Abstract
Objectives. We examined the relation of individual-level perceived discrimination to mortality in a biracial, population-based sample.
Methods. Participants were 4154 older adults from the Chicago Health and Aging Project who underwent up to 2 interviews over 4.5 years. Perceived discrimination was measured at baseline, and vital status was obtained at each follow-up and verified through the National Death Index.
Results. During follow-up, 1166 deaths occurred. Participants reporting more perceived discrimination had a higher relative risk of death (hazard ratio [HR]= 1.05; 95% confidence interval [CI]=1.01, 1.09). This association was independent of differences in negative affect or chronic illness and appeared to be stronger among Whites than among Blacks (Whites: HR=1.12; 95% CI=1.04, 1.20; Blacks: HR=1.03; 95% CI=0.99, 1.07). Secondary analyses revealed that the relation to mortality was related to discriminatory experiences of a more demeaning nature and that racial differences were no longer significant when the sample was restricted to respondents interviewed by someone of the same race.
Conclusions. Perceived discrimination was associated with increased mortality risk in a general population of older adults. The results suggest that subjective experience of interpersonal mistreatment is toxic in old age. This study adds to a growing literature documenting discrimination as an important social determinant of health.
There is growing interest in the health effects of perceived discrimination.1,2 Although evidence has been mixed, several studies have demonstrated that discrimination is related to poor physical and mental health, including blood pressure,3,4 breast cancer,5 self-rated health,4,6–8 psychological distress,7–10 well-being10,11 and depressive symptoms.8,12 Several studies have reported no or conditional associations as well.13–18 Inconsistency in results may be because, at least in part, of the variation in the measurement of discrimination, differences in study methodologies and populations, and the variety of outcomes that have been considered.1,2 Overall, however, it appears that the results have been stronger for mental health than for physical health outcomes. Although the mechanisms are not clear, hypotheses include restricted access to socioeconomic resources, poor health behaviors, and stress responses.6,19–22
Few studies have focused on well-established clinical outcomes, such as hypertension. Although some studies have reported that discrimination increases the risk for hypertension,23,24 others have not found an association.13,14 Discrimination has also been linked with subclinical cardiovascular disease, including carotid intima-media thickness25 and coronary artery calcification.26
We examined perceived discrimination in relation to all-cause mortality for 2 reasons. First, this end point has rarely been considered in relation to discrimination.27,28 Second, mortality serves as the common end point of many disease processes that affect adult populations. Because the negative health effects of discrimination are thought to be nonspecific—that is, they are not restricted to a particular disease process—this end point may be particularly suitable to capture much of the spectrum of adverse outcomes associated with this risk factor.
Racism, racial discrimination, and perceived discrimination have been used interchangeably in the research literature. We focused on perceived discrimination, defined as the subjective experience of common forms of unfair treatment,10 and its relation to mortality in a population-based study of older Blacks and Whites. Because the weight of the current evidence shows that discrimination is associated with poorer health among minorities, we hypothesize that perceived discrimination is related to an increased risk for mortality and that this risk is stronger among Blacks than among Whites.
METHODS
Participants were residents of a geographically defined community who were enrolled in the Chicago Health and Aging Project, an ongoing, population-based longitudinal study of risk factors for Alzheimer disease. The study community consisted of 3 adjacent neighborhood areas in Chicago, Illinois, with large numbers of non-Hispanic Blacks and Whites and a broad representation in socioeconomic status (SES) across race. Residents 65 years and older were invited to participate in the study after a census was taken of all of the households in the community area. Of the 7813 eligible residents, 6158 were enrolled for an in-home, face-to-face baseline interview, for an overall participation rate of 78.9% (Blacks, 81.4%; Whites, 75.1%). Baseline interviews were conducted from 1993 to 1997, followed by successive interview cycles at approximately 3-year intervals. The interviews included structured questions on a range of sociodemographic characteristics, psychosocial variables, medical history, and physical and cognitive performance tests. Questions on perceived discrimination were added to the first follow-up interview (1997–2000), which served as a baseline for these analyses.
Perceived Discrimination
Perceived discrimination was assessed with a previously established 9-item measure.10 The scale assesses the subjective experience of being treated unfairly without reference to racism, discrimination, prejudice, or any demographic characteristics such as race, gender, or age. Respondents indicated how often they experienced 9 instances of discrimination, and the frequency was rated on a 4-point scale (3=often, 2=sometimes, 1=rarely, and 0=never). Following previous work with this measure,8,14 we recoded the responses to a binary format (often or sometimes=1, rarely or never=0) and then summed across items to get the total score (range=0–9), with higher scores indicating more discrimination.
