration of LFn-Ova323 plus PA.
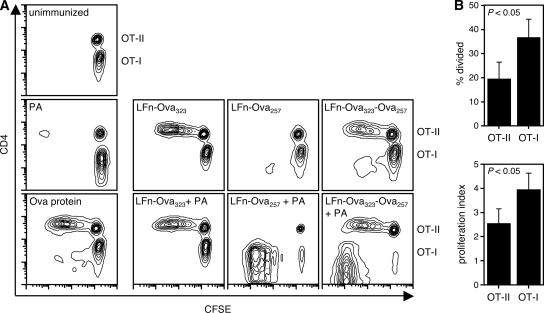
FIG. 3.
Antigen fused to LFn can induce the proliferation of both antigen-specific CD4+ and antigen-specific CD8+ T cells in vivo. C57BL/6 (CD45.2+) mice were injected with a 1:1 mixture of CFSE-labeled OT-II (CD45.1+ Vα2+ CD4+) and CFSE-labeled OT-I (CD45.1+ Vα2+ CD8+) T cells. The following day, groups of mice were immunized i.p. with 150 pmol of the indicated LFn fusion protein plus or minus 30 pmol of PA or with 150 pmol of Ova protein. Peripheral lymph nodes were harvested from the mice 3 days later and the proliferation of transferred T cells was analyzed by flow cytometry. (A) Contour plots are gated on transferred T cells (CD45.1+ CD4+ cells plus CD45.1+ CD8+ cells) and separated by CD4 staining. Data are representative of two to four mice per group. (B) Percentage of transferred OT-II T cells that divided at least once (percent divided) and the average number of divisions that a dividing transferred cell underwent (proliferation index) of four mice immunized with LFn-Ova323-Ova257 plus PA.
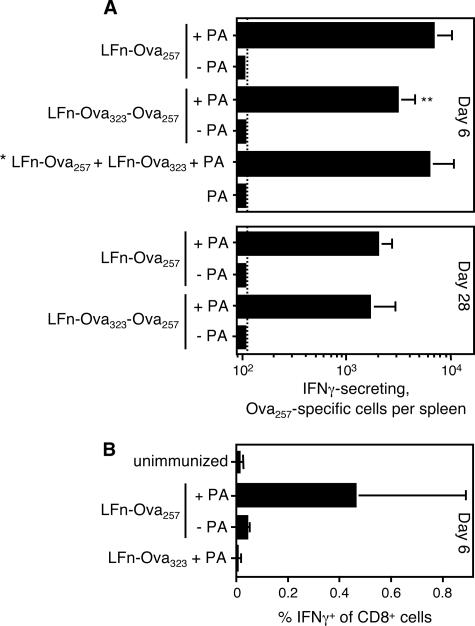
FIG. 4.
Endogenous Ova-specific CD8+ T cells expand and produce IFN-γ following immunization of mice with LFn fused to Ova257. Groups of C57BL/6 mice were immunized i.p. with 150 pmol of the indicated LFn fusion protein plus or minus 30 pmol of PA. The group designated by an asterisk was immunized with 150 pmol of LFn-Ova257 plus 150 pmol of LFn-Ova323 plus 60 pmol of PA. The frequency of splenic Ova257-specific T cells was measured by IFN-γ ELISPOT analysis (A) or ICCS (B) 6 or 28 days later. The dashed line indicates the limit of detection for the ELISPOT assay. Data represent the average values for 3 to 11 mice per group (except data for PA only-immunized group, which are the mean values for two mice) and are compiled from several independent experiments. **, P < 0.01 (compared to mice immunized with LFn-Ova257 plus PA; 11 mice in each of these two groups).
RESULTS
DC treated with LFn fused to a CD4+ T-cell antigen activate antigen-specific CD4+ T cells in vitro.
To generate an LFn fusion protein bearing an MHC-II-restricted CD4+ T-cell epitope, we fused DNA encoding Ova323, a CD4+ T-cell epitope from Ova, to the 3′ end of DNA encoding LFn. This genetic fusion was expressed in Escherichia coli and the resulting LFn-Ova323 protein was purified from cell extracts. We also tested a second LFn fusion protein that had the potential to stimulate both CD4+ and CD8+ T cells. This second fusion protein, LFn-Ova323-Ova257, contains both Ova323 and the MHC-I-restricted CD8+ T-cell epitope Ova257. Because the lethal C-terminal catalytic domain of LF is not contained within LFn, these fusion proteins are completely nontoxic to host cells.
