Abstract
The objective of this randomized double-blind investigation was to compare the anesthetic efficacy and injection discomfort of 3 volumes of 2% lidocaine with 1∶100,000 epinephrine for maxillary infiltration anesthesia. A total of 25 subjects received 0.6, 0.9, and 1.2 mL of the anesthetic buccal to an upper canine. Test teeth were assessed with electrical stimulation to determine onset and duration of pulpal anesthesia; soft tissue anesthesia and injection discomfort were assessed by pin-prick test and visual analog scale (VAS). Data were analyzed by 2-way analysis of variance (ANOVA), Friedman, and chi-square tests (α = 5%). The 1.2 mL dose induced faster onset of pulpal anesthesia, a higher success rate, and a longer duration of soft tissue/pulpal anesthesia than were achieved with the other doses (P < .05). No differences in injection discomfort were observed between treatments. It is concluded that maxillary infiltration anesthesia with lidocaine and epinephrine has a faster onset, a greater success rate, and a longer duration when a volume of 1.2 mL is used than when volumes less than 1.0 mL are used.
Keywords: Lidocaine, Anesthetic efficacy, Infiltration anesthesia
Introduction
The reliable management of pain is an important factor in reducing fear and anxiety in dental treatment. Clinicians must have a thorough knowledge of local anesthetic solutions and techniques. When an agent and a technique are chosen, it is important for the clinician to understand the onset, depth, and duration of anesthesia in relation to the operative procedure to be performed. Ideally, the chosen regimen should have a short onset period and should last for the time necessary to finish the procedure, without an extended recovery period.
Lidocaine, the first commercialized amide local anesthetic, is still the most widely used anesthetic in some countries.1 It is considered a reference for any new local anesthetic.2 Extensive information is available about the efficacy of lidocaine, but little has been published concerning the volume required to produce adequate clinical anesthesia.
It is suggested that a minimum of 1.0 to 1.5 mL is necessary to promote inferior alveolar nerve block.3 It has been shown that volumes exceeding 1.8 mL are not more efficient.4,5
Textbooks on local dental anesthesia2,6 suggest that volumes ranging from 0.5 to 2.0 mL are needed to achieve pulpal anesthesia after local infiltration. Cowan7,8 investigated the doses of lidocaine with epinephrine required to allow various operative dental treatments to be performed following maxillary infiltration but did not use a double-blind design or a controlled stimulus and did not investigate injection discomfort.
The purpose of this study was to evaluate the onset and duration of pulpal anesthesia in target and adjacent teeth, as well as soft tissue anesthesia and injection discomfort, after maxillary buccal infiltration of 3 volumes of 2% lidocaine with 1∶100,000 epinephrine.
Methods
This randomized, double-blind, crossover investigation received ethical approval from the institutional review board. With data from a previous investigation8 and a type I error set at .05, a power calculation dictated that a sample size of 25 would give 99% power. Written informed consent was obtained from each patient. None of the volunteers was taking any medication that would alter pain perception. All test and control teeth were unrestored and caries free.
Each volunteer attended 3 visits that were scheduled at least 2 weeks apart. At each visit, volunteers received one of the following volumes of 2% lidocaine with 1∶100,000 epinephrine (Alphacaine, DFL Industria e Comercio Ltda, Rio de Janeiro, RJ, Brazil), which was injected into the buccal sulcus in the upper left canine region: 0.6 mL, 0.9 mL, or 1.2 mL.
The volume injected at each visit was randomized, and by the end of the trial, each volunteer had received each treatment. The same operator performed all injections with a Carpule self-aspirating syringe (Duflex, SS White, Rio de Janeiro, RJ, Brazil) fitted with a short 30-gauge needle (BD–Brasil, Sao Paulo, SP, Brazil). An aspirating technique was selected, and the solution was deposited at a rate of 1 mL/min.
