Abstract
A retrospective data analysis was conducted to evaluate the usefulness of baseline characteristics in predicting treatment response to antidepressant medication in 97 outpatients with nonpsychotic major depression treated for up to sixteen weeks with nefazodone. Baseline demographics (gender), illness features (symptom severity, length of illness, length of current episode, number of episodes, age of onset, longitudinal subtype, endogenicity, melancholia, family history of mood disorders), and social features (living status) were evaluated. Response to treatment was defined as a ≥ 50% reduction in the 17-item Hamilton Rating Scale for Depression (HRSD17) score. The results of a survival analysis indicated that patients with shorter histories of illness (< 4 years), a negative family history of depression, and those who were either married or were living with someone were more likely to have a positive outcome during the acute phase treatment of depression. The main findings are consistent with extensive previous literature indicating a better short-term outcome of depression where illness is shorter, where there is no family history, and where there is better social support.
Keywords: antidepressant, treatment predictor, social support, major depression
Introduction
Studies attempting to identify moderators and mediators of treatment (Baron and Kenny 1986; Kraemer et al 2002), such as baseline/pretreatment predictors of response to antidepressants, have not yielded consistent findings (Bielski and Friedel 1976; Greenhouse et al 1987; Katz et al 1987; Croughan et al 1988; Hooley and Teasdale 1989; Joyce and Paykel 1989; Kocsis et al 1989, 1990; Brugha et al 1990; Danish University Antidepressant Group 1990; Vallejo et al 1991; Keller et al 1992; Goodwin 1993; Hoencamp et al 1994; Friedman et al 1995; Baldwin et al 1996; Cohn et al 1996; Aliapoulous and Zisook 1996; Nierenberg 2003). The identified clinical predictors have typically fallen into the following categories: (1) demographic characteristics (gender); (2) illness features (severity at baseline, length of illness, age of onset, length of current episode, number of episodes, longitudinal subtype, endogenicity, melancholia, family history of mood disorders); and (3) social factors (living status, social support).
Numerous illness characteristics have been found to be associated with a positive response to antidepressant medications, including severity of depressive symptoms, depressive subtypes, age at onset of illness, and past history of depressive episodes (AHCPR 1993). Several studies have shown that specific features of psychiatric history and of the current episode of depression influence treatment outcomes. Reimherr et al (1990) found that patients with only a single episode of depression responded slightly better to SSRI treatment than those with recurrent episodes (sertraline: 62% vs 52%; amitriptyline: 66% vs 62%). Additionally, patients with melancholic features responded slightly better than those without such features (sertraline: 56% vs 50%; amitriptyline: 63% vs 59%). Based on a sample of patients with recurrent depression, Greenhouse et al (1987) also found age, symptom severity, and number of previous episodes associated with time to sustained treatment response. The most extensively studied area of treatment predictors includes history of illness characteristics, such as number of previous episodes, length of illness, and the presence of either single episode or recurrent longitudinal subtypes. However, findings are not consistent across all studies. Hoencamp et al (1994) demonstrated that the baseline Hamilton Rating Scale for Depression (HRSD) score was of greater significance in predicting recovery than other variables, such as premorbid history, symptomatology, and endogenous features (Danish University Antidepressant Group 1986). Greenhouse et al (1987) found that patients with high HRSD scores tended to take longer to stabilize than patients with lower scores. However, Pande and Sayler (1993) were unable to replicate this finding. Conversely, patients with less severe depressive illness have been shown to be more likely to respond to amitriptyline or imipramine than those with severe depressive illness (Croughan et al 1988). Family history has also been found to be a prognostic indicator of outcomes. When comparing patients who experience full interepisodic recovery with partial and non-interepisodic recovery patients, Akiskal (1982) found that patients with a family history (first degree biological relative) of affective disorders were more likely to have an incomplete recovery when treated with tricyclic antidepressants.
In addition to illness features that predict treatment response, researchers have attempted to examine the effects of social or situational factors on treatment outcome. Direct measures of social support and functioning, ie, Social Adjustment Scale, Social and Occupational Functioning Assessment Scale (Weissman and Bothwell 1976; APA 1994), and indirect measures such as living status have been found to be positively related to response. Vallejo and colleagues (1991) directly tested the effects of social support on response after 6 weeks of medication treatment. They found that patients treated with imipramine, with higher levels of social support showed a greater percent decrease in HRSD scores than patients with lower levels of social support. Tomaszewska and colleagues (1996) obtained similar results in a population of patients with non-melancholic depression, and found higher levels of social support in those patients who responded favorably to treatment.