The results of a previous factor analysis of the 9-item scale produced 2 factors.12 The first factor, consisting of 4 items, was called “unfair treatment” and represented a generic perception of rudeness: How often are you treated with less courtesy, treated with less respect, received poorer service, people acted as if they were better than you? The other factor, consisting of the remaining 5 items, was called “personal rejection” because the items represented a more overt form of demeaning character insults: How often do people act as if you are dishonest, act as if they are afraid of you, act as if you are not smart, call you names or insult you, threaten or harass you? We created summary measures of unfair treatment and personal rejection using the same method as described previously.
Control Variables and Mortality
Other variables include age (on the basis of date of birth), gender, race (non-Hispanic Black or non-Hispanic White), and SES. A composite measure of lifetime SES was constructed on the basis of 4 components of SES that characterize different stages of the life course, as previously described.29 The 4 components were (1) a measure of childhood SES that was based on parents’ years of education, father’s occupational prestige score (based on the respondents’ reports of their fathers’ occupational earning and educational requirements), and family financial status during childhood30; (2) the participant’s level of education; (3) occupational status at age 30 years; and (4) current income. We then calculated z scores for each of the 4 components and computed the average of the nonmissing values of each component. Intercorrelations between the 4 components ranged from 0.29 to 0.67 and had a moderate level of internal consistency, as shown by Cronbach’s coefficient α of 0.76, suggesting that the components were meaningfully related to each other and could be adequately summarized in a composite measure.
We considered 2 additional control variables, depressive symptoms and overall physical health status. Both have been found to be predictive of mortality among older adults31–33 and to vary by race34–36 and may be either potential confounders of the relation between perceived discrimination to mortality or lie in the causal chain between discrimination and mortality. Data on depressive symptoms and medical conditions were derived from the same follow-up interview (1997–2000) as the perceived discrimination data. Depressive symptoms were assessed with a 10-item short form37 of the Center for Epidemiological Studies Depression scale (CES-D),38 a self-report measure of current depressive symptoms, designed for use in community-based studies. The score was the number of symptoms experienced in the past week.
Seven medical conditions were identified in at least 5% of the population at baseline. Classification of heart disease, hypertension, diabetes, cancer, thyroid disease, and herpes zoster was based on medical history. A clinical diagnosis of stroke was based on medical history and examination. As in previous research, we used the number of these conditions present at baseline as an indicator of overall physical health.39 Information on vital status was obtained at each follow-up interview (1997–2000 and 2000–2003), and all reported deaths through December 31, 2003, were verified through the National Death Index.
Data Analysis
We used survival models to analyze time to death as a function of perceived discrimination and other covariates. Time-to-death data were modeled using Cox proportional hazards models.40 In the primary analysis, we tested the relation of perceived discrimination on risk of mortality after adjustment for age, gender, race, and lifetime SES. This model also included a term for the interaction of race and age to allow for the commonly observed attenuation of racial differences in mortality at older ages.41,42 In a subsequent model, we added a term for race by perceived discrimination interaction to test whether the relation of discrimination to mortality differed for Blacks and Whites.
In a series of secondary analyses, we first explored potential bias in the relation between perceived discrimination and mortality, because of interviewer influence on discrimination responses. In a previous analysis, we found that participants reported significantly higher levels of perceived discrimination when paired with an interviewer of the same race.12 We therefore repeated the primary analysis after restricting the sample to respondents interviewed by someone of the same race. Because there were more White interviewers, a higher percentage of White (89%) than Black (66%) respondents were race matched to the interviewer. Next, we added CES-D and number of chronic medical conditions to the primary model as potential confounders of the association between perceived discrimination and mortality. Finally, we examined the relation of the 2 discrimination subscales—unfair treatment and personal rejection—to mortality after adjustment for demographics. Additional models tested whether the relation of the subscales to mortality differed for Blacks and Whites by adding terms for the interaction of each subscale and race, and whether the results changed after restricting the sample to the race-matched subset. All analyses were conducted using SAS software.43 Model assumptions were evaluated graphically and analytically and judged to be adequately met.44
RESULTS
Of the original 6102 non-Hispanic Black or White participants, 4282 participated (86.9% of survivors) in the first follow-up interview. Of these, 128 were excluded because of missing data on perceived discrimination (114 persons) or dates of death (14 persons), leaving a total of 4154 participants (61.8% women, 61.8 % Black). The mean age of the sample was 77.14 years (SD= 6.34). On average, Blacks were younger than Whites (Blacks: mean = 76.2 years [SD= 5.9]; Whites: mean = 78.7 years [SD= 6.7]; P < .001) and had a lower z score on the lifetime measure of SES (–0.23 vs 0.52; P < .001). There were no differences in chronic health conditions between the 2 groups, but Blacks reported more perceived discrimination and more depressive symptoms than did Whites (both P < .001).
