Summary
Background
Organ transplant recipients (OTRs) have 100-fold increased risk of developing squamous cell carcinomas. Cumulative exposure to ultraviolet radiation is the main risk factor and there is evidence that lack of dermatological surveillance may be responsible for poor levels of knowledge and photoprotection among OTRs.
Objectives
This study evaluated whether routine consultation in a specialist OTR dermatology clinic improves understanding of skin cancer risk and compliance with photoprotection measures.
Methods
A cross-sectional questionnaire-based study was performed in a specialist OTR dermatology clinic at Bart's and the London NHS Trust, London, U.K. The subjects were 399 white-skinned patients under surveillance in a renal transplant clinic, who were sent a postal questionnaire from the renal transplant clinic. The main outcome measures were responses to the questionnaire regarding photoprotective practices and skin cancer risk awareness.
Results
Two hundred and ninety-two of 399 (73%) responded, of whom 89% had previously attended the specialist dermatology clinic. Ninety-six per cent recalled receiving photoprotection advice at least once (85% from dermatologists); 92% reported use of sunscreen; 88% specifically dressed to photoprotect themselves; 96% directly avoided sun exposure during summer; 68% were aware that an increased risk of skin cancer was the reason that extra photoprotective measures were important after a transplant. Photoprotective measures and level of skin cancer awareness were significantly lower in those responders who had never attended the specialist clinic. No obvious bias was identified among nonresponders.
Conclusions
Skin cancer awareness and compliance with photoprotective measures in our patient population is generally greater than previously reported, suggesting that delivery of educational messages regarding skin cancer may be improved if provided in a specialist dermatological setting.
Keywords: audit, compliance, organ transplant recipients, photoprotection, skin cancer awareness, specialist dermatology clinics
Nonmelanoma skin cancers (NMSCs) comprising basal cell carcinomas and squamous cell carcinomas (SCCs) are the commonest malignancies diagnosed in fair-skinned populations worldwide and their incidence is rising dramatically.1 Immunosuppressed organ transplant recipients (OTRs) have an increased risk of NMSC, with a cumulative risk of more than 40% by 20 years after transplantation reported in temperate climates,2 rising to more than 80% in Australia.3 NMSCs in OTRs not only place a significant burden on health care resources, but also cause significant morbidity for individuals as rates are 50–100 times that of the general population and tumours are often multiple and may behave more aggressively.4 It is predicted that NMSC incidence will continue to escalate relentlessly as a clinical problem in OTRs as an inevitable consequence of continuing improvements in long-term graft survival.5 Immunosuppression4 and human papillomavirus6 have been implicated as possible cofactors in transplant skin carcinogenesis, but cumulative exposure to ultraviolet radiation remains the dominant risk factor.7,8 Primary and secondary prevention campaigns have accordingly emphasized the importance of photoprotection and self-surveillance. Sunscreen use has been shown to reduce the incidence of recurrent cutaneous SCC in immunocompetent individuals.9
A study in the U.K. by Seukeran et al.10 in 1998 proposed that lack of dermatological input may be responsible for poor levels of knowledge and inadequate photoprotective measures among OTRs. Other research has confirmed variable and often poor levels of awareness and compliance.11-18 A study by Christenson et al.19 emphasized the need for dermatology sub-specialty care of transplant recipients and despite suggestions by authors of many of these studies that routine assessment of OTRs in a dedicated transplant skin clinic may be prudent, such surveillance is uncommon in most countries, including the U.K.,20 and the effectiveness of such clinics in delivering photoprotection and skin cancer awareness educational messages is unclear.
At Bart's and the London NHS Trust, a dedicated OTR skin clinic was established in 1989 to provide all newly transplanted individuals with information on their skin cancer risk and to screen for skin problems by regular outpatient review.2,21 Most patients attending this clinic are renal transplant recipients (RTRs) although a small cohort of nonrenal transplant patients is also followed up in the same way. This is not a cardiac or liver transplant centre and the small number of such patients who are seen in our clinic were excluded from analysis in this study as they do not represent a complete cohort. Patients are not routinely provided with advice prior to transplant, but are usually given advice immediately post-transplant by the renal transplant team (usually the renal transplant nurses). In addition, all OTRs are routinely referred to the physician-led specialist dermatology clinic within 6–12 months of transplantation. They are reviewed annually thereafter, or more frequently if clinically indicated. At the initial clinic visit individual skin cancer risk is assessed through detailed history and full clinical examination by a dermatologist. Patients are counselled regarding their skin cancer risk, and advised on self-surveillance and sun protective measures, including detailed information on sun avoidance, use of photoprotective clothing and application of high sun protection factor (SPF) sunscreen on all exposed body parts daily through at least April to October. Practical advice is also provided on the types of sunscreens available, and patients' general practitioners are requested to provide these on prescription where necessary in order to reduce costs to the patients. Advice is supplemented with written information. More than 1600 transplant skin cancers have been diagnosed and treated through this OTR skin clinic but the value of this systematic surveillance approach in successfully relaying key primary and secondary prevention educational messages has not previously been assessed. The aim of this study was therefore to evaluate levels of compliance with sun protection measures and awareness of skin cancer risk in our renal transplant population. As our unit does have a dedicated dermatology clinic for transplant recipients, this study in effect ‘closes the audit loop’ with regards to suggestions made by Seukeran et al.10 highlighting the need for dermatological input in raising the awareness of transplant patients to their increased risk of NMSC.
