Abstract
Purpose
To derive a regression equation that estimates metabolic equivalent (MET) from accelerometer counts, and to define thresholds of accelerometer counts that can be used to delineate sedentary, light, moderate, and vigorous activity in adolescent girls.
Methods
Seventy-four healthy 8th grade girls, age 13-14 yr, were recruited from urban areas of Baltimore, MD, Minneapolis/St. Paul, MN, and Columbia, SC, to participate in the study. Accelerometer and oxygen consumption (V̇O2) data for 10 activities that varied in intensity from sedentary (e.g., TV watching) to vigorous (e.g., running) were collected. While performing these activities, the girls wore two accelerometers, a heart rate monitor and a Cosmed K4b2 portable metabolic unit for measurement of V̇O2. A random-coefficients model was used to estimate the relationship between accelerometer counts and V̇O2. Activity thresholds were defined by minimizing the false positive and false negative classifications.
Results
The activities provided a wide range in V̇O2 (3-36 mL·kg-1·min-1) with a correspondingly wide range in accelerometer counts (1-3928 counts·30 s-1). The regression line for MET score versus counts was MET = 2.01 + 0.00171 (counts·30 s-1) (mixed model R2 = 0.84, SEE = 1.36). A threshold of 1500 counts·30 s-1 defined the lower end of the moderate intensity (∼4.6 METs) range of physical activity. That cutpoint distinguished between slow and brisk walking, and gave the lowest number of false positive and false negative classifications. The threshold ranges for sedentary, light, moderate, and vigorous physical activity were found to be 0-50, 51-1499, 1500 -2600, and >2600 counts·30 s-1, respectively.
Conclusion
The developed equation and these activity thresholds can be used for prediction of MET score from accelerometer counts and participation in various intensities of physical activity in adolescent girls.
Keywords: ACTIVITY MONITORS, ENERGY EXPENDITURE, PHYSICAL ACTIVITY ASSESSMENT, FITNESS, OXYGEN CONSUMPTION
There is considerable public health interest in the physical activity levels of children and adolescents in the United States, in part because there is an increased prevalence of obesity (16) and because obesity has been associated with lower physical activity (6). Research has documented low physical activity levels of adolescents (2), particularly in girls (8). Furthermore, a precipitous decline in physical activity levels in adolescent girls was recently reported with almost no physical activity reported by ages 18 and 19 yr (9). These concerns have sparked interest in interventions to improve physical activity in this age and gender group. The recently initiated Trial of Activity for Adolescent Girls (TAAG) is a multi-site school-and community-based intervention designed to prevent the decline in physical activity in adolescent girls. This paper reports on a preliminary study using girls from the catchment areas of three TAAG field centers to define accelerometer thresholds for physical activity.
Moderate-to-vigorous intensity physical activity (MVPA) levels result in positive health changes. For example, adolescent participation in activity has been shown to reduce the rate of increase in obesity (13), lower total cholesterol (13), lower circulating insulin levels (20), and slow the age-related increase in blood pressure (7). However, our present state of knowledge precludes good field methods for differentiating between intensity levels. The use of accelerometers or activity monitors has become a promising method to accomplish this goal. The Actigraph (Manufacturing Technologies Inc. Health Systems) accelerometer, previously called the CSA accelerometer, records activity counts in a given time interval, for example, half-minute or minute intervals. Calibrating an accelerometer against a “gold standard” measure of physical activity intensity, such as oxygen consumption (V̇O2), requires a controlled experiment by which V̇O2 and accelerometer counts are observed simultaneously over a range of activity intensities. A calibration curve relating V̇O2 to accelerometer counts can be fit to these data, and used subsequently for the estimation of metabolic equivalent (MET) score from accelerometer counts.
Laboratory-based studies have compared accelerometers to energy expenditure during physical activity in adults (5,15,26,27) and children (17,22,23). However, studies using V̇O2 as the criterion measure to establish cut-points of physical activity specifically in children are few (17). In 26 boys and girls 7-15 yr of age, Puyau et al. (17) reported an equation to predict energy expenditure from accelerometer counts, as well as intensity thresholds for two accelerometers (Actigraph and Actiwatch). Moderate activity ranged from 3200 to 8200 counts·min-1 for the Actigraph (17). No study has involved a large representative sample of middle-school girls.
In the present study, accelerometer counts were calibrated against measured energy expenditure (V̇O2) during a variety of activities. A regression equation to estimate MET (metabolic equivalent) values from accelerometer counts was created. The purpose of the study was to then generate the cut-points defining sedentary, light, moderate, and vigorous activity using accelerometer counts.
METHODS
Participants
In the spring of 2001, 74 healthy 8th grade girls, ages 13-14 yr, were recruited from urban areas of Baltimore, MD, Minneapolis/St. Paul, MN, and Columbia, SC. A sample was recruited that was diverse in terms of height, weight, race, and history of sport participation. None of the participants had physical limitations. The protocol was approved by each participating institution’s Human Subjects Review Board. Consent to participate was obtained from one parent, and assent was obtained from each participant.
Instrumentation
Age and ethnicity were obtained from the participant by questionnaire. Following a standardized protocol, the participant’s weight was measured twice to the nearest 0.1 kg on an electronic scale (Seca, Model 770, Hamburg, Germany). Height was measured twice to the nearest 0.1 cm using a portable stadiometer (Shorr Height Measuring Board, Olney, MD). The average of the two measures was used.
