Abstract
The development of safe and efficacious immunization systems to prevent brucellosis is needed to overcome the disadvantages of the currently licensed vaccine strains that restrict their use in humans. Alginate microspheres coated with a protein of the parasite Fasciola hepatica (vitelline protein B [VpB]) and containing live Brucella melitensis attenuated mutant vjbR::Tn5 (BMEII1116) were evaluated for vaccine efficacy and immunogenicity in mice. A single immunization dose in BALB/c mice with the encapsulated vjbR mutant improved protection against wild-type B. melitensis 16M challenge compared to the nonencapsulated vaccine strain (P < 0.05). The encapsulated mutant was also shown to induce a sustained elevation of Immunoglobulin G levels. Cytokine secretion from spleen cells of mice vaccinated with the encapsulated vjbR::Tn5 revealed elevated secretion of gamma interferon and interleukin-12, but no interleukin-4, suggesting an induction of a T helper 1 response reflecting the enhanced immunity associated with microencapsulation. Together, these results suggest that microencapsulation of live attenuated organisms offers the ability to increase the efficacy of vaccine candidates.
Brucella, an obligate intracellular bacterium, is the causative agent of brucellosis, a zoonosis of nearly worldwide distribution (8). Among the six different Brucella species, Brucella melitensis, B. suis, and B. abortus are pathogenic and virulent not only for sheep, goats, swine, and cattle, respectively, but also for humans. Despite the availability of live vaccine strains for cattle (S19 and RB51) and small ruminants (Rev-1), these vaccines have several drawbacks, including interference with diagnosis, resistance to antibiotics, and residual virulence, that prevent the use of these vaccines in humans (4, 6, 28). Numerous attempts to develop safe and more effective vaccines, including the use of killed organisms, cell extracts, or recombinant proteins, has had limited success (18, 22, 27, 28, 33).
In the absence of defined protective immunogens, the use of attenuated vaccine strains offers the best approach. As an alternative, we have investigated the ability to combine an attenuated live vaccine delivered in a controlled release vehicle. For this purpose, alginate, a naturally occurring biopolymer, offers advantages, including biocompatibility and relatively mild conditions required to produce an alginate matrix or particle (7). Extensive investigation has shown the efficacy of this release system when used to encapsulate protein agents such as insulin, erythropoietins, and chemokines (20, 25, 32). To further increase the efficacy of the capsular delivery, a novel recombinant form of the vitelline protein B (VpB) derived from the eggshell precursor of the parasite Fasciola hepatica was incorporated into the capsules (26). VpB possesses an unusual resistance to enzymatic and chemical breakdown that is expected to extend the time frame of erosion and release of the capsule content (34).
Ongoing research in our laboratory has identified B. melitensis genes required for virulence and survival via transposon mutagenesis (3, 16). Among these, vjbR (BMEII1116), encoding the luxR-like quorum-sensing-related transcriptional regulator, is required for adequate virB expression (10). Although virB expression is diminished in the vjbR mutant, it is not completely abrogated (T. A. Ficht et al., unpublished results). The vjbR mutants of B. melitensis are highly attenuated in mice and macrophages, making such mutants ideal vaccine candidates. Due to their attenuation and rapid clearance from the host, the utility of encapsulation of the vjbR mutant into alginate/VpB microcapsules was examined with the aim of producing enhanced immunization systems that are safe and more efficacious for human use.
In the present study, we demonstrate the efficacy of using controlled release systems with live attenuated B. melitensis vjbR::Tn5 mutant as a vaccine candidate against subsequent B. melitensis exposure. Vaccination with the encapsulated mutant induced a robust and sustained cellular and humoral response that correlated with higher levels of protection compared to the nonencapsulated vaccine. Furthermore, the protective efficacy of the vaccines correlated with a specific improvement in T helper 1 (Th1) response.
MATERIALS AND METHODS
Mice.
A total of 120 4- to 6-week-old female BALB/c mice were obtained from the Jackson Laboratory (Bar Harbor, ME) and acclimated for 2 weeks. All experimental procedures and animal care were performed in compliance with institutional animal care regulations.
Bacterial strains.
The bacterial strains used in these experiments include B. melitensis vjbR::Tn5 as the vaccine candidate and the B. melitensis virulent strain 16M. For assessment of bacterial incorporation inside the capsule, 16M transformed with the pBBR1mcs 6-y plasmid and expressing the reporter protein green fluorescent protein (GFP) was kindly provided by R. Martin Roop II. Bacteria were grown on tryptic soy agar (TSA) at 37°C with 5% (vol/vol) CO2. For vjbR::Tn5, the medium was supplemented with kanamycin (100 μg/ml). After 3 days of incubation, bacteria were harvested from the surface of plates into phosphate-buffered saline. The bacteria were pelleted, washed twice by resuspension in buffer containing morpholinepropanesulfonic acid (MOPS; 10 mM MOPS, 0.85% NaCl [pH 7.4]), and resuspended to a final concentration of 2 × 106 CFU/ml based upon optical density readings obtained using a Klett meter and a standardized curve. The actual viable counts were confirmed by serial dilution and plating of portions onto TSA plates with or without antibiotic.
Evaluation of B. melitensis vjbR::Tn5 in J774A.1 macrophages.
Murine macrophage-like J774.A1 (ATCC TIB-67) were used to assess vjbR::Tn5 mutant survival compared to the parental B. melitensis wild-type 16M. Macrophage survival assays were performed as previously described, with some modifications (24). Briefly, macrophages were cultured in Dulbecco modified Eagle medium with 10% (vol/vol) fetal bovine serum, 1 mM l-glutamine, and 1 mM nonessential amino acids. Monolayers of macrophages containing 2.5 × 105 cells per well were infected at a multiplicity of infection of 1:100 at 37°C with either vjbR::Tn5 or wild-type 16M. At 30 min postinfection, the cells were washed twice with medium without antibiotics and then incubated with 50 μg of gentamicin (Invitrogen)/ml for 30 min to kill any extracellular bacteria. At 1 and 48 h postinfection, macrophages were lysed with 0.05% (vol/vol) Tween 20, and the bacteria were collected. Brucella entry and survival was determined by performing serial dilutions and plating onto TSA plates with or without antibiotic. All assays were performed in triplicate and repeated at least three times.
Evaluation of B. melitensis vjbR::Tn5 attenuation in mice.
Female BALB/c mice were used to evaluate the survival of the vjbR::Tn5 mutant. Briefly, 6- to 8-week-old mice were intraperitoneally inoculated with a total of 2 × 106 CFU of either mutant or wild-type organism. Groups of five mice were euthanized via carbon dioxide asphyxiation at 1, 2, 3, and 4 weeks postinoculation. At each time point, spleens were collected, weighed, and homogenized in 1 ml of peptone saline. Serial dilutions were prepared, and 100-μl aliquots of the different dilutions were plated in duplicate onto TSA or TSA-kanamycin. Levels of infection were expressed as the mean ± the standard error of the mean (SEM) of the individual log CFU/spleen.
Preparation of B. melitensis antigen-loaded microspheres.