Patients and methods
Postal questionnaires were sent to all white-skinned patients identified through the renal transplant database as being under long-term follow-up in the renal department of our institute between August 2004 and April 2005. Over 600 patients are currently under regular surveillance in the renal transplant clinic, but approximately 20% have Fitzpatrick skin types V and VI, and are consequently at low risk of skin cancer and were therefore excluded from this study. After review of available clinical information, additional patient groups excluded were those deemed unable to answer the questionnaire adequately due to documented disorders such as previous severe cerebrovascular accident and learning difficulties. In total, 399 patients were eligible for the study.
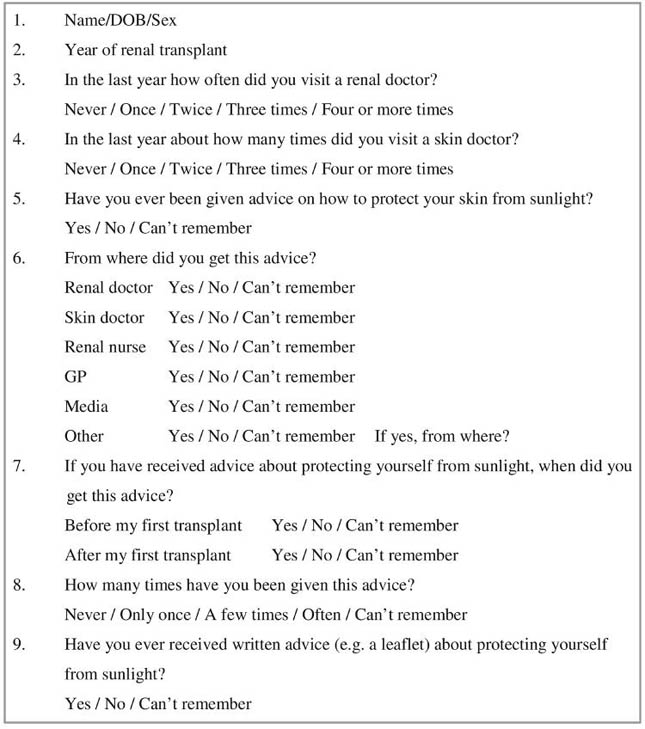
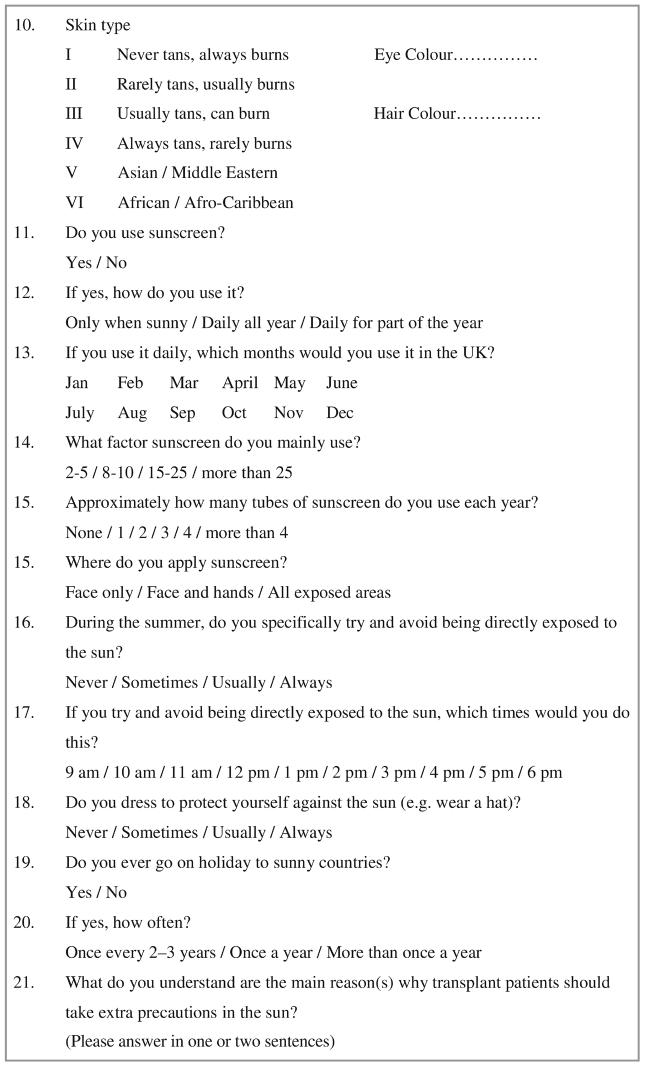
The questionnaire was delivered entirely via the renal department and no mention of the dermatology department was made in order to minimize any bias in answering questions that this may have introduced. The questionnaire consisted of 20 items requesting details of when and where, if ever, patients recalled receiving information on photoprotection, the nature of this advice, the sun protective measures they were currently using (three broad categories were use of sunscreen, use of protective clothing and sun avoidance) and their understanding of why they should take extra photoprotective precautions. Each question had a range of responses which had to be circled, except for the final question which required the patient to write in their own words why sun protection was of particular importance in transplant recipients. Response was considered to be positive if the written answer included the mention of ‘skin cancer’ (see Fig. 1 for outline of questionnaire). A second round of questionnaires was posted to those who had not responded within 6 weeks. In some cases patients were contacted by telephone in order to clarify information submitted in the questionnaire (although unanswered questions were not pursued further).