Oxygen consumption (V̇O2) and heart rate were measured using a portable, breath-by-breath, metabolic unit available from Cosmed (Model K4b2, Rome, Italy). The K4b2 is a lightweight (925 g) system that can be worn on the back. The unit includes a POLAR Pacer heart rate transmitter (Pt. Washington, NY). The calibration of the Cosmed followed standard procedures across all sites. The Cosmed unit was calibrated with standard gases before each visit and recalibrated with gases for the biking outside (an activity described below). The system has been previously validated (11).
All Actigraph (Manufacturing Technologies Inc. Health Systems, Model 7164, Shalimar, FL) accelerometers were checked at the Coordinating Center for similarity of basic functional condition using a standard laboratory shaker before being sent to each field site for subsequent use in this study. The test consisted of shaking the accelerometers secured on a mechanical shaker for 15 min at a low speed (similar to a walk) and 15 min at a high speed (similar to a slow jog). The variation between all units was less than 10%, which is within the limits of acceptability by the manufacturer. Each participant wore two accelerometers, one over each hip. Analysis of the data comparing the right versus the left hip yielded very similar results. All pairwise correlations between predicted METs from accelerometry using counts from the right hip, left hip, and the average of the two were 1.0. Therefore, all accelerometer values used for the analysis were the mean of right and left hip accelerometer counts. The monitors were attached to a belt worn around the waist. For each visit, the monitors were initialized before the first activity, and data were uploaded from the monitor to a PC after performance of all activities was complete. Activity counts were stored in 30-s time intervals. The 30-s epoch was chosen because children tend to do activities in short bursts and more sporadic than adults.
Study design
Participants attended two visits to obtain accelerometer and V̇O2 data for all 10 activities (Table 1). The selected activities were chosen to provide varied intensity from sedentary to vigorous and to reflect typical activities performed by middle school girls. Each participant completed both visits within a 2-wk time frame. Participants were required to fast for 3 h before each visit. At the first visit, participants were given an overview of the physical activity assessments, followed by height and weight measurement. The participant was then fitted with two Actigraph monitors and the Cosmed system and given an opportunity to become familiar with breathing through the mask. Once the prescribed activities and measurements began, accelerometer counts, heart rate, and V̇O2 were recorded simultaneously on a 30-s basis during the entire 7 min of each activity. Rest periods between activities were allowed as necessary to ensure that heart rate was below 100bpm before beginning the next activity.
TABLE 1.
Study description of activities
| Activity | Description |
|---|---|
| Rest | Lie on bed, still, awake, quiet environment |
| Watch TV | Sit in chair, watch movie video (e.g., comedy) |
| Play computer game | Sit in chair, play Chip’s Challenge game on PC |
| Sweep floor | Sweep confetti on floor continuously using broom to a specified location and repeating |
| Slow walk | Walk at 2.5 mph., participant’s pace kept close to that speed with the guidance of timed distances |
| Brisk walk | Walk at 3.5 mph., participant’s pace kept close to that speed with the guidance of timed distances |
| Step aerobics | Step aerobics video, both arm and leg movements, 1 step bench, first practice and instruction from staff before actual measurement, all exercised to the same 7 min of video |
| Bicycling | Ride bicycle outside at 12 mph, cyclometer on bike used to monitor speed, no steep hills, relatively flat |
| Shoot baskets | Shooting the basketball and retrieving the basketball continuously, using girls’ size basketballs |
| Stair walk | Climb stairs in a staircase at 80 steps·min-1 to music tape, without holding the rail except for balance |
| Run | Run at 5.0 mph on track or marked area, paced by staff with the guidance of timed distances |
Activities
Table 1 provides a brief description of the activities assessed. Resting V̇O2 was collected for 15 min in a dimly lighted, quiet room, with the participant in a reclined position. Participants were not allowed to sleep and several minutes of rest were provided before metabolic measurement occurred. Minutes 3-15 were then used for data analysis. Activities were completed in ascending intensities, starting with rest and ending with running. Sites were allowed to vary which activities took place during each visit, as long as the intensity of the activity was ascending. The protocol for visit 1 generally included assessments of rest, watching television, playing computer games, a slow walk, and a stair walk at a specified pace (see Table 1). Activities completed during the second visit generally included sweeping the floor, a brisk walk, step aerobics, shooting baskets with a basketball, and running. The biking activity took place at the end of either the first or second visit. For two activities (watching television and playing the computer game), the participant was seated in a chair. All other activities were in the upright standing position (except bicycling) and were set at specific paces. For all activities other than rest, V̇O2, heart rate and accelerometer counts were collected for 7 min, with the mean value of the last 4-7 min used for data analysis. Participants were considered to be at steady-state energy expenditure during this time (28). In order to standardize the activity (pace and movement), when-ever possible a staff member completed the activity along with the participant. The walking/running speeds for the participants were defined using paces set between marked distances with verbal guidance used to cue the participant to speed up or slow down as needed. For bicycling, a speedometer was used to monitor pace. Data collection was monitored continuously throughout all activities by trained staff. The staff recorded the exact time of the measurements, as well as marking the event button on the Cosmed unit.