At the beginning of each appointment and before the injection, the upper left lateral incisor, canine, and first premolar were individually tested 6 times with an electronic pulp tester (Model 2006, Analytic Technology Corp, Redmond, Wash). Baseline was recorded as the mean of these 6 readings. According to the manufacturer's recommendation, a small portion of fluoride gel was applied to the probe tip, which was placed on the buccal side, midway between the gingival margin and the occlusal edge of the tooth. Every 2 minutes after injection, the teeth were tested, until no response to the maximum stimulus was obtained (80 reading). After this period, the teeth were tested every 10 minutes until values returned to baseline. The upper right canine was used as a control to ensure that the pulp tester was operating properly, and that patients were responding accurately during the study. All pulp testing was performed by a trained operator, who was blinded to the anesthetic volumes administered.
The parameters evaluated were as follows: Onset of pulpal anesthesia was considered as the time from the end of injection to the first of 2 consecutive readings of 80 without response. Duration of pulpal anesthesia was defined as the time from onset of pulpal anesthesia to the time recorded before 2 positive responses to the pulp tester were obtained. Onset of soft tissue anesthesia was the time from the end of injection and the beginning of numbness to pin-prick in the canine buccal gingiva. Duration of soft tissue anesthesia was the time from the beginning to the end of numbness to pin-prick in the canine buccal gingiva.
Anesthesia success was considered as a minimum of 10 minutes of pulpal anesthesia reading (1 reading of 80) without response after establishment of the onset of anesthesia. Noncontinuous anesthesia was defined as 2 consecutive readings of 80 without response, a loss of the 80 reading, and then another 80 reading at the following pulp testing. Anesthesia was classified as short duration when the extent of pulpal anesthesia was 10 minutes (only 1 reading of 80 after establishment of the onset of anesthesia).
Injection discomfort was assessed by the volunteer immediately after injection with a 100 mm visual analog scale (VAS), with end points tagged “no pain” and “pain as bad it could be.”9
Data were analyzed with BioEstat, version 4.0 (Mamiraua Institute, Belem, Brazil). Onset of pulpal anesthesia for the canine was log transformed. Onset and duration of pulpal anesthesia and duration of soft tissue anesthesia were submitted to 2-way ANOVA and Tukey testing. The Friedman test was used to analyze pain sensitivity. Differences in anesthetic success were assessed by means of chi-square tests. The significance level was 5%.
Results
All 25 recruited volunteers (13 women and 12 men) completed the investigation. The mean age of volunteers was 21.1 ± 1.05 years (range, 20 to 40 years).
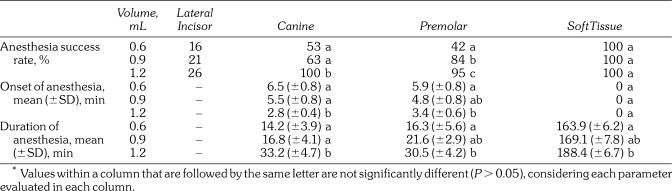
Results for onset and duration of soft tissue and pulpal anesthesia (canine and first premolar) and success rate of anesthesia (soft tissue, lateral incisor, canine, and first premolar) are presented in Table 1. Onset and duration of lateral incisor anesthesia were not analyzed because of the small incidence of successful anesthesia for this tooth.
Table 1.
