Abstract
Objectives. We investigated the risk of entering long-term institutional care after the death of a spouse in relation to the duration of widowhood among older Finnish men and women. We also examined whether high levels of education or household income buffered the effects of bereavement on institutionalization.
Methods. We used linked register-based data on Finnish adults 65 years or older who were living with a spouse at the beginning of the study period (n=140902) and were followed from January 1998 to December 2002.
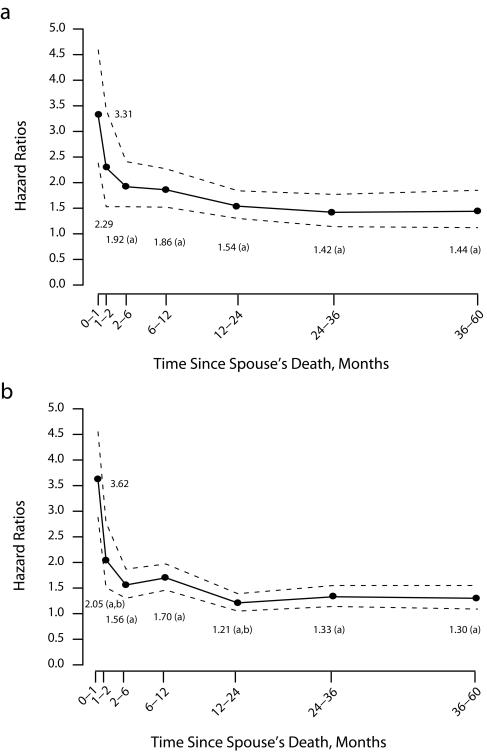
Results. The excess risk of institutionalization was highest during the first month following a spouse’s death compared with still living with a spouse (adjusted hazard ratio=3.31 for men, 3.62 for women). This risk decreased over time among both men and women. The relative effect of the duration of widowhood on institutionalization did not significantly vary according to the level of education or income.
Conclusions. Risk of institutionalization is particularly high immediately after the death of a spouse, demonstrating the importance of loss of social and instrumental support.
Previous studies showed that older adults who live alone or without a spouse have an increased probability of entering institutional care, independent of baseline health status.1–4 These findings indicate the importance of social and instrumental support provided by a spouse in reducing the need for institutionalization. In addition, never-married, widowed, and divorced older persons have been shown to have a higher probability of institutionalization than their married counterparts.5,6 However, few studies have analyzed how the death of a spouse affects the probability of entering institutional care.
The death of a spouse has been shown to be associated with poor mental health, such as depression and anxiety,7,8 and with poor physical health.7 Because poor mental and physical health have both been found to be associated with an increased risk of institutionalization,1,2 it is likely that the death of a spouse also increases the need for institutional care. In addition, some studies have found an association between the death of a spouse and a decline in cognitive status (e.g., memory functioning),9 which is shown to be an important risk factor for admission to institutional care.1,10 Because mental health may improve again after despair and disorganization diminish with time following bereavement,11 it is possible that the risk of institutionalization is highest immediately after the loss of a spouse and decreases over time.
One study from the United States indicated that becoming widowed during a prospective follow-up was associated with an increased probability of nursing home admission, but the recency of widowhood, measured retrospectively at the time of the baseline interviews, was not.12 The latter finding may be misleading, especially if the effect of widowhood is short term and a large proportion of the recently widowed were already institutionalized before the baseline interviews. However, we know of no large-scale prospective studies testing whether the effect of a spouse’s death on institutionalization varies according to the duration of widowhood, and the existence and the magnitude of these effects are unknown.
The effect of widowhood and widowerhood on mortality is well established: the recently bereaved have been shown to have a higher risk of death than the currently married,13–20 especially from alcohol-related diseases, suicides, and other accidents and violence.19 Because both mortality and institutionalization are related to poor health (e.g., poor self-perceived health predicts mortality and institutionalization,3,21 depression predicts mortality,22 and depressive symptoms predict institutionalization among men23), it is possible that the effect of the duration of widowhood is similar for both. Previous studies indicated that excess mortality is highest during the first weeks18,24 or months13,14,16,20,25 after a spouse’s death. Some studies found that excess mortality among the bereaved decreases to the level of the married with time from bereavement among men,13 but others indicated that it continues, although at a lower level, for 10 years and longer.15
The excess risk of death among the recently bereaved may be related to psychosocial mechanisms, such as emotional stress and grief, and to the loss of social, instrumental, and material support.18,19,26 However, previous mortality studies suggested that the bereaved gradually adapt to the loss and learn to cope in their changed social environment. Furthermore, bereaved persons with disabilities may be more likely to be institutionalized immediately after the death of the spouse because there is no longer anybody to take care of them.