The Physical Work Capacity test (PWC170) involved a standardized protocol (18) on a cycle ergometer (Monark, Model 818E, Varberg, Sweden). The test measures fitness, so that we could include in our sample participants within a wide range of fitness levels. This was generally completed on the first visit. The participants completed at least two 3-min stages during which V̇O2 was measured continuously and recorded every 30 s. Cadence was set to a metronome at 60 cycles·min-1. The initial cycling workload was based upon the participant’s weight and subsequent workloads were determined by the heart rate at the end of the stage according to the established PWC170 protocol. Heart rate was recorded during the last 10 s of each minute for each 3-min stage. The test was terminated when the heart rate reached 165 bpm or greater. From the results of the PWC, maximal aerobic power (V̇O2max) was predicted using the methodology outlined by McMurray et al. (12) and Mocellin et al. (14). This information was also used to interpret the intensities of each activity (%V̇O2max) for classification of low, moderate, and high intensity activity.
Statistical analysis
Because resting V̇O2 of youth is higher than adults (21), MET values were first computed based on the girl’s actual resting V̇O2 rather than the standard adult MET (3.5 mL·kg-1·min-1). These MET values were then used for further analyses. A random-coefficients model was used to characterize the relationship between accelerometer counts and V̇O2 over a range of activity intensities, while accounting for the dependence among repeated measurements taken on the same girl (10,19). Letting yij denote the response for the jth observation on the ith participant, the model can be written as
| [1] |
where α and β are fixed effects that denote the population average intercept and slope, and ai and bi represent each participant’s random intercept and slope deviations about the corresponding population parameters. Restricted maximum likelihood estimates of random effects and maximum likelihood estimates of fixed effects were obtained using the MIXED procedure in SAS Version 8.2 (SAS, Cary, NC). Coefficients associated with quadratic and cubic trends (γ, λ) in third-order polynomial model, yij = α + βxij + γ χ2ij +λχ3ij + ai + biχij + eij, were not found to be significantly different from zero. Similarly, age, body mass index, and race were not found to contribute significantly to the fit of the model. Thus, only results from the unadjusted linear mixed model are reported here.
A range of Actigraph counts were considered as candidate cut-points for defining intensity levels. The method of selecting an optimal cut-point was based on two criteria: 1) correct identification of the target or higher intensity activities (i.e., sensitivity); and 2) correct exclusion of lower intensity activities (i.e., specificity).
Three approaches were compared for their potential in choosing the lower threshold for moderate intensity physical activity. Approach 1 defined low intensity activities as watching TV, playing a computer game, sweeping the floor, and slow walking, and moderate or higher intensity activities as brisk walking, stair walking, shooting baskets, step aerobics, and running. Counts observed for low intensity activities that exceeded a given threshold were classified as false positives, and counts observed for moderate or higher intensity activities that fell below the same threshold were classified as false negatives. Thus, a false positive was an observation that did not represent moderate activity but was interpreted as moderate activity, and a false negative was an observation known to represent moderate activity that was interpreted as less than moderate activity. Thresholds between 1100 and 1600 counts·30 s-1 were examined. Bicycling was excluded from the analysis due to the poor correlation between accelerometer counts and V̇O2 during bicycling. Approach 2 was identical to approach 1, but step aerobics was also excluded from the analysis, also due to the poor correlation between accelerometer counts and V̇O2. Approach 3 focused only on slow and brisk walk as indicators of low and moderate intensity activities, respectively, based upon the literature defining brisk walking as a moderate activity (24). A bootstrap validation procedure (3) was used to assess the degree to which the cut-points would be expected to apply to a new sample of adolescent girls. One hundred bootstrap samples, each half the size as the original sample, were generated by drawing observations at random and with replacement from the original sample. The rate of misclassification (false positive and false negatives) was determined for all bootstrap random samples, and 5th and 95th percentile is reported.
The approaches were evaluated by examining the number of activity observations classified as false positive and false negative. The optimal threshold was the cut-point that both balanced and minimized the number of false positives and false negatives.
Based upon our experience in determining the moderate activity threshold using the Actigraph accelerometer, the cut-points for the other intensity levels were established in the same manner. To choose the upper threshold for light activity, counts observed for playing computer games (i.e., sedentary activity <1.5 METs) that exceeded a given threshold were classified as false positives, and counts observed for slow walking (i.e., light activity 3 METs) that fell below the threshold were classified as false negatives. To define the lower threshold of vigorous activity, counts observed for brisk walking (i.e., moderate activity 3.8 METs) above a given threshold were classified as false positives, and counts for running (i.e., vigorous activity 6 METs) below the threshold were classified as false negatives. As with the moderate threshold, the optimal thresholds for the other intensities were the cut-points that both balanced and minimized the number of false positives and false negatives.
RESULTS
Participant characteristics
The participant characteristics are provided in Table 2. Thirty-three Caucasians, 27 African-Americans, 4 Asians, and 10 multi-racial girls participated in the study. There was a wide range in BMI (14-40 kg·m-2) by design. As well, the predicted V̇O2max values from the PWC-170 test reflect a very wide range in fitness, from low fitness (18.5 mL·kg-1·min-1) to high fitness (65.8 mL·kg-1·min-1) levels.
TABLE 2.
