Abstract
Objectives. We examined the relationship of regular exercise and body weight to disability among healthy seniors.
Methods. We assessed body mass index (BMI) and vigorous exercise yearly (1989–2002) in 805 participants aged 50 to 72 years at enrollment. We studied 4 groups: normal-weight active (BMI< 25 kg/m2; exercise> 60 min/wk); normal-weight inactive (exercise≤ 60 min/wk); overweight active (BMI≥ 25 kg/m2); and overweight inactive. Disability was measured with the Health Assessment Questionnaire (0–3; 0= no difficulty, 3= unable to do). We used multivariable analysis of covariance to determine group differences in disability scores after adjustment for determinants of disability.
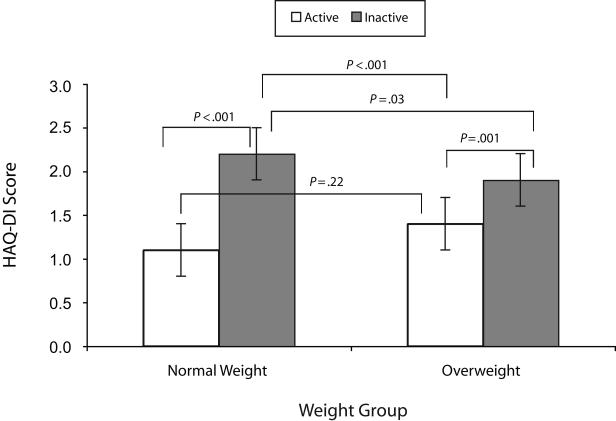
Results. The cohort was 72% men and 96% White, with a mean age of 65.2 years. After 13 years, overweight active participants had significantly less disability than did overweight inactive (0.14 vs 0.19; P= .001) and normal-weight inactive (0.22; P= .03) participants. Similar differences were found between normal-weight active (0.11) and normal-weight inactive participants (P< .001).
Conclusions. Being physically active mitigated development of disability in these seniors, largely independent of BMI. Public health efforts that promote physically active lifestyles among seniors may be more successful than those that emphasize body weight in the prevention of functional decline.
The United States is experiencing a senior “boom” as increasing numbers of adults are living longer and healthier than their parents. By 2030, older adults will compose about 20% of the US population.1 However, this group even now poses enormous challenges to policymakers and health care providers to meet their needs. Older adults are the largest consumers of health care. Five of the 6 leading causes of death among seniors are from chronic diseases1 that can be in part prevented, delayed, or modified through lifestyle.
The identification of strategies to help maintain health and independence as far into the last years of life as possible is of foremost importance to help alleviate the increasing public health burden. However, the sweeping national epidemic of overweight and obesity as indicated by a body mass index (BMI; weight in kilograms divided by height in meters squared) of 25 kg/m2 or more in parallel with the small proportion of the elderly who are sufficiently physically active to achieve health benefits are among major pubic health concerns. More than two thirds of seniors aged 65 to 75 years have a BMI greater than 25 kg/m2, and nearly three fourths are physically inactive.1 Being overweight and physically inactive are recognized risk factors for several chronic diseases and are also important predictors of functional impairment, or disability, among older adults.3–7
Functional limitations in turn have been shown to contribute to poorer health outcomes and increased health care utilization.3,8,9 Nearly 40% of overweight older adults have impaired physical functioning to the extent that it limits their ability to perform common activities of daily living, including walking and reaching.10 Moreover, as weight increases, physical activity decreases, and functional impairment increases.11,12
Physical activity confers myriad health benefits across age groups and among both normal-weight and overweight individuals.6,13,14 Participation in regular physical activity helps to moderate or prevent disability and improves functional ability, especially among seniors. Mortality and morbidity are also positively affected among seniors who participate in regular physical activity.15 As such, physically active older adults demonstrate higher levels of physical functioning than their inactive counterparts.10,16
Healthy weight maintenance and regular participation in physical activity are important goals of public health initiatives.17 In older adults, investigators have compared physical activity with functional status,18,19 body weight with functional status,3,7,8 and overweight and obesity with physical activity11,20 and have reported lower disability both in overweight and nonoverweight participants who were physically active. In cross-sectional studies of the association between leisure-time physical activity, obesity, and disability among aging men21 and aging women,22 the most disability was found among inactive participants.