Relation Between Perceived Discrimination and Mortality
There were 1168 deaths over a mean of 4.8 years (SD= 1.8). Table 1 ▶ shows the distribution of key characteristics of those who died during follow-up compared with those who lived. On average, the deceased had higher perceived discrimination scores at baseline compared with survivors (mean = 1.13 vs 0.99; P < .01).
TABLE 1—
Characteristics of Adults 68 Years and Older Who Died Compared With Those Who Did Not Die During Follow-Up: Chicago Health and Aging Project, Chicago, IL 1997–2003
| Characteristics | Dead (n = 1168) | Alive (n = 2986) |
| Age,** y, mean (SD) | 80.2 (7.34) | 76.0 (5.45) |
| Gender,* % | ||
| Women | 26.3 | 73.7 |
| Men | 31.0 | 69.0 |
| Race,* % | ||
| Black | 26.6 | 73.4 |
| White | 30.5 | 69.5 |
| Lifetime SES,a ** mean Z (SD) | –0.04 (.76) | 0.09 (.76) |
| CES-D score,** mean (SD) | 2.31(2.34) | 1.58 (2.02) |
| Medical conditions,** mean no. (SD) | 1.22 (1.04) | 0.99 (0.93) |
| Perceived discrimination score,b * mean (SD) | 1.13 (1.72) | 0.99 (1.58) |
Note. SES = socioeconomic status. CES-D = Center for Epidemiological Studies Depression Scale–Short Form.
aRange = −2.05 to 2.92.
bPerceived discrimination was assessed with a previously established 9-item measure. The scale assesses the subjective experience of being treated unfairly without reference to racism, discrimination, prejudice, or any demographic characteristics such as race, gender, or age. We recoded the responses to a binary format (often or sometimes = 1, rarely or never = 0) and then summed across items to get the total score (range = 0–9), with higher scores indicating more discrimination.
*P < .01; **P < .001.
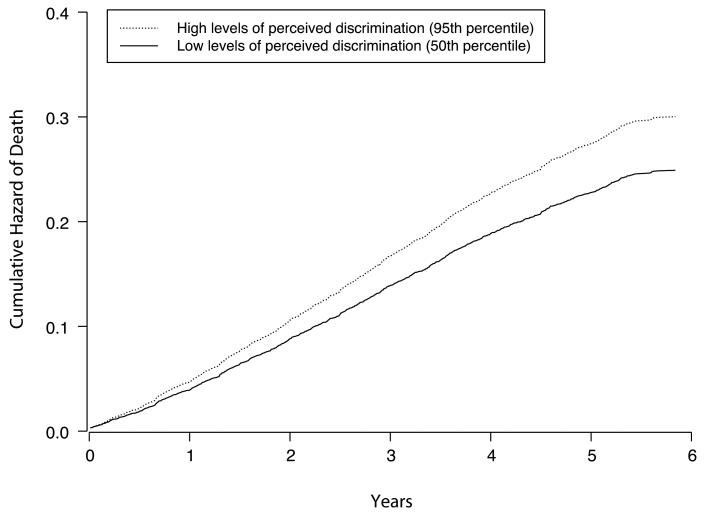
After adjustment for age, gender, race and lifetime SES, perceived discrimination was significantly associated with mortality risk (hazard ratio [HR] = 1.05; 95% confidence interval [CI] = 1.01, 1.09), with each additional point on the discrimination scale conferring an approximately 5% increase in risk of death (Table 2 ▶). To illustrate the magnitude of this effect, we calculated the cumulative hazard of death during the 5-year period for participants with discrimination scores at the 50th and 95th percentiles using the results of the core model shown in Table 2 ▶ (full sample). As shown in Figure 1 ▶, those who scored at the 95th percentile (dotted line) had approximately a 21% increased risk of death compared with those who scored at the 50th percentile (solid line) after adjustment for age, gender, race, and lifetime SES.
TABLE 2—
Hazard Ratios (HRs) of Mortality Associated With Perceived Discrimination Among Adults 65 Years and Older in the Full (N = 4101) and Race-Matched Samples (n = 3070): Chicago Health and Aging Project, Chicago, IL 1997–2003
| Full Sample | Race-Matched Sample | |||
| Predictor | Core Model, HR (95% CI) | Core Model + Discrimination × Race Interaction, HR (95% CI) | Core Model, HR (95% CI) | Core Model + Discrimination × Race Interaction, HR (95% CI) |
| Discrimination scorea | 1.05 (1.01, 1.09) | 1.12 (1.04, 1.20) | 1.07 (1.03, 1.12) | 1.11 (1.03, 1.20) |
| Discrimination score × Black | 0.92 (0.85, 1.00) | 0.95 (0.87, 1.04) | ||
| Discrimination score among Blacksb | 1.03 (0.99, 1.07) | 1.06 (1.01, 1.11) | ||
| Discrimination score among Whitesb | 1.12 (1.04, 1.20) | 1.11 (1.03, 1.20) | ||
Note. CI = confidence interval. The core model included terms for age, gender, race, race × age, and lifetime socioeconomic status.
aRange = 0–9.
bDerived from a model that included terms for age, gender, race, race × age, lifetime socioeconomic status, discrimination, and discrimination × race.
