Abstract
This research evaluated the psychometric properties of a brief self-report measure of HIV-related knowledge, the HIV-KQ-18. Low-income men and women (N = 1019) responded to 27 items that represented the domain of interest. Item analyses indicated that 18 items, with item-total correlations ranging from .24 to .57, be retained. Additional analyses demonstrated the HIV-KQ-18’s internal consistency across samples (alphas = .75 to .89), test-rest stability across several intervals (rs = .76 to .94), and strong associations with a much longer, previously validated measure (rs = .93 to .97). Data from three clinical trials indicated that the HIV-KQ-18 detected knowledge gains in treated participants when compared to untreated controls. We conclude that the HIV-KQ-18 is internally consistent, stable, sensitive to the change resulting from intervention, and suitable for use with low-literacy populations.
Keywords: HIV, AIDS, knowledge, assessment, questionnaire
Most models of HIV-risk taking identify knowledge about disease transmission and self-protective behaviors as one of the determinants of behavior change. For example, Fisher and Fisher (1992) developed the Information-Motivation-Behavioral Skills model, and identified information as one determinant of risk behavior and its reduction. Consistent with this and other behavioral science theories, programs designed to reduce risk behavior typically include education about HIV as one component of the intervention (Kalichman, 1998). Because knowledge is a key component of HIV risk reduction programs, interventionists often use knowledge assessments to guide educational curricula and to provide feedback to enhance risk awareness (Carey & Lewis, 1999); also, program evaluators and researchers often assess knowledge to determine the effectiveness of their interventions. Thus, practitioners and scientists need a reliable, valid, and feasible questionnaire to assess HIV-related knowledge.
The HIV Knowledge Questionnaire (HIV-KQ; Carey, Morrison-Beedy, & Johnson, 1997) is a self-administered instrument that was developed using formative work, item and factor analyses to assess knowledge needed for HIV prevention. Respondents read 45 statements about HIV, and indicate whether they think the statement is true or false, or they indicate that they “don’t know.” Text analyses of the reading level, using Flesch and Spache formulae, indicate that most passages fall within the “fairly easy” to “very easy” range (i.e., at or below the 4th grade level); however, several foreign words (e.g., vaccine, antibiotic) increase the overall level to the 7th grade level. Although such words increase the reading level, they are likely to be widely understood even by low-literacy readers because of their common use in the popular culture. A single summary score is obtained by summing the number of items correctly answered (“don’t know” responses are scored incorrect). Higher scores indicate greater knowledge.
Reliability analyses of the HIV-KQ (N = 1,033) indicate that it is internally consistent (alpha = .91) and stable over one- (r = .83), two- (r = .91), and twelve-week (r = .90) intervals (Carey, Morrison-Beedy, & Johnson, 1997). Evidence for the validity of the HIV-KQ was obtained using known groups [i.e., local and national HIV/AIDS educators and researchers (experts) vs. several samples of non-experts] and treatment outcome analyses. Additional validity evidence was obtained from analyses that revealed associations between scores on the HIV-KQ and two related knowledge measures. Discriminant evidence was obtained through non-significant relationships between the HIV-KQ and potentially biasing constructs, including social desirability. Although the HIV-KQ is psychometrically strong, it contains 45 items, which is impractical for street outreach, field surveys, and intervention evaluation work in settings where evaluators also wish to assess knowledge as well as other constructs with minimum respondent burden. Needed is a briefer, but psychometrically well-established measure.
The purpose of the research described in this paper was to validate a brief version of the HIV-KQ. We sought to assemble evidence of its reliability and validity in a population of low-income adults. Three evaluation criteria (and hypotheses) guided this research. First, we expected the brief HIV-KQ to yield reliability indices (i.e., internal consistency, test-retest reliability) that are at least equal to the limit values to be expected on account of the degree of shortening, using the Spearman-Brown prophecy formula (Crocker & Algina, 1986). Second, we expected the brief HIV-KQ to overlap substantially with the longer version, yielding a correlation ≥ .90. Given the validity evidence obtained previously for the HIV-KQ-45, this strong correlation will provide evidence of the validity of the brief HIV-KQ. Third, we expected the brief HIV-KQ to demonstrate sensitivity to change as a function of educational programs. In a repeated measures ANOVA, we expect a significant time effect (as a result of knowledge gain) and a significant group-by-time interaction due to a stronger knowledge gain in treated groups. We predicted that knowledge gains will be greater in treated groups relative to control groups.
Methods
Participants, Recruitment, and Data Collection
Three samples provided data for the current project.