Subject characteristics (N = 74)
| Mean (SD) | Range | |
|---|---|---|
| Age (yr) | 14.1 (0.3) | 13.4-15.4 |
| Weight (kg) | 60 (15.5) | 35-102 |
| Height (cm) | 160 (6.6) | 146-177 |
| BMI (kg·m-2) | 23.4 (5.8) | 14.4-40.0 |
| V̇O2max predicted (mL·kg-1·min-1) | 38.5(9.9) | 18.5-65.8 |
Accelerometer counts and MET scores
Table 3 includes the V̇O2, MET score and accelerometer counts, expressed both in half minutes (counts·30 s-1) and minutes (counts·min-1) for each activity. All accelerometer counts are presented as the mean of the right and left hip accelerometer counts. The activities are shown in increasing value of V̇O2 and MET scores, with the lowest values for watching TV and computer games, and the highest values for walking the stairs and running. The chosen physical activities provided a wide range in MET scores (1-7.8) with a correspondingly wide range in accelerometer counts (1-3928 counts·30 s-1or 1-7867 counts·min-1). The accelerometer values for bicycling (369 counts·30 s-1) and step aerobics (1371 counts·30 s-1) were considerably lower than what would be expected from the V̇O2 values. For each activity, the counts per minute were not exactly twice the counts per 30 seconds because two sequential 30-s periods do not always have identical counts.
TABLE 3.
V̇02, MET score, and accelerometer counts for each activity
| V̇O2 (mL·kg-1 min-1) |
MET Score* |
Accelerometer Count·30 s-1 |
Accelerometer Count·min-1 |
|||
|---|---|---|---|---|---|---|
| Activity | N | Mean (SD) | % of V̇O2max | Mean (SD) | Mean (SD) | Mean (SD) |
| 1. Rest | 64 | 3.8 (0.9) | 0 (0.7) | |||
| 2. Watch TV | 67 | 3.9 (0.9) | 11 | 1.0 (0.1) | 1 (1.7) | 2 (4.6) |
| 3. Play computer game | 71 | 4.2 (2.0) | 11 | 1.1 (0.5) | 1 (3.2) | 2 (6.4) |
| 4. Sweep floor | 72 | 11.0 (2.2) | 30 | 3.0 (0.6) | 203 (173) | 400 (339) |
| 5. Slow walk | 72 | 11.8 (2.5) | 32 | 3.2 (0.8) | 1180 (280) | 2356 (537) |
| 6. Brisk walk | 73 | 15.6 (2.3) | 43 | 4.3 (1.0) | 2085 (379) | 4160 (748) |
| 7. Step aerobics | 71 | 21.2 (3.8) | 57 | 5.7 (1.4) | 1371 (457) | 2750 (916) |
| 8. Bicycling | 66 | 21.3 (7.6) | 59 | 5.9 (2.3) | 369 (297) | 741 (594) |
| 9. Shoot baskets | 69 | 24.3 (4.8) | 67 | 6.5 (1.6) | 2002 (584) | 4005 (211) |
| 10. Stair walk | 72 | 24.6 (3.7) | 68 | 6.6 (1.4) | 2138 (393) | 4271 (788) |
| 11. Run | 65 | 29.5 (5.0) | 79 | 7.8 (2.2) | 3928 (170) | 7867 (375) |
MET score = (Activity V̇O2 mL·kg-1 min-1)/(Individual Resting V̇O2 mL·kg-1 min-1).
All accelerometer (Actigraph) values are the mean of right and left hip accelerometer counts; counts per 30 seconds are not necessarily half of the counts per minute because consecutive 30-s periods do not always have identical counts.
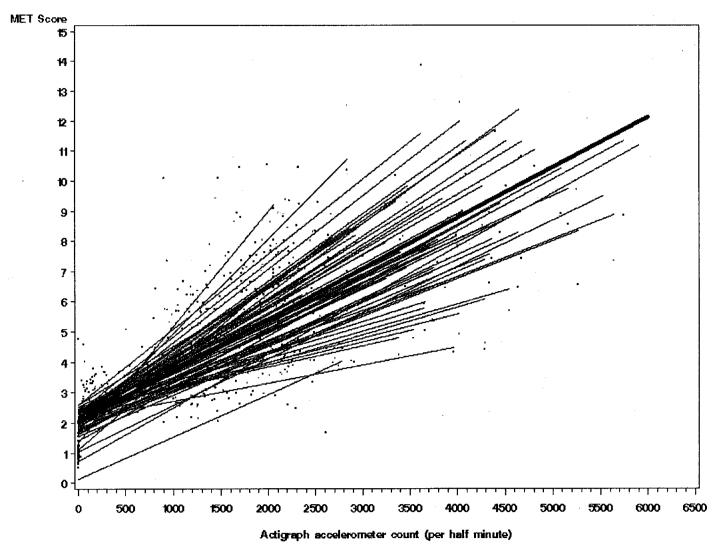
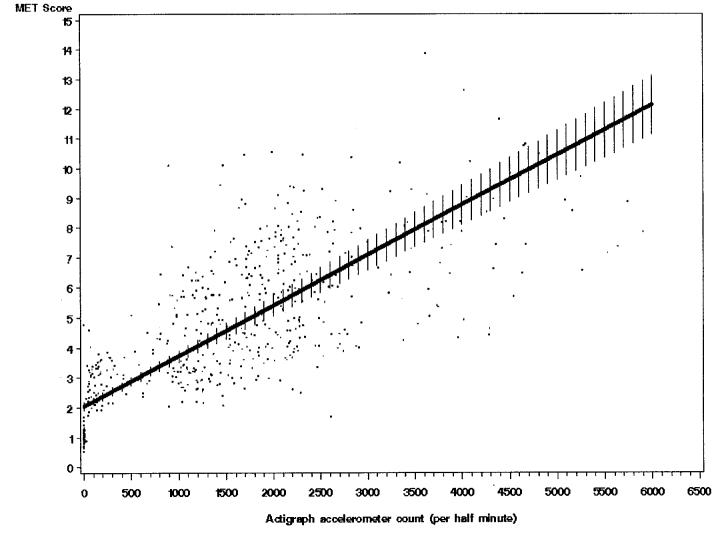
Figure 1 shows the regression lines for MET score versus accelerometer counts for each girl (thin lines) and the over-all regression line (heavy line). Figure 2 illustrates the regression line and 95% CI for the same analysis. Formula (1) estimates MET score using counts. As noted earlier, the results were similar when the data were analyzed separately for the left and right hip accelerometers. Using the left side, MET = 1.98 + 0.00175 (counts·30 s-1), and using the right side, MET = 2.10 + 0.00165 (counts·30 s-1).
