Abstract
The therapeutic workplace is a novel intervention that uses access to paid training and employment to reinforce drug abstinence within the context of standard methadone maintenance. We used the Drug Abuse Treatment Cost Analysis Program as a standard method of estimating the economic costs of this intervention. Over a one-year period, the therapeutic workplace served 122 methadone maintenance clients who had a median length of stay of 22 weeks. The workplace maintained a mean daily census of 48 clients. The combined cost of methadone maintenance and the therapeutic workplace was estimated at $362 per week. This cost is less than other treatments that might be used to promote abstinence in individuals who continue to use drugs during methadone treatment. Given prior evidence of effectiveness, these cost data may be useful to policymakers, social service agencies, and researchers interested in using or further developing the therapeutic workplace intervention.
Keywords: Cost, Economics, DATCAP, substance abuse treatment, addiction treatment, unemployment
1. Introduction
Methadone maintenance is an effective, accepted and widely used treatment for opiate addiction (National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction, 1998), but it has limitations. Despite its effectiveness in reducing opiate use, many patients continue to use drugs during methadone maintenance treatment. Cocaine abuse is particularly common in methadone treatment programs (Hser, Anglin, & Fletcher, 1998). Voucher-based abstinence reinforcement has been an effective means of promoting cocaine abstinence in methadone patients (Silverman et al., 1996; Silverman et al., 1998). Under this intervention, patients receive monetary vouchers exchangeable for goods and services contingent on providing cocaine-free urine samples. As would be expected based on basic operant conditioning principles, the effectiveness of abstinence reinforcement interventions increases as the magnitude of reinforcement increases (Silverman, Chutuape, Bigelow, & Stitzer, 1999). Abstinence reinforcement interventions can have lasting effects (Silverman et al., 1998), but some patients do relapse when the contingency ends. Arranging long-term exposure to abstinence reinforcement contingencies appears to be one means of producing reliable long-term effects (Silverman, Robles, Mudric, Bigelow, & Stitzer, 2004). The need for high magnitude and long-duration abstinence reinforcement has raised questions about the practical feasibility of using abstinence reinforcement contingencies widely in society.
Two broad approaches have been proposed to facilitate dissemination of abstinence reinforcement interventions (Silverman, Kaminski, Higgins, & Brady, in press): 1) lower their cost so that they can be feasibly integrated into community drug abuse treatment programs; 2) identify high magnitude and long-duration reinforcers that are available in the community and harness those reinforcers to promote drug abstinence and other related therapeutic behavior change. These two approaches are not mutually exclusive and could be used together to achieve maximal effect. Although the cost-lowering option is appealing, it is only a partial solution, since it involves reducing the magnitude and duration of reinforcement, which also reduces effectiveness.
In an effort to identify high magnitude reinforcers that are available in communities, some investigators have explored the possibility of using reinforcers that are available in competitive and supported employment settings. Both competitive and supported workplaces control high magnitude reinforcers that might be harnessed for therapeutic purposes. For the subset of persistent drug users who are gainfully employed, competitive employment offers routine wages that are high in magnitude and maintained over time. For chronically unemployed and unskilled individuals, supported workplaces can offer wages or training stipends that can be relatively high in magnitude (Dickinson & Maynard, 1981; Kashner et al., 2002; Milby et al., 1996). One of the largest and most recognized of those programs is the U.S. Department of Veterans Affairs’ Compensated Work Therapy program (Kashner et al., 2002). To harness reinforcers available in employment settings, an employment-based abstinence reinforcement contingency can be arranged in which employees must remain abstinent to work and earn wages. Some investigators have explored employment-based abstinence reinforcement over the years (Cohen, Bigelow, Hargett, Allen, & Halsted, 1973; Crowley, 1986; Milby et al., 1996; Miller, 1975; Silverman, Svikis, Robles, Stitzer, & Bigelow, 2001); however, there has not been a consistent effort to develop and systematically evaluate an employment-based abstinence reinforcement intervention until recently (Knealing, Wong, Diemer, Hampton, & Silverman, 2006; Silverman et al., 2001; Silverman et al., 2002; Silverman, 2004; Silverman et al., 2005; Silverman et al., in press). Silverman and colleagues have developed an employment-based reinforcement intervention called the therapeutic workplace. The therapeutic workplace has been used primarily to promote drug abstinence in individuals who continue to use cocaine and heroin during standard methadone maintenance treatment. It has not been used as an alternative to methadone treatment. Instead, it has been offered to individuals while they continue to receive standard methadone maintenance treatment.