The Women’s Health Project-1 (WHP1) sample included 210 low-income women from a previously published study (Carey, Maisto et al., 1997). As detailed in Table 1, their mean age was 33.9 years; 76% were African-American, 11% Caucasian, and 12% other races or ethnicities. Eighty-seven percent reported an annual family income of less than $20,000 and 59% reported an income of less than $10,000 per year. Seventy-nine percent had children (M = 2.2). The mean level of education was 11.8 years. Risk markers were common, including a history of STDs (48%), multiple sexual partners during the past year (31%), and a partner who had injected drugs during the past three months (27%). Women for this sample had been recruited using handbills, posters, and flyers announcing the “Women’s Health Study”; these materials were distributed at a variety of health, social service, recreational, and business settings that serve economically disadvantaged urban women. The flyer included a brief description of the project, an endorsement from a respected community-based organization (CBO), and a number to telephone for further information. Women who telephoned in response to the flyer were invited to a survey session held at the CBO. During an initial baseline session, they completed the original, 45-item HIV Knowledge Questionnaire (HIV-KQ-45) as well as a number of other measures. A subset (n = 102) of these participants was randomized to receive either an HIV-risk reduction intervention (that included an educational component) or to a control group. These women were then re-assessed at post-intervention and 3 months later.
Table 1.
Demographic Characteristics and Risk Markers in the WHP1, WHP2, and HIP
| WHP1 (N= 209) | WHP2 (N= 357) | HIP (N= 464) | ||||
|---|---|---|---|---|---|---|
| Variables | M | SD | M | SD | M | SD |
| Age | 33.9 | 11.1 | 29.7 | 8.0 | 36.5 | 9.7 |
| Age Range | 15–72 | 16–50 | 18–65 | |||
| Years of education | 11.8 | 1.9 | 11.4 | 1.7 | 11.9 | 2.4 |
|
|
|
|
||||
| n | % | n | % | n | % | |
|
|
|
|
||||
| Females | 209 | 100% | 357 | 100% | 250 | 53.9% |
| Race | ||||||
| African American | 158 | 75.6% | 309 | 86.6% | 100 | 21.6% |
| European American | 23 | 11.0% | 27 | 7.6% | 310 | 66.8% |
| Other | 25 | 12.0% | 19 | 5.3% | 51 | 11.0% |
| Employment | ||||||
| Working | 66 | 31.6% | 91 | 19.6% | ||
| Unemployed | 91 | 43.5% | 373 | 80.4% | ||
| Student | 14 | 6.7% | 81 | 22.7% | ||
| Other | 29 | 13.9% | 273 | 76.5% | ||
| Income | ||||||
| $0–$10,000 ($9,600 in WHP2) | 124 | 59.3% | 292 | 81.8% | 362 | 78.0% |
| $10,000–$20,000 ($19,200 in WHP2) | 54 | 25.8% | 98 | 13.2% | 74 | 16.0% |
| > $20,000 (> $19,200 in WHP2) | 16 | 13.4% | 11 | 3.1% | 28 | 6.0% |
| Children | ||||||
| None | 44 | 21.1% | 70 | 19.6% | 187 | 40.3% |
| 1 child | 40 | 19.1% | 69 | 19.3% | 68 | 14.7% |
| 2 or 3 children | 44 | 21.1% | 141 | 39.5% | 139 | 30.0% |
| > 3 children | 81 | 38.7% | 77 | 21.6% | 68 | 14.7% |
| Risk markers | ||||||
| STD History (lifetime) | 100 | 47.9% | 511 | 14.3% | 176 | 37.9% |
| Ever been tested for HIV | 134 | 64.1% | 264 | 73.9% | 345 | 74.4% |
| ≥2 partners past year | 65 | 31.1% | 124 | 34.7 | 234 | 50.4% |
| Unprotected vaginal sex past 3 months | 89 | 42.6% | 191 | 53.3% | 267 | 57.5% |
| Number reporting one or more IDU partners in the past 3 months | 572 | 27.3% | 23 | 6.4% | 35 | 7.5 % |
Notes. past year;
lifetime; M = mean; SD = standard deviation; WHP1 = Women’s Health Project-1 (Carey et al., 1997); WHP2 = Women’s Health Project-2 (Carey et al., 2000); HIP = Health Improvement Project (Carey et al., 2002).