To test whether these LFn fusion proteins would gain access to the MHC-II processing and presentation pathway of murine cells in vitro, we incubated bone marrow-derived DC with either LFn-Ova323 or LFn-Ova323-Ova257. We then assayed for the presentation of Ova323 on MHC-II molecules by incubating the DC with naïve Ova-specific CD4+ T cells isolated from OT-II TCR transgenic mice. We used flow cytometry to monitor CD69 upregulation on the CD4+ T cells as an indicator of T-cell activation. As shown in Fig. 1A, both LFn-Ova323 and LFn-Ova323-Ova257 induced Ova-specific CD4+ T-cell activation in a dose-dependent manner and over a similar concentration range. Importantly, LFn-Ova257, a control protein bearing only the Ova-derived CD8+ T-cell epitope (6), did not induce Ova-specific CD4+ T-cell activation (either in the presence or absence of PA) (Fig. 1A and data not shown), demonstrating the specificity of the response. Proteolytic release of Ova323 from LFn-Ova323 and LFn-Ova323-Ova257 seemed relatively efficient, even in the latter case, where the epitope is buried within the fusion protein. Specifically, both of the Ova323-bearing fusion proteins induced extents of T-cell activation similar to those seen for an equivalent molar concentration of commercially synthesized Ova323 peptide (Fig. 1A). Furthermore, to achieve the same level of T-cell activation using native Ova protein as achieved by LFn-Ova323 or LFn-Ova323-Ova257, DC had to be treated with an approximately 10-fold-greater concentration of protein (Fig. 1A). Proteolysis of the fusion proteins required cellular factor(s), because fixing the DC with formaldehyde severely inhibited T-cell activation induced by LFn-Ova323 or LFn-Ova323-Ova257 but not activation induced by unconjugated Ova323 peptide (data not shown). Together these results show that LFn fusion proteins gain access to the MHC-II pathway of DC in vitro and induce the activation of CD4+ T cells in an efficient and antigen-specific manner.
Although we have previously shown that PA is required for the stimulation of antigen-specific CD8+ T cells in the LT-based system (4, 5, 25), the data presented here clearly demonstrate that PA is not required for the stimulation of antigen-specific CD4+ T cells. This is perhaps not surprising considering the fact that DC are naturally able to engulf exogenous material, digest the protein content with vacuolar proteases, and present the resulting peptides on MHC-II molecules to antigen-specific CD4+ T cells (18). We wondered, however, whether the addition of PA might affect CD4+ T-cell activation in this system. To investigate this possibility, we incubated DC with either LFn-Ova323 or LFn-Ova323-Ova257 in the presence of PA and compared the level of T-cell activation to that observed in the absence of PA. Interestingly, we found that PA significantly increased the percentage of activated CD4+ T cells at all toxin concentrations tested (Fig. 1A). We also pulsed DC with LFn-Ova323 and mutant PA bearing an R178A substitution (PAR178A) that disrupts its ability to bind LFn but does not affect its ability to oligomerize or interact with host cells (12). In contrast to wild-type PA, PAR178A did not enhance T-cell activation above the level induced by LFn-Ova323 alone (Fig. 1B). These results demonstrate that the stimulatory effect of PA required a direct interaction between PA and LFn fusion proteins and therefore was not due to nonspecific DC activation. We suspected that by binding LFn fusion proteins and facilitating their delivery into endosomal compartments, wild-type PA had the effect of increasing the concentration of antigen with access to the vacuolar MHC-II processing pathway and ultimately presented to CD4+ T cells. However, PA-mediated translocation of LFn fusion proteins from the endosome into the cytosol might reduce the effective antigen pool. Therefore, we wondered whether Ova-specific CD4+ T-cell activation would be further enhanced if PA-mediated translocation were inhibited, trapping LFn fusion proteins in the endosome. To test this, we treated DC with LFn-Ova323 and PAK397D, D425K, a translocation mutant bearing two amino acid substitutions that block pore formation and translocation but not cellular receptor binding, oligomerization, or LFn binding (35, 36). Under these conditions, Ova-specific CD4+ T-cell activation was significantly greater than that observed with LFn-Ova323 and wild-type PA (Fig. 1B). This suggests that some of the antigen delivered into endosomes by wild-type PA is subsequently translocated into the cytosol and sequestered away from the MHC-II pathway. In summary, LFn-Ova323 and LFn-Ova323-Ova257 can induce the activation of Ova-specific CD4+ T cells in vitro by both PA-independent and PA-dependent mechanisms, and the PA-dependent mechanism most likely involves PA-mediated delivery of LFn fusion proteins to the endosomal MHC-II pathway of DC.
Ova-specific CD4+ T cells proliferate and produce IL-2 in mice immunized with LFn carrying the Ova323 epitope.