Alginate beads were prepared as previously described with some modifications(1). Briefly, 6 × 106 CFU of the live B. melitensis mutant vjbR::Tn5 were resuspended in 1 ml of MOPS buffer (10 mM MOPS, 0.85% NaCl [pH 7.4]) and mixed with 5 ml of alginate solution (1.5% sodium alginate, 10 mM MOPS, 0.85% NaCl [pH 7.3]). Spheres were obtained by extruding the suspension through a 200-μm nozzle into a 100 mM calcium chloride solution and stirred for 15 min by using an Inotech Encapsulator I-50 (Inotech Biosystems International, Rockville, MD). After extrusion of the bacterium-alginate mixture into the CaCl2, the capsules were washed twice with MOPS for 5 min and further cross-linked with 0.05% poly-l-lysine (molecular weight. 22,000; Sigma) for 10 min. After two successive washes, the beads were stirred in a solution of 0.03% (wt/vol) alginate for 5 min to apply a final outer shell and washed twice with MOPS before storage at 4°C.
In a second formulation, VpB was added as a component of the alginate core (vjbR::Tn5/VpB/core) by the addition of 1 mg of VpB to the bacterium-alginate suspension described above. Extrusion and capsule formation used the same preparation conditions.
VpB was alternatively added to the shell of the capsule (vjbR::Tn5/VpB/shell) as a cross-linking agent by the addition of VpB in an equimolar ratio of poly-l-lysine/VpB as the third capsule formulation used.
Bacterial viability.
To determine the bacterial content per milliliter of alginate particles, 1 ml of capsules was removed from the encapsulator prior to permanent cross-linking with poly-l-lysine or cross-linking with VpB plus poly-l-lysine. The capsules were allowed to settle and washed twice with MOPS buffer, and particles were dissolved by using 1 ml of depolymerization solution (50 mM sodium citrate, 0.45% NaCl, 10 mM MOPS [pH 7.2]) with stirring for 10 min. Bacterial numbers (in CFU/ml) of capsules were determined by plating onto TSA plates.
Characterization of microspheres.
The bacterial presence inside the capsule, the sphere morphology, and the size were assessed via fluorescence microscopy (Nikon, TMS). Three size determinations were made for each formulation, and the mean values were reported.
In vitro bacterial release from the capsules.
Bacterial release from the capsules was assessed by using 1 ml of capsules containing 109 CFU resuspended in 10 ml of peptone saline (pH 7.2). The release study was conducted for 37 days. At 24-h intervals, 1 ml of peptone saline was removed and plated onto TSA to determine bacterial release from the capsule. The buffer was replaced completely after the withdrawal of each aliquot. Nonencapsulated bacteria were used as a control and subjected to the same procedure. Release profiles were expressed in terms of daily release and plotted versus time. All measurements were performed in triplicate, and the experiment was repeated three times.
Kinetics of bacterial clearance from mice vaccinated with encapsulated vjbR::Tn5.
To further understand the kinetics of bacterial release from alginate microspheres in vivo, BALB/c mice were vaccinated with either encapsulated or nonencapsulated vjbR::Tn5 strain at a dose of 105 CFU. Mice were euthanized at 1, 2, 3, 4, 5, 6, and 7 weeks postinoculation, and the spleens were harvested, weighed, and homogenized in 1 ml of peptone saline. Bacterial suspensions were serially diluted, and 200 μl of the homogenate was plated onto TSA-kanamycin plates. In some instances the whole homogenate was plated to increase the limit of detection to one organism. Bacterial release from the beads was indirectly measured by determination of the CFU encountered in the spleen.
Immunization of mice.
Sixty 6- to 8-week-old female BALB/c mice were randomly divided into groups of 10 for intraperitoneal vaccination. Animals were given a single dose of microcapsules containing 105 CFU of either (i) encapsulated B. melitensis mutant vjbR::Tn5 in alginate (vjbR::Tn5/alginate), (ii) encapsulated vjbR::Tn5 mutant in alginate with VpB inside the capsule (vjbR::Tn5/VpB/core), or (iii) encapsulated vjbR::Tn5 mutant in alginate with VpB in the shell of the sphere (vjbR::Tn5/VpB/shell). Control groups received 105 CFU of either (i) nonencapsulated vjbR::Tn5 mutant, (ii) empty capsules (no bacteria entrapped), or (iii) 200 μl of MOPS buffer.
Evaluation of Brucella-specific antibody.
To determine anti-Brucella-specific antibody in sera from inoculated mice, 100 μl of blood was taken from each mouse 0, 2, 4, 8, 10, 12, 14, 18, 24, and 30 weeks postvaccination and used for immunoglobulin G (IgG) determination by enzyme-linked immunosorbent assay (ELISA). Heat-killed and sonicated B. melitensis whole-cell antigen was used to coat 96-well plates (Nunc-Immuno plates) at a concentration of 25 μg of total protein/well. After overnight incubation at 4°C, plates were washed, blocked with 0.5 ml of blocking buffer (0.25% [wt/vol] bovine serum albumin), and then incubated with mouse sera diluted 1:100 in the same blocking buffer for 1 h at room temperature. After extensive washing to remove unbound antibody, rabbit anti-mouse IgG-horseradish peroxidase conjugate (KPL) was added at a dilution of 1:1,000, and incubation continued for an additional hour. After this incubation the plates were washed again, and horseradish peroxidase substrate was added, followed by incubation for 18 min. The reaction was stopped by the addition of 50 μl of 0.5 M NaOH, and the absorbance was measured at 450 nm (A450). All assays were performed in triplicate and repeated at least three times. For IgG isotype and recall determination, serum samples at the day of challenge and 3 days postchallenge were diluted (1:100 to 1:100,000). Endpoint titers were expressed as the maximum dilution of sample above three standard deviations from the control sera. The results are represented as the mean of triplicate wells for each sample.
Determination of splenocyte cytokine production.
At selected times postvaccination, individual spleens from five animals per group were extracted, and single-cell suspensions were obtained by homogenizing the spleen using glass tissue grinders. After lysis of erythrocytes using red blood cell lysing buffer (8.3 g of NH4Cl in 0.01 M Tris-HCl [pH 7.5]), the cell suspension was washed in complete RPMI 1640 medium containing 10% (vol/vol) fetal bovine serum and 50 μg of gentamicin/ml. The cell number was adjusted, and cells were added to 24-well plates at a concentration of 2.5 × 105 cells/well and cultured following the addition of 25 μg of B. melitensis lysate/well prepared as described above. Cells in control wells received medium alone. At 72 h after incubation at 37°C in 5% (vol/vol) CO2, culture supernatants were collected and stored at −20°C. Interleukin 4 (IL-4), IL-12p70, and gamma interferon (IFN-γ) cytokines were determined in triplicate by using a Bioplex array system (Bio-Rad) according to the manufacturer's instructions. For each cytokine, eight standards ranging from 2 to 32,000 pg/ml were quantitated.
Determination of cytokine production in vivo.