Fig 1.
Outline of questionnaire.
Statistical analysis
Demographics of responders to the questionnaire were analysed and, by examination of their medical records, it was also determined whether they had a history of NMSC and whether they had ever attended the specialist OTR dermatology clinic following transplantation. Responses from patients with and without a history of skin cancer were compared to see whether this influenced their sun protection behaviour. Associations between skin phototype and photoprotective measures were also examined. Responses from patients who had never attended the dermatology clinic were compared with those who had attended at least once. The demographics of nonresponders were also analysed. All data analyses were performed using STATA computer software (StataCorp, College Sation, TX, U.S.A., 2005). Fisher's exact test and unpaired Student's t-test were used to compare response proportions and means, respectively. Exposures with three or more natural ordered categories were tested on one-degree of freedom χ2 test for linear trend. All P-values reported were obtained using two-sided tests of statistical significance.
Results
Two hundred and ninety-two of 399 questionnaires were returned, producing a response rate of 73%. Of the responders, 167 (57%) were male and 125 (43%) female (male/female ratio of 1·3), with a mean age of 52 years and a mean time since transplantation of 12·9 years. Two hundred and sixty-one (89%) responders had attended the dermatology clinic at least once following transplantation. Most were skin type III (Table 1).
Table 1.
Patient demographics
| Responders |
All nonresponders |
|||||
|---|---|---|---|---|---|---|
| Responders | All nonresponders | Attended dermatology clinic |
Never attended dermatology clinic |
Attended dermatology clinic |
Never attended dermatology clinic |
|
| n/N (%) | 292/399 (73·2) | 107/399 (26·8) | 261/292 (89·4) | 31/292 (10·6) | 84/107 (78·5) | 23/107 (21·5) |
| M/F ratio | 1·3 (167/125) | 2·1 (72/35) P = 0·08a |
1·4 (154/107) | 0·7 (13/18) P = 0·08a |
2·1 (57/27) | 1·9 (15/8) P = 0·81a |
| Mean ± SD age, years (range) | 52·1 ± 13·3 (19–82) 1 missing |
47·6 ± 13·8 (20–83) 2 missing P = 0·003b |
52·3 ± 13·0 (21–82) 1 missing |
50·7 ± 15·8 (19–80) 0 missing P = 0·54b |
48·3 ± 13·5 (20–83) 0 missing |
44·9 ± 14·9 (23–72) 2 missing P = 0·32b |
| Mean ± SD time since transplant, years (range) | 12·9 ± 7·6 (1–36) 2 missing |
10·6 ± 7·1 (1–32) 2 missing P = 0·007b |
13·4 ± 7·3 (1–36) 2 missing |
9·1 ± 8·8 (1–29) 0 missing P = 0·003b |
11·4 ± 6·9 (1–32) 0 missing |
7·4 ± 6·8 (1–22) 2 missing P = 0·02b |
| Skin type, n (%) | ||||||
| I | 22 (7·5) | 7 (6·5) | 19 (7·3) | 3 (9·7) | 7 (8·3) | 0 |
| II | 56 (19·2) | 22 (20·6) | 50 (19·2) | 6 (19·4) | 21 (25·0) | 1 (4·3) |
| III | 124 (42·5) | 26 (24·3) | 114 (43·7) | 10 (32·3) | 26 (31·0) | 0 |
| IV | 86 (29·4) | 5 (4·7) | 75 (28·7) | 11 (35·5) | 5 (6·0) | 0 |
| Missing | 4 (1·4) | 47 (43·9) Too many missing values, not tested |
3 (1·2) | 1 (3·2) P = 0·61a |
25 (29·7) | 22 (95·7) Too many missing values, not tested |
| Skin cancers, n (%) | ||||||
| No | 215 (73·6) | 95 (88·8) | 184 (70·5) | 31 (100) | 72 (85·7) | 23 (100) |
| Yes | 77 (26·4) | 12 (11·2) | 77 (29·5) | 0 | 12 (14·2) | 0 |
| Missing | 0 | 0 P = 0·01a |
0 | 0 P < 0·001a |
0 | 0 P = 0·07a |
| Attendance dermatology, n (%) | ||||||
| Ever | 261 (89·4) | 84 (78·5) | ||||
| Never | 31 (10·6) | 23 (21·5) P = 0·008a |
||||
Two-tailed Fisher's exact test
two-tailed Student's t-test.