High levels of education and income, as well as other social and economic resources, may buffer against the harmful effect of spousal loss on institutionalization and mortality. However, persons with higher education20,27,28 and income27 were not found to suffer less excess mortality after a spouse’s death in previous studies. Although high socioeconomic status is associated with lower mortality, it has not been shown to prevent or even buffer the harmful effects of spousal loss. On the contrary, a study of the Israeli Jewish population indicated that the relative excess mortality among those recently bereaved was higher for men with more education.20
Perhaps socioeconomic buffering of the effects of bereavement is greater on institutionalization than on mortality, because the loss of spousal support and access to substitute assistance, such as home help services, are likely to be more effective predictors of institutionalization than of death. However, empirical evidence for this hypothesis is not available. Because older adults with savings and higher incomes may be better able to afford home help services, a high household income at the beginning of a study could also buffer the harmful effects of spousal loss.
We used population-based survival data with a continuous time scale of institutionalization to assess the risk of entering institutional care after the death of a spouse in relation to the duration of widowhood and widowerhood among adults 65 years or older. We analyzed Finnish register-based data containing information on each individual’s dates of first admission into long-term institutional care and death and on the spouse’s date of death during a 5-year follow-up from January 1998 to December 2002. We sought to assess (1) whether recently bereaved older adults had a higher risk of entering institutional care than did those living with a spouse, independent of sociodemographic controls and preexisting medical conditions; (2) how the duration of widowhood was associated with the risk of entering institutional care; and (3) whether the relative effects of a spouse’s death were smaller among persons with a higher level of education or a higher household income. The first 2 analyses were performed separately for men and women.
METHODS
Data
We analyzed a 40% individual-level random sample of the Finnish population 65 years or older on December 31, 1997, drawn from a population registration database at Statistics Finland. These data, which contain detailed sociodemographic information, are collected annually from different administrative records to provide labor-force statistics.29 Already linked with dates of death and dates of spousal death, these data were further linked with register-based information on institutionalization and hospital diagnoses provided by the National Research and Development Centre for Welfare and Health and with medication registers provided by the Social Insurance Institution. The linkage was carried out with personal identification codes.
We included all those who were living in private households with a partner (N = 140902), including a married spouse (96.4%) and a nonmarried partner (3.6%), at the beginning of the study period. This sample was followed for first admission into long-term institutional care, death, and spousal death from January 1, 1998, to December 31, 2002. The data were unique in that they covered a large number of persons bereaved during the follow-up and gave the dates of bereavement and of first admission into institutional care. Furthermore, missing information and loss to follow-up were minimal in these nationally representative data that linked various administrative registers.
Long-Term Institutional Care and Bereavement
Long-term institutional care was defined as 24-hour care in nursing homes and service homes and as inpatient care in hospitals and health centers lasting more than 90 days or confirmed by a long-term-care decision. Long-term psychiatric care was included. The more-than-90-days criterion was met if a patient had stayed in the same institution or successively in different institutions for that period. We used care episodes in nursing and service homes (social care) as well as those in hospitals and health centers (health care) to identify periods of long-term institutional care that consisted of several stays in a row in different institutions. This is important in studying long-term care because elderly persons often move between hospital and nursing home according to the intensity of the care they need. Furthermore, in many individual cases of long-term care in Finland it is often difficult or arbitrary to define which of these care types is primary or predominant, because, for example, long-term institutional care often starts in hospitals or health centers, where disabled elderly persons wait to get a place in a nursing home. More information on institutional care for older persons in Finland is available elsewhere.30,31
A person was considered bereaved if the spouse (a married spouse or cohabiting partner of the opposite gender) had died 1 day or more prior to his or her own date of institutionalization or death. We divided the time since the bereavement into 7 categories: 0 to 1 month (1–30 days), 1 to 2 months (31–60 days), 2 to 6 months (61–180 days), 6 to 12 months (181–360 days), 12 to 24 months (361–720 days), 24 to 36 months (721–1080 days), and more than 36 months (> 1081 days); for the analyses of socioeconomic interactions, we used 4 categories: 0 to 2 months, 2 to 6 months, 6 to 12 months, and more than 12 months.