However, there are little longitudinal data evaluating the specific relationship between disability, body weight, and physical activity among older healthy men and women, and more specifically those who are classed as overweight and who participate in regular physical activity. Brach et al.20 examined this relationship in older women in both cross-sectional and longitudinal studies over 17 years of follow-up and reported less disability in physically active overweight and obese women, although they were unable to control for baseline disability. In their 16-year study of living habits, obesity, and mortality in middle-aged and older Finnish men, Haapenen-Niemi et al.23 concluded that being obese was not an independent predictor of mortality, although low levels of physical activity, perceived physical fitness, and physical functioning predicted increased risk. In a cohort of older adults from the Health, Aging, and Body Composition Study, Houston et al. found that excess weight was linked with objective measures of physical performance.4
Our primary objective was to examine the relationship of body weight and physical activity to disability in a cohort of healthy, older adults over 13 years of follow-up. We hypothesized that physically active overweight and normal-weight seniors would have less disability than their less-active counterparts.
METHODS
Participants were from a cohort of 1195 adults who were recruited between 1984 and 1991 from a national runners’ association and from the local Stanford University community to participate in a longitudinal prospective study of the health effects of running.24 Men and women were eligible for study inclusion at time of enrollment if they were aged 50 to 72 years, had at least a high school diploma, and spoke English as their primary language.24 There were no inclusion criteria regarding physical activity level. An earlier publication described the original cohort as being better educated and having more professionals than national population samples at the time.24 Runners’ association members were also younger, included more men, had significantly lower BMIs, and the biggest difference was the number of miles run, compared with the community controls.24
Data for this study originated in 1989, the first year that data for all relevant variables were available (e.g., weight, physical activity, and disability). Participant selection was based on availability of relevant data regardless of original group membership (i.e., whether from the runners’ group or community sample). In addition, investigators were blinded to original group membership. Participants were eligible for this study if they had at least 2 years of follow-up with weight, physical activity, and disability data during the 13-year study period, from 1989 to 2002. Overall, two thirds (66.5%) of the participants had an average of at least 11 years of follow-up data, which ranged from 2 to 13 years. The study protocol was approved by Stanford University’s Administrative Panel on Human Subjects in Medical Research, and each participant gave written informed consent.
Data Collection
Self-report data were collected yearly by mail with the Stanford Health Assessment Questionnaire (HAQ).25 Rigorous, standardized protocols were followed for data collection and quality control. These included follow-up telephone calls to nonrespondents and review of all returned questionnaires for completeness, ambiguities, or inconsistencies, with subsequent telephone contact as needed by trained outcome assessors.25
Demographic and health data.
Participant characteristics (age, gender, years of education, race/ethnicity, years of follow-up, disability, medical history, exercise, smoking status, comorbid conditions, pain, and global health status) were obtained by self-report. Racial/ethnic groups were derived from patient self-identification as non-Hispanic White, non-Hispanic African American, Asian or Pacific Islander, American Indian/Alaskan Native, Canadian Indian, Hispanic, or other. Smoking status was assessed by whether respondents were currently smoking cigarettes. Comorbidity data were obtained by asking respondents if they had ever been told by a physician that they had cardiovascular, pulmonary, neurological, endocrinological, gastrointestinal, or musculoskeletal conditions, or cancer. Assessment of overall health and vitality was measured on the Health Assessment Questionnaire’s (HAQ’s) double-anchored global health visual analog scale (scored 0–100; 100 = very healthy). The HAQ global health scale has been validated as a “generic” measure of health-related quality of life.26
Assessment of disability.