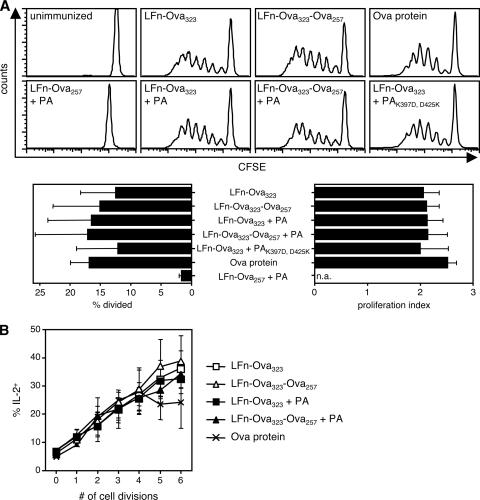
Once we found that both LFn-Ova323 and LFn-Ova323-Ova257 could deliver antigen to the MHC-II pathway of host DC in vitro, we wanted to test whether Ova-specific CD4+ T cells were stimulated in vivo following immunization of mice with these fusion proteins. Therefore, we adoptively transferred CFSE-labeled, Ova-specific CD4+ T cells from OT-II TCR transgenic mice into the tail veins of C57BL/6 mice. The following day, groups of recipient mice were immunized i.p. with 150 pmol (approximately 5 μg) of either LFn-Ova323 or LFn-Ova323-Ova257. Three days later, we used flow cytometry to analyze T-cell proliferation. As shown in Fig. 2A, adoptively transferred Ova-specific CD4+ T cells lost CFSE fluorescence, demonstrating that they proliferated extensively in peripheral lymph nodes of LFn-Ova323-immunized or LFn-Ova323-Ova257-immunized mice. We observed a similar level of T-cell proliferation in a parallel group of mice immunized with the same molar concentration of full-length Ova protein but essentially no T-cell proliferation in groups of unimmunized or LFn-Ova257-plus-PA-immunized mice (Fig. 2A). The proliferation profile seen 3 days postimmunization was similar to that observed 5 days postimmunization, except that at the later time point proliferating CD4+ T cells could also be detected in the spleens of the immunized mice (data not shown). Collectively, these data demonstrate that LFn fusion proteins can elicit PA-independent, antigen-specific CD4+ T-cell responses in vivo.
FIG. 2.
Ova-specific CD4+ T cells transferred into mice proliferate and produce IL-2 in response to LFn fused to Ova323. C57BL/6 mice (CD45.2+) were injected with CFSE-labeled OT-II T cells (CD45.1+ Vα2+ CD4+). The following day, groups of mice were left unimmunized, were immunized i.p. with 150 pmol of the indicated LFn fusion protein plus or minus 30 pmol of PA (wild type or K397D, D425K translocation mutant), or were immunized i.p. with 150 pmol of Ova protein. Peripheral lymph nodes were harvested from the mice 3 days later. (A) Flow cytometry was used to analyze the proliferation of OT-II cells and histograms are gated on CD45.1+ CD4+ cells. Graphs indicate the average percentage of transferred OT-II T cells that divided at least once (percent divided) and the average number of divisions that a dividing transferred cell underwent (proliferation index) of four to nine mice per group, compiled from several independent experiments. n.a., not applicable. (B) Average percentage of OT-II cells in each cell division peak that were IL-2+ after brief ex vivo stimulation with Ova323 peptide.
To determine whether PA could also enhance CD4+ T-cell stimulation in vivo, we again immunized groups of mice with LFn-Ova323 or LFn-Ova323-Ova257 but now included 30 pmol (2.5 μg) of either wild-type PA or PAK397D, D425K (the mutant that blocks translocation of LFn fusion proteins into the cytosol). In contrast to the in vitro results described above, the addition of wild-type PA or PAK397D, D425K did not affect either the percentage of transgenic T cells in the starting population that divided (percent divided) or the average number of cell divisions completed by a proliferating cell present in the starting population (proliferation index) (Fig. 2A). In other words, in vivo CD4+ T-cell proliferation was not enhanced (or inhibited) by PA at the tested protein concentrations.
Many of the proliferating Ova-specific CD4+ T cells isolated from mice immunized with Ova323-containing proteins produced the growth cytokine IL-2 (Fig. 2B). Furthermore, the percentage of IL-2+ cells positively correlated with the number of rounds of cell division (Fig. 2B). In contrast, very little IL-2 was produced by the undivided OT-II cells isolated from these same immunized mice (Fig. 2B), and less than 5% of OT-II cells isolated from LFn-Ova257-plus-PA-immunized or unimmunized mice were IL-2+ (data not shown). We could detect no IFN-γ or IL-4 production by the proliferating OT-II cells (data not shown).
Antigen fused to LFn simultaneously induces the proliferation of both CD4+ and CD8+ T cells in vivo.