Socioeconomic and Control Variables
Education and household disposable income were the socioeconomic variables, and age, region of residence, and chronic medical conditions were control variables. Household size was excluded from the models because adding it did not improve the fit. The socioeconomic and control variables were measured at the beginning of the follow-up at the end of 1997, with the exception of medical conditions, which were defined during 1996 and 1997. Education and household income were adjusted to control for a shared socioeconomic environment that could affect both the spouse’s probability of death and study participant’s probability of institutionalization. These variables were also used to analyze whether a higher socioeconomic status buffered the effects of bereavement.
The educational categories were determined by the highest educational qualification. The 2 categories were tertiary or intermediate education and basic education or less. If there was no information on education, the participants were classified as having basic education or less by Statistics Finland.
Household disposable income per consumption unit was used to measure income, meaning all annual taxable income received by household members, including pensions, wages, capital income, unemployment benefits, and other taxable income transfers. Taxes and certain social security payments, such as income, capital, municipal and church taxes, and health and pension insurance payments were subtracted. Disposable income of a household was adjusted for the number of persons in the household: the first member was weighted as 1.0 unit and any other as 0.7 units. This corresponds to the Organisation for Economic Co-operation and Development Equivalence Scale,32 with the exception of children who were weighted as adults because of the data restrictions. This did not affect our results, because the inclusion of children in this study population was very rare. Income was divided into quintiles: the cut-off points for the quintiles were calculated from the combined data for older men and women living with a spouse.
Region of residence was adjusted to control for difference in the supply of and access to institutional care between the areas. It was categorized into the 20 official regions of Finland,33 with the exception of Uusimaa, which was divided into 3 parts: Helsinki, the metropolitan area, and the rest of Uusimaa.
Eighteen dichotomous indicators of chronic medical conditions were used to control for preexisting health status: cancer, diabetes, dementia, psychosis, depressive symptoms, other mental health disorders, Parkinson’s disease, other neurological diseases, heart disease, stroke, chronic asthma or other similar chronic obstructive pulmonary diseases, other respiratory diseases, arthritis, osteoarthritis, hip fracture, other conditions related to accident or violence, other hospital diagnoses, and other chronic diseases. The study participants were categorized as having a medical condition if it appeared in 1 or more of the following sources: (1) registers showing the principal cause of hospitalization in 1996 to 1997; (2) registers showing the right to reimbursement for drug costs under the special refund categories for certain diagnosed chronic conditions in 1997, and (3) registers of prescription medication in 1996 to 1997.
The data on the principal cause of hospitalization were derived from the Finnish Version of the International Classification of Diseases, 10th Revision.34 Data on the right to reimbursement for drug costs under the special refund categories were derived from the Finnish disease classification of the Social Insurance Institution,35 and data on purchases of prescription medication were derived from the Anatomical Therapeutic Chemical Classification.36,37 Precise definitions, coverage, and effects of these conditions were discussed in a previous study.31 The distribution of the control variables, excluding Finnish regions, is shown in Table 1 ▶.
TABLE 1—
Sample Characteristics of Finnish Adults 65 Years or Older Living With a Spouse at the Beginning of the Study Period, by Gender: Finland, December 1997
| Men (n = 78 151), % or mean (SD) | Women (n = 62 751), % or mean (SD) | |
| Age, y | 72.0 (5.6) | 71.2 (5.0) |
| Education | ||
| Tertiary or intermediate | 28.3 | 23.7 |
| Basic or less | 71.7 | 76.3 |
| Household income | ||
| Fifth quintile (highest) | 21.0 | 18.5 |
| Fourth quintile | 20.5 | 20.0 |
| Third quintile | 19.2 | 19.8 |
| Second quintile | 19.9 | 20.9 |
| First quintile (lowest) | 19.4 | 20.8 |
| Prevalence of chronic medical conditions | ||
| Cancer | 5.1 | 4.0 |
| Diabetes | 10.0 | 9.4 |
| Dementia | 0.5 | 0.4 |
| Psychosis | 1.3 | 2.2 |
| Depressive symptoms | 5.9 | 9.1 |
| Other mental health disorders | 3.7 | 3.9 |
| Parkinson’s disease | 1.8 | 1.4 |
| Other neurological diseases | 4.7 | 3.7 |
| Heart disease | 29.8 | 21.7 |
| Stroke | 2.5 | 1.3 |
| Chronic asthma or COPD | 7.7 | 6.8 |
| Other respiratory diseases | 3.7 | 2.0 |
| Arthritis | 2.5 | 4.8 |
| Osteoarthritis | 1.9 | 2.8 |
| Hip fracture | 0.4 | 0.6 |
| Other accident or violence | 3.0 | 2.9 |
| Other hospital diagnoses | 24.5 | 22.3 |
| Other diseases | 34.7 | 40.7 |
Note. COPD = chronic obstructive pulmonary disease.