Disability was assessed with the Stanford HAQ Disability Index (HAQ-DI),25 which includes items that evaluate fine movements of the upper extremity, locomotor activity of the lower extremity, and activities that involve both upper and lower extremities. The HAQ-DI contains 20 items in 8 categories of functioning—rising, dressing, eating, walking, hygiene, reaching, gripping, and ability to do usual daily activities. Responses are made on a scale from 0 (no difficulty) to 3 (unable to do). The maximum item scores in each of the 8 categories were summed, then averaged, to obtain an overall HAQ-DI from 0 (no disability) to 3 (completely disabled). The HAQ-DI has been extensively studied and is valid and sensitive to change.25
Assessment of physical activity.
Physical activity was assessed as the number of minutes spent weekly doing vigorous exercise. Vigorous exercise was defined on the questionnaire as “vigorous exercise that will cause you to sweat and your pulse, if taken, will be above 120.” Activities under this definition included running, swimming, bicycling or using a stationary bike, aerobic dance and exercise, stair steppers, brisk walking, hiking or using a treadmill, racket sports, and also periods of rapid walking at work and in daily activities. For convenience, we chose to use the terms “active” and “inactive” to describe physical activity groups in this study. Participants were categorized as active if they participated in vigorous exercise for more than 60 minutes per week or inactive if they participated in vigorous exercise for 60 minutes or fewer per week.
Assessment of body weight.
Self-reported body weight was classified by BMI. Participants were categorized as either normal weight (< 25 kg/m2) or overweight (≥ 25 kg/m2) in accord with the National Institutes of Health Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults.2 Frequency of obesity (≥ 30 kg/m2) among participants was also examined.
Study Groups
We formed 4 study groups based on BMI and vigorous exercise level on the 1989 questionnaire, the first year that data were available for all variables relevant to this study, or on the respondent’s first questionnaire, which could have ranged from 1989 to 1991. Accordingly, respondents were assigned to normal-weight active (BMI<25 kg/m2; exercise>60 min/wk); normal-weight inactive (exercise≤ 60 min/wk); overweight (BMI≥ 25 kg/m2) active; or overweight inactive.
Statistical Analyses
The primary comparisons for analysis were the active participants compared with the inactive participants within each weight group. The HAQ-DI score was the primary dependent outcome variable. The covariates chosen for the model were correlated with disability at P< .05. These were age, gender, ethnicity (categorized as White or non-White, because numbers of participants in specific racial/ethnic groups were too small to analyze separately), education (years), number of comorbid conditions, and baseline HAQ-DI score. We also tested the data for any interactions between weight and exercise at baseline.
Baseline differences in the HAQ-DI score and covariates between the 2 exercise groups within each weight group were compared using the χ2 and 2-tailed t tests. Comparisons at P< .05 were considered statistically significant. Multivariable analysis of covariance with disability as the dependent variable was used to determine differences among the active and inactive participants and the weight groups after adjustment. We used generalized estimating equations, a method of parameter estimation analysis of longitudinal data that includes repeated measures of an individual or cluster of individuals over time.27 Thus, changes in covariates were taken into account in the multivariable analyses. Analyses were performed in a staged manner to examine the impact of specific covariates on group differences and were conducted with SAS version 9.1 (SAS Institute Inc, Cary, North Carolina).
RESULTS
Our findings were based on the 805 participants from the original cohort of 1195 men and women who had weight, exercise, and disability data and met this study’s criterion of having at least 2 years of follow-up during the study period (1989–2002). In the cohort, 57% (n = 460) of the participants were from the runners’ association group and 43% (n = 345) were from the community sample. Participants’ characteristics mirrored that of the original cohort; the majority were well-educated White men.
Of all participants, 70% (n = 565) had a normal BMI of less than 25 kg/m2. Of normal-weight participants, 78% (n=442) fell into the active group (exercise > 60 min/wk), whereas 64% (n = 153) of the overweight group was active. About 14% (n = 33) of the overweight participants were obese (≥ 30 kg/m2), composing 6% (n = 14) of the overweight active group and 8% (n = 19) of the overweight inactive group.