Anesthesia Success Rate, Onset of Pulpal and Soft Tissue Anesthesia, and Duration of Soft Tissue and Pulpal Anesthesia After Buccal Infiltration in the Upper Left Canine Region With 2% Lidocaine With 1∶100,000 Epinephrine Solution*
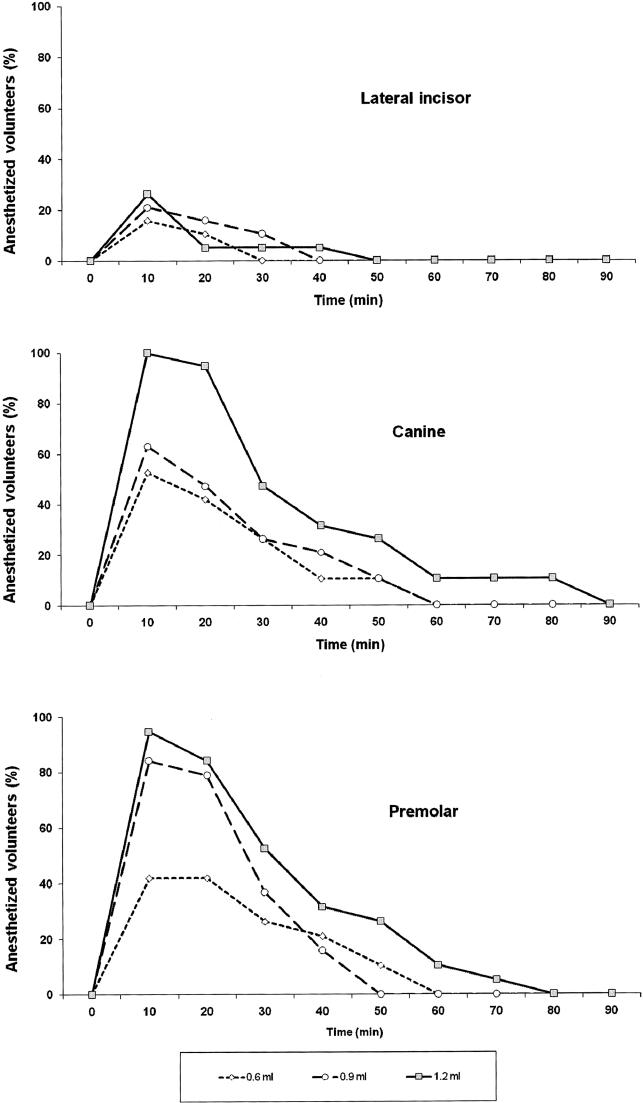
The Figure shows the incidence of pulpal anesthesia (no response to 80 reading) throughout the testing period. The success rate of anesthesia varied with the teeth tested (Table 1). The greatest success was seen with the canine (100% success at the highest dose), which was the tooth nearest to the site of deposition of the anesthetic. Anesthetic success was higher for the 1.2 mL volume than for the other doses (P < .001) for the canine (Table 1). No difference (P > .05) was observed between the 0.6 and 0.9 mL volumes.
Incidence of pulpal anesthesia as determined by lack of response to electrical pulp testing at maximum setting (percentage of 80 readings) for 0.6 mL, 0.9 mL, and 1.2 mL.
Successful premolar anesthesia showed statistically significant differences between 0.6 and 0.9 mL (P < .001), 0.6 and 1.2 mL (P < .001), and 0.9 and 1.2 mL (P = .01). Lateral incisor anesthesia was not affected by volume (P > .05), and low success rates were shown for all doses.
Significant improvement in the onset of anesthesia for both canine and premolar was observed with the 1.2 mL dose. All volunteers presented soft tissue anesthesia immediately after the end of the injection.
The 1.2 mL dose also produced longer-lasting pulpal and soft tissue anesthesia when compared with the other volumes (Table 1). When the canine was considered, differences were found with use of the 1.2 mL dose in relation to each of the other volumes (P < .001); for premolar pulpal anesthesia and soft tissue numbness, differences were only between 0.6 and 1.2 mL (P < .05). No statistically significant differences (P > .05) were noted between the durations of soft tissue and pulpal anesthesia provided by 0.6 and 0.9 mL.
Noncontinuous anesthesia produced by 0.9 mL occurred in 4, 12, and 16% of lateral incisors, canines, and premolars, respectively. The use of 1.2 mL produced noncontinuous anesthesia in 4, 0, and 12% of lateral incisors, canines, and premolars, respectively.
Anesthesia of short duration for 0.6, 0.9, and 1.2 mL doses was observed in 4, 4, and 20% of lateral incisors; 12, 16, and 4% of canines; and 0, 4, and 12% of premolars, respectively.
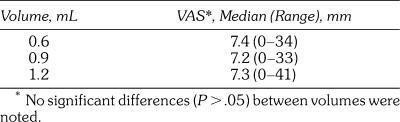
VAS scores for injection discomfort are shown in Table 2. No differences (P > .05) in injection discomfort were observed between treatments.
Table 2.