Statistical Methods
Cox proportional hazards regression models were used to assess how a spouse’s death was associated with the risk of institutionalization. The outcome was the time from the start of the study until the first entry into long-term institutional care. Censoring occurred at the time of death or at the end of the follow-up. Bereavement or its duration was considered a time-varying covariate, and the reference category comprised those who had a spouse. The results were presented as hazard ratios (HRs). The controls were considered as time-invariant variables. We used Stata/SE 9.2 (StataCorp LP, College Station, TX) for all the analyses.
RESULTS
Duration of Widowhood
Among men, we observed a 71% higher risk of institutionalization for the bereaved than for persons living with a spouse, independent of the socioeconomic and control variables. The corresponding figure for women was 49% (Table 2 ▶). The excess risk of institutionalization was highest during the first month after the spouse’s death: 231% among men (HR = 3.31) and 262% among women (HR = 3.62; Figure 1 ▶). This excess risk decreased with time from the spouse’s death among both men and women, dropping to approximately 40% to 50% among men and 20% to 30% among women 1 year after bereavement. Although the overall excess risk of institutionalization among the bereaved stabilized at a somewhat higher level among men than among women after 1 year, the interaction between gender and the duration of widowhood was not statistically significant in the combined model for men and women.
TABLE 2—
Adjusted Hazard Ratios of Institutionalization Among Finnish Men and Women 65 Years or Older Living With a Spouse at the Beginning of Follow-Up, by Bereavement Status: Finland, 1998–2002
| Men (n=78151) | Women (n=62751) | |
| Institutionalized, % | 6.8 | 7.0 |
| Bereaved, % | 7.1 | 21.0 |
| Bereavement, HR (95% CI) | ||
| Not bereaved (Ref) | 1.00 | 1.00 |
| Bereaved | 1.71 (1.55, 1.87) | 1.49 (1.38, 1.61) |
Note. HR = hazard ratio; CI = confidence interval. Models included age, region of residence, education, household income, and chronic medical conditions as control variables.
FIGURE 1—
Adjusted hazard ratios and 95% confidence intervals of institutionalization in relation to duration of bereavement (not bereaved: hazard ratio=1) among men and women 65 years and older living with a spouse at the beginning of the follow-up study: Finland, 1998–2002.
Note. Models included age, region of residence, education, household income, and chronic medical conditions. Difference from duration category of 0 to 1 month at the 5% significance level (a); difference from previous duration category at the 5% significance level (b).
Buffers Against the Effects of Bereavement
Although high household income (fifth quintile [highest, reference category]; fourth quintile: HR = 1.08; 95% confidence interval [CI] = 1.00, 1.16; third quintile: HR = 1.21; 95% CI = 1.12, 1.30; second quintile: HR = 1.30; 95% CI = 1.21, 1.40; first quintile: HR = 1.29; 95% CI = 1.20, 1.38) and more education (reference category; less education: HR = 1.07; 95% CI = 1.01, 1.12) were associated with a lower risk of institutionalization, the overall effect of bereavement did not significantly vary according to the level of income or education (Table 3 ▶). Furthermore, the effect of the duration of widowhood was similar regardless of income.