Work from our laboratory has previously shown that LFn-antigen fusion proteins plus PA can induce antigen-specific CD8+ T-cell responses in mice (4-6, 14, 25). Here we wanted to examine the capacity of a single LFn fusion protein to deliver epitopes to both the MHC-II and the MHC-I processing and presentation pathways, resulting in the induction of both CD4+ and CD8+ T-cell responses in the same mouse. Therefore, we adoptively transferred a 1:1 mixture of CFSE-labeled, Ova-specific CD4+ and CD8+ T cells (isolated from OT-II and OT-I TCR transgenic mice, respectively) into recipient mice. The following day, we immunized groups of these mice with LFn-Ova323-Ova257, LFn-Ova323, or LFn-Ova257. Each fusion protein was administered both with and without PA. Three days later, we measured the proliferation of the CFSE-labeled T cells in the peripheral lymph nodes of the mice by flow cytometry. Ova-specific CD4+ and Ova-specific CD8+ T cells both proliferated extensively in mice immunized with LFn-Ova323-Ova257 plus PA, whereas essentially none of the transferred T cells proliferated in parallel groups of unimmunized or PA only-immunized mice (Fig. 3A). The specificity of the T-cell response was evident for mice immunized with the toxin fusion proteins bearing only the MHC-II- or the MHC-I-restricted epitope, where only the CD4+ T cells or the CD8+ T cells proliferated, respectively (Fig. 3A). We further confirmed that CD8+ T-cell proliferation was PA dependent and CD4+ T-cell proliferation was not (Fig. 3A), again demonstrating that PA is required to deliver antigen to the MHC-I pathway but not to the MHC-II pathway of host cells. Together these data show that a single LFn fusion protein and PA can deliver antigen to both the MHC-II and the MHC-I pathways for stimulation of both antigen-specific CD4+ and CD8+ T cells.
These data also allowed us to directly compare the Ova-specific CD8+ and CD4+ T-cell responses in individual mice immunized with LFn-Ova323-Ova257 plus PA. We found that a significantly greater percentage of the transferred CD8+ T cells divided at least once, and on average a proliferating CD8+ T cell went through a greater number of cell divisions (Fig. 3B). The differential CD8+ and CD4+ T-cell responses could not be accounted for by differences in antigen load, because LFn-Ova323-Ova257 contains a 1:1 ratio of each peptide epitope. We also compared the T-cell response induced by LFn-Ova323-Ova257 plus PA to that induced by the same molar amount of Ova protein (also injected i.p.). While both immunizations induced similar Ova-specific CD4+ T-cell responses, only LFn-Ova323-Ova257 plus PA induced a robust Ova-specific CD8+ T-cell response (Fig. 3A). In other words, the Ova257 epitope was more efficiently delivered to the intracellular MHC-I processing and presentation pathway by the toxin-based system than as a native protein.
Endogenous Ova-specific CD8+ T cells are stimulated and produce IFN-γ in mice immunized with LFn fused to Ova257.
We have previously shown that CD4 knockout mice are unable to generate an endogenous CD8+ T-cell response following immunization with LFn fusion proteins and PA (4). This implies that CD4+ T cells are required for the stimulation and/or maintenance of antigen-specific CD8+ T cells in this system, and furthermore, that an antigenic epitope recognized by CD4+ T cells might be contained within the LFn or PA backbone. We wanted to determine whether adding a known CD4+ T-cell epitope to the LFn-Ova257 fusion protein would affect the magnitude of the endogenous Ova257-specific CD8+ T-cell response. In this experiment, we immunized groups of mice with 150 pmol of LFn-Ova257 or LFn-Ova323-Ova257, each plus or minus 30 pmol of PA. Six days later, at the peak of the endogenous CD8+ T-cell response (data not shown), we measured the frequency of Ova257-specific T cells by IFN-γ ELISPOT assay or ICCS. As shown in Fig. 4, we detected a burst of Ova-specific, IFN-γ-producing CD8+ T cells in the spleens of the immunized mice at this time point. As expected, given our previously published observations (4-6, 25) and the proliferation data above, CD8+ T-cell stimulation was entirely PA dependent (Fig. 4A and B). The endogenous CD8+ T-cell response was also antigen specific, because the Ova-specific CD8+ T-cell pool did not expand in a parallel group of mice immunized with LFn-Ova323 plus PA (Fig. 4B). Interestingly, we found that the number of Ova257-specific, IFN-γ-producing CD8+ T cells was not boosted by the addition of the Ova323 epitope but was instead significantly depressed (Fig. 4A). One possible explanation was that the stimulation of Ova-specific CD4+ T cells negatively impacted the stimulation of Ova-specific CD8+ T cells. Alternatively, the Ova257 epitope in the longer LFn fusion protein might be less efficiently delivered to the MHC-I pathway and/or less efficiently degraded than the same epitope in the shorter protein, resulting in less presentation of Ova257 to T cells. In an attempt to distinguish between these possibilities, we immunized mice with PA plus 150 pmol of each LFn-Ova257 and LFn-Ova323. This immunization contains the same molar quantity of each epitope as 150 pmol of LFn-Ova323-Ova257, but in the former the epitopes are in trans, while in the latter they are in cis. We found that the frequency of Ova-specific CD8+ T cells in LFn-Ova257-plus-LFn-Ova323-plus-PA-immunized mice was restored to that observed for LFn-Ova257-plus-PA-immunized mice (Fig. 4A). This suggests that by itself the Ova323 epitope is not inhibitory but that its proximity to Ova257 in the longer protein results in less presentation of Ova257 peptide to CD8+ T cells. It is noteworthy that the Ova323 epitope did not seem to have a negative impact on LFn-Ova323-Ova257-induced proliferation of adoptively transferred OT-I CD8+ T cells (Fig. 3A), perhaps due to the high precursor frequency of T cells in those experiments or to differences in the T-cell response between the spleen and the peripheral lymph nodes.