Note. Analyses adjusted for age, gender, race, and lifetime socioeconomic status.
FIGURE 1—
Cumulative hazard of death among adults 68 years and older: Chicago, IL, 1997–2003.
The next model revealed that discrimination appeared to be related differently to mortality among Blacks and Whites. Contrary to our expectation, the relation was stronger among Whites than among Blacks (Table 2 ▶, full sample, core model + discrimination × race interaction). Each additional point on the discrimination scale was associated with a 12% increase in mortality risk (HR = 1.12; 95% CI = 1.04, 1.20) among Whites, but only a 3% increase among Blacks (HR = 1.03; 95% CI = 0.99, 1.07).
Interviewers were of the same race for 3070 (74%) of the 4154 participants. In this subset, the increase in mortality related to perceived discrimination remained significant (HR = 1.07; 95% CI = 1.03, 1.12; Table 2 ▶). However, when the interaction between race and perceived discrimination was added, the term for the interaction was no longer significant (Table 2 ▶, race-matched sample, core model + discrimination × race interaction), indicating that the relation between discrimination and mortality did not differ significantly between Blacks and Whites in this subset.
The overall association between perceived discrimination and mortality remained unchanged after adjustment for number of medical conditions (HR = 1.04; 95% CI = 1.01, 1.08). Adjustment for depressive symptoms lead to a slight decrease in the mortality risk because of discrimination (HR = 1.07; 95% CI = 0.99, 1.15). Furthermore, the differential effect of perceived discrimination by race was no longer significant (P = .11 and P = .13, respectively) in either model (data not shown).
Unfair Treatment, Personal Rejection, and Mortality
We found a nonsignificant increase in mortality risk related to unfair treatment (HR = 1.05; CI = 0.99, 1.11) and no differential effect of unfair treatment by race (Table 3 ▶). By contrast, personal rejection was associated with a significantly increased risk of mortality (HR = 1.12; 95% CI = 1.05, 1.20). In a separate model that included an interaction term for race and personal rejection, the relation of personal rejection to mortality was found to differ significantly by race (Table 3 ▶, interaction added model). Taking the interaction term into account revealed a stronger relation among Whites than Blacks (Whites: HR = 1.29; 95% CI = 1.12, 1.48; Blacks: HR = 1.09; 95% CI = 1.01, 1.17).
TABLE 3—
Hazard Ratios (HRs) of Mortality Associated With Unfair Treatment and Personal Rejection Among Adults Aged 68 Years and Older in the Full and Race-Matched Samples: Chicago Health and Aging Project, Chicago, IL, 1997–2003
| Predictor | Full Sample Core Model, HR (95% CI) | Interaction Added, HR (95% CI) | Race-Matched Sample Core Model, HR (95% CI) | Interaction Added, HR (95% CI) |
| Unfair treatment scorea | 1.05 (0.99, 1.11) | 1.12 (1.00, 1.24) | 1.09 (1.02, 1.16) | 1.14 (1.02, 1.28) |
| Unfair treatment × Blacks | 0.92 (0.81, 1.04) | 0.94 (0.82, 1.07) | ||
| Unfair treatment among Blacksb | 1.03 (0.96, 1.09) | 1.07 (0.99, 1.15) | ||
| Unfair treatment among Whitesb | 1.12 (1.00, 1.24) | 1.14 (1.02, 1.28) | ||
| Personal rejection scorec | 1.12 (1.05, 1.20) | 1.29 (1.12, 1.48) | 1.16 (1.07, 1.25) | 1.22 (1.04, 1.43) |
| Personal rejection × Blacks | 0.84 (0.72, 0.99) | 0.93 (0.78, 1.12) | ||
| Personal rejection among Blacksb | 1.09 (1.01, 1.17) | 1.14 (1.04, 1.24) | ||
| Personal rejection among Whitesb | 1.29 (1.12, 1.48) | 1.22 (1.04, 1.43) |
Note. CI = confidence interval. Core model included terms for age, gender, race, race × age, and lifetime socioeconomic status.
aRange = 0–4.
bDerived from a model that included terms for age, gender, race, race × age, lifetime socioeconomic status, discrimination, and discrimination × race.
cRange = 0–5.