| [2] |
FIGURE 1.
Regression line for MET score versus accelerometer (Actigraph) counts (random regression line for each girl and overall regression line).
FIGURE 2.
Regression line and 95% CI for MET score versus accelerometer counts.
The mixed model concordance correlation coefficient (25), corresponding to an R2 in standard linear regression, was 0.84 (SEE = 1.36).
Threshold for moderate intensity physical activity
Examination of thresholds from 1100 to 1600 counts·30 s-1 for approach 1 (excluding bicycling) gave high false positives and high false negatives (data not shown). By excluding step aerobics and bicycling (approach 2), the number of false positives and false negatives was lower than by excluding bicycling alone (Table 4); even so, approach 2 still gave high false positives (3-43) and high false negatives (6-32). Approach 3, which distinguished between slow and brisk walking, gave the lowest and most similar number of false positives and false negatives (Table 5). Under Approach 3, the number of false positives was similar to the number of false negatives for the 1470-1580 counts·30 s-1 accelerometer range (four to six false positives and three to eight false negatives). At the mid-point of this range (i.e., 1530 counts), there were five false positives and four false negatives. At a count of 1500, six false positives and three false negatives and the lowest total number of classification errors occurred. Therefore, a threshold of 1500 counts·30 s-1 was accepted as the lower end of the moderate intensity range of physical activity, using approach 3.
TABLE 4.
Choosing the threshold for moderate-to-vigorous intensity physical activity by examining the false positives and false negatives based for approach 2 (eight activities)
| Accelerometer (counts·30 s-1) | True Positive (N) | True Negative (N) | False Positive (N)* | False Negative (N)** | Error Rate (%) | Validation Error Rate (%)*** (5th, 95th Percentile) |
|---|---|---|---|---|---|---|
| 1100 | 239 | 273 | 43 | 6 | 8.7 | 6.4,11.4 |
| 1150 | 242 | 273 | 40 | 6 | 8.2 | 5.9,10.3 |
| 1200 | 252 | 270 | 30 | 9 | 7.0 | 4.6, 8.9 |
| 1250 | 259 | 270 | 23 | 9 | 5.7 | 3.5, 7.5 |
| 1300 | 263 | 269 | 19 | 10 | 5.2 | 3.4, 7.0 |
| 1350 | 268 | 267 | 14 | 12 | 4.6 | 2.9, 6.7 |
| 1400 | 269 | 266 | 13 | 13 | 4.6 | 3.0, 6.7 |
| 1450 | 274 | 261 | 8 | 18 | 4.6 | 3.0, 6.6 |
| 1500 | 276 | 258 | 6 | 21 | 4.8 | 2.8, 6.5 |
| 1550 | 277 | 250 | 5 | 29 | 6.1 | 4.1, 7.9 |
| 1600 | 279 | 247 | 3 | 32 | 6.2 | 3.9, 8.2 |
Counts measured under the protocols for watching TV, playing a computer game, sweeping the floor, and slow walking that were above the threshold for moderate intensity activity were considered as false positives.
Counts measured under the protocols for brisk walk, stair walk, shoot baskets, and run that were below the threshold for moderate intensity activity were considered as false negative (exclude step aerobics and bicycling).
Based on 100 bootstrap samples, each half the size as the original sample.
TABLE 5.
Choosing the threshold for moderate-to-vigorous intensity physical activity by examining the false positives and false negatives based for approach 3 (slow and brisk walking)
| Accelerometer (counts·30 s-1) | True Positive (N) | True Negative (N) | False Positive (N)* | False Negative (N)** | Error Rate (%) | Validation Error Rate (%)*** (5th, 95th Percentile) |
|---|---|---|---|---|---|---|
| 1100 | 29 | 73 | 43 | 0 | 29.7 | 21.7,37.4 |
| 1150 | 32 | 73 | 40 | 0 | 27.6 | 19.8,34.9 |
| 1200 | 42 | 72 | 30 | 1 | 21.4 | 14.2,28.2 |
| 1250 | 49 | 72 | 23 | 1 | 16.6 | 9.6,22.0 |
| 1300 | 53 | 72 | 19 | 1 | 13.8 | 7.9,19.8 |
| 1350 | 58 | 72 | 14 | 1 | 10.3 | 6.0,16.7 |
| 1400 | 59 | 72 | 13 | 1 | 9.7 | 5.6,13.9 |
| 1450 | 64 | 71 | 8 | 2 | 6.9 | 3.5,11.5 |
| 1500 | 66 | 70 | 6 | 3 | 6.2 | 2.5, 9.4 |
| 1550 | 67 | 65 | 5 | 8 | 9.0 | 4.0,13.8 |
| 1600 | 69 | 65 | 3 | 8 | 7.6 | 2.7,12.5 |
Counts measured under the protocol for slow walk that were above the threshold for moderate intensity activity were considered as false positive.