TABLE 3—
Adjusted Hazard Ratios of Institutionalization in Relation to Duration of Bereavement Among Adults 65 Years or Older Living With a Spouse at the Beginning of Follow-Up, by Level of Education and Household Income: Finland, 1998–2002
| Education | Household Income | |||
| Tertiary or Intermediate (n = 36 984) | Basic or Less (n = 103 918) | Highest Quintile (n = 27 958) | Lower Quintiles (n = 112 944)a | |
| Institutionalized, % | 5.8 | 7.3 | 5.0 | 7.3 |
| Bereaved, % | 10.8 | 14.2 | 9.9 | 14.2 |
| Duration of bereavement, HR (95% CI) | ||||
| Not bereaved (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 0–2 mo | 2.02 (1.33, 3.08) | 3.03 (2.58, 3.56) | 2.77 (1.78, 4.32) | 2.88 (2.46, 3.37) |
| 2–6 mo | 1.83 (1.33, 2.53) | 1.67 (1.43, 1.95) | 1.89 (1.28, 2.80) | 1.68 (1.44, 1.95) |
| 6–12 mo | 2.14 (1.66, 2.77) | 1.69 (1.47, 1.93) | 1.69 (1.19, 2.39) | 1.78 (1.57, 2.03) |
| > 12 mo | 1.56 (1.32, 1.84) | 1.31 (1.20, 1.42) | 1.45 (1.18, 1.78) | 1.34 (1.23, 1.45) |
| P for interaction | .056 | .635 | ||
| Total bereaved, HR (95% CI) | 1.73 (1.52, 1.98) | 1.54 (1.44, 1.64) | 1.63 (1.38, 1.92) | 1.57 (1.47, 1.67) |
| P for interaction | .143 | .194 | ||
Note. HR = hazard ratio; CI = confidence interval. All models included gender, age, region of residence, education, household income, and chronic medical conditions as control variables.
aFour lowest income quintiles.
However, we detected a slightly different effect of duration of widowhood on institutionalization among more- and less-educated persons, although the difference was not significant. The excess risk of institutionalization seemed to be lower among the more versus the less educated immediately after the spouse’s death (first 2 months: HR=2.02 vs 3.03), but in the longer term, the more educated seemed to have a higher excess risk (e.g., after 1 year: HR=1.56 vs 1.31). Overall, we found no evidence of strong interactions between bereavement and education and income when these were assessed as rate differences (on the absolute scale; results not shown).
DISCUSSION
Duration of Widowhood
We found that the risk of entering long-term institutional care was higher among older adults who had lost their spouse than among those living with their spouse. The excess risk of institutionalization was highest during the first month after the spouse’s death—more than 3 times among both men and women—and decreased with time from bereavement, stabilizing at approximately 20% to 50% higher over 1 to 5 years. Our results cannot be compared with those of previous studies because no other large-scale prospective studies analyzing institutionalization in relation to the duration of widowhood are available. However, our findings are similar to those reported in mortality studies showing a larger immediate effect of bereavement that decreased with time from the spouse’s death.13,15,16,18–20,24,26–28 In Finland, however, the excess risk of institutionalization after the death of a spouse seems to be higher and more long term than the risk of death.18
The large excess risk of institutionalization occurring immediately after a spouse’s death may be related to the loss of social and instrumental support,19 in the form of care and help with daily activities such as help in cooking, cleaning, and shopping formerly shared with the deceased spouse. Furthermore, there may be nobody to provide personal care for bereaved persons with severe functional disabilities, and family members and medical professionals may recommend institutional care. Those most vulnerable to entering institutional care are likely to do so immediately after their spouse’s death; the risk of institutionalization is, on average, more moderate among those surviving longer after bereavement. The bereaved may also lose other social networks if these were mainly maintained by the spouse. The death of a spouse could also cause a fall in income, which may complicate living in the community.
The excess risk of institutionalization among the bereaved may also be related to emotional stress following the death of a loved partner. Grief and spousal loss may cause various symptoms, such as depression and anxiety, loss of appetite, sleep disturbances, fatigue, retardation of thought, loss of concentration, and changes in drug-taking habits, including an increase in the use of psychotropic medicines, alcohol, and tobacco.7 Furthermore, grief may cause increased susceptibility to physical diseases, for example, by lowering immunity to infections or aggravating stress-related diseases, including heart disease. These symptoms and their behavioral, psychic, and cognitive consequences may increase the risk of institutionalization.
Fortunately, a large proportion of the widowed are likely to recover from partner loss, and feelings of despair and anxiety diminish over time.11 Emotional recovery could be one of the underlying mechanisms explaining why the very large excess risk of entering institutional care among those recently bereaved dropped with time from the spouse’s death.
It has been suggested that the stronger short-term effects of widowhood on mortality may be caused by emotional stress and grief and the more moderate long-term effects by the loss of social, instrumental, and material support.18,19 However, the loss of spousal support in daily activities may be an important risk factor for institutionalization, even immediately after the spouse’s death, because eating properly and housekeeping are crucial in maintaining an independent life in the community.