The vast majority of research evaluating the relationship between social support and major depressive disorder (MDD) has largely focused on the role played by social support in improving clinical outcomes in general. Research has not focused as much on patients being treated specifically with antidepressant medications or psychotherapy. The relationship between social support and psychological wellbeing has long been documented (Myers et al 1975; Dean and Lin 1977; Andrews et al 1978; Cohen and Wills 1985). Studies have suggested that social support plays a significant role in mediating the development of depressive symptoms by buffering the effects of negative life events (Aneshensel and Stone 1982; Brown 1988; George et al 1989; Zlotnick et al 1996). Brugha et al (1997) found that patients with a longer course of illness, as manifested by multiple recurrent episodes, reported significantly lower levels of social support than patients with a shorter course of illness. Ezquiaga et al (1998) found that the psychological support provided by a spouse was significant, with high levels of support being associated with positive treatment outcomes. In a sample of 552 women aged 18–65, Costello (1982) found that lack of intimacy with a spouse or cohabitant and lack of a confidant were associated with clinically significant levels of depression. Hooley and Teasdale (1989) found, in a 9-month post-hospitalization follow-up of patients with unipolar depression, that patients with higher levels of marital discord had significantly higher relapse rates. Coyne and colleagues (2002) found higher levels of marital distress in depressed females than in community controls. Interestingly, there appear to be gender differences in the reporting of marital distress, with depressed females reporting higher levels of marital distress than their partners (Ensel 1982; Crowther 1985). In their 1992 study, Goering et al found that in a population of women with MDD, few demographic or clinical factors were related to the course of symptoms over the 6-month study period. Recovery was predicted based on the patients’ ratings of their current marital relationship and by the spousal rating of their premorbid relationship.
The purpose of this study was to identify baseline demographic, illness, and social features that predict response to an antidepressant medication, nefazodone, in patients with MDD. The demographic, illness, and social feature predictors evaluated were: gender, age of onset, severity at baseline, length of illness, length of current episode, number of episodes, longitudinal subtype, endogenicity, melancholia, family history of mood disorders, and living status.
Methods
Subjects
Participants in this study were 97 outpatients with MDD: 59 females and 38 males, age 38.5 ± 10.0 (mean ± SD). They were treated for up to sixteen weeks with nefazodone in the Department of Psychiatry, The University of Texas Southwestern Medical Center, Dallas, USA. This sample has been reported as part of a larger multicenter trial (Trivedi et al 2001). Prior to interview, all patients provided written informed consent. All participants met the Structured Clinical Interview for DSM-III-R (SCID) (Spitzer et al 1992) criteria for MDD and were 18 years of age or older. The duration of the current major depressive episode was ≥ 6 months. Patients with bipolar disorder, seasonal affective disorder, substance abuse or dependence disorders, as well as those with delusions or hallucinations during the current episode, were excluded. Patients judged to be at serious risk of suicide and those with a concurrent diagnosis of organic mental syndrome, schizophrenia, or any other psychotic disorder, were not included in the sample. All patients had a 17-item Hamilton Rating Scale for Depression (HRSD17) (Hamilton 1960, 1967) score ≥ 20 at the baseline evaluation. See Table 1.
Table 1.
Predictors of response to antidepressants: baseline
| Predictors of response | n | Mean | SD | % |
|---|---|---|---|---|
| Age | 97 | 38.5 | 10.0 | |
| Females/Males | 97 | 60.8/39.2 | ||
| Marital status | 97 | |||
| Single | 19.6 | |||
| Engaged | 1.0 | |||
| Married | 37.1 | |||
| Cohabiting | 8.2 | |||
| Divorced | 32.0 | |||
| Widowed | 2.1 | |||
| HRSD at baseline | 97 | 23.9 | 2.1 | |
| Age at onset | 96 | 25.1 | 11.0 | |
| Length of illnessa | 96 | 13.2 | 9.7 | |
| Length of current episode | 97 | 67.0 | 75.8 | |
| Number of episodes | 95 | 2.3 | 1.9 | |
| Single/Recurrent | 95 | 40.0/60.0 | ||
| Endogenous/Nonendogenous | 81 | 42.0/58.0 | ||
| Melancholic/Nonmelancholic | 97 | 43.3/56.7 | ||
| Family history of affective disorder(Positive/Negative) | 94 | 36.2/63.8 |
Months
Abbreviations: HRSD, Hamilton Rating Scale for Depression.