Baseline values by study group are presented in Table 1 ▶ and show few differences among the groups. The study cohort was predominantly White (96%) and well-educated (> 16 years of education). There were significantly more physically active men than inactive men in both weight groups (P< .05 for each weight group). The normal-weight inactive participants were slightly older than their physically active counterparts (66.6 years vs 64.8 years; P< .05), and the age difference between the overweight inactive and active participants was similar (66.0 years vs 65.1 years; P> .05).
TABLE 1—
Baseline Participant Characteristics Among 805 Healthy US Seniors: 1989–2002
| Normal Weighta | Overweightb | |||
| Physically Activec (n = 442) | Physically Inactived (n = 123) | Physically Activec (n = 153) | Physically Inactived (n = 87) | |
| White, % | 96 | 95 | 98 | 98 |
| Men, % | 74 | 53* | 83 | 67* |
| Age, y, mean (SE) | 64.8 (0.3) | 66.6 (0.6)* | 65.1 (0.5) | 66.0 (0.7) |
| Education, y, mean (SE) | 16.6 (0.1) | 16.5 (0.2) | 16.8 (0.2) | 16.1 (0.3) |
| Follow-up, y, mean (SE) | 11.5 (0.2) | 10.9 (0.4) | 11.2 (0.3) | 10.7 (0.5) |
| Comorbid conditions, no. (SE) | 0.07 (0.01) | 0.15 (0.02) | 0.09 (0.02) | 0.14 (0.04) |
| Smokers, % | 7 | 2* | 9 | 3* |
| Global health scoree, mean (SE) | 84.2 (0.6) | 73.6 (1.7)* | 79.9 (1.2) | 74.2 (1.4)* |
| HAQ-DI scoref, mean (SE) | 0.07 (0.01) | 0.16 (0.02)* | 0.12 (0.02) | 0.17 (0.03) |
| Exercise, min/wk, mean (SE) | 302.7 (9.8) | 15.7 (2.1)* | 251.0 (14.2) | 12.3 (2.4)* |
| BMI, kg/m2, mean (SE) | 22.2 (0.8) | 22.3 (0.2) | 27.1 (0.2) | 28.3 (0.3)* |
Note. HAQ-DI = Stanford Health Assessment Questionnaire Disability Index; BMI = body mass index.
aDefined as a BMI of < 25 kg/m2.
bDefined as a BMI of ≥ 25 kg/m2.
cDefined as vigorous exercise for more than 60 minutes per week.
dDefined as vigorous exercise for 60 minutes or less per week.
eMeasured 0 to 100; 100 = very healthy.
fMeasured 0 to 3; 0 = no difficulty, 3 = unable to do.
* P < .05, between the active and inactive categories within weight group.
We found a significant interaction between weight and exercise, because as body weight increased, exercise decreased. This was not unexpected, because research has shown that heavier individuals tend to exercise less.11,12 Years of follow-up did not differ among study groups. Comorbidities were infrequent in all groups, indicating that this was a relatively healthy cohort, but were slightly higher in the inactive compared with active participants. Overall, smoking prevalence was low, but in both weight groups, there was a smaller proportion of smokers in the physically inactive than active groups (P< .05). Within each weight group, the physically inactive participants reported statistically poorer overall health (P< .05).
Although baseline disability was low in all groups, it was higher in the normal-weight physically inactive participants (P< .05) compared with their active counterparts. Baseline disability also trended higher among the overweight inactive respondents compared with their active peers (P= .07). By design, exercise minutes were significantly higher in active compared with inactive participants in both weight groups (P< .05). Body mass index was slightly higher in the overweight inactive versus overweight active participants (28.3 vs 27.1; P< .05), but was nearly identical when physical activity groups were compared in the normal-weight participants (22.2 vs 22.3; P> .05).
Data for the staged multivariable analyses by weight group with disability as the dependent variable are presented in Table 2 ▶. The full model included adjustment for age, gender, race/ethnicity (White vs non-White), education years, smoking status, number of co-morbid conditions, and baseline HAQ-DI score. After adjustment, the physically inactive participants had significantly more disability than the active participants regardless of weight group.