Counts measured under the protocol for brisk walk that were below the threshold for moderate intensity activity were considered as false negative.
Based on 100 bootstrap samples, each half the size as the original sample.
Thresholds for sedentary, light, and vigorous intensity physical activity
The summary of threshold counts for sedentary, light, moderate, and vigorous physical activity for the accelerometer is presented in Table 6. Thresholds for data collection periods of both 30-s intervals and 1-min intervals are shown. A lower threshold for light activity of 50 counts·30 s-1 resulted in no false positives and false negatives. By default, counts below 50 were defined as sedentary. The optimal lower threshold for vigorous physical activity (and the upper limit moderate activity) was observed at a threshold of 2600 counts·30 s-1, with only eight brisk walking observations above the threshold (false positives) and nine running observations below the threshold (false negatives).
TABLE 6.
Summary of intensity threshold counts for sedentary, light, moderate, and vigorous physical activity (PA) for the Actigraph accelerometer
| Activity Level | Accelerometer (counts·30 s-1) | Accelerometer (counts·min-1) |
|---|---|---|
| Sedentary PA | <50 | <100 |
| Light PA | 51-1499 | 101-2999 |
| Moderate PA | 1500-2600 | 3000-5200 |
| Vigorous PA | >2600 | >5200 |
DISCUSSION
In this study, we developed a regression equation to predict MET score from the accelerometer counts. The model fit was good, as evidenced by a mixed model equivalent to R2 for linear regression of 0.84, even so, the large standard error of ±1.36 METs might suggest that the equation be used only as a gross estimate of energy expenditure. The use of the MET score for the prediction is a unique approach as previous papers typically use caloric expenditure in kilocalories (5,17). The use of MET values also allows for the use of the Compendium of Physical Activity to estimate energy expenditure over a large range of activities (1). Our equation will be useful to others interested in predicting a MET score with their own accelerometer data. It has already been useful in defining moderate-to-vigorous physical activity for the main trial data from TAAG. As well, this equation can be used in reducing the accelerometer data collected in TAAG.
There is relatively little other research using accelerometry to predict energy expenditure in children. In one study (17), activity energy expenditure was predicted from Actigraph accelerometer counts using controlled laboratory conditions in a room calorimeter as well as free-living field activities. Both boys and girls of varying ages participated and a high correlation was found (R2adj = 0.75). In adults, other laboratory-based studies have compared accelerometers to energy expenditure during physical activity (5,15,26,27). Freedson et al. (5) predicted energy expenditure (kcal·min-1) measured in adults while walking at different speeds on the treadmill from Actigraph counts and BMI, reporting an R2 of 0.82. In two studies of adults by Welk et al. (26,27), validation coefficients between several accelerometers (Actigraph, Biotrainer, and Actitrac) with energy expenditure measured under treadmill and field conditions were also moderate to high (range r = 0.62-0.91). Thus, our equation to estimate MET levels from accelerometer counts in adolescent girls appears comparable to previous reports in children and adults.
In order to define our activity thresholds appropriately, we utilized the V̇O2 values above each girl’s own resting metabolic rate. One MET is defined as 3.5 mL·kg-1·min-1 for adults (1), and in our study, this value was slightly higher (3.8 ± 0.9 mL·kg-1·min-1). Utilizing the adult value for 1 MET might have biased the estimated energy cost of the physical activities measured in these adolescent girls. Thus, we chose to use the participants’ actual resting values to estimate MET levels.
Our three different approaches for determining our thresholds identified activities that were falsely classified. In approach 1 where bicycling was excluded, counts for watching TV, playing a computer game, sweeping the floor, and slow walking that were above the threshold were classifiedas false positive for moderate intensity activity, and counts for brisk walking, stair walking, shooting baskets, and running below the same threshold were classified as false negative. There were high numbers of false negatives, mostly related to step aerobics. This may have been expected since the accelerometer senses a walk (or step), but the participant had to lift her weight up a 6-inch step each step; thus, metabolic rate would be increased above walking. In approach 2, step aerobics and bicycling were both removed from the analysis. The numbers of false positives and false negatives were lower than excluding bicycling alone. This suggests that the accelerometer does not respond appropriately during activities in which body motion is somewhat independent of exercise intensity. Approach 3 had the lowest number of false positive and false negative classifications. This approach used differences between a slow and brisk walk to identify thresholds. Brisk walking has previously been categorized as a moderate activity (24). In particular, the recent guidelines for meeting the minimum level of physical activity levels use brisk walking as an example of a moderate activity for individuals (2,4). Thus, although we tested many activities with a wide range of intensities, a potentially limiting factor in the study is that we relied on differentiating between two walking speeds to determine our moderate threshold.