Procedures
Patients were evaluated at baseline using a SCID to obtain demographic (age and gender), social (living status), and illness features (length of episode, depressive subtype, age at onset, recurrence, length of illness, number of episodes, family history of depression). Melancholia was characterized based on the SCID (Spitzer et al 1992), and endogenicity was defined using the Research Diagnostic Criteria (Spitzer et al 1977). Symptom severity was assessed at baseline using the HRSD17 and the thirty-item Inventory of Depressive Symptomatology – Clinician Rated (IDS-C30) (Rush et al 1986, 1996) and again with the HRSD17 at weeks 1, 2, 3, 4, 6, 8, 10, 12, and 16. Nefazodone was administered twice daily for 12 weeks. Dosages were titrated up to 400 mg/day by the end of the second week. Patients not responding to the initial titration schedule were titrated to 500 or 600 mg/day after week 3. Patients were restricted from concomitant use of other drugs except lorazepam, temazepam, or oxazepam.
Statistical analysis
Cox’s proportional hazard models (Cox 1972) were used to test for differences in treatment response for a series of demographic, social support, and illness features. The demographic characteristic and social support predictors evaluated were gender and living status, respectively. Illness features included length and severity of current episode, length of illness, number of episodes, age at onset, longitudinal subtype, endogenicity (Spitzer et al 1977), melancholia (Spitzer et al 1992), and family history of mood disorders. For these analyses response to treatment was defined as a >50% reduction in the baseline HRSD total score.
Results
Demographic and social features
The analysis of living status indicated better response to treatment for the married patients (married or cohabiting) than those patients living alone (single, engaged, divorced, widowed): 84% and 51%, respectively (χ2 = 6.9, df = 1, p < 0.009). While the response rates were similar in the first few weeks of treatment, after week 4, married patients show clearly higher rates of response than the unmarried patients (see Figure 1). This result is qualified by differences in the dropout rates (single, 34%; married, 14%). There was no statistically significant effect for gender. See Table 2.
Figure 1.
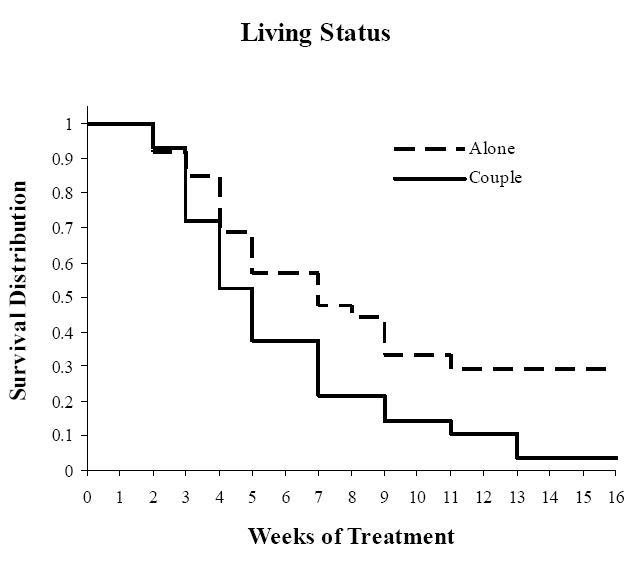
Estimated likelihood of response based on Cox’s regression analyses for living status.
Table 2.