Methadone maintenance patients can participate in two phases in the therapeutic workplace. The initial phase of the intervention is designed to initiate drug abstinence and to establish skills that participants would need to succeed in the workplace. The second phase of the intervention is designed to maintain abstinence and employment over time. Throughout both phases, individuals receive standard methadone treatment and are also paid to work in a workplace. To promote and maintain drug abstinence, participants are required to provide drug-free urine samples to gain and maintain access to the workplace. In that way, participants can work and earn wages, but only as long as they remain abstinent from drugs.
During phase 1 of the intervention, each individual’s job is to participate in an intensive training program designed to teach skills that the individual will need to maintain gainful employment. Participants are paid in vouchers exchangeable for goods and services to reduce the chance that participants will use their earnings to purchase drugs. Once abstinent and skilled, participants can proceed to phase 2 of the intervention. In that phase, participants are employed in real jobs and are paid in standard paychecks. Participants in the initial therapeutic workplace were taught data entry skills during the initial phase of the intervention, and were then hired to serve as data entry operators in a data entry business in the second phase.
The therapeutic workplace intervention was initially shown to be effective in reducing opiate and cocaine use in a population of pregnant and recently post-partum women enrolled in methadone treatment (Silverman et al., 2001; Silverman et al., 2002). In that study, participants were randomly assigned to a therapeutic workplace or a usual care control group. Compared to the usual-care control group, therapeutic workplace participants provided significantly more urine samples negative for opiates and cocaine during the first 6 months of treatment (33% vs. 59% negative, respectively; Silverman et al., 2001) and comparable significant differences were maintained for 3 years after intake (Silverman et al., 2002).
Since the initial demonstration of efficacy, the therapeutic workplace has been transformed from a manually administered intervention to a web-based system to reduce costs and make the process more efficient (Silverman et al., 2005). This web-based therapeutic workplace intervention was shown to be effective in promoting cocaine abstinence in a population of unemployed injection drug users who were enrolled in community methadone treatment programs in Baltimore city, but who continued to use cocaine at high rates (Silverman et al., in press).
In that study, participants were invited to attend the workplace where they could work 20 hours per week and earn about $10 per hour in vouchers. Participants were also required to provide urine samples three times per week. Initially, participants could work and earn vouchers independent of their urinalysis results. Participants who attended the workplace consistently and continued to provide cocaine-positive samples were randomly assigned to a Work Only or Abstinence & Work group. Like typical competitive or supported employment, Work Only participants could work and earn wages independent of urinalysis results. In contrast, Abstinence & Work participants could continue to work only when they provided urine samples that confirmed recent cocaine abstinence. If a participant ever provided a cocaine-positive urine sample, the participant was not allowed to work that day and experienced a temporary decrease in the pay. The percentage of cocaine-negative urine samples was significantly higher in the Abstinence & Work (29%) compared to the Work Only (10%) group. These results showed that the therapeutic workplace could increase cocaine abstinence in methadone patients and that the abstinence contingency is critical to increasing cocaine abstinence.
The studies above suggest that the therapeutic workplace intervention could be useful as an adjunct to standard methadone maintenance treatment. The therapeutic workplace could be useful either as a short-term intervention designed to initiate abstinence and establish job skills (i.e., phase 1 only) or as a long-term intervention designed to maintain abstinence over time (i.e., phases 1 and 2). Long-term exposure to both phases of the therapeutic workplace intervention might be useful for many persistent drug users who are at risk for relapse. Short-term exposure might be useful to initiate abstinence and thereby prepare individuals to benefit from other less intensive and less costly interventions. Prior research on voucher-based abstinence reinforcement suggests that if the therapeutic workplace intervention can initiate cocaine abstinence in methadone patients, then other less costly interventions (e.g., take-home abstinence reinforcement contingencies) might be able to maintain abstinence after the voucher-based abstinence reinforcement intervention is discontinued (Silverman et al., 2004). Thus, the therapeutic workplace could reasonably be used as a short-term (e.g., six-month) or as a long-term intervention.