At 0, 10, and 30 weeks postvaccination, animals were bled and serum was obtained from each individual mouse for cytokine determination. Quantification of IFN-γ and IL-12p70 was determined by ELISA (Ebioscience) according to the manufacturer's instructions. All samples were performed in triplicate, and the assay was repeated three times. For each cytokine, standards ranging from 0.2 to 1,000 pg/ml were quantitated. Background levels obtained for t = 0 were subtracted from the samples. The differences between the encapsulated and nonencapsulated formulations at each time point were determined by analysis of variance (ANOVA). The results are represented as the mean picograms of each cytokine/ml ± the standard deviation.
Efficacy of vaccination.
At selected times postvaccination, mice (n = five animals per group) were challenged interperitoneally with 105 CFU of B. melitensis wild-type 16M/mouse. At 1 week postchallenge, mice were euthanized by CO2 asphyxiation, and the spleens were removed, weighed, and homogenized in 1 ml of peptone saline. Serial dilutions were prepared, and 100-μl portions were plated onto TSA plates. In some instances, 200 to 1,000 μl of spleen homogenate was plated to determine organism recovery. To differentiate between the vaccine candidate and the challenge strain, each dilution was also plated on TSA with kanamycin to identify any residual kanamycin-resistant vaccine strain present. Levels of infection were expressed as the mean ± the SEM of individual log10 CFU/spleen. The efficacy of the vaccine compared to naive animals was determined by subtracting the mean CFU/spleen recovered from mice vaccinated with the nonencapsulated or encapsulated (vjbR::Tn5/alginate, vjbR::Tn5/VpB/core, or vjbR::Tn5/VpB/shell) vaccine from the mean CFU/spleen recovered from naive nonvaccinated but challenged mice. The efficacy of the encapsulated vaccine compared to the nonencapsulated vaccine was determined by subtracting the mean CFU/spleen recovered from mice vaccinated with the capsules from the mean CFU/spleen recovered from mice immunized with the nonencapsulated vaccine.
Statistical procedures.
Macrophage infection and survival were expressed as the mean log CFU ± the standard deviation for each group. The intensity of infection (bacterial clearance and efficacy of vaccine) at each time point was expressed as the mean log CFU ± the SEM for each group. Cytokine production in vitro and in vivo was expressed as mean cytokine concentration ± the standard deviation for each group of five mice. Bacterial release from the capsules was expressed in terms of daily release and plotted versus time. Efficacy studies compared mice vaccinated with the encapsulated organism and subsequently challenged mice to mice receiving the nonencapsulated mutant as a vaccine control that were challenged with wild-type organism. The significance of differences between vaccinates were analyzed by ANOVA followed by Tukey's honestly significant difference post test comparing all groups to one another. For ANOVA, P values of <0.05 were considered statistically significant.
RESULTS
B. melitensis vjbR::Tn5 mutant is highly attenuated for survival in macrophages and in mice.
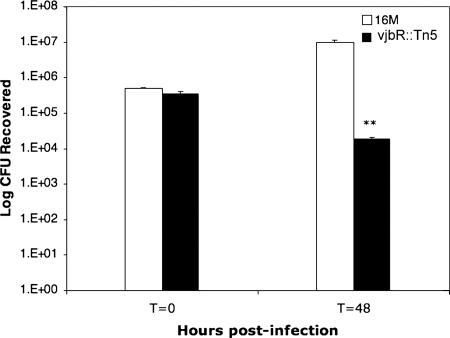
To assess the vjbR::Tn5 attenuation, J774A.1 macrophages were infected with the mutant and compared to the wild-type B. melitensis 16M. Using a multiplicity of infection of 100, the ability of the bacteria to enter and replicate within macrophages was evaluated. Shortly after infection (t = 0 h) there was no difference (P > 0.05) between the wild type and the mutant in the number of bacteria (three to four per cell) infecting the macrophage (Fig. 1). In contrast, by 48 h postinfection there was a 2.5-log difference (P < 0.005) in the number of organisms surviving inside the macrophage (100 per cell for 16M and less than 1 per cell for the vjbR::Tn5). These results demonstrate that the vjbR::Tn5 mutant has a severely limited capacity to replicate within J774A.1 macrophages.
FIG. 1.
Survival of the B. melitensis vjbR::Tn5 mutant in J774A.1 macrophages. Wild-type strain 16M and the B. melitensis mutant vjbR::Tn5 were used to infect J774A.1 macrophages at a multiplicity of infection of 1:100. After 30 min of incubation, followed by 1 h of treatment with gentamicin, infected macrophages were further incubated for 0 or 48 h. Treated cells were lysed, serially diluted, and plated on TSA or TSA-kanamycin plates for CFU determination. The values are the means of three independent experiments ± the standard deviation. Differences in macrophage colonization by wild-type 16M and the vjbR::Tn5 mutant were analyzed by Student's t test (**, P < 0.005).
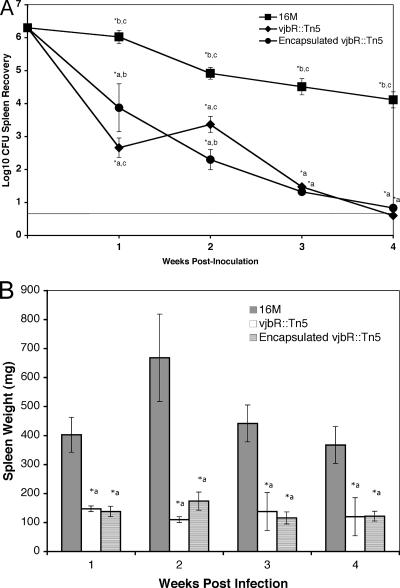
To evaluate survival in vivo, BALB/c mice were inoculated intraperitoneally with 2 × 106 CFU of B. melitensis vjbR::Tn5 or the 16M parental wild-type strain. Compared to the wild-type strain 16M, the vjbR::Tn5 mutant was significantly reduced by 1.5 to 3.6 logs at all of the time points chosen. There appears to be a brief period between weeks 1 (P < 0.001) and 2 (P > 0.05) during which the organism replicates and the numbers of B. melitensis vjbR::Tn5 in the spleen increase, but by 3 weeks postinoculation the number of organisms in the spleen exhibits a drastic decline (P < 0.001) and drops below the level of detection by 4 weeks postinfection (P < 0.001) (Fig. 2A). In addition, disruption of vjbR significantly reduced (P < 0.001) splenomegaly at all time points, a finding consistent with the reduction in colonization of the spleen (Fig. 2B).
FIG. 2.
Kinetics of clearance and spleen weights in BALB/c mice during B. melitensis vjbR::Tn5 infection. Each BALB/c mouse (n = five animals/time point) was infected with 2 × 106 CFU of wild-type 16M, the vjbR::Tn5 mutant or encapsulated vjb::Tn5. (A) At 1, 2, 3, and 4 weeks postinfection, mice were euthanized, and the spleens were assessed for bacterial colonization. The solid line represents the limit of detection, which is ≥5 CFU. (B) Spleens from the same mice and at the same time points were weighed to determine the degree of inflammation conferred by the mutant. For both sets of data, values are the means + SEM. Differences in colonization or spleen weights were compared by ANOVA followed by Tukey's honestly significant difference posttest to compare all groups to each other. *, P < 0.05, with a, b, and c indicating the M16, nonencapsulated vjb::Tn5 mutant, and encapsulated vjb::Tn5 mutant groups, respectively.