To determine whether the endogenous Ova-specific CD8+ T-cell response induced by LFn-Ova257 plus PA and LFn-Ova323-Ova257 plus PA would persist, we measured the frequencies of these T cells in the spleen 28 days postimmunization. Ova-specific, IFN-γ-producing CD8+ T cells were readily detectable at this later time point, but the pool had contracted 71% in mice immunized with LFn-Ova257 plus PA, and 58% in mice immunized with LFn-Ova323-Ova257 plus PA (Fig. 4A). Again, the frequency of Ova257-specific CD8+ T cells was less for mice immunized with LFn-Ova323-Ova257 plus PA than for mice immunized with LFn-Ova257 plus PA, although the difference was not statistically significant at this time point.
DISCUSSION
We have generated nontoxic anthrax LT fusion proteins bearing a heterologous CD4+ T-cell antigen from Ova and demonstrated that treatment of DC with these fusion proteins results in the activation of naïve Ova-specific CD4+ T cells in vitro. We have also shown that Ova-specific CD4+ T cells proliferate in mice following a single i.p. injection with 150 pmol of LFn fused to the Ova-derived CD4+ T-cell epitope. We have previously reported that an LT-based system can induce the stimulation of antigen-specific CD8+ T cells (4-6, 14, 25). The results presented here extend the capabilities of this antigen delivery system to now include the stimulation of antigen-specific CD4+ T cells. One key difference between these two applications of the system is that LFn fusion proteins on their own (without PA) are sufficient to induce only a CD4+ T-cell response. Because LFn is not thought to induce its own uptake into cells in the absence of PA, the engulfment of LFn fusion proteins by DC during the constitutive process of antigen sampling must deliver a level of antigen to the MHC-II processing and presentation pathway sufficient to elicit a measurable CD4+ T-cell response. In agreement with our findings, PA-independent delivery of LFn-antigen fusion proteins to the MHC-II pathway of host cells in vitro has been previously demonstrated using human peripheral blood mononuclear cells (26). These studies also showed that presentation of the antigenic epitope required endosomal processing and was MHC-II restricted (26).
Because we were interested in using the LT-based system to simultaneously induce CD4+ and CD8+ T cells, and we knew that inclusion of PA would be necessary to induce a CD8+ T-cell response (4, 5, 25), we investigated what effect PA would have on the induction of CD4+ T cells. Interestingly, we found that PA significantly enhanced the in vitro activation of antigen-specific CD4+ T cells. Because PAR178A (which cannot bind LFn) did not have this stimulatory effect, we were able to conclude that enhancement of CD4+ T-cell activation required a direct interaction between PA and LFn. We postulate that the ability of PA to bind LFn fusion proteins and recruit them specifically to host endosomal compartments increases the amount of antigen delivered to the vacuolar MHC-II pathway. Our finding that the PAK397D, D425K translocation mutant further amplified the CD4+ T-cell response supports this hypothesis and suggests that PA-mediated translocation of LFn fusion proteins out of the endosome and into the cytosol effectively limits the potential pool of antigen with access to the MHC-II pathway. This translocation step must not be 100% efficient, however, leaving sufficient antigen in the endosome to explain the overall increase in T-cell activation in the presence of wild-type PA. We do not yet know whether the PA-independent pathway of LFn fusion protein acquisition by DC is at all affected by the addition of PA to the cells. Therefore, we cannot state what fraction of the observed CD4+ T-cell response in the presence of PA was due to antigen uptake by PA-dependent versus PA-independent pathways.
Surprisingly, we were not able to detect a stimulatory effect of PA on LFn-Ova323- or LFn-Ova323-Ova257-induced CD4+ T-cell stimulation in mice. Perhaps the in vivo assays were not sensitive enough to detect small differences in antigen presentation or T-cell activation. Alternatively, PA-dependent effects may be evident only at toxin immunization doses other than those tested in this study. We should also emphasize that the cellular receptors for PA are widely distributed in mouse tissue (10, 11, 33). Therefore, including PA in the LFn-Ova323 or LFn-Ova323-Ova257 immunization may target the delivery of LFn fusion proteins not only to DC but also to many other cell types. Any PA-mediated enhancement of antigen delivery to the MHC-II pathway of DC may be offset by an adsorption of the antigen by other cell types that do not express MHC-II and cannot stimulate CD4+ T cells.