Anesthetic Injection Pain as Assessed by Visual Analog Scale (VAS)
Discussion
When local anesthetic efficacy is compared, it is important that a reproducible outcome measure be obtained. Operative dental procedures will produce uncontrolled stimuli, so a reliable alternative is required. The use of electrical stimulation is considered a safe and precise method of evaluating pulpal anesthesia in vital asymptomatic teeth.10–12 The absence of perception to the maximum output of the pulp tester (80 reading) has been widely used as a criterion for pulpal anesthesia.4,13–21
Local anesthesia is not always effective in dentistry. The success of inferior alveolar nerve blocks ranges from 53 to 100%.4,14–16,19–21 It would be expected that a higher degree of success is achieved with infiltration anesthesia because it is an easier technique to perform, and it should not be affected by collateral nerve supply. Nevertheless, infiltration injection is not always 100% successful. Success is reported to range from 50 to 100% in maxillary teeth.19,22–25 This variation can be explained by differences in the smoothness, density, porosity, and thickness of the bone surrounding the maxillary teeth,3 as well as by individual variation in response to the drug administered.18
When only the anterior maxillary teeth are considered for the anesthetic, success has been reported to range from 68 to 100% for the lateral incisor, with local anesthetic volumes ranging from 0.5 to 1.8 mL.18,24,26–28 Haas et al29 reported 65% success with 1.5 mL of 4% prilocaine with 1∶200,000 epinephrine or 4% articaine with 1∶200,000 epinephrine for the maxillary canine. Successful anesthesia obtained for the canine in the present study was in a similar range (53 to 100%).
Results of the present study show that the success of anesthesia was dependent upon the dose of local anesthetic injected (Table 1). Cowan7 suggested that doses of less than 0.75 mL of 2% lidocaine with 1∶80,000 epinephrine were adequate for 2 adjacent teeth after maxillary infiltration. The present results, although obtained with a different concentration of epinephrine, highlight advantages of using doses greater than 1.0 mL, especially when anesthesia of adjacent teeth is required. Knoll-Kohler and Fortsch27 reported 100% success when 0.5 mL of 2% lidocaine with 1∶100,000 epinephrine was injected into the maxillary incisor; in the present study, this rate was obtained only for the canine with the 1.2 mL dose. These findings are similar to those of Nusstein et al18 with 1.8 mL of the same solution infiltrated into the apical region of the upper lateral incisor (85%), and of Nordenram and Danielsson28 with 1.0 mL of 2% lidocaine with 1∶80,000 epinephrine injected at the apex of the upper lateral incisor (100%). Differences in method and sample size could explain the variable results because Knoll-Kohler and Fortsch27 used 10 volunteers, and the other authors studied at least 20 volunteers.
Successful anesthesia for teeth adjacent to the targeted tooth was less common than for the canine. Success for lateral incisors was very low (26% or less), but the premolar showed greater success (ranging from 42 to 95%). This could possibly be explained by the supine position of the patient, which allowed the local anesthetic solution to diffuse to the posterior region because of gravity. Success rates obtained for the premolar were very similar to those obtained by Moore et al30 after infiltration of 1.0 mL of 4% articaine with 1∶100,000 or 1∶200,000 epinephrine, that is, 93.5 and 95.2%, respectively.
Cowan7 intimated that, although no statistically significant relationship was evident in his results between onset time and dose of 2% lidocaine with 1∶80,000 epinephrine, larger doses produced quicker onset times. He suggested that onset time decreased as volume rose to 0.75 mL, with any further increase in dose having no effect. Results of the present study (Table 1) confirm that anesthetic onset time for both canine and premolar decreased with increasing dose, and that this effect was apparent at doses above 0.75 mL. The mean onset of pulpal anesthesia for the canine and premolar in the present study ranged from 2.8 to 6.5 minutes and from 3.4 to 5.9 minutes, respectively. These onset times are similar to those obtained by others31,32 with infiltration of 1.8 mL of the same solution into the posterior maxillary and canine regions.