The Women’s Health Project-2 (WHP2) sample included 357 low-income women from a previously published study (Carey et al., 2000). As detailed in Table 1, their mean age was 29.7 years; 87% were African-American, 7% Caucasian, and 5% other races or ethnicities. Ninety-five percent reported an annual family income of less than $20,000 and 82% reported an income of less than $10,000 per year. Eighty percent had children (M = 2.2). The mean educational level was 11.4 years. Risk markers included an STD during the past year (14%), multiple sexual partners during the past year (35%), and a partner who had injected drugs during the past three months (6%). Recruitment for the WHP2 sample was identical to the procedures for the WHP1 sample. Once recruited, participants completed the HIV-KQ as well as a number of other health-related measures. A subset (n = 102) of these participants was randomized to receive either an HIV-risk reduction intervention (that included an educational component) or to a control group. These women were then re-assessed at post-intervention and 3 months later.
The Health Improvement Project (HIP) sample included 464 men and women who received psychiatric treatment at one of six outpatient psychiatric clinics associated with two local hospitals (Carey et al., 2002). As detailed in Table 1, their mean age was 36.5 years; 22% were African-American, 67% Caucasian, and 11% other races or ethnicities. Ninety-four percent reported an annual family income of less than $20,000 and 78% reported an income of less than $10,000 per year. Sixty percent had children (M = 1.6). The mean level of education was 11.9 years. Risk markers were common, including a lifetime history of an STD (38%), multiple sexual partners during the past year (50%), and a partner who had injected drugs during the past three months (7%). Participants were recruited during routine clinical visits for the HIP; this project is an ongoing randomized clinical trial that seeks to evaluate the efficacy of two risk reduction programs as compared to a standard care condition. As part of their experience in the HIP, participants completed the HIV-KQ-45 (as well as other measures not used for this report) during an initial baseline session. These participants were randomized to receive either an HIV-risk reduction intervention (that included an educational component), or to one of two comparison groups. Participants taking part in the intervention study were then re-assessed at a post-intervention session.
Development of the Brief HIV-KQ
The development of the brief form followed the rationale applied in the development of the HIV-KQ-45 (Carey, Morrison-Beedy, & Johnson, 1997). Item selection followed a two-step strategy. In the first step, a set of relevant items representing the domain was chosen. Second, empirical item analyses were performed. Overall, the selection was guided by the following criteria: (a) The short version should keep the diversity of items available in the long form and should span the conceptual domain as defined below. Empirical item selection should optimize (b) the measure’s internal consistency, and (c) its ability to assess knowledge gain, while maintaining the diversity of items representing the knowledge domain.
Domain-specific item selection
From the initial pool of 45 items, a smaller set of items was selected representing the domain of interest. The purpose of the test was defined as a brief but reliable method for the assessment of HIV knowledge in high-risk populations. Its application field should span the diagnosis of information deficits and misconceptions about HIV risks and self-protective behaviors, and the ability to assess knowledge gain as an effect of HIV risk reduction interventions or similar educational programs. Accordingly, the knowledge domain was defined as HIV-related information relevant for awareness of sexual risk behavior, informed decisions, and behavior change. Further, the test should include items assessing misconceptions about the risk associated with close contact with persons suspected or known to be infected with HIV. Based on these ideas, a preliminary set of 27 of the original 45 items was chosen by the investigators for further analyses.
Empirical item selection
Descriptive item analyses and internal consistency analyses were performed in all three samples. In order (a) to keep the diversity of the questionnaire while (b) optimizing alpha and (c) maximizing sensitivity to change. Empirical criteria were not applied rigidly, but used to guide item selection. In this regard, the absence of a ceiling effect (in order to improve sensitivity for change) was suggested by a mean (M) correct response ≤ 90%, whereas a high corrected item-test correlation (in order to improve internal consistency and overlap with the original test) was suggested by an item-total minus the item (rit-i) ≥.3. However, if the observed M or rit-i values were close to the limits and the item was regarded as crucial for the representation of the knowledge domain, an item would be retained. This decision rule facilitated retention of items that measured critical knowledge, and enhanced the face validity as well as the usefulness of the measure.
Several overlapping item pairs from the HIV-KQ-45 were defined in order to choose the better alternative. For example, two items assessed whether HIV is an easily observable infection: “People who have been infected with HIV quickly show serious signs of being infected” and “You can usually tell if someone has HIV by looking at them.” In this case, we choose the first item because of its lower mean and higher test-item correlation. If empirical decisions on item pairs were difficult, items were eliminated based on content, such as gender-specificity. Two items were eliminated because of their undesirable item statistics (extreme ceiling effects, poor convergence with the sum score). The result was the HIV-KQ-18. In the next step, we tested the HIV-KQ-18 for its psychometric properties.