We went on to demonstrate that many of the Ova-specific CD4+ T cells that proliferated in mice immunized with LFn-Ova323 or LFn-Ova323-Ova257 produced the growth cytokine IL-2. However, they did not produce a detectable quantity of either the TH1 cytokine IFN-γ or the TH2 cytokine IL-4. The Mosmann laboratory has described a similar cytokine production profile by antigen-specific CD4+ T cells stimulated in response to i.p. injection of other soluble proteins (13, 39). This expanded pool of primed IL-2+ IFN-γ− IL-4− CD4+ T cells was termed “uncommitted” because these cells had the potential to subsequently differentiate into either TH1 or TH2 cells under the appropriate polarizing conditions (39). We are interested in determining whether the Ova-specific CD4+ T cells primed in response to LT-based fusion protein immunization also possess these qualities.
We have also shown that LFn-Ova323-Ova257 plus PA simultaneously induced the proliferation of both Ova-specific CD4+ and CD8+ T cells in the same mouse. While the CD4+ T-cell response was not affected by PA and was initially restricted to the peripheral lymph nodes, the CD8+ response required PA, was detectable both in the spleen and the peripheral lymph nodes, and was more robust than the CD4+ T-cell response. There are several possible explanations for why the CD8+ T-cell response was more robust. For example, delivery of LFn fusion protein to the cytosolic MHC-I antigen processing pathway may be more efficient than delivery to the endosomal MHC-II antigen processing pathway. Alternatively, proteolytic release of the Ova257 peptide may be more efficient than release of the Ova323 peptide. Furthermore, the stimulation of CD4+ T cells is generally thought to require a greater quantity and longer persistence of cognate antigen than the stimulation of CD8+ T cells (3, 21, 22, 34). Therefore, the Ova-specific CD4+ T-cell response might be more robust if mice were immunized with a larger dose of LFn fusion protein, or if the antigen were made to persist by giving several injections of protein spread over time. Finally, it is possible that the (relatively) weaker CD4+ T-cell response was an artifact of the adoptive transfer experiment, as clonal competition between an artificially high number of precursor T cells has previously been shown to specifically inhibit the proliferation of CD4+ T cells (15).
When characterizing the endogenous CD8+ T-cell response to LFn-Ova257 plus PA or LFn-Ova323-Ova257 plus PA, we observed an expanded pool of Ova257-specific T cells in the spleens of mice immunized 6 or 28 days earlier. Unlike the Ova-specific CD4+ T cells, these CD8+ T cells produced IFN-γ. We have previously shown that CD4+ T-cell help is required for stimulation of antigen-specific CD8+ T cells by the LT-based system (4). However, mice injected with LFn-Ova323-Ova257, bearing a known CD4+ T-cell antigen, did not have a greater frequency of primary or memory endogenous Ova257-specific CD8+ T cells than mice injected with LFn-Ova257 without the addition of the CD4+ T-cell epitope. It is possible that optimal CD4+ T-cell help is provided by antigen-nonspecific CD4+ T cells or by CD4+ T cells stimulated in response to an epitope within the toxin backbone and therefore that stimulation of Ova-specific CD4+ T cells does not have an additive benefit. Alternatively, LFn-Ova323-Ova257 may not stimulate a sufficiently robust Ova-specific CD4+ T-cell response or may stimulate CD4+ T cells that are incapable of providing help to CD8+ T cells.
In conclusion, we have demonstrated the ability of nontoxic LT bearing heterologous MHC-II- and MHC-I-restricted epitopes to simultaneously induce antigen-specific CD4+ and CD8+ T-cell responses in mice. Besides the LT-based system developed in our laboratory, other detoxified bacterial toxins, such as Bordetella pertussis adenylate cyclase toxin, have been used to induce both antigen-specific CD4+ and CD8+ T cells (32). These studies, together with our findings, underscore the versatility of toxins as antigen delivery vehicles. Systems such as these that target antigen to the cytosolic MHC-I pathway as well as the endosomal MHC-II pathway without any resulting toxicity are potentially attractive vaccine candidates.
Acknowledgments
We thank Adrianus van der Velden for his critical review of the manuscript.
This work was supported by National Institutes of Health grant AI055962 to M.N.S.
Editor: V. J. DiRita
Footnotes
Published ahead of print on 17 March 2008.