Unfortunately, we were not able to directly investigate the mechanisms that mediated the effects of losing a spouse on institutionalization because of data limitations. For example, we did not have information on the role of the main caregiver or on change in chronic medical conditions during the follow-up. Furthermore, the data did not contain direct information on functional disabilities1,3,4,10,38,39 or childlessness,6 conditions that have been shown to be associated with institutionalization. The absence of a measure of childlessness may have led to the overestimation of the overall effect of widowhood on institutionalization if being childless was strongly associated with becoming widowed. However, the very large immediate short-term effect of widowhood that decreased with time was unlikely to be biased because of the absence of information on certain baseline characteristics.
Buffers Against the Effects of Bereavement
Our results indicated that neither high household income nor education buffered against the harmful effects of spousal loss. The lack of interactions between income and spousal loss could be related to the fact that, in Finland, publicly provided institutional care is equally accessible to all older persons regardless of income. Although user charges are tied to income, income is unlikely to influence bereaved persons’ decisions on institutional care. Clients in institutions are allowed to keep a minimum of 20% of their disposable income, or if income is very low, a fixed amount, for personal use.
The duration of widowhood had a slightly different association with the relative risk of institutionalization among more- and less-educated persons, although in an unexpected way. The harmful effects of bereavement seemed to be weaker among the more educated during the first 2 months after bereavement but became stronger as more time elapsed. However, the differences were not statistically significant. These results partly agree with a study on mortality in Israel indicating that the relative effect of bereavement is greater among more-educated men.20 However, Lusyne et al. indicated that more-educated persons in Belgium seemed to have relatively more excess mortality during the period immediately following the spouse’s death.28
Manor and Eisenbach suggested that highly educated men may have more to lose in bereavement because they enjoy several roles, including the head of the household and the main breadwinner.20 Furthermore, individuals with the most educational and financial resources and with more control over their circumstances may be emotionally more vulnerable to spousal loss. However, our results did not support the idea that persons with more education are emotionally more vulnerable to their spouse’s death, because they indicated a smaller short-term relative effect of bereavement.
Because having children,6 especially daughters,40 is known to reduce the probability of entering institutional care among older adults, it is likely that getting more help from children after a spouse’s death buffers the effects of bereavement on institutionalization, even in Finland, where contacts between older parents and their children are less frequent than in southern European countries.41 Further research is needed to examine whether the harmful effects of bereavement are smaller among those who have living children and whether daughters and sons play different roles in buffering the effects of spousal loss. More research is also needed to assess the effects of bereavement according to the disability status of the bereaved and to investigate in detail the mechanisms that mediate the effect of bereavement on institutionalization.
Conclusions
The follow-up data we used contained information on the dates of spousal death and admission into institutional care, providing a unique opportunity to study institutionalization after the death of a spouse. Our study showed a particularly high risk of institutionalization immediately after bereavement, which decreased over time. These results provide indirect evidence of the effect of the loss of social and instrumental support on the risk of institutionalization. Furthermore, we found that high levels of education and income did not buffer the effects of bereavement. Because long-term institutional care is extremely expensive for society, community-based home help services could be targeted to the bereaved immediately after a spouse’s death to reduce the need for institutional care.
Acknowledgments
This work was supported by the Finnish Post-Graduate School of Social Sciences/Population, Health, and Living Conditions; the Finnish Cultural Foundation; and the Academy of Finland (grant 213060). It was part of a European Union–funded research program on Major Ageing and Gender Issues in Europe (MAGGIE).
We thank Anja Noro and Unto Häkkinen, National Research and Development Centre for Welfare and Health, for their guidance in designing and using the database and Seppo Koskinen and Antti Reunanen, National Public Health Institute, for helping us with the hospital and medication registers.
Human Participant Protection Permission to use the register-based data was obtained from all register authorities involved, including Statistics Finland, the National Research and Development Centre for Welfare and Health (STAKES), and the Social Insurance Institution (permission TK 53-576-04 and TK 53-499-05).
Peer Reviewed
Contributors Both authors designed the study. E. Nihtilä led the writing and completed the analyses. P. Martikainen supervised the study and reviewed drafts of the article.