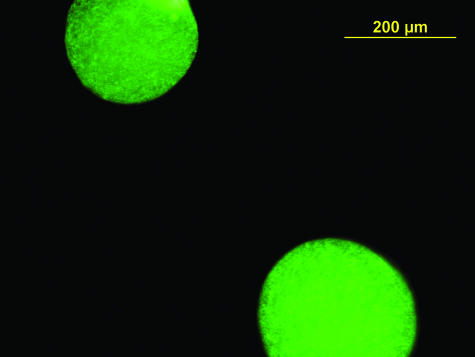
Evaluation of capsule characteristics.
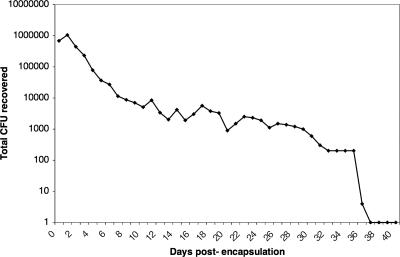
Three different types of capsules were prepared by using the same basic alginate formulation. Variations in the formulations included the addition of VpB to the core or to the shell of the capsule. In general, the results demonstrate that, despite the differences in formulations, all of the capsules prepared appeared spherical and uniform, with a mean diameter of 300 μm. To characterize the bacterial entrapment inside the capsule, B. melitensis 16M transformed with a GFP-expressing plasmid was encapsulated. The results revealed the presence of bacteria inside the capsule (Fig. 3). Furthermore, bacterial viability after encapsulation exceeded 95%, as demonstrated by recovery of the organism after dissolution of the capsules. Bacterial release from the microspheres was monitored in vitro for 40 days. The results revealed an initial bacterial burst that occurred in the first 2 days, followed by a sustained release that lasted 36 days (Fig. 4).
FIG. 3.
Fluorescence microscopy image of alginate microspheres loaded with wild-type 16M. B. melitensis wild-type 16M was transformed with a GFP-expressing plasmid and encapsulated into alginate microspheres. The bacterial presence inside the capsule and sphere morphology was assessed via fluorescence microscopy.
FIG. 4.
Kinetics of bacterial release in vitro from alginate microcapsules. Alginate microbeads were prepared containing 109 CFU of vjbR::Tn5 mutant/ml, and 1 ml of capsules was resuspended in peptone saline. Every day, the buffer was completely removed and new peptone saline was added. Aliquots (100 μl) of the buffer were serially diluted and plated onto TSA-kanamycin plates to determine the number of bacteria released into the buffer. The solid line represents the limit of detection, which is ≥5 CFU.
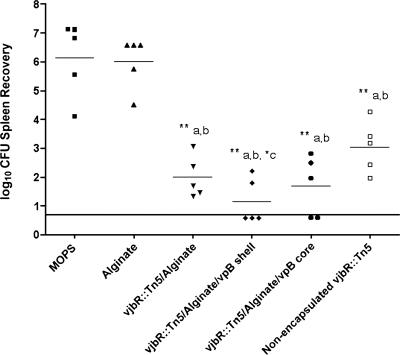
Encapsulated B. melitensis vjbR::Tn5 protects against 16M wild-type challenge.
In order to determine the effect of encapsulation on immunization, the level of protection provided by equal numbers of encapsulated and nonencapsulated B. melitensis vjbR::Tn5 was evaluated against wild-type challenge at 31 weeks postvaccination. At this time point, nonspecific activation due to innate immune response to persistent infection or delayed release of the encapsulated organism had passed based upon the decrease observed in humoral immunity and the absence of recovery of the vaccine strain (Fig. 5). At 32 weeks postvaccination (1 week after challenge), all mice, including the nonencapsulated group, demonstrated a statistically significant decrease in bacterial load in the spleen relative to naive mice, with a 3.14-log reduction (P < 0.05) for nonencapsulated mutant, a 4.14-log reduction (P < 0.005) for BM vjbR::Tn5 mutant in alginate, a 4.45-log reduction (P < 0.001) for BM vjbR::Tn5 mutant in VpB core, and a 4.98-log reduction (P < 0.001) for BM vjbR::Tn5 mutant in VpB shell compared to naive mice. All groups of mice receiving encapsulated vaccination exhibited a statistically significant degree of protection against infection compared to the nonencapsulated mutant (P < 0.001). Among the three encapsulated vaccines, the BM vjbR::Tn5 mutant with a VpB shell provided the best level of protection, increasing the vaccine efficacy by 1.84 logs (P < 0.05) compared to the nonencapsulated vaccine. Moreover, the challenge organism was undetectable in 60% of the BM vjbR::Tn5 mice (Fig. 6).
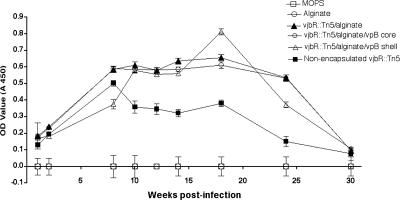
FIG. 5.
IgG anti-Brucella antibodies in serum from mice immunized with vjbR::Tn5 mutant. BALB/c mice (n = 10) were inoculated intraperitoneally with 105 CFU of either nonencapsulated B. melitensis vjbR::Tn5 mutant, encapsulated B. melitensis (vjbR::Tn5/alginate), encapsulated B. melitensis vjbR::Tn5 with VpB in the core (vjbR::Tn5/alginate/VpB/core), or encapsulated B. melitensis vjbR::Tn5 mutant with VpB in the shell (vjbR::Tn5/alginate/VpB/shell). Control groups received empty capsules or MOPS. At 0, 2, 4, 8, 10, 12, 14, 18, 24, and 30 weeks postvaccination, serum samples were collected and used at a 1:1,000 dilution for IgG determination by ELISA. The results are shown as means ± the standard deviations of the absorbance at A450.
FIG. 6.
Immunization efficacy of B. melitensis vjbR::Tn5 vaccine formulations. BALB/c mice were immunized intraperitoneally with 105 CFU of either nonencapsulated B. melitensis vjbR::Tn5 mutant, encapsulated B. melitensis vjbR::Tn5/alginate, encapsulated B. melitensis vjbR::Tn5 mutant with VpB in the core (vjbR::Tn5/alginate/VpB core), or encapsulated B. melitensis vjbR::Tn5 mutant with VpB in the shell (vjbR::Tn5/alginate/VpB shell). Control groups received empty capsules or MOPS. After 31 weeks, mice were challenged intraperitoneally with 105 CFU of wild-type 16M. At 1 week postchallenge, mice were euthanized, spleens were harvested, and the bacterial load was determined. Values are reported as the log10 recovery of 16M from spleens, with individual mice in each treatment group represented. The solid line represents the limit of detection, which is ≥5 CFU. Differences in colonization between nonencapsulated and encapsulated groups were determined by ANOVA followed by Tukey's honestly significant difference posttest to compare all groups to each other. *, P < 0.05, and **, P < 0.005, with lowercase letters indicating the groups as follows: a, MOPS group; b, alginate group; c, vjb::Tn5/alginate group, d, vjb::Tn5/alginate/VpB shell group; e, vjb::Tn5/alginate/VpB core group; and f, nonencapsulated vjb::Tn5 group.