To determine if the therapeutic workplace can be a practical and economically viable intervention for patients who continue to use drugs during methadone treatment, the current analysis estimated the cost of implementing the therapeutic workplace in combination with methadone treatment. This combined cost could be useful to compare to the costs of alternative treatments that might be considered for patients who persist in using drugs despite exposure to standard methadone treatment, such as intensive outpatient or residential treatment.
The web-based therapeutic workplace has been in operation since April of 2000 at the Center for Learning and Health, a treatment-research unit in Baltimore, MD. In this report, we used the Drug Abuse Treatment Cost Analysis Program (DATCAP; French, Dunlap, Zarkin, McGeary, & McLellan, 1997) to estimate the economic costs of implementing phase 1 of the therapeutic workplace intervention. The costs of methadone treatment were based on data from previously published reports (Roebuck, French, & McLellan, 2003). Economic costs were estimated from the societal perspective, were presented as weekly costs per client, and were derived based on the operation of the therapeutic workplace intervention over the course of a full calendar year, from September 1, 2003 through August 31, 2004. All participants were enrolled in phase 1 of the therapeutic workplace intervention during this period.
2. Materials and Methods
2.1 Participants
During the time of this cost analysis, the therapeutic workplace served cocaine users who were also enrolled in community methadone treatment programs located in Baltimore city (n = 99), homeless alcohol-dependent adults (n = 22), and adults in the Baltimore city drug court system (n = 1). Fifty seven percent of participants were women, 88% were African-American, and 11% were White. Participants were between 23 and 58 years of age at the time of admission (mean of 45 years). All participants were enrolled in randomized controlled studies that were evaluating the therapeutic workplace as an intervention for drug or alcohol addiction. The Johns Hopkins University School of Medicine Institutional Review Board or the Western Institutional Review Board approved all studies and all participants signed informed consent prior to participation.
2.2 Therapeutic Workplace Overview
Detailed descriptions of the therapeutic workplace are provided elsewhere (Silverman et al., 2005; Silverman et al., in press). A brief description will be provided here. A web-based therapeutic workplace intervention was used that computerized most aspects of the intervention. The therapeutic workplace was open for training from 10:00 am to 12:00 pm and 1:00 pm to 3:00 pm every weekday, except for holidays and weather emergencies. Attendance and work hours were monitored with bar-coded picture IDs and electronic card readers. Throughout each workday, participants sat at workstations to work on the computerized typing, keypad and data entry training programs. Participants could earn a base hourly wage for hours worked and productivity pay for performance on the training programs. Earnings were rendered in the form of vouchers exchangeable for goods and services.
2.2.1 Urine collection, testing and feedback
Prior to entering the workroom on Mondays, Wednesdays, and Fridays, participants were required to provide a urine and breath sample under observation. Staff-observed urine collection was done using procedures designed to ensure specimen validity. Breath samples were collected with the AlcoSensor III to assess breath alcohol levels. Urine samples were tested using the Abbott AxSym® system (Abbott Laboratories, Abbott Park, IL) for opiates and cocaine. After the breath and urine samples were tested, results were shared with the participant. Because participants were enrolled in randomized controlled studies, some participants were required to provide drug-free urine samples or alcohol-free breath samples to gain access to the workroom, but some participants (who were enrolled in control groups) were not.
2.2.2 Typing, keypad and data entry training programs
The typing and keypad programs were designed to teach participants to copy characters using the alphanumeric keyboard and the number pad, respectively. Both programs were divided into small steps that participants could master sequentially. In both of the programs, participants practiced the skills taught on each step in one-minute timings. The mastery criteria for steps were specified in terms of the minimum correct and maximum incorrect characters per minute. Once a participant met the mastery criteria for a given step, the program advanced the participant to the next step. The data-entry training program was designed to teach participants how to enter data from a paper copy into the computerized data entry program. This program also consisted of steps that had to be mastered sequentially.