TABLE 2—
Adjusted HAQ-DI Scores for Staged Multivariable Analysis of Covariance for Differences Between Physical Activity Groups Within Each Weight Group Among 805 US Seniors: 1989–2002
| Normal Weighta | Overweightb | |||
| Physically Activec (n = 442), Mean (SE) | Physically Inactived (n = 123), Mean (SE) | Physically Activec (n = 153), Mean (SE) | Physically Inactived (n = 87), Mean (SE) | |
| Age only | 0.09 (0.01) | 0.28** (0.03) | 0.16 (0.02) | 0.26** (0.02) |
| Age + gender | 0.12 (0.01) | 0.28** (0.03) | 0.20 (0.02) | 0.28** (0.02) |
| Age + race/ethnicitye | 0.09 (0.02) | 0.25** (0.03) | 0.16 (0.02) | 0.25** (0.03) |
| Age + education | 0.09 (0.02) | 0.25** (0.03) | 0.16 (0.02) | 0.25** (0.03) |
| Age + smoking | 0.07 (0.03) | 0.24** (0.04) | 0.15 (0.03) | 0.24** (0.04) |
| Age + number of comorbid conditions | 0.08 (0.03) | 0.24** (0.04) | 0.15 (0.03) | 0.24** (0.04) |
| Age + baseline HAQ-DI score | 0.11 (0.03) | 0.22** (0.03) | 0.14 (0.03) | 0.19* (0.03) |
Note. HAQ-DI = Stanford Health Assessment Questionnaire Disability Index. Having a disability was the reference variable.
aDefined as a body mass index (BMI) of < 25 kg/m2.
bDefined as a BMI of ≥ 25 kg/m2.
cDefined as vigorous exercise for more than 60 minutes per week.
dDefined as vigorous exercise for 60 minutes or less per week.
eWhite vs non-White.
* P = .001; **P < .001, between active and inactive categories within weight group.
Figure 1 ▶ presents adjusted data by both weight and physical activity group showing the differences among groups. Physically inactive participants in both weight groups had the highest levels of disability. Overweight active participants had significantly less disability than their normal-weight inactive counterparts (0.14 vs 0.22; P< .001). Normal-weight active participants had the lowest disability, which was significantly different from the other groups, except for their overweight peers.
FIGURE 1—
Selected adjusted mean (SE) disability scores, by weight and activity group.
Note. HAQ-DI = Stanford Health Assessment Questionnaire Disability Index; BMI = body mass index. Normal weight was defined as a BMI of less than 25 kg/m2; overweight was defined as a BMI of 25 kg/m2 or more. Data were adjusted for age, gender, race/ethnicity (White vs non-White), education, smoking status, comorbidities, and baseline disability. Active (exercise > 60 min/wk), Inactive (exercise ≤ 60 min/wk).
DISCUSSION
Results from this longitudinal study of healthy seniors with 13 years of observation support the hypothesis that being physically active helps mitigate development of disability, largely independent of weight status. We found significantly less disability among both the overweight active and normal-weight active participants compared with their inactive counterparts, which is consistent with previous research by our group28 as well as with Brach et al.’s longitudinal analysis of older women.20
These findings likewise contribute to the body of evidence documenting that regular physical activity postpones disability, and that seniors who are physically active report superior physical functioning compared with those who do little or no physical activity.19,29,30 They further suggest that physical activity is an important factor and may be a more compelling component than body weight in mitigating development of disability in older adults.31–33 There are also plausible biological factors supporting these findings, which demonstrate that physically active overweight adults have improved physical indicators of health status, such as muscle strength and bone density, which contribute to better functional ability.14,15,30 In addition, data support lower risks of morbidity and mortality, such as cardiovascular disease and diabetes, in this population.6,30
Strengths and Limitations
The strengths of our study included the advantage of having been able to study a cohort of healthy aging seniors with initial low levels of disability, rather than a subset of seniors who were frail or ill, in whom initial disability may have been a confounding factor.3,34 Ours is also one of the few longitudinal studies that has examined these factors and used functional status as the primary outcome variable. Moreover, we had access to comprehensive annual data and used a longitudinal study design that enabled the assessment of disability progression over 13 years. Use of repeated-measures analyses27 that took into account intraparticipant correlations over time helped to improve the estimation of model parameters and to control for temporal changes in covariates that could affect the outcome, including age, gender, ethnicity, race, smoking, and comorbidities. In addition, because we controlled for baseline disability, we could infer with some confidence that these results were independent of initial functional status.