The duration of pulpal and soft tissue anesthesia also increased with the volume of local anesthetic. Injection of 1.2 mL significantly increased the duration of anesthesia compared with injection of other volumes. Values obtained with 1.2 mL for the canine (33.2 minutes) and premolar (30.5 minutes) were close to those obtained by Costa et al31 (39.2 minutes), Nusstein et al18 (41.4 minutes), and Oliveira et al32 (46.5 minutes) for the same solution, but values were smaller than that reported by Knoll-Kohler and Fortsch27 (61.7 minutes). Cowan7,8 also reported that the duration of soft tissue anesthesia increased as the dose of lidocaine with epinephrine increased.
More than 10 minutes of pulpal anesthesia is required for many dental procedures; this explains the decrease in production of lidocaine plain.2 Results of the present study show that, in addition to any influence provided by added vasoconstrictors, the success, onset, and duration of pulpal anesthesia are affected by the volume injected. Unfortunately, the increase in pulpal duration is also followed by an increase in soft tissue anesthesia (Table 1), which is not necessary for many dental procedures and is an inconvenience to patients who are undergoing nonsurgical procedures.
Noncontinuous anesthesia has been reported by others4,5,16 after inferior alveolar nerve block. This may be the result of the equilibrium between ionized and nonionized forms of the anesthetic, which causes periods of inadequate pulpal anesthesia. Results of the present investigation show that this phenomenon can also occur after infiltration anesthesia.
In the present study, anesthesia of short duration was defined as a maximum period of 10 minutes without response to maximum electrical stimulus, because this is approximately the duration of pulpal anesthesia for lidocaine plain, which is insufficient for many dental procedures. Anesthesia of short duration was observed for almost all volumes evaluated, ranging from 0 to 20%. The percentage of short duration anesthesia in the present study was similar to that reported for inferior alveolar nerve blocks.4,5
The dose of local anesthetic injected might be expected to influence discomfort. The volume injected has been reported to affect postoperative discomfort following gingival surgery.33 Results of the present study show that injection discomfort did not vary between treatments. This is consistent with the findings of other workers,17 who reported no difference in injection pain between 0.9 and 1.8 mL volumes of lidocaine with epinephrine injected as buccal infiltration into the mandible. Levels of discomfort reported for most injections in the present study are considered as low-intensity pain.34 Only 3 volunteers (1 at each of the volumes studied) reported discomfort considered as moderate, that is, greater than 30 mm on the VAS.34 These values are shown in Table 2 (highest value in each volume group). Other authors15,35 have reported injection discomfort related to the pH of the local anesthetic solution and the rate of injection.
Conclusion
We concluded that results of the present study suggest that maxillary infiltration anesthesia has a faster onset, a greater success rate, and a longer duration when a volume of 1.2 mL is used than when volumes less than 1.0 mL are given.
References
- Corbett I.P, Ramacciato J.C, Groppo F.C, Meechan J.G. A survey of local anaesthetic use among general dental practitioners in the U.K. attending post-graduate courses on pain control. Br Dent J. 2005;199:784–787. doi: 10.1038/sj.bdj.4813028. [DOI] [PubMed] [Google Scholar]
- Malamed S.F. Handbook of Local Anesthesia. 5th ed. St Louis, Mo: Mosby; 2004. pp. 53–59.pp. 160–164. [Google Scholar]