REFERENCES
- 1.Abrami, L., S. Liu, P. Cosson, S. H. Leppla, and F. G. van der Goot. 2003. Anthrax toxin triggers endocytosis of its receptor via a lipid raft-mediated clathrin-dependent process. J. Cell Biol. 160321-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arora, N., and S. H. Leppla. 1993. Residues 1-254 of anthrax toxin lethal factor are sufficient to cause cellular uptake of fused polypeptides. J. Biol. Chem. 2683334-3341. [PubMed] [Google Scholar]
- 3.Bajenoff, M., O. Wurtz, and S. Guerder. 2002. Repeated antigen exposure is necessary for the differentiation, but not the initial proliferation, of naive CD4+ T cells. J. Immunol. 1681723-1729. [DOI] [PubMed] [Google Scholar]
- 4.Ballard, J. D., R. J. Collier, and M. N. Starnbach. 1998. Anthrax toxin as a molecular tool for stimulation of cytotoxic T lymphocytes: disulfide-linked epitopes, multiple injections, and role of CD4+ cells. Infect. Immun. 664696-4699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ballard, J. D., R. J. Collier, and M. N. Starnbach. 1996. Anthrax toxin-mediated delivery of a cytotoxic T-cell epitope in vivo. Proc. Natl. Acad. Sci. USA 9312531-12534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ballard, J. D., A. M. Doling, K. Beauregard, R. J. Collier, and M. N. Starnbach. 1998. Anthrax toxin-mediated delivery in vivo and in vitro of a cytotoxic T-lymphocyte epitope from ovalbumin. Infect. Immun. 66615-619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnden, M. J., J. Allison, W. R. Heath, and F. R. Carbone. 1998. Defective TCR expression in transgenic mice constructed using cDNA-based α- and β-chain genes under the control of heterologous regulatory elements. Immunol. Cell Biol. 7634-40. [DOI] [PubMed] [Google Scholar]
- 8.Bevan, M. J. 2004. Helping the CD8+ T-cell response. Nat. Rev. Immunol. 4595-602. [DOI] [PubMed] [Google Scholar]
- 9.Blaustein, R. O., T. M. Koehler, R. J. Collier, and A. Finkelstein. 1989. Anthrax toxin: channel-forming activity of protective antigen in planar phospholipid bilayers. Proc. Natl. Acad. Sci. USA 862209-2213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonuccelli, G., F. Sotgia, P. G. Frank, T. M. Williams, C. J. de Almeida, H. B. Tanowitz, P. E. Scherer, K. A. Hotchkiss, B. I. Terman, B. Rollman, A. Alileche, J. Brojatsch, and M. P. Lisanti. 2005. ATR/TEM8 is highly expressed in epithelial cells lining Bacillus anthracis' three sites of entry: implications for the pathogenesis of anthrax infection. Am. J. Physiol. Cell Physiol. 288C1402-C1410. [DOI] [PubMed] [Google Scholar]
- 11.Bradley, K. A., J. Mogridge, M. Mourez, R. J. Collier, and J. A. Young. 2001. Identification of the cellular receptor for anthrax toxin. Nature 414225-229. [DOI] [PubMed] [Google Scholar]
- 12.Cunningham, K., D. B. Lacy, J. Mogridge, and R. J. Collier. 2002. Mapping the lethal factor and edema factor binding sites on oligomeric anthrax protective antigen. Proc. Natl. Acad. Sci. USA 997049-7053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Divekar, A. A., D. M. Zaiss, F. E. Lee, D. Liu, D. J. Topham, A. J. Sijts, and T. R. Mosmann. 2006. Protein vaccines induce uncommitted IL-2-secreting human and mouse CD4 T cells, whereas infections induce more IFN-γ-secreting cells. J. Immunol. 1761465-1473. [DOI] [PubMed] [Google Scholar]
- 14.Doling, A. M., J. D. Ballard, H. Shen, K. M. Krishna, R. Ahmed, R. J. Collier, and M. N. Starnbach. 1999. Cytotoxic T-lymphocyte epitopes fused to anthrax toxin induce protective antiviral immunity. Infect. Immun. 673290-3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Foulds, K. E., and H. Shen. 2006. Clonal competition inhibits the proliferation and differentiation of adoptively transferred TCR transgenic CD4 T cells in response to infection. J. Immunol. 1763037-3043. [DOI] [PubMed] [Google Scholar]
- 16.Goletz, T. J., K. R. Klimpel, N. Arora, S. H. Leppla, J. M. Keith, and J. A. Berzofsky. 1997. Targeting HIV proteins to the major histocompatibility complex class I processing pathway with a novel gp120-anthrax toxin fusion protein. Proc. Natl. Acad. Sci. USA 9412059-12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gordon, V. M., S. H. Leppla, and E. L. Hewlett. 1988. Inhibitors of receptor-mediated endocytosis block the entry of Bacillus anthracis adenylate cyclase toxin but not that of Bordetella pertussis adenylate cyclase toxin. Infect. Immun. 561066-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guermonprez, P., J. Valladeau, L. Zitvogel, C. Thery, and S. Amigorena. 2002. Antigen presentation and T cell stimulation by dendritic cells. Annu. Rev. Immunol. 20621-667. [DOI] [PubMed] [Google Scholar]