Despite these strengths, there are factors that limit the generalizability of our findings. These include the homogeneous nature of the cohort, which was predominantly well-educated White men. As such, this cohort may not represent a broader range of apparently healthy seniors who may have different or less-healthy lifestyles. These findings may not be applicable to aging seniors such as women, other ethnic groups, the less-educated, the morbidly obese, heavy smokers, seniors who are ill or frail, or to octogenarians or older-aged individuals. We also based physical activity levels on the amount of vigorous activity compared with other studies that have used less-vigorous kinds of activity such as walking.20 Data on moderate or light activities were not collected in earlier years of this study, thus the impact of less-vigorous activity could not be assessed. Consequently, whether the same results would accrue for the casually or lightly exercising senior is unknown. Use of BMI to classify individuals also may have influenced the findings because BMI is not an entirely accurate measure of body composition and may result in misclassification of certain groups, such as the elderly.2 In this study, higher BMI among exercising individuals may have been associated with greater muscle mass, whereas the same BMI among inactive individuals may have been associated with greater adiposity.
On the other hand, the cohort’s homogeneity may favor these findings by limiting the number of potential factors that could confound results, such as education and access to health care. Also, there are no compelling reasons to presume that benefits accrued from participating in regular physical activity would differ substantially for other groups of seniors, because these results are consistent with an increasing evidence base that supports improved functional status in diverse cohorts of physically active older adults, including women,19 Blacks,33 and Asians.35,32
Although self-selection by study participants may affect the strength of the association and cannot be ruled out completely, all participants from the original cohort were included in this study based solely on the availability of data relevant to this investigation. We had no knowledge of original group membership or other variables of interest. Thus, there is no reason to expect that the data would be systematically affected by recruitment source. In addition, validation studies of reporting bias of physical function in this cohort have shown no intergroup differences in self-report.24 Despite these factors, this cohort may have been distinctive in characteristics not captured in analyses, but that may be in some way linked with exercise, weight, and disability in aging.
All the same, these findings should be interpreted with caution. They should not be construed to imply that if people are overweight and are physically active then they do not need to be at a relatively healthy weight. Obesity is one of the nation’s most prevalent epidemics of modern times and is among the most compelling current public health concerns. Regular physical activity in and of itself is one of the principal means by which energy balance can be enhanced to promote a healthy weight.36
Conclusions
With life expectancy increasing, delaying or preventing physical disability in the elderly is a key global issue, although many questions have yet to be answered about the best and most appropriate strategies for achieving this goal. The rapidly growing numbers of seniors,1 the escalating epidemic of overweight and obesity,37 the established relationship between excess body weight and disability,8,11 and the lack of consistently effective interventions for long-term weight loss2 indicate that modifiable risk factors need to be identified to inform public health and clinical recommendations so that interventions to help delay onset of disability or improve functional status can be developed. It may be more attainable for overweight individuals to become physically active than to lose body weight and sustain that reduction. Shifting some public health efforts to focus on preventive approaches to reduce functional impairment associated with overweight through physical activity rather than to emphasize body weight issues may be a more viable strategy.
Peer Reviewed
Contributors B. Bruce originated the study, conducted analyses, and participated in development and revision of the article. J. F. Fries and H. Hubert assisted with the study and participated in analyses and article development and finalization. All authors helped to conceptualize ideas, interpret findings, and review and revise drafts of the article.
Human Participant Protection The study protocol was approved by Stanford University’s Administrative Panel on Human Subjects in Medical Research, and each participant gave written informed consent.