2.2.3 Voucher system
The voucher system was adapted from a system that was originally developed by Higgins and his colleagues (Higgins et al., 1991) for the treatment of primary cocaine dependent patients. Participants could use voucher earnings to purchase goods and services available in the community. When a participant accumulated enough voucher earnings, the participant could complete a purchase order to request a specific item. The staff member then purchased the item(s) from the community. Gift certificates and gift cards were kept on hand from popular vendors to reduce the costs associated with making individual purchases and to expedite the purchasing process for participants. Because participants were enrolled in randomized controlled studies, eight of the participants (6% of participants) did not earn vouchers.
2.2.4 Personnel
Direct care, supervisory, and administrative staff were required to implement the therapeutic workplace intervention. Direct care staff included the workroom assistants, laboratory assistants, and the voucher system assistants. Direct care staff had at least a high school degree, but individuals with college degrees performed most of the direct care activities. Workroom assistants introduced participants to the rules and benefits (e.g., how to earn vouchers and how much could be earned in vouchers) of the therapeutic workplace; recorded (by swiping their bar-coded IDs) participants as they entered and existed the workrooms; monitored and managed their professional behavior in the workplace; provided assistance with problems related to the web-based training programs; created remediation steps when there were problems with the training programs; and performed other tasks related to the daily conduct of the classroom environment. Laboratory assistants collected and tested urine specimens for drugs of abuse; collected breath samples for alcohol; maintained all supplies and equipment needed to operate the urinalysis laboratory; and entered all urinalysis and breath alcohol data into the therapeutic workplace software. The voucher system assistant collected voucher requests from participants, filled voucher requests (including shopping for special items and gift cards and writing/delivering checks for bill payments), implemented procedures to maintain funds in the voucher account, and implemented procedures to ensure the integrity of the voucher system (e.g., balancing the voucher account).
A therapeutic workplace manager had a master’s degree in behavior analysis and supervised all of the intervention activities in the therapeutic workplace. The therapeutic workplace manager hired and supervised the workroom and laboratory assistants, performed their routine evaluations, taught staff how to perform their jobs, ensured that procedures were being implemented properly, and addressed problems that the workroom or laboratory assistants did not know how to handle. The administrative assistant was responsible for purchasing supplies; processing all personnel and payroll paperwork within the Johns Hopkins University system for staff; and managing all contracts with non-university vendors. The Director supervised the therapeutic workplace manager and the administrative assistant, and was responsible for oversight of all of the intervention activities, particularly for addressing unique problems for which standard procedures were not available.
2.3 Cost Estimating Procedures
To estimate the economic cost of the therapeutic workplace intervention, the DATCAP was used. The DATCAP provides a consistent and valid method for assessing the economic costs of drug abuse treatment programs from a societal perspective (French et al., 1997). The DATCAP has been used to assess and compare costs of various types of drug abuse treatments (Roebuck et al., 2003). The procedures used to estimate costs in this analysis were similar to the procedures used in prior analyses.
First, information on client/participant caseloads and length of stay in the intervention program was assembled. The number of participants enrolled in the program was calculated for each day and then the mean number of participants per day was calculated (i.e., average daily census). As in prior cost analyses using the DATCAP (Roebuck et al., 2003), the estimate for the number of participants served in a year was based on the number of participants whose last day was during the period of this analysis (9/1/2003 and 8/31/2004). While not perfect, this method is necessary because individuals enroll in the program continually over time. Given this circumstance of rolling admissions and discharges, we considered two options to estimate the number of participants/clients served in a year. One option was to count the number of intakes within a 1-year time frame; the other was to count the number of participants/clients who ended services within a 1-year time frame. We opted for this latter method, because it is the approach that was used in prior analyses (Roebuck et al., 2003). For each of those participants, a length of stay in treatment from day of enrollment to last day attended was calculated. These values were used to determine the median length of stay in the program. The median was selected since there were a small number of individuals who dropped out early, a small number of individuals who dropped out across the weeks of the intervention period, and a majority of participants who remained in the intervention for the full duration, which produced a fairly skewed distribution. These numbers were used only for estimating total number of clients served in a year and estimating how long participants remained in the intervention.
Next, data quantifying resource use and costs in the delivery of the intervention were collected and separated into six categories: personnel, supplies and materials, contracted services, buildings and facilities, equipment, and miscellaneous resources. All resources employed in the delivery of the intervention were identified and valued based upon both their actual accounting cost, and the compensation they would have received in their highest and best use. The latter of these two types of costs, known as economic or opportunity costs, is preferred for economic evaluation purposes and is presented in this paper (French et al., 1997).