Data Analytic Plan
In addition to descriptive analyses on item and scale level, reliability coefficients were compared against criterion values derived with the Spearman-Brown formula from the respective reliability indices of the 45-item version. We expected a reduction in the reliability coefficients due to shortening of the measure. The Spearman-Brown adjusted expected values served as the limit the short form should meet or exceed in order to evaluate the reduction in reliability as acceptable.
Sensitivity to change was evaluated testing treatment effects in all three samples. Repeated measure ANOVAs were performed separately for the time intervals between baseline and post-intervention, and baseline and follow-up. In each analysis, significant time and group-by-time interactions were expected. Additional group comparisons were performed by t-tests, using difference scores between post-intervention and baseline (i.e., Time 2–Time 1), and between follow-up and baseline (i.e., Time 3–Time 1), as the dependent variables. In accordance with the hypothesis, one-sided significance tests were performed.
Results
To determine the psychometric properties of the HIV-KQ-18 and, as the main criteria for goodness-of-fit, we evaluated (a) item and test statistics (internal consistencies, distribution characteristics), (b) correlations between the long and short version of the HIV-KQ, (c) stability over time in the control groups, and (d) sensitivity for change.
Item and Test Statistics
Table 2 lists the items and item statistics of the HIV-KQ-18. On an item level, the means ranged from .23 to .94 (see the 1st, 4th, and 7th columns in Table 2). Given that each item has a likelihood of .5 to be answered correctly by chance, this range is quite good. Item means > .9 were rare due to the exclusion of items with ceiling effects.
Table 2.
Item Content and Item Statistics of HIV-KQ-18
| WHP1 (n=209) | WHP2 (n=357) | HIP (n=464) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Item | M | SD | rit-i | M | SD | rit-i | M | SD | rit-i |
| Coughing and sneezing DO NOT spread HIV. (T) | .62 | .49 | .33 | .57 | .50 | .30 | .80 | .40 | .31 |
| A person can get HIV by sharing a glass of water with someone who has HIV. (F) | .77 | .42 | .41 | .81 | .39 | .36 | .76 | .43 | .36 |
| Pulling out the penis before a man climaxes/cums keeps a woman from getting HIV during sex. (F) | .80 | .40 | .46 | .78 | .41 | .47 | .81 | .39 | .42 |
| A woman can get HIV if she has anal sex with a man. (T) | .73 | .44 | .49 | .76 | .43 | .33 | .83 | .38 | .36 |
| Showering, or washing one’s genitals/private parts, after sex keeps a person from getting HIV. * (F) | .86 | .34 | .51 | .89 | .32 | .44 | .88 | .33 | .34 |
| All pregnant women infected with HIV will have babies born with AIDS. (F) | .61 | .49 | .41 | .58 | .49 | .35 | .59 | .49 | .36 |
| People who have been infected with HIV quickly show serious signs of being infected. (F) | .82 | .39 | .46 | .58 | .39 | .40 | .77 | .42 | .38 |
| There is a vaccine that can stop adults from getting HIV. (F) | .75 | .44 | .45 | .74 | .44 | .41 | .80 | .40 | .34 |
| People are likely to get HIV by deep kissing, putting their tongue in their partner’s mouth, if their partner has HIV. (F) | .55 | .50 | .33 | .60 | .49 | .27 | .52 | .50 | .24 |
| A woman cannot get HIV if she has sex during her period. (F) | .81 | .39 | .51 | .80 | .40 | .43 | .76 | .43 | .30 |
| There is a female condom that can help decrease a woman’s chance of getting HIV. (T) | .60 | .49 | .32 | .64 | .48 | .29 | .58 | .49 | .28 |
| A natural skin condom works better against HIV than does a latex condom. (F) | .55 | .50 | .45 | .53 | .50 | .30 | .48 | .50 | .34 |
| A person will NOT get HIV if she or he is taking antibiotics. (F) | .81 | .40 | .57 | .81 | .39 | .52 | .58 | .49 | .40 |
| Having sex with more than one partner can increase a person’s chance of being infected with HIV. (T) | .87 | .34 | .44 | .92 | .26 | .31 | .94 | .23 | .27 |
| Taking a test for HIV one week after having sex will tell a person if she or he has HIV. (F) | .76 | .43 | .44 | .83 | .37 | .33 | .69 | .46 | .32 |
| A person can get HIV by sitting in a hot tub or a swimming pool with a person who has HIV. (F) | .56 | .50 | .30 | .56 | .50 | .28 | .72 | .45 | .35 |
| A person can get HIV from oral sex. ** (T) | .64 | .48 | .36 | .65 | .48 | .30 | .72 | .45 | .28 |
| Using Vaseline or baby oil with condoms lowers the chance of getting HIV. (F) | .75 | .43 | .48 | .76 | .43 | .49 | .23 | .42 | .28 |
Notes. Correct answers appear in parentheses (T = true; F = false).