We experienced some difficulties using the accelerometer to establish the thresholds for light and vigorous activity. In our attempt to define a vigorous threshold, we designed the study to include activities that would be at an intensity > 6 METs. Previous literature has defined 6 METs as vigorous (24). As shown in Table 3, shooting baskets and the stair walking yielded MET values greater than 6 METs, but the activity counts were very low. As adolescents perform activities in variable ways, it is evident that the accelerometer does not work well in evaluating the intensity of such activities. Perhaps accelerometers attached to the waist lack in their ability to account for upper extremity work. It is also possible that the accelerometers might detect movement when in fact the adolescent was sedentary (e.g., car/bus travel). This could have influenced the number of false negatives for the sedentary threshold. Thus, accelerometers are limited in their ability to estimate activity levels or metabolic rates during cycling, step aerobics, stair stepping, or other similar activities where the accelerometer counts are less accurate.
One study (17) evaluated similar cut-points in children using the Actigraph accelerometer during treadmill walking/running and jogging outside at their own speed. A slightly higher value for the lower threshold for moderate activity was reported (<3200 counts·min-1). This corresponded to <0.05 kcal·kg-1·min-1 (17). Their reported threshold for vigorous activity was >8200 counts, with sedentary defined as <800 counts·min-1. Our values were lower and may be due to the types and intensities of activities chosen to determine these thresholds. For example, vigorous activity included treadmill walking (that specifically controlled speed and step rate) and jogging on a track (17), whereas we did not use a treadmill. Greater variability would be expected with our run at 5 mph (8 kph). Our participants had to follow a set pace and were verbally encouraged to either speed up or slow down if the pace deviated.
Because we evaluated the fitness levels of the participants using a cycle ergometer test (PWC170), we were able to verify how our chosen thresholds relate to V̇O2max. Moderate physical activity should correspond to 40-60% of V̇O2max. In these participants with a predicted average V̇O2max of ∼39 mL·kg-1·min-1, 40-60% would be equivalent to 16 -23 mL·kg-1·min-1. The measured V̇O2 values for the slow walk in our study are below this range whereas the value for brisk walking (4.3 METs and V̇O2 = 15.6 mL·kg-1·min-1) was at the low end for the range of 40 - 60% V̇O2max. Thus using slow and brisk walking as activities to separate light from moderate activity to define our activity thresholds appears to be appropriate. We can also compare our chosen activities and measured V̇O2 to a percentage of this estimated V̇O2max. The 11 chosen activitierange from 11% to 79% of predicted V̇O2max. Thus, we can be confident that our prediction equation for MET score was developed from the entire range of exercise intensities. One limitation of our prediction is that these values were predicted from cycle ergometry, which is lower than what would be predicted from treadmill walking. Nevertheless, we did include a wide range of exercise intensities into the design of the study.
One unique component of this study was the setting of the accelerometers to collect activity counts in 30-s intervals. Children’s activities tend to be spontaneous, sporadic, and done in shorter intervals. Our rationale for this shorter data collection interval was that sensitivity might be increased and the activities might be better detected with the 30 s rather than 1 min collection time. We presented the data also in counts per minute for our thresholds, as this has been the standard in the literature (5,17).
Based on our study, a prediction equation for estimating MET score from accelerometer counts is now available for use in adolescent girls. The accelerometer thresholds to define girls’ physical activity levels can also be used to determine the amount of sedentary, light, moderate, and vigorous physical activity. This type of determination is useful for surveillance research or to determine the effects of physical activity interventions designed to promote activity.
Acknowledgments
We would like to thank the girls who participated in the study, the project coordinators for participant recruitment, and the members of the TAAG Steering Committee, including: Russell Pate, Ph.D., University of South Carolina; Deborah Rohm-Young, Ph.D., University of Maryland College Park; Leslie Lytle, Ph.D., University of Minnesota; Timothy Lohman, Ph.D., University of Arizona; Larry Webber, Ph.D., Tulane University; John Elder, Ph.D., San Diego State University; June Stevens, Ph.D., The University of North Carolina at Chapel Hill; and Charlotte Pratt, Ph.D., National Heart, Lung, and Blood Institute.
This research was funded by grants from the National Heart, Lung, and Blood Institute (U01HL66858, U01HL66857, U01HL66845, U01HL66856, U01HL66855, U01HL66853, U01HL66852).