Photoprotection measures and skin cancer awareness
Overall, 96% of responders recalled receiving photoprotection advice at least once, 85% from dermatologists, 51% from renal physicians, 28% from renal transplant nurses, 11% from general practitioners, 29% from the media, and 60% of patients recalled receiving written advice on photoprotection. This advice was received before transplantation by 19% of patients. Two hundred and sixty-nine (92%) of responders reported using sunscreen: 82 (30%) used SPF 15–25 and 173 (64%) used SPF > 25; 29 (11%) applied sunscreen daily all year round, 96 (36%) used it daily for at least part of the year and 143 (53%) used sunscreen only during sunny weather. Of those patients who used sunscreen daily for part of the year, 22% did so throughout the months of April to October with the remainder using it predominantly in between these months, during the summer. Of the 269 responders who used sunscreen, 215 (80%) applied it to all sun-exposed areas, 41 (15%) applied it to the face and hands only and 12 (4%) to the face only. One hundred and fifty-nine of 223 (71%) patients who responded to the question used two or more tubes of sunscreen each year. Two hundred and eighty-two (96%) responders avoided exposure to the sun in summer with 45 (15%), 140 (48%) and 97 (33%) doing so sometimes, usually and always, respectively. Two hundred and fifty-six (88%) dressed to protect themselves from the sun at least sometimes. One hundred and ninety-nine (68%) were aware that an increased risk of skin cancer was the main reason extra photoprotective measures were important after a transplant.
Skin cancer status and skin phototype
As shown in Table 2, 77 (26%) responders had a previous biopsy-proven skin cancer, with a mean time since transplantation of 16·8 years compared with 11·5 years in those patients without skin cancer (P < 0·001). There was no difference in skin phototypes between the two groups. All 77 responders with skin cancer had previously attended the dermatology clinic and all reported having received photoprotection advice, as did 203 of 215 (94%) of those without skin cancer. Higher levels of sunscreen use were reported in patients with a history of NMSC (99% vs. 90%; P = 0·02). Unexpectedly, levels of skin cancer awareness were greater in those without a prior history of NMSC compared with those who have had previous skin cancer (70% vs. 62%; P = 0·03). The reasons for this are not clear but may in part be related to this being a free text question (the only such one in the entire questionnaire). There were no significant differences in sunscreen use and skin cancer awareness according to skin phototype.
Table 2.
Skin cancer status and clinic attendance
| History of NMSC |
Attendance at dermatology clinic |
|||
|---|---|---|---|---|
| Yes | No | Yes | No | |
| Responders, n/N (%) | 77/292 (26·4) | 215/292 (73·6) | 261/292 (89·4) | 31/292 (10·6) |
| M/F ratio | 1·6 (47/30) | 1·3 (120/95) P = 0·50a |
1·4 (154/107) | 0·7 (13/18) P = 0·08a |
| Mean ± SD age, years (range) | 58·6 ± 11·0 (31–82) 0 missing |
49·8 ± 13·3 (19–81) 1 missing P < 0·001b |
52·3 ± 13·0 (21–82) 1 missing |
50·7 ± 15·8 (19–80) 0 missing P = 0·54b |
| Mean ± SD time since treatment, years (range) | 16·8 ± 6·3 (2–33) 0 missing |
11·5 ± 7·5 (1–36) 2 missing P < 0·001b |
13·4 ± 7·3 (1–36) 2 missing |
9·1 ± 8·8 (1–29) 0 missing P = 0·003b |
| Skin type, n (%) | ||||
| I | 7(9·1) | 15 (7·0) | 19 (7·3) | 3 (9·7) |
| II | 16 (20·8) | 40 (18·6) | 50 (19·2) | 6 (19·4) |
| III | 31 (40·2) | 93 (43·2) | 114 (43·7) | 10 (32·2) |
| IV | 23 (29·9) | 63 (29·3) | 75 (28·7) | 11 (35·5) |
| Missing | 0 | 4 (1·9) P = 0·88a |
3 (1·1) | 1 (3·2) P = 0·61a |
| Photoprotection advice, n (%) | 77 (100) | 203 (94·4) P = 0·04a |
256 (98·1) | 24 (77·4) P < 0·001a |
| Use of sunscreen, n (%) | 76 (98·7) | 193 (89·8) P = 0·02a |
248 (95·0) | 21 (67·7) P < 0·001a |
| Skin type, n (%)c | ||||
| I | 7 (9·2) | 12 (6·2) | 18 (7·3) | 1 (4·8) |
| II | 16 (21·1) | 36 (18·7) | 49 (19·8) | 3 (14·3) |
| III | 31 (40·8) | 87 (45·1) | 109 (44·0) | 9 (42·9) |