With the assistance of the project economist M. Christopher Roebuck (second author), the therapeutic workplace staff provided information on the use of resources during the year from 9/1/2003 through 8/31/2004. These calculations required some estimates of how much staff time was spent devoted to research and how much was spent devoted to the intervention aspects of the therapeutic workplace program. These estimates were used to determine what portion of each staff member’s salary would be considered in the calculation of intervention costs. These same percentages were used to allocate costs for office space. In addition to these costs, the University charged an indirect cost rate of 25% on all direct costs except for rent. Those indirect costs were also included in this analysis. Any costs incurred by the program during that year wholly attributable to research were excluded from this cost analysis.
We then estimated the total annual economic cost of the intervention program and the average cost per client per week. The total annual cost of the intervention program was simply the sum of all resources and costs incurred by the program during the sampled year. The average weekly cost per client was determined by dividing the total annual cost by the mean daily census and then dividing that result by 52.14 weeks.
3. Results
The therapeutic workplace served a total of 122 clients during the year between September 1, 2003 and August 31, 2004, and maintained a mean daily census of 48 clients enrolled. The number of clients enrolled (filled circles, Figure 1) and present (open circles, Figure 1) in the workplace varied across time. The median length of stay for the 122 clients was 22 weeks (Table 1). Overall, during this one-year period, the therapeutic workplace provided 21,482 hours of client service. To provide the therapeutic workplace for these participants, the following staffing efforts, reported in proportions of a full-time equivalent (FTE) position, were required: 0.25 FTE of the director, 0.48 FTE of the administrator, 0.60 FTE of the therapeutic workplace manager, 2.2 FTE of the workroom assistants, 0.30 of the voucher assistant, 1.20 FTE of the laboratory assistants.
Figure 1.
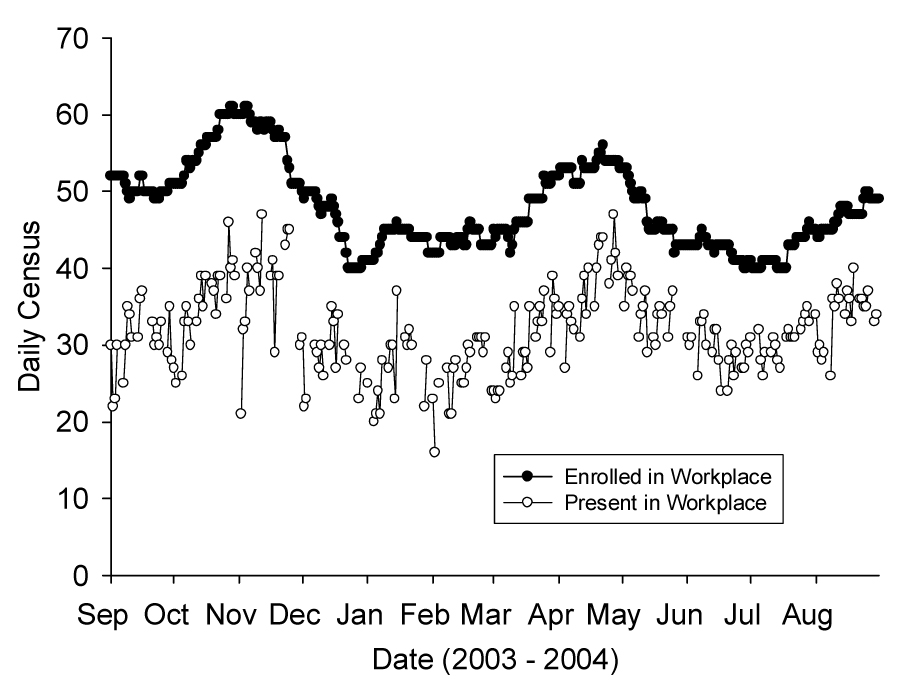
The daily census in the therapeutic workplace across consecutive workdays throughout the year of the cost analysis. Solid symbols represent the number of participants enrolled in the workplace; open symbols represent the number of participants that actually attended the workplace. Missing open symbols indicate days when the workplace was closed due to holidays or weather emergencies.
Table 1.