- Jorgensen N.B, Hayden J. Sedation, Local and General Anesthesia in Dentistry. Philadelphia, Pa: Lea & Febiger; 1973. pp. 35–47. [Google Scholar]
- Vreeland D.L, Reader A, Beck M, Meyers W, Weaver J. An evaluation of volumes and concentrations of lidocaine in human inferior alveolar nerve block. J Endod. 1989;15:6–12. doi: 10.1016/S0099-2399(89)80091-3. [DOI] [PubMed] [Google Scholar]
- Nusstein J, Reader A, Beck F.M. Anesthetic efficacy of different volumes of lidocaine with epinephrine for inferior alveolar nerve blocks. Gen Dent. 2002;50:372–375. [PubMed] [Google Scholar]
- Meechan J.G, Robb N.D, Seymour R.A. Pain and Anxiety Control for the Conscious Dental Patient. Oxford, England: Oxford University Press; 1998. pp. 101–107. [Google Scholar]
- Cowan A. A clinical evaluation of Xylocaine anesthesia. J Dent Res. 1955;35:824–839. doi: 10.1177/00220345560350060201. [DOI] [PubMed] [Google Scholar]
- Cowan A. Minimum dosage technique in the clinical comparison of representative modern local anesthetic agents. J Dent Res. 1964;43:1228–1249. doi: 10.1177/00220345640430063401. [DOI] [PubMed] [Google Scholar]
- Jensen M.P, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- Certosimo A.J, Archer R.D. A clinical evaluation of the electric pulp tester as an indicator of local anesthesia. Oper Dent. 1996;21:25–30. [PubMed] [Google Scholar]
- Dreven L.J, Reader A, Beck M, Meyers W.J, Weaver J. An evaluation of an electric pulp tester as a measure of analgesia in human vital teeth. J Endod. 1987;13:233–238. doi: 10.1016/s0099-2399(87)80097-3. [DOI] [PubMed] [Google Scholar]
- McDaniel K.F, Rowe N.H, Charbeneau G.T. Tissue response to an electric pulp tester. J Prosthet Dent. 1973;29:84–87. doi: 10.1016/0022-3913(73)90144-3. [DOI] [PubMed] [Google Scholar]
- Branco F.P, Ranali J, Ambrosano G.M, Volpato M.C. A double-blind comparison of 0.5% bupivacaine with 1∶200,000 epinephrine and 0.5% levobupivacaine with 1∶200,000 epinephrine for the inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endodon. 2006;101:442–447. doi: 10.1016/j.tripleo.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Hinkley S.A, Reader A, Beck M, Meyers W.J. An evaluation of 4% prilocaine with 1∶200,000 epinephrine and 2% mepivacaine with 1∶20,000 levonordefrin compared with 2% lidocaine with 1∶100,000 epinephrine for inferior alveolar nerve block. Anesth Prog. 1991;38:84–89. [PMC free article] [PubMed] [Google Scholar]
- Kanaa M.D, Meechan J.G, Corbett I.P, Whitworth J.M. Efficacy and discomfort associated with slow and rapid inferior alveolar nerve block injection. J Endod. 2006;32:919–923. doi: 10.1016/j.joen.2006.04.004. [DOI] [PubMed] [Google Scholar]
- McLean C, Reader A, Beck M, Meyers W.J. An evaluation of 4% prilocaine and 3% mepivacaine compared with 2% lidocaine (1∶100,000 epinephrine) for inferior alveolar nerve block. J Endod. 1993;19:146–150. doi: 10.1016/s0099-2399(06)80510-8. [DOI] [PubMed] [Google Scholar]
- Meechan J.G, Kanaa M.D, Corbett I.P, Whitworth J.M. Pulpal anaesthesia for mandibular permanent first molar teeth: a comparison of buccal and buccal plus lingual infiltration injections. Int Endod J. 2006;39:764–769. doi: 10.1111/j.1365-2591.2006.01144.x. [DOI] [PubMed] [Google Scholar]
- Nusstein J, Wood M, Reader A, Beck M, Weaver J. Comparison of the degree of pulpal anesthesia achieved with the intraosseous injection and infiltration injection using 2% lidocaine with 1∶100,000 epinephrine. Gen Dent. 2005;53:50–53. [PubMed] [Google Scholar]
- Teplitsky P.E, Hablichek C.A, Kushneriuk J.S. A comparison of bupivacaine to lidocaine with respect to duration in the maxilla and mandible. J Can Dent Assoc. 1987;53:475–478. [PubMed] [Google Scholar]