| IV | 22 (29·0) | 58 (30·1) | 72 (29·0) | 8 (38·1) |
| Missing | 0 | 0 P = 0·78a |
0 | 0 P = 0·85a |
| SPF, n (%)c | ||||
| 2–5 | 0 | 1 (0·5) | 1 (0·4) | 0 |
| 8–10 | 1 (1·3) | 10 (5·2) | 7 (2·8) | 4 (19·1) |
| 15–25 | 19 (25·0) | 63 (32·6) | 76 (30·7) | 6 (28·6) |
| > 25 | 56 (73·7) | 117 (60·6) | 163 (65·7) | 10 (42·6) |
| Missing | 0 | 2 (1·0) χ2 (1) = 4·7, P trend = 0·03 |
1 (0·4) | 1 (4·8) χ2 (1) = 5·2, P trend = 0·02 |
| Frequency of sunscreen use, n (%)c | ||||
| Sunny | 38 (49·4) | 105 (54·4) | 130 (52·4) | 13 (61·9) |
| Daily all year | 11 (14·3) | 18 (9·3) | 27 (10·9) | 2 (9·5) |
| Daily part of year | 27 (35·1) | 69 (35·8) | 90 (36·3) | 6 (28·6) |
| Missing | 0 | 1 (0·5) P = 0·47a |
1 (0·4) | 0 P = 0·76a |
| Sun avoidance in summer, n (%) | ||||
| Never | 0 | 4 (1·9) | 3 (1·1) | 1 (3·2) |
| Sometimes | 4 (5·2) | 41 (19·1) | 40 (15·3) | 5 (16·1) |
| Usually | 37 (48·0) | 103 (47·9) | 129 (49·4) | 11 (35·5) |
| Always | 36 (46·8) | 61 (28·4) | 84 (32·2) | 13 (41·9) |
| Missing | 0 | 6 (2·8) χ2 (1) = 13·1, P trend < 0·001 |
5 (1·9) | 1 (3·2) χ2 (1) = 0·14, P trend = 0·71 |
| Dress to protect from the sun, n (%) | ||||
| Never | 3 (3·9) | 26 (12·1) | 24 (9·2) | 5 (16·1) |
| Sometimes | 13 (16·9) | 69 (32·1) | 72 (27·6) | 10 (32·3) |
| Usually | 34 (44·2) | 65 (30·2) | 92 (35·2) | 7 (22·5) |
| Always | 27 (35·0) | 48 (22·3) | 68 (26·1) | 7 (22·5) |
| Missing | 0 | 7 (3·3) χ2 (1) = 12·3, P trend < 0·001 |
5 (1·9) | 2 (6·5) χ2 (1) = 1·72, P trend = 0·19 |
| Understanding of reasons for extra photoprotection, n (%) | ||||
| Mention of ‘cancer’ | 48 (62·3) | 151 (70·2) | 186 (71·3) | 13 (41·9) |
| Other answers | 28 (36·4) | 47 (21·9) | 62 (23·8) | 13 (41·9) |
| Missing | 1 (1·3) | 17 (7·9) P = 0·03a |
13 (5·0) | 5 (16·1) P = 0·01a |
NMSC, nonmelanoma skin cancer; SPF, sun protection factor.
Two-tailed Fisher's exact test
two-tailed Student's t-test.
Restricted to people who answered positively for the question on sunscreen use.
Attenders vs. nonattenders
As shown in Table 2, 31 (11%) of responders had never previously attended the dermatology clinic. Of these, none had a history of skin cancer compared with 77 (30%) of attenders (P < 0·001) and the mean time since transplantation was 9·1 years compared with 13·4 years in attenders (P = 0·003). Mean age and skin phototype were similar, but sunscreen use was lower in nonattenders (68% vs. 95% of attenders; P < 0·001) and 43% of nonattenders used SPF > 25 (compared with 66% of attenders; P trend = 0·02). Skin cancer awareness was also significantly lower in nonattenders (42% vs. 71% of attenders; P = 0·01).
Responders vs. nonresponders
As shown in Table 1, 107 of 399 (27%) patients failed to respond after posting questionnaires twice, and one patient declined to participate. Demographic and other features were analysed for nonresponders by examining clinical records in order to identify possible sources of bias. Seventy-two of 107 (67%) nonresponders were male, with a male/female ratio of 2 contrasting with a ratio of 1·3 for responders (P = 0·08). The mean time since transplantation was also significantly lower in nonresponders (10·6 years vs. 12·9 years; P = 0·007). Other key demographic variables were no different between responders and nonresponders. Eighty-four of 107 (79%) nonresponders had attended dermatology clinic at least once and 12 (11%) had a history of skin cancer (P = 0·03).
Discussion
In this prospective, questionnaire-based study of transplant recipients' photoprotective practices and levels of skin cancer awareness, 96% of responders recalled receiving photoprotection advice, 92% reported use of sunscreen, 88% specifically dressed to photoprotect themselves, 96% directly avoided sun exposure during summer, and 68% were aware that an increased risk of skin cancer was the reason that photoprotective measures were important after a transplant. Photoprotective measures and level of skin cancer awareness were significantly lower in those responders who had not attended the specialist dermatology clinic. No obvious bias was identified in nonresponders.