In WHP2, a gender-specific version of this item was used;
Gender specific forms of this item were used in all samples; M = mean; SD = standard deviation; WHP1 = Women’s Health Project-1 (Carey et al., 1997); WHP2 = Women’s Health Project-2 (Carey et al., 2000); HIP = Health Improvement Project (Carey et al., 2002); rit-t = item-total (less the item) correlation.
On a scale level, the means and distributions of the scores show a pattern to be expected for dichotomous item sets assessing knowledge (Figure 1). The scale means vary between 71.3 (WHP1), 72.5 (WHP2), and 69.2 (HIP). These values differ from a chance mean of 50 % and leave room for improvement, which is a necessary precondition for a measure sensitive to knowledge gain. The distributions also deviate from a normal curve (WHP1: χ2 = 26.2, p < .001; WHP2: χ2 = 45.1, p < .001; HIP: χ2 = 17.2, p < .001). Such distributions are expected and natural for a knowledge scale with dichotomous items. That is, a scale score < 50% would require a significant lack of knowledge, gross misconceptions about HIV transmission, and/or bad luck in guessing; thus, there are only a small number of scores in the lower half of the scale.
Figure 1.
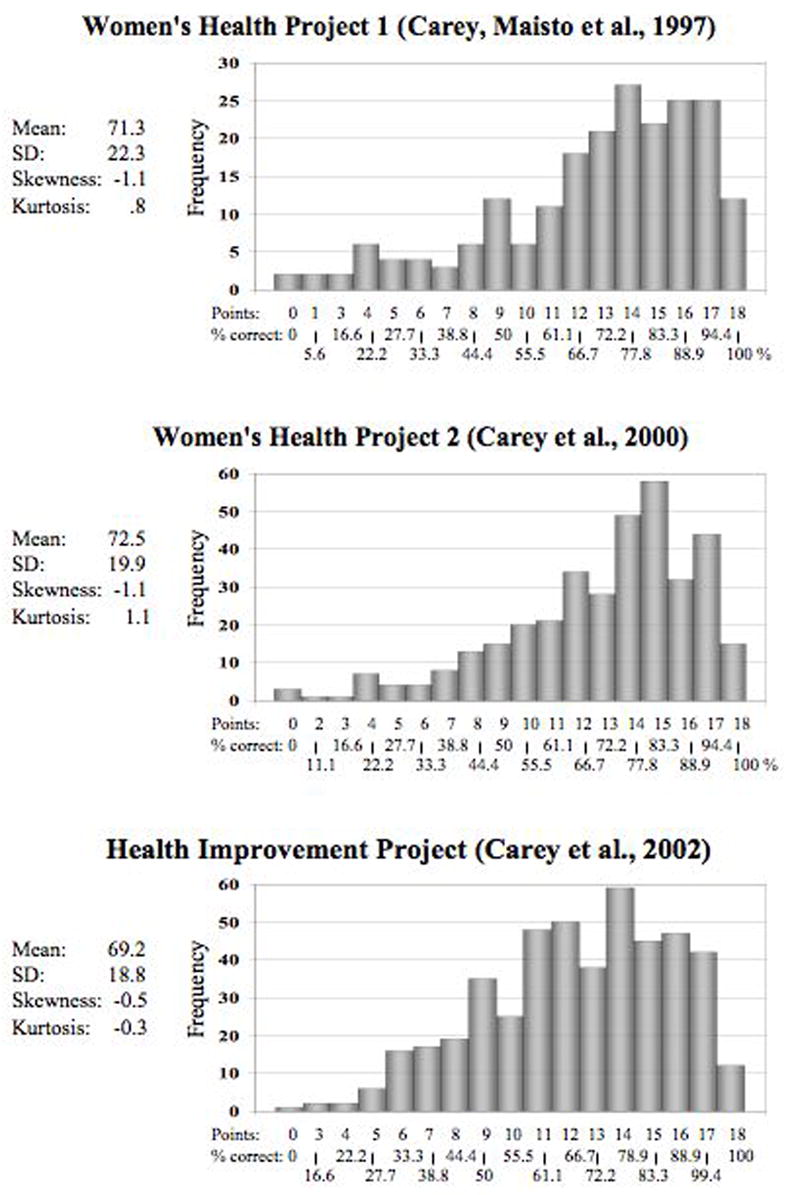
Distributions of the HIV-KQ-18 in three samples
As depicted in the 3rd, 6th, and 9th columns of Table 2, the item -- total (less the item) correlations ranged from .24 to .57, indicating a convergence among the items. On scale level, the HIV-KQ-18 shows good internal consistencies with αs ranging from .75 to .89 (Table 3). Because intervention effects in the treatment group (ceiling effects, reduced variance) can reduce α, internal consistencies at post-intervention and follow-up were computed again for the control groups only. The control groups in the WHP1 and WHP2 samples showed slightly higher internal consistencies at post-intervention and follow-ups. We further compared the internal consistencies with criterion values derived from the HIV-KQ-45, using Spearman-Brown’s formula (see Table 3, numbers in parentheses). For example, α in the baseline data of WHP1 was .90 for the HIV-KQ-45. According to the Spearman-Brown formula, this leads to an expected α of .79 for a test that is reduced to 40% of its original length. The internal consistencies found at each assessment consistently met the criterion of α ≥ the limit value derived from the long form.