- 19.Harty, J. T., A. R. Tvinnereim, and D. W. White. 2000. CD8+ T cell effector mechanisms in resistance to infection. Annu. Rev. Immunol. 18275-308. [DOI] [PubMed] [Google Scholar]
- 20.Hogquist, K. A., S. C. Jameson, W. R. Heath, J. L. Howard, M. J. Bevan, and F. R. Carbone. 1994. T cell receptor antagonist peptides induce positive selection. Cell 7617-27. [DOI] [PubMed] [Google Scholar]
- 21.Iezzi, G., K. Karjalainen, and A. Lanzavecchia. 1998. The duration of antigenic stimulation determines the fate of naive and effector T cells. Immunity 889-95. [DOI] [PubMed] [Google Scholar]
- 22.Kaech, S. M., and R. Ahmed. 2001. Memory CD8+ T cell differentiation: initial antigen encounter triggers a developmental program in naive cells. Nat. Immunol. 2415-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaufmann, S. H. 1993. Immunity to intracellular bacteria. Annu. Rev. Immunol. 11129-163. [DOI] [PubMed] [Google Scholar]
- 24.Koehler, T. M., and R. J. Collier. 1991. Anthrax toxin protective antigen: low-pH-induced hydrophobicity and channel formation in liposomes. Mol. Microbiol. 51501-1506. [DOI] [PubMed] [Google Scholar]
- 25.Lu, Y., R. Friedman, N. Kushner, A. Doling, L. Thomas, N. Touzjian, M. Starnbach, and J. Lieberman. 2000. Genetically modified anthrax lethal toxin safely delivers whole HIV protein antigens into the cytosol to induce T cell immunity. Proc. Natl. Acad. Sci. USA 978027-8032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McEvers, K., M. Elrefaei, P. Norris, S. Deeks, J. Martin, Y. Lu, and H. Cao. 2005. Modified anthrax fusion proteins deliver HIV antigens through MHC class I and II pathways. Vaccine 234128-4135. [DOI] [PubMed] [Google Scholar]
- 27.Milne, J. C., and R. J. Collier. 1993. pH-dependent permeabilization of the plasma membrane of mammalian cells by anthrax protective antigen. Mol. Microbiol. 10647-653. [DOI] [PubMed] [Google Scholar]
- 28.Milne, J. C., D. Furlong, P. C. Hanna, J. S. Wall, and R. J. Collier. 1994. Anthrax protective antigen forms oligomers during intoxication of mammalian cells. J. Biol. Chem. 26920607-20612. [PubMed] [Google Scholar]
- 29.Mogridge, J., K. Cunningham, and R. J. Collier. 2002. Stoichiometry of anthrax toxin complexes. Biochemistry 411079-1082. [DOI] [PubMed] [Google Scholar]
- 30.Mourez, M. 2004. Anthrax toxins. Rev. Physiol. Biochem. Pharmacol. 152135-164. [DOI] [PubMed] [Google Scholar]
- 31.Pamer, E., and P. Cresswell. 1998. Mechanisms of MHC class I-restricted antigen processing. Annu. Rev. Immunol. 16323-358. [DOI] [PubMed] [Google Scholar]
- 32.Schlecht, G., J. Loucka, H. Najar, P. Sebo, and C. Leclerc. 2004. Antigen targeting to CD11b allows efficient presentation of CD4+ and CD8+ T cell epitopes and in vivo Th1-polarized T cell priming. J. Immunol. 1736089-6097. [DOI] [PubMed] [Google Scholar]
- 33.Scobie, H. M., G. J. Rainey, K. A. Bradley, and J. A. Young. 2003. Human capillary morphogenesis protein 2 functions as an anthrax toxin receptor. Proc. Natl. Acad. Sci. USA 1005170-5174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seder, R. A., and R. Ahmed. 2003. Similarities and differences in CD4+ and CD8+ effector and memory T cell generation. Nat. Immunol. 4835-842. [DOI] [PubMed] [Google Scholar]
- 35.Sellman, B. R., M. Mourez, and R. J. Collier. 2001. Dominant-negative mutants of a toxin subunit: an approach to therapy of anthrax. Science 292695-697. [DOI] [PubMed] [Google Scholar]
- 36.Sellman, B. R., S. Nassi, and R. J. Collier. 2001. Point mutations in anthrax protective antigen that block translocation. J. Biol. Chem. 2768371-8376. [DOI] [PubMed] [Google Scholar]
- 37.Shaw, C. A., and M. N. Starnbach. 2006. Stimulation of CD8+ T cells following diphtheria toxin-mediated antigen delivery into dendritic cells. Infect. Immun. 741001-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Villadangos, J. A. 2001. Presentation of antigens by MHC class II molecules: getting the most out of them. Mol. Immunol. 38329-346. [DOI] [PubMed] [Google Scholar]
- 39.Wang, X., and T. Mosmann. 2001. In vivo priming of CD4 T cells that produce interleukin (IL)-2 but not IL-4 or interferon (IFN)-γ, and can subsequently differentiate into IL-4- or IFN-γ-secreting cells. J. Exp. Med. 1941069-1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wong, P., and E. G. Pamer. 2003. CD8 T cell responses to infectious pathogens. Annu. Rev. Immunol. 2129-70. [DOI] [PubMed] [Google Scholar]