There have been eight previous studies examining one or more aspects of photoprotective practice and skin cancer knowledge in OTRs: these are summarized in Table 3. Although there is variation in sample size, setting and study design, in general the levels of knowledge and compliance with photoprotective measures in our OTR patient population were greater than those previously reported.10-17
Table 3.
Summary of findings in previous studies of photoprotection and skin cancer awareness in organ transplant recipients
| Reference, country, year |
No. patients/no. responders |
M/F ratio |
Type/ dermatology settinga |
Dedicated transplant skin clinicb |
Mean time from transplant (years) |
% who had previously ever attended dermatology clinic |
% who had received photoprotection advice |
% advised by a dermatologist |
% using sunscreen /dailyc |
SPF of sunscreen |
% practising sun avoidanced |
Clothing used to photoprotect (%)e |
Knowledge of skin cancer risk (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 11, Wales, 1997 | 204/128 | 1·46 | Postal/no | No | NA | NA | 46 | NA | 40/NA | < 10 in > 90% | NA | NA | NA |
| 10, U.K., 1998 | 202/202 | 1·69 | Oral/no | No | 6·8 | 17 | 54 | 17 | 57/NA | < 15 in 63% | 18 | 40 | 30 |
| 12, U.S.A., 1999f | 122/NA | 1·49 | Oral/no | No | 3·1 | 27 | 41 | NA | 67/NA | NA | NA | NA | 59 |
| 13, Canada, 2004 | 205/NA | 2·11 | Oral/yes | Yes | 51·2% > 5 years |
NA | NA | NA | 70/36 | NA | 77 | 81 | NA |
| 14, U.S.A., 2004f | 200/NA | 1·0 | Telephone/no | No | 2·9 | NA | NA | NA | 35/NA | NA | 20 | 21 | 12 |
| 15, France, 2004 | 520/445 | 1·6 | Written/yesg | Yes | 12·5 | NA | 91 | 80 | 63/NA | > 60 in 69% | 63 | 36 | 47 |
| 16, Poland, 2004h | 151/NA | 1·52 | Written/no | No | 3·2 | NA | 75 | 6 | 38/NA | Mean 12 | 73 | 80 | 68 |
| 17, Ireland, 2005 | 270/NA | 2·07 | Oral/yes (some) | Yes | 6·8 (median) |
37 | NA | NA | 74/NA | NA | NA | NA | NA |
| Present study, U.K., 2005 | 399/292 | 1·34 | Postal/no | Yes | 12·9 | 89 | 96 | 85 | 92/43 | > 25 in 64% | 96 | 88 | 68 |
NA, information not available; SPF, sun protection factor.
Type of survey/questionnaire is detailed; whether this was presented in a dermatology setting is also indicated.
Centres in which a dedicated transplant skin clinic is established are indicated. In reference 17, it seems that the dedicated clinic may have been established after completion of the survey.
Percentage of patients using sunscreen at least during sunny weather; ‘daily’ use refers to daily at least through the summer months.
Avoidance of midday sun, or avoidance of intentional tanning.
Highest percentage of patients reporting clothing worn at least ‘sometimes’ is recorded here.
Although the questionnaire was delivered anonymously, a covering letter stressed the importance of sun protection and the need to evaluate patients' knowledge and compliance with this.
Two patients with a history of skin cancer were excluded.
Several studies have been reported from centres without a dedicated transplant dermatology clinic. The first report from the U.K. used a postal questionnaire to evaluate knowledge of the need to reduce sun exposure and sun photoprotective measures taken by 204 RTRs.11 Of 128 respondents, 91% were aware of the hazards of sun exposure (although knowledge of skin cancer was not specifically assessed). However, fewer than 40% used sunscreens and in 90% of cases this was SPF < 10. The authors suggested that these patients were not receiving adequate information about photoprotection and proposed that the transplant team should take responsibility for providing this information at the time of transplant and regularly thereafter. Seukeran et al.10 subsequently undertook a clinician-delivered questionnaire-based survey of 202 patients in a U.K. renal transplant clinic. Of 202 patients, 54% recalled receiving advice on photoprotection of whom 17% had received this advice from dermatologists. Fifty-seven per cent used sunscreen with 63% using SPF < 15, and only 30% were aware of skin cancer risk in OTRs. A similar study from the U.S.A. also reported low levels of knowledge and compliance.12 In a second study from the U.S.A., Robinson and Rigel14 compared sun protection attitudes and behaviours in a telephone survey of 200 OTRs and a random sample of 1091 U.S. residents. Only 12% of OTRs were aware of their increased risk of skin cancer and 35% reported regularly using sunscreen. In a Polish study,16 Szepietowski et al. questioned 151 RTRs: although 68·2% were aware of skin cancer risk and 74·8% of patients had been informed about the need for sun protection, 62·3% did not comply with this advice. None of these studies mentioned the existence of a dedicated OTR dermatology clinic, and additionally, details of individual skin phototypes, the proportion of the transplant cohort interviewed, and details of nonresponders were not presented. A Swedish study analysing skin cancer risk matched 95 transplant patients with SCC to 154 patients without18 and requested details of sun protection measures taken and sources of advice received. The authors report that 42% of cases and 39% of controls had received sun protection advice but do not present detailed analysis of this.