Key DATCAP Results of Therapeutic Workplace for the Year 9/1/2003 through 8/31/2004
| Measure | Result |
|---|---|
| Total Number of Clients | 122 |
| Mean Daily Census | 48 |
| Median Length of Stay (weeks) | 22.0 (mean, 22.4) |
| Total Annual Economic Costsa | $662,343 |
| Weekly Economic Cost per Clienta | $265 |
In 2004 dollars.
Different measures of cost were derived based on the above data. The total annual cost of the intervention program was $662,343 (Table 2). The mean cost per client per week was $265 dollars. The majority of intervention costs were personnel costs (35%), followed by client earnings (30%). Buildings and facilities, supplies and materials, and equipment were 16% of total intervention costs, and contracted services and miscellaneous costs were negligible (< 2%).
Table 2.
Distribution of Economic Costs of Therapeutic Workplace across Resource Categories for the Year 9/1/2003 through 8/31/2004
| Resource Category | Economic Costa (Percent of Total) |
|---|---|
| Personnel | $229,148 (35%) |
| Client Earnings | $201,309 (30%) |
| Buildings and Facilities | $49,734 (8%) |
| Supplies and Materials | $33,505 (5%) |
| Equipment | $19,475 (3%) |
| Contracted Services | $3,409 (1%) |
| Miscellaneous | $3,241 (< 1%) |
| University Indirect Costs | $122,522 (18%) |
| Total | $662,343 (100%) |
In 2004 dollars.
The controlled evaluations of the therapeutic workplace have been conducted in methadone maintenance patients who continued to use heroin and cocaine during standard methadone treatment. Thus, to date the therapeutic workplace has been used as an adjunct to methadone maintenance. In addition, most of the participants in the current analysis were enrolled in methadone maintenance in a community treatment program in Baltimore City while they attended the therapeutic workplace. To estimate the costs of the therapeutic workplace in combination with the costs of methadone treatment, we used costs of methadone treatment that were calculated by Roebuck et al. (2003). They used the DATCAP to estimate the costs of 11 different methadone maintenance treatment programs. That analysis showed that methadone maintenance costs on average $91 per week per client in 2001 dollars ($97 in 2004 dollars, the time period of the current study; U.S. Department Of Labor Bureau Of Labor Statistics, Consumer Price Indexes, 2007). Thus, the total cost of the therapeutic workplace intervention plus methadone maintenance treatment was $362 per week per client ($265 per week for therapeutic workplace plus $97 for methadone maintenance).
4. Discussion
This paper presents an estimate of the economic cost of providing the therapeutic workplace intervention in combination with methadone maintenance treatment. The analysis presented here shows that the weekly economic cost of implementing the therapeutic workplace intervention, including the costs of methadone maintenance treatment, is approximately $362 per client in 2004 dollars. In comparison, Roebuck et al. (2003)) estimated that intensive outpatient treatment costs $462 per week in 2001 dollars, which would be $492 per week in 2004 dollars; and residential treatment costs $700 per week in 2001 dollars, which would be $746 per week in 2004 dollars.
The therapeutic workplace intervention is unusual among the various alternative drug abuse treatments in that 30% of the cost is based on earnings that clients received for working. The treatment community has expressed some objection to the use of incentives in drug abuse treatment on the basis that they cost too much (Kirby, Benishek, Dugosh, & Kerwin, 2006). Yet, despite the use of relatively high magnitude voucher reinforcement (i.e., incentives) in the therapeutic workplace, the overall cost of the therapeutic workplace plus methadone maintenance is still within the range of other drug abuse treatment modalities that might be applied to address the needs of treatment-refractory methadone maintenance patients.
Participants in the current study were enrolled in the training phase (phase 1) of the therapeutic workplace. In this context, all aspects of the intervention, including the earnings, are appropriately considered costs. However, if the therapeutic workplace procedures were implemented in the context of an income producing business in which the participants earn wages for producing goods or services which are sold to customers (see Silverman et al., 2005), some of the costs could be offset by the income received by the business for those goods or services. In that context, from a societal perspective, costs like earnings might more appropriately be considered transfer payments.