References
- 1.Branch LG, Jette AM. A prospective study of long-term care institutionalization among the aged. Am J Public Health. 1982;72:1373–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foley DJ, Ostfeld AM, Branch LG, Wallace RB, McGloin J, Cornoni-Huntley JC. The risk of nursing home admission in three communities. J Aging Health. 1992;4:155–173. [DOI] [PubMed] [Google Scholar]
- 3.Steinbach U. Social networks, institutionalization, and mortality among elderly people in the United States. J Gerontol. 1992;47(4):S183–S190. [DOI] [PubMed] [Google Scholar]
- 4.Wolinsky FD, Callahan CM, Fitzgerald JF, Johnson RJ. The risk of nursing home placement and subsequent death among older adults. J Gerontol. 1992; 47(4):S173–S182. [DOI] [PubMed] [Google Scholar]
- 5.Grundy E, Glaser K. Trends in, and transitions to, institutional residence among older people in England and Wales, 1971–91. J Epidemiol Community Health. 1997;51:531–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grundy E, Jitlal M. Socio-demographic variations in moves to institutional care 1991–2001: a record linkage study from England and Wales. Age Ageing. 2007;36: 424–430. [DOI] [PubMed] [Google Scholar]
- 7.Stroebe W, Stroebe MS. Bereavement and Health: The Psychological and Physical Consequences of Partner Loss. Cambridge, England: Cambridge University Press; 1987.
- 8.Bruce ML, Kim K, Leaf PJ, Jacobs S. Depressive episodes and dysphoria resulting from conjugal bereavement in a prospective community sample. Am J Psychiatry. 1990;147:608–611. [DOI] [PubMed] [Google Scholar]
- 9.Aartsen MJ, Van Tilburg T, Smits CH, Comijs HC, Knipscheer KC. Does widowhood affect memory performance of older persons?. Psychol Med. 2005;35: 217–226. [DOI] [PubMed] [Google Scholar]
- 10.Shapiro E, Tate R. Who is really at risk of institutionalization? Gerontologist. 1988;28:237–245. [DOI] [PubMed] [Google Scholar]
- 11.Hyrkäs K, Kaunonen M, Paunonen M. Recovering from the death of a spouse. J Adv Nurs. 1997;25: 775–779. [DOI] [PubMed] [Google Scholar]
- 12.Wolinsky FD, Johnson RJ. Widowhood, health status, and the use of health services by older adults: a cross-sectional and prospective approach. J Gerontol. 1992;47(1):S8–S16. [DOI] [PubMed] [Google Scholar]
- 13.Young M, Benjamin B, Wallis C. The mortality of widowers. Lancet. 1963;454–456. [DOI] [PubMed]
- 14.Parkes CM, Benjamin B, Fitzgerald RG. Broken heart: a statistical study of increased mortality among widowers. Br Med J. 1969;1:740–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mellström D, Nilsson A, Oden A, Rundgren A, Svanborg A. Mortality among the widowed in Sweden. Scand J Soc Med. 1982;10:33–41. [DOI] [PubMed] [Google Scholar]
- 16.Jagger C, Sutton CJ. Death after marital bereavement–is the risk increased? Stat Med. 1991;10: 395–404. [DOI] [PubMed] [Google Scholar]
- 17.Schaefer C, Quesenberry CP Jr, Wi S. Mortality following conjugal bereavement and the effects of a shared environment. Am J Epidemiol. 1995;141: 1142–152. [DOI] [PubMed] [Google Scholar]
- 18.Martikainen P, Valkonen T. Mortality after death of spouse in relation to duration of bereavement in Finland. J Epidemiol Community Health. 1996;50: 264–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martikainen P, Valkonen T. Mortality after the death of a spouse: rates and causes of death in a large Finnish cohort. Am J Public Health. 1996;86: 1087–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Manor O, Eisenbach Z. Mortality after spousal loss: are there socio-demographic differences? Soc Sci Med. 2003;56:405–413. [DOI] [PubMed] [Google Scholar]
- 21.Wolinsky FD, Johnson RJ. Perceived health status and mortality among older men and women. J Gerontol. 1992;47(6):S304–S312. [DOI] [PubMed] [Google Scholar]
- 22.Kiecolt-Glaser JK, Glaser R. Depression and immune function: central pathways to morbidity and mortality. J Psychosom Res. 2002;53:873–876. [DOI] [PubMed] [Google Scholar]
- 23.Nuotio M, Tammela TL, Luukkaala T, Jylhä M. Predictors of institutionalization in an older population during a 13-year period: the effect of urge incontinence. J Gerontol A Biol Sci Med Sci. 2003;58: 756–762. [DOI] [PubMed] [Google Scholar]
- 24.Kaprio J, Koskenvuo M, Rita H. Mortality after bereavement: a prospective study of 95 647 widowed persons. Am J Public Health. 1987;77:283–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones DR. Cancer mortality following widow(er)-hood: some further results from the office of population censuses and surveys longtudinal study. Stress Med. 1986;2:129–140. [Google Scholar]
- 26.Bowling A. Mortality after bereavement: a review of the literature on survival periods and factors affecting survival. Soc Sci Med. 1987;24:117–124. [DOI] [PubMed] [Google Scholar]
- 27.Martikainen P, Valkonen T. Do education and income buffer the effects of death of spouse on mortality? Epidemiology. 1998;9:530–534. [PubMed] [Google Scholar]
- 28.Lusyne P, Page H, Lievens J. Mortality following conjugal bereavement, Belgium 1991–96: the unexpected effect of education. Popul Stud (Camb). 2001; 55:281–289. [DOI] [PubMed] [Google Scholar]
- 29.Statistics Finland. Työssäkäyntitilaston laatuseloste [The quality of the labour force statistics]. Available at: http://www.stat.fi/til/tyokay/tyokay_2004-11-23_laa_001.html. Accessed December 1, 2006.