Two recent studies have reported findings from centres in which dedicated OTR dermatology clinics are already established.13,15 In a study from Paris, Mahé et al.15 reported that 91% of 445 responders to a questionnaire had been informed of the need for photoprotection, 47% were aware of skin cancer risk and 63% applied sunscreen regularly, the majority using SPF 60 or above (although 46% used no more than one tube of sunscreen per year). However, a major drawback of this study is that it was conducted through the dermatology clinic and, in a letter accompanying the questionnaire, the authors stressed the importance of sun protection in OTRs and the need to evaluate patients' knowledge and compliance with sun protection measures. Such statements may well introduce bias in subsequently answering questions, and we specifically sought to avoid this in our study by dissociating the questionnaire from the dermatology clinic and omitting all mention of expected endpoints. A Canadian study was also conducted in the setting of a specialist dermatology clinic.13 Although it evaluated sun protection behaviour of 205 consecutive newly transplanted individuals (who presumably had not previously attended the dermatology clinic), the institution had a policy of providing some education concerning skin cancer risk and prevention to all patients prior to transplant. This may account for their higher levels of sunscreen use at 70%. No information is provided on skin cancer awareness of these patients.
In the most recent series reported from Dublin, 270 patients were interviewed in the settings of both renal and dermatology clinics,17 of whom 99 (37%) patients had previously attended a dermatology clinic. Prior to transplant, 68·5% of patients reported never using a sunscreen while 5·6% always used a sunscreen on a sunny day; post-transplant, these figures were 25·9% and 36·7%, respectively. In contrast to our study, no significant differences were identified in sun protection measures in association with attendance at a dermatology clinic. This may reflect the smaller numbers who had ever attended a dermatology clinic (99 vs. 261 in our study). No data are provided on patients' knowledge of skin cancer risk.
While we have attempted to eliminate possible sources of bias by specifically avoiding association of the questionnaire with the dermatology clinic, bias may have been introduced in other ways. In particular, 27% of patients did not respond to our questionnaire and we therefore examined this group in more detail using clinical records. Nonresponders were represented by a higher proportion of younger males transplanted for a shorter period of time. This may be because females are more aware of the need for sun protection and are more compliant with sun protection measures, as has been shown in other studies,14-16 and may therefore have been more likely to have answered our questionnaire, thereby introducing bias. Insufficient information was available to determine whether there was a significant difference in skin type between responders and nonresponders. Skin cancer was significantly less common in nonresponders (11·2% vs. 26·4%; P = 0·01). Responders without skin cancer had high skin cancer awareness but lower levels of overall photoprotection as compared with those with skin cancer, emphasizing the importance of continued reinforcement of sun protection advice.
The possibility of differences between nonattenders and attenders at the dermatology clinic as a source of bias was also separately assessed. None of the nonattenders had a history of skin cancer and their mean time since transplantation was shorter than that of attenders (P = 0·003). One possible explanation is that this may reflect the small number of patients who have been transplanted for less than 12 months and who have not yet been referred to the dermatology clinic by the renal physicians. There were no significant differences in the proportion of patients with skin phototypes I and II between attenders and nonattenders, suggesting that patients at potentially higher risk of developing skin cancer are no more likely to attend the dermatology clinic. The possibility that our population differs from other OTR cohorts cannot be excluded, although there is no evidence to suggest that this is the case.
In summary, it appears that our policy of routine surveillance has resulted in a well-informed patient population who report higher levels of photoprotective practices and skin cancer awareness compared with previous studies. The standard of care that all transplant patients should be seen in a dedicated dermatology clinic in order to optimize skin cancer education is supported by our findings. However, sun exposure patterns post-transplant may not necessarily correlate with skin cancer risk,18 and follow-up is required, specifically to confirm whether this improved level of knowledge and photoprotective behaviour will have beneficial long-term effects in reducing skin cancer incidence in this high-risk population.
Acknowledgments
F.I. is supported by the Medical Research Council; C.A.H. and C.M.P. are supported by Cancer Research UK.
Footnotes
Conflicts of interest
None declared.