In secondary analyses restricted to the subset matched by race to the interviewer, both unfair treatment and personal rejection were significantly related to increased risk of mortality (unfair treatment: HR = 1.09; 95% CI = 1.02, 1.16; personal rejection: HR = 1.16; 95% CI = 1.07, 1.25). In subsequent models, these effects did not vary by race, as revealed by the term for the discrimination by race interaction (Table 3 ▶, interaction added models).
DISCUSSION
Adverse Health Effects of Perceived Discrimination
Our findings suggest that perceived discrimination is associated with increased mortality risk in a population of older adults. The magnitude of this effect amounts to approximately a 21% increase in risk in the 95th versus the 50th percentile of the perceived discrimination measure. The association was independent of differences in SES, negative affect, or chronic illnesses. Contrary to our expectation, the association appeared stronger among Whites than among Blacks, even though Blacks reported more instances of perceived discrimination. Experiences of a more demeaning nature, such as those related to personal rejection, were related to mortality, as opposed to more-generic perceptions of rudeness.
These results add to a growing understanding of the potentially harmful effects of perceived discrimination on health. Previous studies have provided support for the notion that perceived discrimination is associated with poor health outcomes,9,10,25,26,45,46 and results have generally been stronger for mental than physical health. Few studies have focused on well-established clinical outcomes,14,25,26 with the majority relying on self-report measures. Further, most studies have been limited to middle-aged persons or younger adults.1,2 We were able to identify only 1 prospective study that investigated mortality in relation to discrimination,28 but the sample included only Blacks. Among Blacks exposed to perceived racism, respondents with a system-blaming orientation had a higher survival rate than did those with a self-blaming orientation. Our study is the first prospective study of which we are aware that compares the relation of perceived discrimination to mortality among Blacks and Whites. We have thus extended research on the adverse health effects of perceived discrimination by investigating a well-established clinical outcome in a population-based, biracial sample of older adults, with a wide range of SES across both racial groups.
Discrimination and Mortality
Our data suggest that discrimination may have a more adverse effect on survival among older Whites than Blacks. Although this difference is contrary to our previous hypothesis, a similarly harmful effect attributable to perceived discrimination among Whites but not Blacks has been noted previously for psychological distress and well-being.47,48 Among older Whites, perceived discrimination may reflect relatively new experiences of discrimination associated with ageism.49 Such perceptions may have an adverse effect on psychological mood states, which may increase mortality risk.50,51 In our own data, perceived discrimination was strongly correlated with depressive symptoms,12 and adjustment for these symptoms in the current study appeared to slightly reduce the relation of discrimination to mortality, suggesting that a part of this relation may be mediated by depressive symptoms.
Conversely, among older Blacks, experiences with discrimination may be more normative, with discrimination likely to have been much more common throughout life. Older Blacks may therefore have developed strategies of coping and adaptation52–54 that enable them to more effectively offset the harmful effects of discrimination, even if they face more instances of discrimination. We did not assess coping orientation or particular cognitive styles that may influence the interpretation of perceived negative treatment or the personality characteristics associated with these perceptions.
Another factor that may have contributed to the stronger adverse effect among Whites is the absence of a time frame in the survey questions on discriminatory experiences. According to a recent review,1 failure to provide a time frame may induce a recency effect in reporting perceptions of discrimination, which has been argued to contribute to a higher proportion of statistically significant associations in this research. Recent experiences with discrimination may have been salient for older Whites because of lack of exposure in previous stages of life, which may account in part for the unexpected higher risk associated with these experiences among Whites.
Black–White Differences
There are 2 reasons why the unexpected greater adverse effect among Whites may be an artifact of our data. First, to administer the measure of perceived discrimination uniformly among Blacks and Whites, we did not pair instances of discrimination with attributions about the source, such as race or skin color. Although we controlled for other individual characteristics typically associated with discrimination, such as gender and age, it is possible that a measure of racism-based discrimination would have shown greater adverse effects among older Blacks. In addition, racism or discrimination may exist at 3 broad levels: individual (experienced on a personal level), institutional (embedded in the policies of a given institution), and cultural (arising from cultural practices at a group level).55 The measure we used focused only on individual-level discrimination. Information on other forms of discrimination may have provided a more complete picture of experiences of discrimination that have deleterious health effects in the Black population.
Second, our data suggest that the results of the primary analysis may have been affected by interviewer–participant mismatches by race. Previous research has shown that responses to sensitive survey questions may be influenced by the degree of correspondence between respondents and interviewers on key demographic characteristics, particularly race and gender.56–58 In a previous analysis of data from this cohort, older Blacks reported significantly higher levels of perceived discrimination when matched to a Black interviewer than when matched to a White interviewer. In this study, restricting the analysis to race-matched interviewers reduced the differential effect by race to a nonsignificant level, suggesting that there is no racial difference in mortality risk because of perceived discrimination and that humiliating experiences are equally toxic for both groups. Overall, we are inclined to give greater credence to the results of the race-matched analysis given the sensitive nature of discrimination-related questions and the clear interviewer effects in the responses. Yet we recognize that this was a secondary analysis, which should be interpreted with more caution than the primary analysis.