References
- 1.Older Americans 2004: Key Indicators of Well-Being. Washington, DC: Federal Interagency Forum on Aging-Related Statistics; 2004.
- 2.[No authors listed.] Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Arch Intern Med. 1998;158:1855–1867. [DOI] [PubMed] [Google Scholar]
- 3.Jenkins KR. Obesity’s effects on the onset of functional impairment among older adults. Gerontologist. 2004;44:206–216. [DOI] [PubMed] [Google Scholar]
- 4.Houston DK, Ding J, Nicklas BJ, et al. The association between weight history and physical performance in the Health, Aging and Body Composition study. Int J Obes (Lond). 2007;31:1680–1687. [DOI] [PubMed] [Google Scholar]
- 5.Villareal DT, Apovian CM, Kushner RF, Klein S. Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res. 2005;13: 1849–1863. [DOI] [PubMed] [Google Scholar]
- 6.Blair SN, Brodney S. Effects of physical inactivity and obesity on morbidity and mortality: current evidence and research issues. Med Sci Sports Exerc. 1999; 31(suppl 11):S646–S662. [DOI] [PubMed] [Google Scholar]
- 7.Jensen GL, Friedmann JM. Obesity is associated with functional decline in community-dwelling rural older persons. J Am Geriatr Soc. 2002;50:918–923. [DOI] [PubMed] [Google Scholar]
- 8.Ferraro KF, Su YP, Gretebeck RJ, Black DR, Badylak SF. Body mass index and disability in adulthood: a 20-year panel study. Am J Public Health. 2002;92: 834–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jenkins KR. Body-weight change and physical functioning among young old adults. J Aging Health. 2004;16:248–266. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Prevalence of physical inactivity during leisure time among overweight persons—Behavioral Risk Factor Surveillance System, 1994. MMWR Morb Mortal Wkly Rep. 1996;45:185–188. [PubMed] [Google Scholar]
- 11.Goya Wannamethee S, Gerald Shaper A, Whincup PH, Walker M. Overweight and obesity and the burden of disease and disability in elderly men. Int J Obes Relat Metab Disord. 2004;28:1374–1382. [DOI] [PubMed] [Google Scholar]
- 12.Apovian CM, Frey CM, Wood GC, Rogers JZ, Still CD, Jensen GL. Body mass index and physical function in older women. Obes Res. 2002;10:740–747. [DOI] [PubMed] [Google Scholar]
- 13.Lee CD, Blair SN, Jackson AS. Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. Am J Clin Nutr. 1999; 69:373–380. [DOI] [PubMed] [Google Scholar]
- 14.Stevens J, Cai J, Evenson KR, Thomas R. Fitness and fatness as predictors of mortality from all causes and from cardiovascular disease in men and women in the lipid research clinics study. Am J Epidemiol. 2002; 156:832–841. [DOI] [PubMed] [Google Scholar]
- 15.[No authors listed.] American College of Sports Medicine Position Stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 1998;30: 992–1008. [PubMed] [Google Scholar]
- 16.Spirduso WW, Cronin DL. Exercise dose-response effects on quality of life and independent living in older adults. Med Sci Sports Exerc. 2001;33(6 suppl):S598–S608; discussion S609–S610. [DOI] [PubMed] [Google Scholar]
- 17.Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington DC: Dept of Health and Human Services; 2000.