Table 3.
Internal Consistencies, Correlations With the 45-Item Long Form, and Stability Coefficients
| Sample | N | Cronbach’s α | r18–45 | rTT | |||||
|---|---|---|---|---|---|---|---|---|---|
| All | Control | All | Control | All | Control | T1 | T2 | ||
| WHP1 | T1 | 209 | .83 (.79) | .95 | |||||
| T2 | 75 | 32 | .83 (.80) | .85 (.82) | .95 | .95 | .86 (.78) | ||
| T3 | 66 | 31 | .86 (.82) | .86 (.84) | .96 | .96 | .86 (.75) | .76 (.65) | |
| WHP2 | T1 | 357 | .78 (.74) | .95 | |||||
| T2 | 98 | 48 | .85 (.83) | .89 (.87) | .96 | .97 | .93 (.91) | ||
| T3 | 91 | 40 | .79 (.78) | .86 (.85) | .94 | .96 | .94 (.90) | .88 (.83) | |
| HIP | T1 | 464 | .75 (.71) | .93 | |||||
| T2 | 325 | 210 | .76 (.72) | .75 (.71) | .94 | .94 | .77 (.62) | ||
Notes. WHP1 = Women’s Health Project-1 (Carey et al., 1997); WHP2 = Women’s Health Project-2 (Carey et al., 2000); HIP = Health Improvement Project (Carey et al., 2002); r18–45 = Correlation between the long and short versions of the HIV-KQ; rTT = test-retest correlations; T1 = baseline; T2 = post-intervention; T3 = follow-up; Numbers in parentheses indicate limit criterion values for alpha and rTT (observed values should equal or exceed limit criterion values if the brief version of a test is to be acceptable according to Spearman-Brown formula).
Association with the HIV-KQ-45
As one of the criteria for successful shortening of a measure, we evaluated overlap with the original item pool. We correlated the long and short form of the HIV-KQ in all three samples at baseline and follow-up assessments, and found a strong overlap between r = .93 and r = .97 (Table 3). Thus, the HIV-KQ-18 assesses nearly exactly the same dimension as the original 45-item scale.
Test-Retest Reliability of the HIV-KQ-18
The last two columns of Table 3 show the test-retest correlations between baseline, post, and follow-up assessments. Test-retest coefficients for the baseline—post assessments were computed in control groups only because knowledge scores were expected to improve over time in the treatment group. For the post—follow-up correlations, however, the whole sample was used because no intervention occurred during this interval and scores were expected to remain stable over this interval. The stability coefficients varied between .76 and .94, providing evidence for satisfactory to excellent reliability of the test scores. These reliability coefficients were once again compared to criterion values derived from the 45-item questionnaire, which were adjusted for the test length using the Spearman-Brown formula. All coefficients in the table exceeded the expected values. The average weighed test-retest correlation was r̄ =.83, providing evidence for the stability of the HIV-KQ-18.