Blatant Versus Subtle Discrimination
Analyses in the full sample suggested that personal rejection had a particularly adverse effect on mortality. The scale items that reflect personal rejection include demeaning experiences of judgment and criticism that undermine one’s character or more-overt acts of passive violence. By contrast, the scale items that measured unfair treatment captured more-generic perceptions of rudeness or discourteousness.12 These results are consistent with a previous study with this cohort,12 in which personal rejection had a stronger association with depressive symptoms than unfair treatment and suggest that more-overt indicators of discrimination are related to the pathway by which perceived discrimination affects adverse health outcomes, in this case mortality.
Our study had several limitations. First, as stated previously, our measure of perceived discrimination did not assess the perceived reason for discrimination. However, this limitation is offset, at least in part, by our multivariate analysis in which we controlled for characteristics typically related to discrimination, in particular, age, gender, and SES. Second, we examined the relation between discrimination and mortality in adults older than 68 years at follow-up. Psychosocial predictors tend to be less strongly associated with mortality in older adults, possibly because other factors have a stronger influence on mortality patterns, such as poor health and other common conditions of aging. Third, we did not assess the cause of mortality. We did exclude the 17 deaths that were caused by external forces (e.g., unintentional injuries or accidents), and their removal did not change the pattern of results. However, it is possible that stronger racial differences may have emerged for vascular-related causes of mortality. Fourth, we used number of chronic medical conditions as an indicator of overall health in analyses, which assumes that all conditions have equal weight in terms of severity. Finally, our follow-up time was a little less than 5 years. A longer follow-up interval would have produced more deaths and may have resulted in a stronger association between discrimination and mortality.
Perceived discrimination was associated with an increased risk of mortality in a prospective population-based study of older adults. Contrary to our expectations, we did not find the relation to be stronger among Blacks. Further, the association appeared to be related to discriminatory experiences of a more demeaning nature. The results support the idea that perceived discrimination has an adverse influence on health. Although older Blacks experience higher levels of discrimination than do Whites, it is possible that discrimination among Blacks in this age group may have lost some of its influence.
Acknowledgments
This work was supported by National Institute on Aging (grants AG11101 and AG22018) and the National Institute on Environmental Health Science (grant ES10902).
The authors thank the residents of Morgan Park, Washington Heights, and Beverly who participated in the study. They also thank Ann Marie Lane for community development and oversight of project coordination; Michelle Bos, Holly Hadden, Flavio LaMorticella, and Jennifer Tarpey for coordination of the study; and Todd Beck for analytic programming.
Human Participant Protection The study was approved by the institutional review board of Rush University Medical Center.
Peer Reviewed
Contributors L. L. Barnes was the primary writer of the article and participated in its conception, statistical analysis, and interpretation of data. C. F. Mendes de Leon participated in the study design, conception, data acquisition, statistical analysis, and interpretation of data and provided critical revision and supervision. T.T. Lewis participated in interpretation of data and provided critical revision. J. L. Bienias contributed to the analysis and interpretation of data and provided technical support and critical revision. R. S. Wilson participated in conception and design and provided critical revision. D. A. Evans was the principal investigator and was key in conception and design, provided logistic support for conducting the study and acquiring data, contributed to the analysis and interpretation of data, and provided supervision and critical revision.