Encapsulated BM vjbR::Tn5 elicits vigorous humoral and cytokine responses.
Serum collected at 0, 1, 2, 8, 10, 12, 14, 18, 24, and 30 weeks postvaccination was assayed for the presence of Brucella-specific antibodies by ELISA. Immunization with BM vjbR::Tn5 mutant elicited a IgG response that was clearly detectable at 2 weeks postvaccination for either encapsulated or nonencapsulated vaccines (Fig. 5). In mice vaccinated with the nonencapsulated BM vjbR::Tn5 vaccine, IgG levels peaked at 8 weeks postimmunization, whereas in mice immunized with BM vjbR::Tn5 with VpB in the shell, the IgG levels increased steadily and reached a maximum by 18 weeks postimmunization. In this case, an induction of higher and sustained antibody levels correlated with enhanced protection for both BM vjbR::Tn5 in alginate and vjbR::Tn5 in VpB shell formulations.
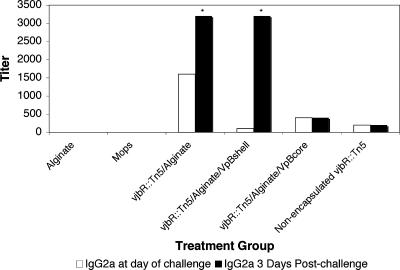
To determine the magnitude of the memory response induced by the different vaccine formulations, mice were challenged at week 31 postvaccination, and the IgG recall response was evaluated 3 days postchallenge. Animals immunized with BM vjbR::Tn5/alginate and vjbR::Tn5/VpB/shell underwent a rapid antibody recall (Fig. 7). The recall responses were stronger for the IgG2a isotype, with a fivefold increase in animals that received vjbR::Tn5/VpB/shell and a threefold increase in vjbR::Tn5/alginate vaccinees. Only a modest increase in IgG1 (twofold) was observed in the vjbR::Tn5/VpB/shell-immunized mice (data not shown). In contrast, there was a minimal recall response in mice vaccinated with the nonencapsulated mutant. There were no increases in antibody titers in naive but challenged animals, clearly indicating that the responses observed here were recall responses rather than an initial priming.
FIG. 7.
IgG2a recall response of B. melitensis vjbR::Tn5 vaccine formulations. BALB/c mice were immunized intraperitoneally with 105 CFU of either nonencapsulated B. melitensis vjbR::Tn5 mutant, encapsulated B. melitensis vjbR::Tn5/alginate mutant, encapsulated B. melitensis vjbR::Tn5 mutant with VpB in the core (vjbR::Tn5/alginate/VpB/core), or encapsulated B. melitensis vjbR::Tn5 mutant with VpB in the shell (vjbR::Tn5/alginate/VpB/shell). Control groups received empty capsules or MOPS. After 31 weeks, mice were challenged intraperitoneally with 105 CFU wild-type 16M. At 3 days postchallenge mice were bled, and IgG2a titers were determined by ELISA. Differences in responses between the nonencapsulated and the encapsulated groups were determined by Student's t test, comparing the changes in antibody titer on the day of challenge to that at 3 days postchallenge for each individual treatment group (*, P < 0.05).
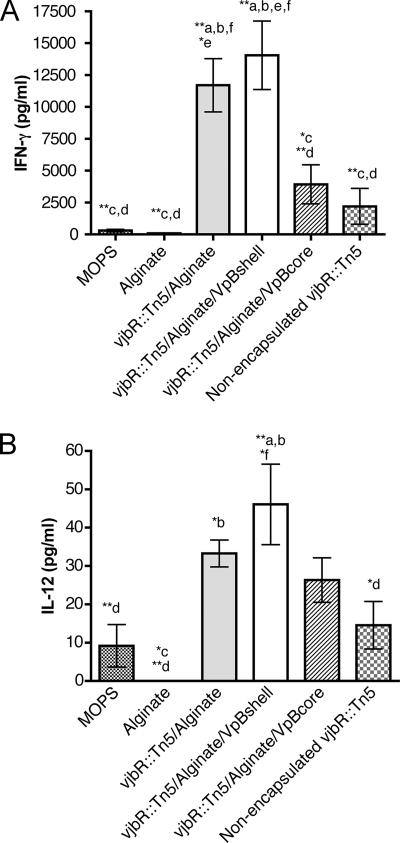
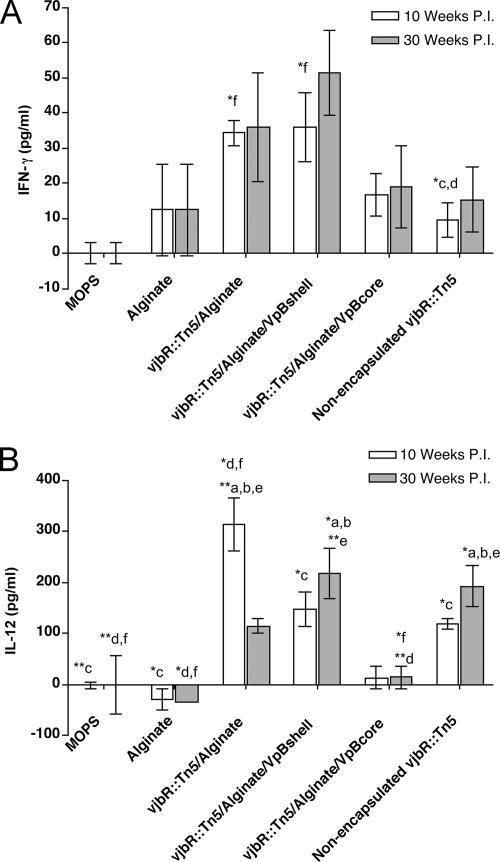
To obtain additional information on the type of immune response induced by the different BM vjbR::Tn5 capsule formulations at the time of bacterial challenge, the cellular immune response was characterized based on the cytokine secretion in culture supernatants of spleen cells from immunized mice. All three capsule formulations stimulated elevated levels of IFN-γ (P < 0.005) and IL-12p70 (P < 0.05) (Fig. 8) compared to the nonencapsulated group. All cytokine levels were statistically significant compared to nonvaccinated animals (P < 0.005). In general, induction of higher Th1 cytokine levels correlated with the elevated protection exhibited in the encapsulated vaccine groups. Spleen cells from all immunized mice failed to produce IL-4 when stimulated with antigen (data not shown). No difference in IL-4 responses were detected between the vaccinated and nonvaccinated animals or between mice immunized with encapsulated and nonencapsulated formulations. Empty capsules failed to elicit the production of any of the cytokines measured. The proinflammatory cytokine profile observed after in vitro splenocyte stimulation correlated with the in vivo cytokine responses of IFN-γ and IL-12, whose levels were significantly (P < 0.05, P < 0.005) higher in animals vaccinated with encapsulated vaccines (Fig. 9).