- 18.Miller ME, Rejeski WJ, Reboussin BA, Ten Have TR, Ettinger WH. Physical activity, functional limitations, and disability in older adults. J Am Geriatr Soc. 2000;48:1264–1272. [DOI] [PubMed] [Google Scholar]
- 19.Huang Y, Macera CA, Blair SN, Brill PA, Kohl HW III, Kronenfeld JJ. Physical fitness, physical activity, and functional limitation in adults aged 40 and older. Med Sci Sports Exerc. 1998;30:1430–1435. [DOI] [PubMed] [Google Scholar]
- 20.Brach JS, VanSwearingen JM, FitzGerald SJ, Storti KL, Kriska AM. The relationship among physical activity, obesity, and physical function in community-dwelling older women. Prev Med. 2004;39:74–80. [DOI] [PubMed] [Google Scholar]
- 21.Di Francesco V, Zamboni M, Zoico E, et al. Relationships between leisure-time physical activity, obesity and disability in elderly men. Aging Clin Exp Res. 2005;17:201–206. [DOI] [PubMed] [Google Scholar]
- 22.Sulander T, Martelin T, Rahkonen O, Nissinen A, Uutela A. Associations of functional ability with health-related behavior and body mass index among the elderly. Arch Gerontol Geriatr. 2005;40:185–199. [DOI] [PubMed] [Google Scholar]
- 23.Haapanen-Niemi N, Miilunpalo S, Pasanen M, Vuori I, Oja P, Malmberg J. Body mass index, physical inactivity and low level of physical fitness as determinants of all-cause and cardiovascular disease mortality—16 y follow-up of middle-aged and elderly men and women. Int J Obes Relat Metab Disord. 2000;24: 1465–1474. [DOI] [PubMed] [Google Scholar]
- 24.Lane NE, Bloch DA, Wood PD, Fries JF. Aging, long-distance running, and the development of musculoskeletal disability. A controlled study. Am J Med. 1987;82:772–780. [DOI] [PubMed] [Google Scholar]
- 25.Bruce B, Fries JF. The Stanford Health Assessment Questionnaire: a review of its history, issues, progress, and documentation. J Rheumatol. 2003;30: 167–178. [PubMed] [Google Scholar]
- 26.Fries JF, Ramey DR. “Arthritis specific” global health analog scales assess “generic” health related quality-of-life in patients with rheumatoid arthritis. J Rheumatol. 1997;24:1697–1702. [PubMed] [Google Scholar]
- 27.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73: 13–22. [Google Scholar]
- 28.Wang BW, Ramey DR, Schettler JD, Hubert HB, Fries JF. Postponed development of disability in elderly runners: a 13-year longitudinal study. Arch Intern Med. 2002;162:2285–2294. [DOI] [PubMed] [Google Scholar]
- 29.Stewart KJ, Turner KL, Bacher AC, et al. Are fitness, activity, and fatness associated with health-related quality of life and mood in older persons? J Cardiopulm Rehabil. 2003;23:115–121. [DOI] [PubMed] [Google Scholar]
- 30.Bean JF, Vora A, Frontera WR. Benefits of exercise for community-dwelling older adults. Arch Phys Med Rehabil. 2004;85(7 suppl 3):S31–S42; quiz S43–S44. [DOI] [PubMed] [Google Scholar]
- 31.LaCroix AZ, Guralnik JM, Berkman LF, Wallace RB, Satterfield S. Maintaining mobility in late life. II. Smoking, alcohol consumption, physical activity, and body mass index. Am J Epidemiol. 1993;137: 858–869. [DOI] [PubMed] [Google Scholar]
- 32.Simonsick EM, Lafferty ME, Phillips CL, et al. Risk due to inactivity in physically capable older adults. Am J Public Health. 1993;83:1443–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clark DO. The effect of walking on lower body disability among older blacks and whites. Am J Public Health. 1996;86:57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hamerman D. Toward an understanding of frailty. Ann Intern Med. 1999;130:945–950. [DOI] [PubMed] [Google Scholar]
- 35.Wu SC, Leu SY, Li CY. Incidence of and predictors for chronic disability in activities of daily living among older people in Taiwan. J Am Geriatr Soc. 1999; 47:1082–1086. [DOI] [PubMed] [Google Scholar]
- 36.Brooks GA, Butte NF, Rand WM, Flatt JP, Caballero B. Chronicle of the Institute of Medicine physical activity recommendation: how a physical activity recommendation came to be among dietary recommendations. Am J Clin Nutr. 2004;79:921S–930S. [DOI] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. State-specific prevalence of obesity among adults—United States, 2005. MMWR Morb Mortal Wkly Rep. 2006; 55:985–988. [PubMed] [Google Scholar]