Predictors of response to antidepressants and baseline HRSD
| Baseline HRSD | |||
|---|---|---|---|
| Predictors of response | n | Mean | SD |
| Gender | |||
| Female | 59 | 23.9 | 2.2 |
| Male | 38 | 23.8 | 2.1 |
| Marital statusa | |||
| Unmarried | 53 | 23.9 | 1.9 |
| Married | 44 | 23.8 | 2.4 |
| Age at onset | |||
| 0–19 | 40 | 23.8 | 2.1 |
| 20+ | 56 | 23.9 | 2.2 |
| Length of illnessa | |||
| 0–9 | 42 | 24.1 | 2.4 |
| 10+ | 54 | 23.7 | 1.9 |
| Length of current episode | |||
| 0–48 | 50 | 24.0 | 2.2 |
| 49+ | 47 | 23.7 | 2.1 |
| Number of episodes | |||
| 1 | 40 | 23.9 | 2.1 |
| 2 | 26 | 23.9 | 2.6 |
| 3+ | 30 | 23.8 | 1.9 |
| Single | 38 | 23.9 | 2.1 |
| Recurrent | 57 | 23.8 | 2.2 |
| Endogenous | 34 | 23.3 | 1.4 |
| Nonendogenous | 47 | 24.4 | 2.7 |
| Melancholic | 42 | 24.5 | 2.5 |
| Nonmelancholic | 55 | 23.4 | 1.7 |
| Family history of affective disorder | |||
| Positive | 34 | 23.8 | 2.4 |
| Negative | 60 | 23.9 | 2.0 |
p < 0.05 comparing 2 subgroups (survival analysis).
Abbreviations: HRSD, Hamilton Rating Scale for Depression.
Illness features
Four predictors were used to create a test for differences in response based on characteristics of the current depressive episode: severity (HRSD score 20–23 vs HRSD score ≥ 24); length of the current episode (0–48 months vs > 49 months (this median split provided sample size for the two groups to make a reasonable comparison)); endogenous vs nonendogenous; and melancholic vs nonmelancholic. Length of the current episode revealed that patients whose current episode was less than 4 years were more likely to respond (70%) than those with longer current episodes (62%). This effect was marginally significant (χ2 = 3.2, df = 1, p < 0.08). Dropout rates were about the same for these two groups (28% and 26%, respectively). Since chronic depression has been defined as episodes lasting 2 years or more, a secondary analysis was conducted using a 24-month threshold to distinguish short vs longer current episodes. No statistically significant differences were found. Baseline severity, endogenicity, and the presence of melancholia were not significantly related to treatment response.
Four measures were used to define strata based on history of illness (single vs recurrent; age at onset: 1–19 vs 20 or older; length of illness: 0–9 years vs > 10 years; and number of episodes: 1 vs 2 vs 3 or more). Length of illness was significantly related (χ2 = 5.2, df = 1, p < 0.03) to outcome. Patients with shorter illnesses were more likely to respond than those with longer illnesses (see Figure 2). Single versus recurrent depression, age of onset, and number of episodes were not significantly related to treatment response.
Figure 2.
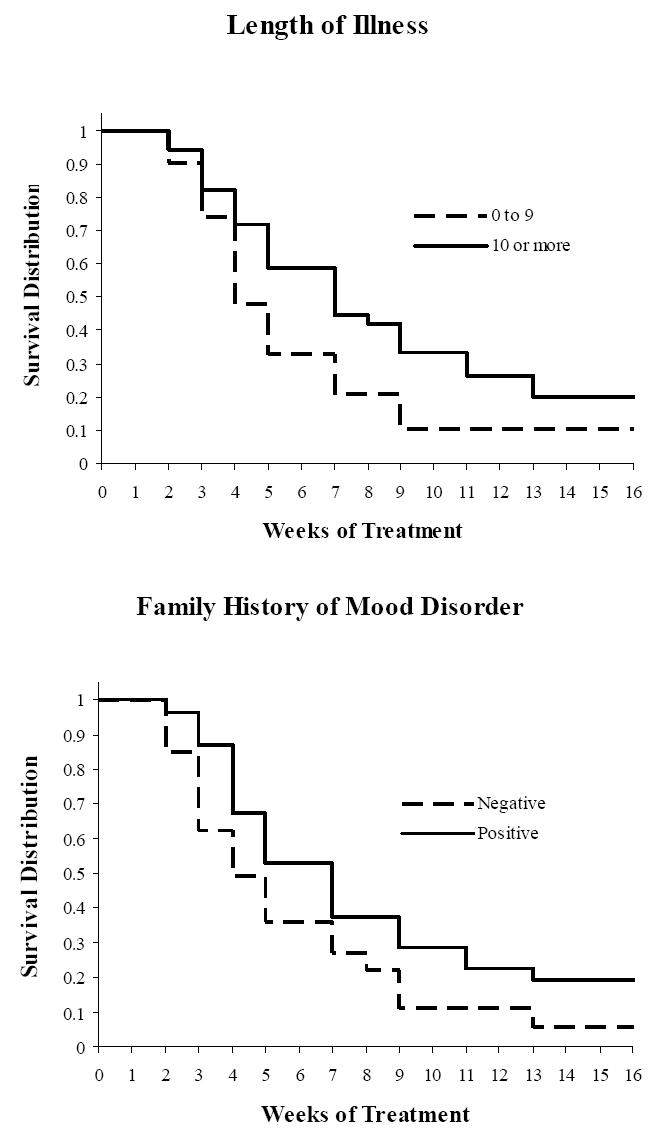
Estimated likelihood of response based on Cox’s regression analyses for length of illness and family history of depression.