Sensitivity to Change
As a measure sensitive to change, the HIV-KQ-18 was expected to show significant increase in the knowledge scores of the treatment groups. Sensitivity to change was tested by a series of repeated measures ANOVAs comparing change over time in treatment and control groups. The results are summarized in Table 4. We found significant main effects for time as well as significant group-by-time interactions in each of the analyses. Post-hoc group comparisons were performed, using difference scores between baseline and follow-up assessments as outcome. The results confirm that knowledge gains were stronger in the treatment groups compared to the control groups in each analysis (WHP1: Mdiff-T2-T1 = 11.3 vs. 1.7, t = 2.73, p < .004; Mdiff-T3-T1 = 9.6 vs. 1.1, t = 2.19, p < .02; WHP2: Mdiff-T2-T1 = 9.3 vs. 2.2, t = 2.57, p < .006; Mdiff-T3-T1 = 11.1 vs. 4.4, t = 2.40, p < .01; HIP: Mdiff-T2-T1 = 13.6 vs. 1.0, t = 7.91, p < .0001).
Table 4.
Sensitivity to Change as Indicated by Significant Increase Over Time and Group-by-Time Interactions
| T1 (Baseline) | T2 (Post) | T3 (Follow-up) | Fa | Fa | Fa Group- | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Analysis | Group | n | M | (SD) | M | (SD) | M | (SD) | Time | Group | by-Time |
| WHP1 | |||||||||||
| T1-T2 | E | 43 | 75.8 | (18.7) | 86.8 | (14.1) | 12.7 *** | 5.9 ** | 7.4 ** | ||
| C | 32 | 70.5 | (22.2) | 71.9 | (22.8) | (1/73) | (1/73) | (1/73) | |||
| T1-T3 | E | 35 | 76.9 | (18.4) | 86.4 | (16.9) | 7.8 ** | 4.4 * | 4.8 * | ||
| C | 31 | 71.3 | (22.8) | 72.4 | (23.9) | (1/64) | (1/64) | (1/64) | |||
| T1-T2-T3 | E | 35 | 76.9 | (18.4) | 86.9 | (14.5) | 86.3 | (16.9) | 5.0 ** | 4.6 * | 3.9 * |
| C | 25 | 73.2 | (21.3) | 73.2 | (20.8) | 75.3 | (22.1) | (2/57) | (1/58) | (2/57) | |
|
| |||||||||||
| WHP2 | |||||||||||
| T1-T2 | E | 49 | 74.7 | (20.2) | 84.0 | (14.0) | 17.4 *** | 3.5 * | 6.6 ** | ||
| C | 48 | 70.4 | (24.8) | 72.6 | (26.1) | (1/95) | (1/95) | (1/95) | |||
| T1-T3 | E | 50 | 72.4 | (19.5) | 83.6 | (12.4) | 31.3 *** | 1.5 | 5.7 ** | ||
| C | 40 | 71.0 | (23.6) | 75.4 | (23.4) | (1/88) | (1/88) | (1/88) | |||
| T1-T2-T3 | E | 41 | 73.7 | (19.7) | 84.6 | (13.8) | 85.0 | (12.9) | 14.0 *** | 3.8 * | 4.5 ** |
| C | 36 | 70.5 | (24.1) | 72.2 | (24.8) | 74.8 | (24.5) | (2/74) | (1/75) | (2/74) | |
|
| |||||||||||
| HIP | |||||||||||
| T1-T2 | E | 115 | 67.0 | (19.8) | 80.5 | (16.1) | 84.3 *** | 2.9 * | 62.6 *** | ||
| C | 210 | 69.9 | (17.8) | 70.9 | (18.6) | (1/323) | (1/323) | (1/323) | |||
Notes. Means are presented as percentage of correct answers; WHP1 = Women’s Health Project-1 (Carey et al., 1997); WHP2 = Women’s Health Project-2 (Carey et al., 2000); HIP = Health Improvement Project (Carey et al., 2002); groups are coded as E = experimental group (i.e., received education about HIV and would be expected to improve knowledge over time), C = control group; T1 = baseline; T2 = post-intervention; T3 = follow-up.
Numbers in parentheses refer to hypotheses and error degrees of freedom.
p < .05,
p < .01,
p < .001 (one-tailed).
Discussion
The primary purpose of this research was to develop a brief measure of HIV-knowledge that would be suitable for use in a variety of clinical, educational, and public health settings. Beginning with the 45-item HIV Knowledge Questionnaire (HIV-KQ-45), we selected 23 items that assessed critical knowledge regarding the transmission and prevention of HIV disease. Item analyses revealed that 18 items provided optimal coverage of the targeted domain while enhancing the psychometric properties of the resulting instrument, the HIV-KQ-18. Subsequent psychometric analyses indicated that the HIV-KQ-18 provides strong levels of internal consistency and test-retest stability. For example, the internal consistencies across samples ranged from .75 to .89, easily exceeding the .70 standard recommended by Nunnally and Bernstein (1994). Even though the HIV-KQ-18 has only 40% of the items of its predecessor, this brief measure retains a strong association with the longer 45-item version. Finally, the HIV-KQ-18 was demonstrated to be sensitive to knowledge changes resulting from risk reduction interventions that contained an educational component.