Estimating the costs of the therapeutic workplace intervention in combination with methadone maintenance treatment is important in that it can help public and private social service agencies determine the extent to which that intervention might be implemented with available treatment funds. In addition, these cost estimates can be used in future cost-benefit and cost-effectiveness evaluations of this intervention. Finally, given that the cost of implementing the therapeutic workplace intervention with methadone maintenance is within the range of other drug abuse treatments, researchers interested in conducting research to develop and evaluate the therapeutic workplace might view the intervention as feasible and worthy of further investigation.
There were some limitations inherent in the analysis of economic costs conducted for the therapeutic workplace. Some expert judgment was necessary to estimate the amount of staff time that was devoted to intervention tasks relative to research tasks in calculating the costs of personnel for this program. Attempts were made to exclude things that were solely for research in order to produce the most accurate estimate of intervention costs possible. The judgments used to estimate the amount of time devoted exclusively to intervention tasks are imperfect and may have added some error into the cost estimates.
The findings presented in this report suggest that economic costs of the therapeutic workplace added to methadone maintenance are within the range of costs of other drug abuse treatment modalities. These cost data offer practical and policy-relevant information on the financial feasibility of offering the therapeutic workplace intervention as an ancillary service to patients who continue to use heroin and cocaine during standard methadone maintenance treatment.
Acknowledgements
Todd W. Knealing is now at the Department of Psychology, Briar Cliff University, Sioux City, Iowa. Conrad J. Wong is now at the Department of Behavioral Science, University of Kentucky, College of Medicine, Lexington, Kentucky.
This research was supported by research grants R01DA12564 and R01DA13107 from the National Institute on Drug Abuse and grant R01AA012154 from the National Institute on Alcohol Abuse and Alcoholism.
Corresponding author: Kenneth Silverman, PhD, Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, 5200 Eastern Avenue, Suite 142 West, Baltimore, MD, 21224, (email: ksilverm@jhmi.edu).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Cohen M, Bigelow G, Hargett A, Allen R, Halsted C. The use of contingency management procedures for the treatment of alcoholism in a work setting. Alcoholism. 1973;9:97–104. [Google Scholar]
- Crowley TJ. Doctor’s drug abuse reduced during contingency-contracting treatment. Alcohol and Drug Research. 1986;6:299–307. [PubMed] [Google Scholar]
- Dickinson K, Maynard R. The Impact Of Supported Work On Ex-Addicts. New York: Manpower Demonstration Research Corporation; 1981. [Google Scholar]
- French MT, Dunlap LJ, Zarkin GA, McGeary KA, McLellan AT. A structured instrument for estimating the economic cost of drug abuse treatment. The Drug Abuse Treatment Cost Analysis Program (DATCAP) Journal of Substance Abuse Treatment. 1997;14:445–455. doi: 10.1016/s0740-5472(97)00132-3. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Delaney DD, Budney AJ, Bickel WK, Hughes JR, Foerg F, et al. A behavioral approach to achieving initial cocaine abstinence. The American Journal of Psychiatry. 1991;148:1218–1224. doi: 10.1176/ajp.148.9.1218. [DOI] [PubMed] [Google Scholar]
- Hser YI, Anglin MD, Fletcher B. Comparative treatment effectiveness. effects of program modality and client drug dependence history on drug use reduction. Journal of substance abuse treatment. 1998;15:513–523. doi: 10.1016/s0740-5472(97)00308-5. [DOI] [PubMed] [Google Scholar]
- Kashner TM, Rosenheck R, Campinell AB, Suris A, Crandall R, Garfield NJ, et al. Impact of work therapy on health status among homeless, substance-dependent veterans: A randomized controlled trial. Archives of General Psychiatry. 2002;59:938–944. doi: 10.1001/archpsyc.59.10.938. [DOI] [PubMed] [Google Scholar]