- 30.Official Statistics of Finland. Care and Services for Older People 2002. SVT: Social Security 2003:1. Helsinki, Finland: National Research and Development Centre for Welfare and Health; 2003.
- 31.Nihtilä EK, Martikainen PT, Koskinen SV, Reunanen AR, Noro AM, Häkkinen UT. Chronic conditions and the risk of long-term institutionalization among older people. Eur J Public Health. 2008;18:77–84. [DOI] [PubMed] [Google Scholar]
- 32.Organisation for Economic Co-operation and Development. The OECD List of Social Indicators. Paris, France: Organisation for Economic Co-operation and Development; 1982.
- 33.Suomen maakunnat [Finnish regions]. Available at: http://fi.wikipedia.org/wiki/Luokka:Suomen_maakunnat. Accessed November 11, 2006.
- 34.Sosiaali- ja terveysalan tutkimus- ja kehittämiskeskus [National Research and Development Centre for Welfare and Health]. Tautiluokitus ICD-10 [Finnish version of the International Statistical Classification of Diseases and Related Health Problems, 10th revision]. 2nd ed. Vol 1. Helsinki, Finland: Sosiaali- ja terveysalan tutkimus- ja kehittämiskeskus; 1999.
- 35.Kansaneläkelaitos [Social Insurance Institution]. Kansaneläkelaitoksen tilastollinen vuosikirja 1997 [Statistical Yearbook of the Social Insurance Institution, Finland, 1997], T1:33. Helsinki, Finland: Kansaneläkelaitos; 1998.
- 36.Lääkelaitos [National Agency for Medicines]. Lääkkeiden luokitus (ATC) ja määritellyt vuorokausiannokset (DDD) [Classification of medicines (ATC) and defined daily doses (DDD)]. Helsinki, Finland: Lääkelaitos; 1997.
- 37.Lääkelaitos [National Agency for Medicines]. Lääkkeiden luokitus (ATC) ja määritellyt vuorokausiannokset (DDD) [Classification of medicines (ATC) and defined daily doses (DDD)]. Helsinki, Finland: Lääkelaitos; 1998.
- 38.Aguero-Torres H, von Strauss E, Viitanen M, Winblad B, Fratiglioni L. Institutionalization in the elderly: the role of chronic diseases and dementia. Cross-sectional and longitudinal data from a population-based study. J Clin Epidemiol. 2001;54:795–801. [DOI] [PubMed] [Google Scholar]
- 39.Tomiak M, Berthelot JM, Guimond E, Mustard CA. Factors associated with nursing-home entry for elders in Manitoba, Canada. J Gerontol A Biol Sci Med Sci. 2000;55(5):M279–M287. [DOI] [PubMed] [Google Scholar]
- 40.Freedman VA. Family structure and the risk of nursing home admission. J Gerontol B Psychol Sci Soc Sci. 1996;51(2):S61–S69. [DOI] [PubMed] [Google Scholar]
- 41.Tomassini C, Kalogirou S, Grundy E, et al. Contacts between elderly parents and their children in four European countries: current patterns and future prospects. Eur J Ageing. 2004;1:54–63. [DOI] [PMC free article] [PubMed] [Google Scholar]