References
- 1.Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35:888–901. [DOI] [PubMed] [Google Scholar]
- 2.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93:200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: relationship to cardiovascular reactivity among African American and European American women. Health Psychol. 2001;20:315–325. [DOI] [PubMed] [Google Scholar]
- 4.Ryan AM, Gee GC, Laflamme DF. The association between self-reported discrimination, physical health and blood pressure: findings from African Americans, Black immigrants, and Latino immigrants in New Hampshire. J Health Care Poor Underserved. 2006; 17(suppl 2):116–132. [DOI] [PubMed] [Google Scholar]
- 5.Taylor TR, Williams CD, Makambi KH, et al. Racial discrimination and breast cancer incidence in US Black women: the Black Women’s Health Study. Am J Epidemiol. 2007;166:46–54. [DOI] [PubMed] [Google Scholar]
- 6.Landrine H, Klonoff EA. The schedule of racist events. J Black Psychol. 1996;22:144–168. [Google Scholar]
- 7.Ren XS, Amick BC, Williams DR. Racial/ethnic disparities in health: the interplay between discrimination and socioeconomic status. Ethn Dis. 1999;9:151–165. [PubMed] [Google Scholar]
- 8.Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: results from a longitudinal analysis. Am J Public Health. 2006;96:1265–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–230. [PubMed] [Google Scholar]
- 10.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socioeconomic status, stress and discrimination. J Health Psychol. 1997;2:335–351. [DOI] [PubMed] [Google Scholar]
- 11.Schulz A, Israel B, Williams D, Parker E, Becker A, James S. Social inequalities, stressors and self reported health status among African American and White women in the Detroit metropolitan area. Soc Sci Med. 2000;51:1639–1653. [DOI] [PubMed] [Google Scholar]
- 12.Barnes LL, Mendes de Leon CF, Wilson RS, Bienias JL, Bennett DA, Evans DA. Racial differences in perceived discrimination in a community population of older Blacks and Whites. J Aging Health. 2004;16:315–337. [DOI] [PubMed] [Google Scholar]
- 13.Broman CL. The health consequences of racial discrimination: a study of African Americans. Ethn Dis. 1996;6:148–153. [PubMed] [Google Scholar]
- 14.Brown C, Matthews KA, Bromberger JT, Chang Y. The relation between perceived unfair treatment and blood pressure in a racially/ethnically diverse sample of women. Am J Epidemiol. 2006;164:257–262. [DOI] [PubMed] [Google Scholar]
- 15.Dressler WW. Lifestyle, stress, and blood pressure in a southern Black community. Psychosom Med. 1990; 52:182–198. [DOI] [PubMed] [Google Scholar]
- 16.Jackson JS, Brown TN, Williams DR, Torres M, Sellers SL, Brown K. Racism and the physical and mental health status of African Americans: a thirteen year national panel study. Ethn Dis. 1996;6:132–147. [PubMed] [Google Scholar]
- 17.Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990;30:1273–1281. [DOI] [PubMed] [Google Scholar]
- 18.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young Black and White adults. Am J Public Health. 1996;86:1370–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans. A biopsy-chosocial model. Am Psychol. 1999;54:805–816. [DOI] [PubMed] [Google Scholar]
- 20.Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethn Health. 2000;5:243–268. [DOI] [PubMed] [Google Scholar]
- 21.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol. 1995;21:349–386. [Google Scholar]
- 22.Yen IH, Kaplan GA. Poverty area residence and changes in depression and perceived health status: evidence from the Alameda County Study. Int J Epidemiol. 1999;28:90–94. [DOI] [PubMed] [Google Scholar]
- 23.Cozier Y, Palmer JR, Horton NJ, Fredman L, Wise LA, Rosenberg L. Racial discrimination and the incidence of hypertension in US Black women. Ann Epidemiol. 2006;16:681–687. [DOI] [PubMed] [Google Scholar]
- 24.Din-Dzietham R, Nembhard WN, Collins R, Davis SK. Perceived stress following race-based discrimination at work is associated with hypertension in African-Americans. The metro Atlanta heart disease study, 1999–2001. Soc Sci Med. 2004;58:449–461. [DOI] [PubMed] [Google Scholar]
- 25.Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychol. 2003;22:300–309. [DOI] [PubMed] [Google Scholar]
- 26.Lewis TT, Everson-Rose SA, Powell LH, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosom Med. 2006;68:362–368. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy BP, Kawachi I, Lochner K, Jones C, Prothrow-Stith D. (Dis)respect and Black mortality. Ethn Dis. 1997;7:207–214. [PubMed] [Google Scholar]
- 28.LaVeist TA, Sellers R, Neighbors HW. Perceived racism and self and system blame attribution: consequences for longevity. Ethn Dis. 2001;11:711–721. [PubMed] [Google Scholar]
- 29.Mendes de Leon CF, Barnes LL, Bienias JL, Skarupski KA, Evans DA. Racial disparities in disability: recent evidence from self-reported and performance-based disability measures in a population-based study of older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60:263–271. [DOI] [PubMed] [Google Scholar]
- 30.Everson-Rose SA, Mendes de Leon CF, Bienias JL, Wilson RS, Evans DA. Early life conditions and cognitive functioning in later life. Am J Epidemiol. 2003; 158:1083–1089. [DOI] [PubMed] [Google Scholar]