REFERENCES
- 1.Ainsworth BE, Haskell WL, Whitt MC, et al. Compen- dium of physical activity: an update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000;32:S498–S516. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Guidelines for school and community programs to promote lifelong physical activity among young people. MMWR. 1997;46(No RR6):1–36. [PubMed] [Google Scholar]
- 3.Efron B, Tibshirani R. An Introduction to the Bootstrap. Chapman and Hall; New York: 1993. [Google Scholar]
- 4.Food and Nutrition Board (FNB) and the Institute of Medicine (IOM) Dietary Reference Intakes for Energy, Carbo- hydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) The National Acade- mies Press and Joseph Henry Press; Washington, DC: 2002. Energy; pp. 93–206. [Google Scholar]
- 5.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Gazzaniga JM, Burns TL. Relationship between diet composition and body fatness, with adjustments for resting energy expenditure and physical activity, in preadolescent children. Am. J. Clin. Nutr. 1993;58:21–28. doi: 10.1093/ajcn/58.1.21. [DOI] [PubMed] [Google Scholar]
- 7.Harrell JS, McMurray RG, Gansky SA, Bangdiwala SI, Frauman AC, Bradley CB. Public health versus a risk based intervention to improve cardiovascular health in elementary school children: the cardiovascular health in children study. Am. J. Pub. Health. 1999;89:1529–1536. doi: 10.2105/ajph.89.10.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kimm SYS, Glynn NW, Kriska AA, et al. Longitudinal changes in physical activity in a biracial cohort during adolescence. Med. Sci. Sports Exerc. 2000;32:1445–1454. doi: 10.1097/00005768-200008000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Kimm SYS, Glynn NW, Kriska AM, et al. Decline in physical activity in black girls and white girls during adolescence. N. Engl. J. Med. 2002;347:709–715. doi: 10.1056/NEJMoa003277. [DOI] [PubMed] [Google Scholar]
- 10.Littell RC, Milliken GA, Stroup WW, WolfinGer RD. SAS System for MIXED Models. SAS Institute, Inc; Cary, NC: 1996. pp. 253–255. [Google Scholar]
- 11.McLaughlin JG, King GA, Howley ET, Bassett DR, Ainsworth BA. Validation of the Cosmed K4b2 portable metabolic system. Int J. Sports Med. 2001;22:280–284. doi: 10.1055/s-2001-13816. [DOI] [PubMed] [Google Scholar]
- 12.McMurray RG, Guion WK, Ainsworth BE, Harrell JS. Predicting aerobic power in children. J. Sports Med. Phys. Fitness. 1998;38:227–233. [PubMed] [Google Scholar]
- 13.McMurray RG, Harrell JS, Bangdiwala SI, BradLey CB, Deng S, Levine A. A school-based intervention can reduce body fat and blood pressure in young adolescents. J. Adolesc. Health. 2002;31:125–132. doi: 10.1016/s1054-139x(02)00348-8. [DOI] [PubMed] [Google Scholar]
- 14.Mocellin R, Lindermann H, Rutenfranz J, Sbresny W. Determination of W170 and maximal oxygen uptake in children by different methods. Acta Paediatr. Scand. Suppl. 1971;217:13–17. doi: 10.1111/j.1651-2227.1971.tb05683.x. [DOI] [PubMed] [Google Scholar]
- 15.Nichols JF, Morgan CG, Sarkin JA, Sallis JF, Calfas KJ. Validity, reliability, and calibration of the Tritrac accelerometer as a measure of physical activity. Med. Sci. Sports Exerc. 1999;31:908–912. doi: 10.1097/00005768-199906000-00022. [DOI] [PubMed] [Google Scholar]
- 16.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA. 2002;288:1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 17.Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children. Obes. Res. 2002;10:150–157. doi: 10.1038/oby.2002.24. [DOI] [PubMed] [Google Scholar]
- 18.Pate RR, Trost GS, Dowda M, et al. Tracking of physical activity, physical inactivity, and health-related physical fitness in rural youth. Pediatr. Exerc. Sci. 1999;11:364–376. [Google Scholar]
- 19.Raudenbush SW, Bryk AS. Hierarchical Linear Models. 2nd Ed. Sage Publications; Thousand Oaks, CA: 2002. pp. 26–29. [Google Scholar]
- 20.Schmitz KH, Jacob DR, Hong CP, Steinberger J, Moran A, Sinaiko AR. Association of physical activity with insulin sensitivity in children. Int. J. Obes. 2002;26:1310–1316. doi: 10.1038/sj.ijo.0802137. [DOI] [PubMed] [Google Scholar]
- 21.Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Am. J. Clin. Nutr. 1985;39C(Suppl):5–41. [PubMed] [Google Scholar]
- 22.Trost SG, Pate RR, Freedson PS, Sallis JF, Taylor WC. Using objective physical activity measures with youth: how many days of monitoring are needed? Med. Sci. Sports Exerc. 2000;32:426–431. doi: 10.1097/00005768-200002000-00025. [DOI] [PubMed] [Google Scholar]
- 23.Trost SG, Pate RR, Sallis JF, et al. Age and gender differences in objectively measured physical activity in youth. Med. Sci. Sports Exerc. 2002;34:350–355. doi: 10.1097/00005768-200202000-00025. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition and Physical Activity . Promoting Physical Activity: A Guide for Community Action. Human Kinetics; Champaign, IL: 1999. p. 17. [Google Scholar]
- 25.Vonesh EF, Chinchilli VM, Kewei P. Goodness-of-fit in generalized nonlinear mixed-effects models. Biometrics. 1996;52:572–587. [PubMed] [Google Scholar]
- 26.Welk GJ, Blair SN, Wood K, Jones S, Thompson KW. A comparative evaluation of three accelerometry-based physical activity monitors. Med. Sci. Sports Exerc. 2000;32:S489–S497. doi: 10.1097/00005768-200009001-00008. [DOI] [PubMed] [Google Scholar]
- 27.Welk GJ, Morss G, Church T, Differding J. Laboratory calibration of the Biotrainer and Actitrac activity monitors. Med. Sci. Sports Exerc. 2002;34:S140. [Google Scholar]
- 28.Withers RT, Davis GJ, Crouch RG. A comparison of three W170 protocols. Eur. J. Appl. Physiol. 1977;37:123–127. doi: 10.1007/BF00421698. [DOI] [PubMed] [Google Scholar]