FIG. 8.
Production of cytokines in stimulated spleen cells from vjbR::Tn5-vaccinated BALB/c mice. Mice were vaccinated with 105 CFU of either nonencapsulated B. melitensis vjbR::Tn5 mutant, encapsulated B. melitensis vjbR::Tn5/alginate mutant, encapsulated B. melitensis vjbR::Tn5 mutant with VpB in the core (vjbR::Tn5/alginate/VpBcore), or encapsulated B. melitensis vjbR::Tn5 mutant with VpB in the shell (vjbR::Tn5/alginate/VpBshell). Control groups received empty capsules or MOPS. At 31 weeks postvaccination, mice were euthanized, and splenocytes were harvested and stimulated with heat-inactivated B. melitensis 16M or medium alone as a control. IFN-γ (A) and IL-12p70 (B) production (pg/ml) was detected after 72 h of stimulation by using a multiplex suspension array system (Bioplex). Cytokine production was expressed as the mean cytokine concentration ± SEM for each group of mice. Differences in colonization between the nonencapsulated and encapsulated groups were determined by ANOVA followed by Tukey's honestly significant difference posttest comparing all groups to each other. *, P < 0.05, and **, P < 0.01, with lowercase letters indicating the groups as follows: a, MOPS group; b, alginate group; c, vjb::Tn5/alginate group, d, vjb::Tn5/alginate/VpB shell group; e, vjb::Tn5/alginate/VpB core group; and f, nonencapsulated vjb::Tn5 group.
FIG. 9.
Cytokine production in the sera of BALB/c mice immunized with the vjbR::Tn5 mutant. Mice were vaccinated with 105 CFU of either nonencapsulated B. melitensis vjbR::Tn5 mutant, encapsulated B. melitensis vjbR::Tn5/alginate mutant, encapsulated B. melitensis vjbR::Tn5 mutant with VpB in the core (vjbR::Tn5/alginate/VpBcore), or encapsulated B. melitensis vjbR::Tn5 mutant with VpB in the shell (vjbR::Tn5/alginate/VpBshell). Control groups received empty capsules or MOPS. Mice were bled at 0, 10, and 30 weeks postvaccination. IFN-γ (A) or IL-12 (B) determination from the serum was performed by ELISA. The results are represented as the mean cytokine concentration ± SEM for each group of mice. Differences in colonization between the nonencapsulated and encapsulated groups were determined by ANOVA followed by Tukey's honestly significant difference posttest comparing all groups to each other. *, P < 0.05, and **, P < 0.01, with lowercase letters indicating the groups as follows: a, MOPS group; b, alginate group; c, vjb::Tn5/alginate group, d, vjb::Tn5/ alginate/VpB shell group; e, vjb::Tn5/alginate/VpB core group; and f, nonencapsulated vjb::Tn5 group.
DISCUSSION
Efficacious immunization systems to protect against brucellosis are needed to overcome the disadvantages of the currently available vaccines with regard to efficacy in a wide variety of hosts (28). Second only to immune protection, safety is of critical importance for ideal live Brucella vaccines. The absence of virulence in the target host and in humans will help to avoid virulence-related sequelae. Increasing knowledge of virulence factors and Brucella pathogenesis mechanisms provide us with the tools to construct new attenuated strains. Previous studies in our laboratory using transposon-based mutagenesis strategies have identified genes related to survival and virulence (16, 36). Among the genes identified, vjbR::Tn5 mutants were evaluated for survival in macrophages and the mouse model to confirm attenuation and immune potential. As shown in the present study, BM vjbR::Tn5 was defective for survival within macrophages and rapidly cleared from the spleen in BALB/c mice. In mice, the mutant was significantly reduced in number by 1 week postinfection and was completely cleared by 4 weeks. In contrast, 16M persists in the mouse spleen for more than 16 weeks (17). vjbR::Tn5 safety was further revealed by the absence of splenomegaly in inoculated mice. Even at 2 weeks, when the bacterial load in the spleen was high, the mean spleen weights in BM vjbR::Tn5-inoculated mice was 110 mg versus 653 mg for 16M (Fig. 2B). The currently available vaccine strains S19 and Rev-1 induce splenomegaly in mice, totally undesirable side effects for human vaccination (29). Differences in survival and inflammatory response exhibited by vjbR::Tn5 provide an opportunity to evaluate its use as an improved vaccine candidate for possible human use.
Recent data suggest that the manner in which antigen reaches the lymph organs and how it is delivered to the antigen-presenting cells is fundamental in the induction of an optimal immune response (11). There is experimental evidence to support the observation that microencapsulation serves to modify the uptake and processing of the antigen (11, 30). Based on these observations, we developed a controlled release strategy using highly attenuated mutants. Alginate-VpB microspheres permit a constant or pulsed release of encapsulated organism, simulating continuous exposure, that might potentiate the vaccine efficacy. Release from alginate matrices generally occurs by diffusion through pores of the capsule or by erosion of the polymer network (35). In the case of standard bacterial entrapment methods used for Mycobacterium bovis BCG or bifidobacteria, cells escape through erosion rather than diffusion due to bacterial size and surface charge (2, 9). VpB was added to the formulation in an attempt to extend the time frame over which the capsule dissolution occurs, due to the characteristic resistance of the protein to enzymatic breakdown (34).
During microsphere formulation microorganisms were exposed to relatively mild conditions that did not cause significant bacterial death; this approach permits the development of live encapsulated vaccines in contrast to previously published encapsulation procedures in which the viability of the bacteria is compromised due to the extreme conditions, including ultrasound homogenization, direct exposure to organic solvents, and shear stress (19). The use of a GFP plasmid-transformed organism helped to confirm bacterial entrapment inside the capsules and demonstrated uniform spherical capsule formation. This morphology was maintained even with the inclusion of VpB, which enhances capsule stability via cross-linking due to its high lysine and arginine content when substituted for poly-l-lysine (26, 34).
Protection studies against wild-type challenge with both nonencapsulated and encapsulated organisms protected mice significantly, but the vaccine efficacy was increased substantially when the mutant was delivered in an encapsulated form. The addition of VpB in the core or shell of the capsule further enhanced protection. VpB is a protease-resistant protein from Fasciola hepatica that retards capsule erosion and extends the release profile. Encapsulation and incorporation of VpB in vaccine formulations is one approach to improving immunization efficacy for Brucella and other organisms.
The degree of protection conferred by the different vaccine formulations was evaluated via antibody response. Immunization with B. melitensis vjbR::Tn5 mutant in microcapsules induced prolonged elevation of total IgG levels compared to the nonencapsulated vaccine, as predicted for our controlled release format. Vaccination efficacy relies on the effective generation and maintenance of immunological memory. After challenge, encapsulated vjbR::Tn5/alginate/VpB/shell and vjbR::Tn5/alginate induced anti-Brucella IgG levels within 3 days; such a quick response can be attributed to the generation of an immunological memory response by the vaccine. Isotype analysis revealed a correlation between elevated IgG2a antibody titers with higher IL-12 responses, suggesting the induction of a Th1 cell-mediated response. These results strongly suggest the induction of a protective immune response against intracellular pathogens, enhanced by encapsulation and controlled release. Future experiments are designed to distinguish between increased antibody avidity and recognition of additional antigenic epitopes.