References
- 1.Diepgen TL, Mahler V. The epidemiology of skin cancer. Br J Dermatol. 2002;146(Suppl. 61):1–6. doi: 10.1046/j.1365-2133.146.s61.2.x. [DOI] [PubMed] [Google Scholar]
- 2.Glover MT, Niranjan N, Kwan JT, Leigh IM. Non-melanoma skin cancer in renal transplant recipients: the extent of the problem and a strategy for management. Br J Plast Surg. 1994;47:86–9. doi: 10.1016/0007-1226(94)90164-3. [DOI] [PubMed] [Google Scholar]
- 3.Ramsay HM, Fryer AA, Hawley CM, et al. Non-melanoma skin cancer risk in the Queensland renal transplant population. Br J Dermatol. 2002;147:950–6. doi: 10.1046/j.1365-2133.2002.04976.x. [DOI] [PubMed] [Google Scholar]
- 4.Euvrard S, Kanitakis J, Claudy J. Skin cancers after organ transplantation. N Engl J Med. 2003;348:1681–91. doi: 10.1056/NEJMra022137. [DOI] [PubMed] [Google Scholar]
- 5.Hariharan S, Johnson CP, Bresnahan BA, et al. Improved graft survival after renal transplantation in the United States, 1988 to 1996. N Engl J Med. 2000;342:605–12. doi: 10.1056/NEJM200003023420901. [DOI] [PubMed] [Google Scholar]
- 6.Harwood CA, Proby CM. Human papillomaviruses and non-melanoma skin cancer. Curr Opin Infect Dis. 2002;15:101–14. doi: 10.1097/00001432-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 7.International Agency for Research on Cancer . Solar and Ultraviolet Radiation and Human Exposure: IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Vol. 55. Lyon: IARC; 1992. [PMC free article] [PubMed] [Google Scholar]
- 8.Vitasa BC, Taylor HR, Strickland PT, et al. Association of nonmelanoma skin cancer and actinic keratosis with cumulative solar ultraviolet exposure in Maryland watermen. Cancer. 1990;65:2811–17. doi: 10.1002/1097-0142(19900615)65:12<2811::aid-cncr2820651234>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 9.Green A, Williams G, Neale R, et al. Daily sunscreen application and betacarotene supplementation in suppression of basal cell and squamous cell carcinomas of the skin. Lancet. 1999;354:723–9. doi: 10.1016/S0140-6736(98)12168-2. [DOI] [PubMed] [Google Scholar]
- 10.Seukeran DC, Newstead CG, Cunliffe WJ. The compliance of renal transplant recipients with advice about sun protection measures. Br J Dermatol. 1998;138:301–4. doi: 10.1046/j.1365-2133.1998.02079.x. [DOI] [PubMed] [Google Scholar]
- 11.Butt A, Roberts DL. Renal transplant recipients and protection from sun: need for education. Lancet. 1997;349:179–80. doi: 10.1016/s0140-6736(05)60981-6. [DOI] [PubMed] [Google Scholar]
- 12.Cowen EW, Billingsley EM. Awareness of skin cancer by kidney transplant patients. J Am Acad Dermatol. 1999;40:687–701. doi: 10.1016/s0190-9622(99)70149-0. [DOI] [PubMed] [Google Scholar]
- 13.Donovan JCH, Rosen CF, Shaw JC. Evaluation of sun-protective practices of organ transplant recipients. Am J Transplant. 2004;4:1852–8. doi: 10.1111/j.1600-6143.2004.00584.x. [DOI] [PubMed] [Google Scholar]
- 14.Robinson JK, Rigel DS. Sun protection attitudes and behaviors of solid-organ transplant recipients. Dermatol Surg. 2004;30:610–15. doi: 10.1111/j.1524-4725.2004.30145.x. [DOI] [PubMed] [Google Scholar]
- 15.Mahé E, Morelon E, Fermanian J, et al. Renal-transplant recipients and sun protection. Transplantation. 2004;78:741–4. doi: 10.1097/01.tp.0000131818.24302.b8. [DOI] [PubMed] [Google Scholar]
- 16.Szepietowski JC, Reich A, Nowicka D, et al. Sun protection in renal transplant recipients: urgent need for education. Dermatology. 2005;211:93–7. doi: 10.1159/000086435. [DOI] [PubMed] [Google Scholar]
- 17.Moloney FJ, Almarzouqi E, O'Kelly P, et al. Sunscreen use before and after transplantation and assessment of risk factors associated with skin cancer development in renal transplant recipients. Arch Dermatol. 2005;141:978–82. doi: 10.1001/archderm.141.8.978. [DOI] [PubMed] [Google Scholar]
- 18.Lindelof B, Granath F, Dal H, et al. Sun habits in kidney transplant recipients with skin cancer: a case–control study of possible causative factors. Acta Derm Venereol (Stockh) 2003;83:189–93. doi: 10.1080/00015550310007193. [DOI] [PubMed] [Google Scholar]
- 19.Christenson LJ, Geusau A, Ferrandiz C, et al. Specialty clinics for the dermatologic care of solid-organ transplant recipients. Dermatol Surg. 2004;30:598–603. doi: 10.1111/j.1524-4725.2004.00143.x. [DOI] [PubMed] [Google Scholar]
- 20.Harden PN, Reece SM, Fryer AA, et al. Skin cancer surveillance in renal transplant recipients: questionnaire survey of current UK practice. BMJ. 2001;323:600–1. doi: 10.1136/bmj.323.7313.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harwood CA, Leedham-Green M, Leigh IM, Proby CM. Low-dose retinoids in the prevention of cutaneous squamous cell carcinomas in organ transplant recipients: a 16-year retrospective study. Arch Dermatol. 2005;141:456–64. doi: 10.1001/archderm.141.4.456. [DOI] [PubMed] [Google Scholar]