- Kirby KC, Benishek LA, Dugosh KL, Kerwin ME. Substance abuse treatment providers' beliefs and objections regarding contingency management: Implications for dissemination. Drug and Alcohol Dependence. 2006;85:19–27. doi: 10.1016/j.drugalcdep.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Knealing TW, Wong CJ, Diemer KN, Hampton J, Silverman K. A randomized controlled trial of the therapeutic workplace for community methadone patients: A partial failure to engage. Experimental and Clinical Psychopharmacology. 2006;14:350–360. doi: 10.1037/1064-1297.14.3.350. [DOI] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Raczynski JM, Caldwell E, Engle M, Michael M, et al. Sufficient conditions for effective treatment of substance abusing homeless persons. Drug and Alcohol Dependence. 1996;43:39–47. doi: 10.1016/s0376-8716(96)01286-0. [DOI] [PubMed] [Google Scholar]
- Miller PM. A behavioral intervention program for chronic public drunkenness offenders. Archives of General Psychiatry. 1975;32:915–918. doi: 10.1001/archpsyc.1975.01760250107012. [DOI] [PubMed] [Google Scholar]
- National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction. Effective medical treatment of opiate addiction. The Journal of the American Medical Association. 1998;280:1936–1943. [PubMed] [Google Scholar]
- Roebuck MC, French MT, McLellan AT. DATStats: Results from 85 studies using the drug abuse treatment cost analysis program. Journal of Substance Abuse Treatment. 2003;25:51–57. doi: 10.1016/s0740-5472(03)00067-9. [DOI] [PubMed] [Google Scholar]
- Silverman K. Exploring the limits and utility of operant conditioning in the treatment of drug addiction. The Behavior Analyst. 2004;27:209. doi: 10.1007/BF03393181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Chutuape MA, Bigelow GE, Stitzer ML. Voucher-based reinforcement of cocaine abstinence in treatment-resistant methadone patients: Effects of reinforcement magnitude. Psychopharmacology. 1999;146:128–138. doi: 10.1007/s002130051098. [DOI] [PubMed] [Google Scholar]
- Silverman K, Higgins ST, Brooner RK, Montoya ID, Cone EJ, Schuster CR, et al. Sustained cocaine abstinence in methadone maintenance patients through voucher-based reinforcement therapy. Archives of General Psychiatry. 1996;53:409–415. doi: 10.1001/archpsyc.1996.01830050045007. [DOI] [PubMed] [Google Scholar]
- Silverman K, Kaminski BJ, Higgins ST, Brady JV. Behavior Analysis and treatment of drug addiction. In: Fisher WW, Piazza CC, Roane HS, editors. Handbook of Applied Behavior Analysis. New York, NY: Guilford Publication, Inc.; (in press) [Google Scholar]
- Silverman K, Needham MJ, Diemer KN, Knealing TW, Crone-Todd D, Fingerhood M, et al. A randomized trial of employment-based reinforcement of cocaine abstinence in injection drug users. Journal of Applied Behavior Analysis. doi: 10.1901/jaba.2007.40-387. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Robles E, Mudric T, Bigelow GE, Stitzer ML. A randomized trial of long-term reinforcement of cocaine abstinence in methadone-maintained patients who inject drugs. Journal of Consulting and Clinical Psychology. 2004;72:839–854. doi: 10.1037/0022-006X.72.5.839. [DOI] [PubMed] [Google Scholar]
- Silverman K, Svikis D, Robles E, Stitzer ML, Bigelow GE. A reinforcement-based therapeutic workplace for the treatment of drug abuse: Six-month abstinence outcomes. Experimental and Clinical Psychopharmacology. 2001;9:14–23. doi: 10.1037/1064-1297.9.1.14. [DOI] [PubMed] [Google Scholar]
- Silverman K, Svikis D, Wong CJ, Hampton J, Stitzer ML, Bigelow GE. A reinforcement-based therapeutic workplace for the treatment of drug abuse: Three-year abstinence outcomes. Experimental and Clinical Psychopharmacology. 2002;10:228–240. doi: 10.1037//1064-1297.10.3.228. [DOI] [PubMed] [Google Scholar]
- Silverman K, Wong CJ, Grabinski MJ, Hampton J, Sylvest CE, Dillon EM, et al. A web-based therapeutic workplace for the treatment of drug addiction and chronic unemployment. Behavior Modification. 2005;29:417–463. doi: 10.1177/0145445504272600. [DOI] [PubMed] [Google Scholar]
- Silverman K, Wong CJ, Umbricht-Schneiter A, Montoya ID, Schuster CR, Preston KL. Broad beneficial effects of cocaine abstinence reinforcement among methadone patients. Journal of Consulting and Clinical Psychology. 1998;66:811–824. doi: 10.1037//0022-006x.66.5.811. [DOI] [PubMed] [Google Scholar]