Published reports have shown that spleen cells from mice previously inoculated with live vaccines induced a Th1 type response to Brucella antigens in vitro, while splenocytes from mice immunized with killed vaccines induced Th2 responses (37). Moreover, it has been clearly established that IFN-γ is an important component of the Th1 response, activating macrophages for increased microbial killing (5, 15, 23). Studies performed with highly attenuated Brucella mutants indicate that both nonencapsulated and encapsulated vaccine induced higher IFN-γ levels than were observed in naive mice; however, encapsulation increased IFN-γ levels threefold over noncapsulated, suggesting a strong potentiation of the protective immune response induced through controlled release. This is consistent with in vitro results indicating continuous release of the organism for up to 35 days (Fig. 4), suggesting continuous boosting of the host immune system with antigen. In addition, higher cytokine concentrations coincided with the increased levels of protection generated by encapsulation. These data were corroborated by cytokine analysis of serum samples.
Although IFN-γ is critical for activating macrophages, other cytokines also play an important role in controlling Brucella. IL-12, a Th1-type cytokine mainly produced by macrophages, promotes IFN-γ production by T cells that induce murine B cells to switch to an IgG2a isotype (13). It also induces differentiation of CD4 Th1 cells (31). In this vaccination trial, IL-12 was also produced in significant levels compared to naive mice. Two of the three groups of animals that received microcapsules (vjbR::Tn5/alginate and vjbR::Tn5/alginate/VpB/shell) produced statistically significant levels compared to the nonencapsulated vaccine, suggesting that IL-12 plays an important role. One alternative may be that elevated IL-12 levels influence the development of antibody-mediated protective immunity, contributing to the clearance of the infection (12, 13, 21). Isotype analysis confirmed the correlation between elevated IgG2a antibody titers with the higher IL-12 responses (14).
It is important to mention that the microcapsules alone are insufficient to provoke the secretion of cytokines in cell culture supernatants. Furthermore, statistically significant concentrations of any cytokine were not detected in mice vaccinated with empty capsules, suggesting that the booster effect generated by the three capsule formulations was due to a continuous presentation of antigen. Experiments in progress are designed to further characterize the basis for this response.
In the present study, mice were vaccinated with a single dose of an attenuated Brucella mutant for 31 weeks. Previous studies have not analyzed vaccine candidate performance at such late time points. We chose the 6-month time point to rule out the action of the innate immunity due to the presence of the organism (because of the sustained release of the mutant from the capsule) to better asses the quality of the memory response generated by the different vaccine formulations delivered as a single dose. No vaccine strain was detectable at the time of challenge.
In summary, our findings suggest that encapsulation of live Brucella provides enhancement of vaccine efficacy. Adequate priming of the immune system is of extreme importance in determining the quality of a memory response. We were able to achieve this by encapsulation of the organism in a single dose, which is ideal for patient compliance. The vjbR::Tn5 mutant is a suitable vaccine candidate that warrants further investigation based upon its reduced virulence in macrophages and BALB/c mice and its ability to generate protection in the mouse model. We were able to demonstrate a specific Th1 response that did improve when the vaccine was given using a controlled release vehicle. Further studies are planned to generate a deletion mutant to avoid the use of vaccine strains with antibiotic resistance genes and to rule out the possibility of reversion to virulence. Experiments under way are designed to elucidate the role of capsules in antigen presentation.
Acknowledgments
This study was supported by the Western Regional Center for Excellence grant IU54AI 057156.
Editor: V. J. DiRita
Footnotes
Published ahead of print on 24 March 2008.
REFERENCES
- 1.Abraham, S. M., R. F. Vieth, and D. J. Burgess. 1996. Novel technology for the preparation of sterile alginate-poly-l-lysine microcapsules in a bioreactor. Pharm. Dev. Technol. 163-68. [DOI] [PubMed] [Google Scholar]
- 2.Aldwell, F. E., M. A. Baird, C. E. Fitzpatrick, A. D. McLellan, M. L. Cross, M. R. Lambeth, and G. S. Buchan. 2005. Oral vaccination of mice with lipid-encapsulated Mycobacterium bovis BCG: anatomical sites of bacterial replication and immune activity. Immunol. Cell Biol. 83549-553. [DOI] [PubMed] [Google Scholar]
- 3.Allen, C. A., L. G. Adams, and T. A. Ficht. 1998. Transposon-derived Brucella abortus rough mutants are attenuated and exhibit reduced intracellular survival. Infect. Immun. 661008-1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ashford, D. A., J. di Pietra, J. Lingappa, C. Woods, H. Noll, B. Neville, R. Weyant, S. L. Bragg, R. A. Spiegel, J. Tappero, and B. A. Perkins. 2004. Adverse events in humans associated with accidental exposure to the livestock brucellosis vaccine RB51. Vaccine 223435-3439. [DOI] [PubMed] [Google Scholar]
- 5.Baldwin, C. L., and M. Parent. 2002. Fundamentals of host immune response against Brucella abortus: what the mouse model has revealed about control of infection. Vet. Microbiol. 90367-382. [DOI] [PubMed] [Google Scholar]
- 6.Berkelman, R. L. 2003. Human illness associated with use of veterinary vaccines. Clin. Infect. Dis. 37407-414. [DOI] [PubMed] [Google Scholar]
- 7.Blandino, A., M. Macias, and D. Cantero. 1999. Formation of calcium alginate gel capsules: influence of sodium alginate and CaCl2 concentration on gelation kinetics. J. Biosci. Bioeng. 88686-689. [DOI] [PubMed] [Google Scholar]
- 8.Boschiroli, M. L., V. Foulongne, and D. O'Callaghan. 2001. Brucellosis: a worldwide zoonosis. Curr. Opin. Microbiol. 458-64. [DOI] [PubMed] [Google Scholar]
- 9.Cui, J. H., J. S. Goh, P. H. Kim, S. H. Choi, and B. J. Lee. 2000. Survival and stability of bifidobacteria loaded in alginate poly-l-lysine microparticles. Int. J. Pharm. 21051-59. [DOI] [PubMed] [Google Scholar]