- Tofoli G.R, Ramacciato J.C, de Oliveira P.C, Volpato M.C, Groppo F.C, Ranali J. Comparison of effectiveness of 4% articaine associated with 1∶100,000 or 1∶200,000 epinephrine in inferior alveolar nerve block. Anesth Prog. 2003;50:164–168. [PMC free article] [PubMed] [Google Scholar]
- Volpato M.C, Ranali J, Ramacciato J.C, de Oleveira P.C, Ambrosano G.M, Groppo F.C. Anesthetic efficacy of bupivacaine solutions in inferior alveolar nerve block. Anesth Prog. 2005;52:132–135. doi: 10.2344/0003-3006(2005)52[132:AEB]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielsson K, Evers H, Nordenram A. Long-acting local anesthetics in oral surgery: an experimental evaluation of bupivacaine and etidocaine for oral infiltration anesthesia. Anesth Prog. 1985;32:65–68. [PMC free article] [PubMed] [Google Scholar]
- Haas D.A, Harper D.G, Saso M.A, Young E.R. Lack of differential effect by Ultracaine (articaine) and Citanest (prilocaine) in infiltration anaesthesia. J Can Dent Assoc. 1991;57:217–223. [PubMed] [Google Scholar]
- Kennedy M, Reader A, Beck M, Weaver J. Anesthetic efficacy of ropivacaine in maxillary anterior infiltration. Oral Surg Oral Med Oral Pathol Oral Radiol Endodon. 2001;91:406–412. doi: 10.1067/moe.2001.114000. [DOI] [PubMed] [Google Scholar]
- Petersen J.K, Luck H, Kristensen F, Mikkelsen L. A comparison of four commonly used local analgesics. Int J Oral Surg. 1977;6:51–59. doi: 10.1016/s0300-9785(77)80059-8. [DOI] [PubMed] [Google Scholar]
- Axelsson S, Isacsson G. The efficacy of ropivacaine as a dental local anaesthetic. Swed Dent J. 2004;28:85–91. [PubMed] [Google Scholar]
- Knoll-Kohler E, Fortsch G. Pulpal anesthesia dependent on epinephrine dose in 2% lidocaine: a randomized controlled double-blind crossover study. Oral Surg Oral Med Oral Pathol Oral Radiol Endodon. 1992;73:537–540. doi: 10.1016/0030-4220(92)90091-4. [DOI] [PubMed] [Google Scholar]
- Nordenram A, Danielsson K. Local anaesthesia in elderly patients: an experimental study of oral infiltration anaesthesia. Swed Dent J. 1990;14:19–24. [PubMed] [Google Scholar]
- Haas D.A, Harper D.G, Saso M.A, Young E.R. Comparison of articaine and prilocaine anesthesia by infiltration in maxillary and mandibular arches. Anesth Prog. 1990;37:230–237. [PMC free article] [PubMed] [Google Scholar]
- Moore P.A, Boynes S.G, Hersh E.V, et al. The anesthetic efficacy of 4 percent articaine 1∶200,000 epinephrine: two controlled clinical trials. J Am Dent Assoc. 2006;137:1572–1581. doi: 10.14219/jada.archive.2006.0093. [DOI] [PubMed] [Google Scholar]
- Costa C.G, Tortamano I.P, Rocha R.G, Francischone C.E, Tortamano N. Onset and duration periods of articaine and lidocaine on maxillary infiltration. Quintessence Int. 2005;36:197–201. [PubMed] [Google Scholar]
- Oliveira P.C, Volpato M.C, Ramacciato J.C, Ranali J. Articaine and lignocaine efficiency in infiltration anaesthesia: a pilot study. Br Dent J. 2004;197:45–46. doi: 10.1038/sj.bdj.4811422. [DOI] [PubMed] [Google Scholar]
- Jorkjend L, Skoglund L.A. Increase in volume of lignocaine/adrenaline-containing local anaesthetic solution causes increase in acute postoperative pain after gingivectomy. Br J Oral Maxillofac Surg. 2000;38:230–234. doi: 10.1054/bjom.1999.0447. [DOI] [PubMed] [Google Scholar]
- Collins S.L, Moore A, McQuay H.J. The visual analogue pain intensity scale: what is moderate pain in millimetres. Pain. 1997;72:95–97. doi: 10.1016/s0304-3959(97)00005-5. [DOI] [PubMed] [Google Scholar]
- Meechan J.G, Day P.F. A comparison of intra-oral injection discomfort produced by plain and epinephrine-containing lidocaine local anesthetic solutions: a randomised, double-blind, split mouth, volunteer investigation. Anesth Prog. 2002;49:44–48. [PMC free article] [PubMed] [Google Scholar]