Two limitations of the HIV-KQ-18 and of this research should be noted. First, although our research began with careful operationalization of the domain of HIV-related knowledge and with a rational item selection phase, the resulting measure cannot be considered a comprehensive measure of HIV-related knowledge. Because the measure emphasizes the sexual transmission of HIV, it does not assess comprehensively transmission by other vectors, such as needle-sharing or blood products. Moreover, the measure does not attempt to assess knowledge regarding the natural history, clinical course, or treatment of HIV and AIDS. Thus, in applications or settings where a more comprehensive assessment is needed, we recommend use of the longer HIV-KQ-45.
Second, our evaluation relied on data from primarily low-income, low-literacy, and heterosexual samples. It is possible that better-educated samples might yield higher summary scores (Peruga & Celentano, 1993), introducing the possibility of “ceiling effects” in correlational or behavior change analyses. Although we acknowledge this potential limitation, we want to point out that more education is not always associated with greater HIV-related knowledge. In prior research with the HIV-KQ-45 we found that community-dwelling married couples with college educations scored lower on the HIV-KQ-45 (M = 52%) than did low-income urban women with high school educations (M = 72%; Carey et al., 1997). However, because of the associations between poverty and HIV (Fournier & Carmichael, 1998), and between low literacy level and HIV (Kalichman, Benotsch, Suarez, Catz, & Miller, 2000), we believe that instruments assessing HIV knowledge in low-income and low-literacy populations are most needed, justifying our sampling strategy.
We conclude that the HIV-KQ-18 provides educators, program evaluators, and researchers with a brief, easy-to-administer and easy-to-score measure of HIV-related knowledge. We hope that this measure will prove useful in the many settings where self-reported knowledge of HIV is needed.
Acknowledgments
This work was supported by grants from the National Institute of Mental Health (# R01-MH54929 and K02-MH01582) to the first author. We thank the participants and the members of the Women’s Health Project and the Health Improvement Project teams for their contributions to this research.
References
- Carey MP, Braaten LS, Maisto SA, Gleason JR, Forsyth AD, Durant LE, Jaworski BC. Using information, motivational enhancement, and skills training to reduce the risk of HIV infection for low-income urban women: A second randomized clinical trial. Health Psychology. 2000;19:3–11. doi: 10.1037//0278-6133.19.1.3. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Maisto SA, Gordon CM, Schroder KEE, Vanable PA. Reducing HIV risk behavior among adults with a severe and persistent mental illness: A randomized controlled trial. 2002. Manuscript submitted for publication. [Google Scholar]
- Carey MP, Lewis BP. Motivational strategies can augment HIV-risk reduction programs. AIDS and Behavior. 1999;3:269–276. doi: 10.1023/a:1025429216459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Maisto SA, Kalichman SC, Forsyth AD, Wright EM, Johnson BT. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. Journal of Consulting and Clinical Psychology. 1997;65:531–541. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Morrison-Beedy D, Johnson BT. The HIV-Knowledge Questionnaire: Development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS and Behavior. 1997;1:61–74. [Google Scholar]
- Crocker L, Algina A. Introduction to classical and modern test theory. New York: Holt, Reinhart, & Winston; 1986. [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fournier AM, Carmichael C. Socioeconomic influences on the transmission of human immunodeficiency virus infection: The hidden risk. Archives of Family Medicine. 1998;7:214–217. doi: 10.1001/archfami.7.3.214. [DOI] [PubMed] [Google Scholar]
- Kalichman SC. Preventing AIDS: A sourcebook for behavioral interventions. Mahwah, NJ: Erlbaum; 1998. [Google Scholar]
- Kalichman SC, Benotsch E, Suarez T, Catz S, Miller J. Health literacy and health-related knowledge among men and women living with HIV-AIDS. American Journal of Preventive Medicine. 2000;18:325–331. doi: 10.1016/s0749-3797(00)00121-5. [DOI] [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric theory. 3. New York: McGraw-Hill; 1994. [Google Scholar]
- Peruga A, Celentano DD. Correlates of AIDS knowledge in samples of the general population. Social Science and Medicine. 1993;36:509–524. doi: 10.1016/0277-9536(93)90412-w. [DOI] [PubMed] [Google Scholar]