- 31.Blazer DG, Hybels CF, Pieper CF. The association of depression and mortality in elderly persons: a case for multiple, independent pathways. J Gerontol A Biol Sci Med Sci. 2001;56:505–509. [DOI] [PubMed] [Google Scholar]
- 32.Penninx BW, Geerlings SW, Deeg DJ, van Eijk JT, van TW, Beekman AT. Minor and major depression and the risk of death in older persons. Arch Gen Psychiatry. 1999;56:889–895. [DOI] [PubMed] [Google Scholar]
- 33.Penninx BW, Pahor M, Woodman RC, Guralnik JM. Anemia in old age is associated with increased mortality and hospitalization. J Gerontol A Biol Sci Med Sci. 2006; 61:474–479. [DOI] [PubMed] [Google Scholar]
- 34.Levine RS, Foster JE, Fullilove RE, et al. Black-White inequalities in mortality and life expectancy, 1933–1999: implications for healthy people 2010. Public Health Rep. 2001;116:474–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sachs-Ericsson N, Plant EA, Blazer DG. Racial differences in the frequency of depressive symptoms among community dwelling elders: the role of socioeconomic factors. Aging Ment Health. 2005;9:201–209. [DOI] [PubMed] [Google Scholar]
- 36.Skarupski KA, Mendes de Leon CF, Bienias JL et al. Black-White differences in depressive symptoms among older adults over time. J Gerontol B Psychol Sci Soc Sci. 2005;60:136–142. [DOI] [PubMed] [Google Scholar]
- 37.Kohout F, Berkman L, Evans D, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5:179–193. [DOI] [PubMed] [Google Scholar]
- 38.Radloff L. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measure. 1977;1:385–401. [Google Scholar]
- 39.Wilson RS, Mendes de Leon CF, Barnes LL, et al. Participation in cognitively stimulating activities and risk of incident Alzheimer disease. JAMA. 2002;287:742–748. [DOI] [PubMed] [Google Scholar]
- 40.Cox DR. Regression models and life tables (with discussion). J R Stat Soc Ser B. 1972;74:187–220. [Google Scholar]
- 41.Corti MC, Guralnik JM, Ferrucci L, et al. Evidence for a Black-White crossover in all-cause and coronary heart disease mortality in an older population: the North Carolina EPESE. Am J Public Health. 1999;89:308–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: the National Longitudinal Mortality Study. Am J Public Health. 1995;85:949–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.SAS Institute Inc. SAS OnlineDoc 9.1.3. Cary, NC: SAS Institute Inc; 2004.
- 44.Collett D. Modelling Survival Data in Medical Research. 2nd ed. Boca Raton, FL: Chapman & Hall; 2003.
- 45.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92:615–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Karlsen S, Nazroo JY. Relation between racial discrimination, social class, and health among ethnic minority groups. Am J Public Health. 2002;92:624–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pavalko EK, Mossakowski KN, Hamilton VJ. Does perceived discrimination affect health? Longitudinal relationships between work discrimination and women’s physical and emotional health. J Health Soc Behav. 2003;44:18–33. [PubMed] [Google Scholar]
- 48.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188. [DOI] [PubMed] [Google Scholar]
- 49.Tougas F, Lagace M, de la Sablonniere R, Kocum L. A new approach to the link between identity and relative deprivation in the perspective of ageism and retirement. Int J Aging Hum Dev. 2004;59:1–23. [DOI] [PubMed] [Google Scholar]
- 50.Everson SA, Goldberg DE, Kaplan GA et al. Hopelessness and risk of mortality and incidence of myocardial infarction and cancer. Psychosom Med. 1996;58:113–121. [DOI] [PubMed] [Google Scholar]
- 51.Wilson RS, Bienias JL, Mendes de Leon CF, Evans DA, Bennett DA. Negative affect and mortality in older persons. Am J Epidemiol. 2003;158:827–835. [DOI] [PubMed] [Google Scholar]
- 52.Johnson CL. Determinants of adaptation of oldest old Black Americans. J Aging Stud. 1995;9:231–244. [Google Scholar]
- 53.Lincoln KD, Chatters LM, Taylor RJ. Psychological distress among Black and White Americans: differential effects of social support, negative interaction and personal control. J Health Soc Behav. 2003;44:390–407. [PMC free article] [PubMed] [Google Scholar]
- 54.Williams DR, Spencer MJ, Jackson JS. Race, stress, and physical health. In: Contrada RJ, Ashmore RD, eds. Self, Social Identity, and Physical Health: Interdisciplinary Exploration. New York, NY: Oxford University Press; 1999:71–100.
- 55.Jones JM. Prejudice and Racism. 2nd ed. New York, NY: McGraw-Hill; 1997.
- 56.Edwards WS, Berk ML. Effect of interviewer and respondent characteristics on reporting of chronic conditions. In: Proceedings of the American Statistical Association, Section on Survey Research Methods, 1. Alexandria, VA: American Statistical Association; 1993:330–334.
- 57.Hatchett S, Schuman H. White respondents and race-of-interviewer effects. Public Opin Q. 1975;39:523–528. [Google Scholar]
- 58.Jackson JS. Methodological issues in survey research on older minority adults. In: Lawton MP, Herzog AR, eds. Special Research Methods for Gerontology. Society and Aging. Amityville, NY: Baywood Publishing Co, Inc; 1989:137–161.