- 10.Delrue, R. M., C. Deschamps, S. Leonard, C. Nijskens, I. Danese, J. M. Schaus, S. Bonnot, J. Ferooz, A. Tibor, X. De Bolle, and J. J. Letesson. 2005. A quorum-sensing regulator controls expression of both the type IV secretion system and the flagellar apparatus of Brucella melitensis. Cell Microbiol. 71151-1161. [DOI] [PubMed] [Google Scholar]
- 11.Eyles, J. E., Z. C. Carpenter, H. O. Alpar, and E. D. Williamson. 2003. Immunological aspects of polymer microsphere vaccine delivery systems. J. Drug Target 11509-514. [DOI] [PubMed] [Google Scholar]
- 12.Gately, M. K., L. M. Renzetti, J. Magram, A. S. Stern, L. Adorini, U. Gubler, and D. H. Presky. 1998. The interleukin-12/interleukin-12-receptor system: role in normal and pathologic immune responses. Annu. Rev. Immunol. 16495-521. [DOI] [PubMed] [Google Scholar]
- 13.Germann, T., M. Bongartz, H. Dlugonska, H. Hess, E. Schmitt, L. Kolbe, E. Kolsch, F. J. Podlaski, M. K. Gately, and E. Rude. 1995. Interleukin-12 profoundly up-regulates the synthesis of antigen-specific complement-fixing IgG2a, IgG2b, and IgG3 antibody subclasses in vivo. Eur. J. Immunol. 25823-829. [DOI] [PubMed] [Google Scholar]
- 14.Germann, T., E. Rude, and E. Schmitt. 1995. The influence of IL-12 on the development of Th1 and Th2 cells and its adjuvant effect for humoral immune responses. Res. Immunol. 146481-486. [DOI] [PubMed] [Google Scholar]
- 15.Golding, B., D. E. Scott, O. Scharf, L. Y. Huang, M. Zaitseva, C. Lapham, N. Eller, and H. Golding. 2001. Immunity and protection against Brucella abortus. Microbes Infect. 343-48. [DOI] [PubMed] [Google Scholar]
- 16.Hong, P. C., R. M. Tsolis, and T. A. Ficht. 2000. Identification of genes required for chronic persistence of Brucella abortus in mice. Infect. Immun. 684102-4107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kahl-McDonagh, M. M., and T. A. Ficht. 2006. Evaluation of protection afforded by Brucella abortus and Brucella melitensis unmarked deletion mutants exhibiting different rates of clearance in BALB/c mice. Infect. Immun. 744048-4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leclerq, S., J. S. Harms, G. M. Rosinha, V. Azevedo, and S. C. Oliveira. 2002. Induction of a Th1-type of immune response but not protective immunity by intramuscular DNA immunization with Brucella abortus GroEL heat-shock gene. J. Med. Microbiol. 5120-26. [DOI] [PubMed] [Google Scholar]
- 19.Lima, K. M., and J. M. Rodrigues, Jr. 1999. Poly-dl-lactide-co-glycolide microspheres as a controlled release antigen delivery system. Braz. J. Med. Biol. Res. 32171-180. [DOI] [PubMed] [Google Scholar]
- 20.Marschutz, M. K., and A. Bernkop-Schnurch. 2000. Oral peptide drug delivery: polymer-inhibitor conjugates protecting insulin from enzymatic degradation in vitro. Biomaterials 211499-1507. [DOI] [PubMed] [Google Scholar]
- 21.Metzger, D. W., L. A. Vogel, V. H. Van Cleave, T. L. Lester, and J. M. Buchanan. 1995. The effects of IL-12 on B-cell subset function. Res. Immunol. 146499-505. [DOI] [PubMed] [Google Scholar]
- 22.Montaraz, J. A., and A. J. Winter. 1986. Comparison of living and nonliving vaccines for Brucella abortus in BALB/c mice. Infect. Immun. 53245-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paranavitana, C., E. Zelazowska, M. Izadjoo, and D. Hoover. 2005. Interferon-gamma associated cytokines and chemokines produced by spleen cells from Brucella-immune mice. Cytokine 3086-92. [DOI] [PubMed] [Google Scholar]
- 24.Pei, J., and T. A. Ficht. 2004. Brucella abortus rough mutants are cytopathic for macrophages in culture. Infect. Immun. 72440-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qiu, B., S. Stefanos, J. Ma, A. Lalloo, B. A. Perry, M. J. Leibowitz, P. J. Sinko, and S. Stein. 2003. A hydrogel prepared by in situ cross-linking of a thiol-containing poly(ethylene glycol)-based copolymer: a new biomaterial for protein drug delivery. Biomaterials 2411-18. [DOI] [PubMed] [Google Scholar]
- 26.Rice-Ficht, A. C., K. A. Dusek, G. J. Kochevar, and J. H. Waite. 1992. Eggshell precursor proteins of Fasciola hepatica. I. Structure and expression of vitelline protein B. Mol. Biochem. Parasitol. 54129-141. [DOI] [PubMed] [Google Scholar]
- 27.Schurig, G. G., R. M. Roop II, T. Bagchi, S. Boyle, D. Buhrman, and N. Sriranganathan. 1991. Biological properties of RB51, a stable rough strain of Brucella abortus. Vet. Microbiol. 28171-188. [DOI] [PubMed] [Google Scholar]
- 28.Schurig, G. G., N. Sriranganathan, and M. J. Corbel. 2002. Brucellosis vaccines: past, present, and future. Vet. Microbiol. 90479-496. [DOI] [PubMed] [Google Scholar]
- 29.Stevens, M. G., S. C. Olsen, G. W. Pugh, Jr., and D. Brees. 1995. Comparison of immune responses and resistance to brucellosis in mice vaccinated with Brucella abortus 19 or RB51. Infect. Immun. 63264-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun, H., K. G. Pollock, and J. M. Brewer. 2003. Analysis of the role of vaccine adjuvants in modulating dendritic cell activation and antigen presentation in vitro. Vaccine 21849-855. [DOI] [PubMed] [Google Scholar]
- 31.Szabo, S. J., B. M. Sullivan, S. L. Peng, and L. H. Glimcher. 2003. Molecular mechanisms regulating Th1 immune responses. Annu. Rev. Immunol. 21713-758. [DOI] [PubMed] [Google Scholar]
- 32.Takenaga, M., Y. Yamaguchi, A. Kitagawa, Y. Ogawa, Y. Mizushima, and R. Igarashi. 2002. A novel sustained-release formulation of insulin with dramatic reduction in initial rapid release. J. Control Release 7981-91. [DOI] [PubMed] [Google Scholar]
- 33.Toth, T. E., J. A. Cobb, S. M. Boyle, R. M. Roop, and G. G. Schurig. 1995. Selective humoral immune response of BALB/c mice to Brucella abortus proteins expressed by vaccinia virus recombinants. Vet. Microbiol. 45171-183. [DOI] [PubMed] [Google Scholar]
- 34.Waite, J. H., and A. C. Rice-Ficht. 1992. Eggshell precursor proteins of Fasciola hepatica. II. Microheterogeneity in vitelline protein B. Mol. Biochem. Parasitol. 54143-151. [DOI] [PubMed] [Google Scholar]
- 35.Wee, S., and W. R. Gombotz. 1998. Protein release from alginate matrices. Adv. Drug Deliv. Rev. 31267-285. [DOI] [PubMed] [Google Scholar]
- 36.Wu, Q., J. Pei, C. Turse, and T. A. Ficht. 2006. Mariner mutagenesis of Brucella melitensis reveals genes with previously uncharacterized roles in virulence and survival. BMC Microbiol. 6102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhan, Y., A. Kelso, and C. Cheers. 1995. Differential activation of Brucella-reactive CD4+ T cells by Brucella infection or immunization with antigenic extracts. Infect. Immun. 63969-975. [DOI] [PMC free article] [PubMed] [Google Scholar]