Strata were created based on a positive versus negative family history of major mood disorders in first-degree relatives. There was a significant difference based on family history (χ2 = 4.6, df = 1, p < 0.04). Patients with a negative family history were more likely to respond (77%) than those with a positive family history (62%) (see Figure 2). Dropout rates before completing 16 weeks of treatment were similar (21% and 30%, respectively).
Analyses of combined predictors
To explore the relationships between individual baseline features that predicted response, survival analysis was conducted and included all three individual predictors: marital status, length of illness, and family history. Once living status entered the model, no other predictors significantly improved the model. Thus, there was substantial overlap between these individual predictors, as might be expected in this relatively small sample. The parallel analyses conducted using an HRSD score ≥ 10 criteria produced the same results for living status (χ2 = 7.7, df = 1, p < 0.006) and length of illness (χ2 = 4.3, df = 1, p < 0.04). A significant difference, as opposed to a marginal difference, was found for length of episode (χ2 = 4.3, df = 1, p < 0.04). Only one major difference was found for the single vs recurrent depression groups. A significant difference was found using this response criterion (χ2 = 4.6, df = 1, p < 0.04). Patients with a recurrent history responded better than those in their first episode.
Discussion
The results of this study suggest that three easily discernable patient characteristics can help predict a patient’s response to antidepressant medication, in this case, nefazodone. The characteristics found to be most useful were, living status, total length of illness, and family history of depression. The findings associated with illness features are consistent with previous studies reporting longer current episodes associated with a lower likelihood of response to antidepressants (Bielski and Friedel 1976; Rush et al 1983; Keller et al 1984, 1992).
Although more elaborate methods of outcome prediction such as receptor analysis or neuroimaging (Espisito and Goodnick 2003) may be useful, they have not yet led to consistent findings and are very likely not to be practical in routine clinical practice. The results of this study suggest, simple, easy to obtain data, such as marital status, show great promise in the prediction of response to antidepressant treatment. Interestingly, in our sample, being married or living together appeared to have a profound positive effect on the overall response rates, with married or cohabiting patients meeting criteria for treatment response with greater frequency than their single cohorts. Living status also had an impact on the patients’ willingness to stay in treatment. The married/cohabiting group remained in treatment longer even in the absence of response, a finding consistent with Hagerty and Williams (1999) who found patients living alone were more likely to drop out of treatment. Numerous drug utilization studies have shown that over 45%–50% of patients who start an antidepressant are not in treatment by 3 months, suggesting a strong need to be able to preemptively identify predictors of not only response but also dropouts. While not all studies have found social support to be a significant predicator of treatment outcome (Hirshfeld et al 1986; George et al 1989), the majority of the studies have suggested social support and even more specifically marital status as positive predictors of response. The quality of the marital relationship also provides a significant aid in predicting treatment response. Moreover, recent data from a number of studies (Hunkeler et al 2000; Unutzer et al 2002; Trivedi et al 2004) suggest there is a clear benefit for a disease management approach in the treatment of depression. These studies have emphasized more frequent patient contact as well as more robust psychosocial and educational support for patients to enhance adherence, improve the patient’s ability to self-monitor their symptoms, and increase patients’ understanding of the chronic medical illness nature of their depressive disorders. These data thus provide another dimension of evidence that optimal outcome can be enhanced if pharmacotherapy is augmented with social support.
The current study is limited by several factors including a moderate sample size, the use of only one antidepressant medication, and the lack of a placebo control group. It is also possible that factors indicating a chronic and or severe disorder like length of illness may predict poorer outcome irrespective of the treatment(s) used. Moreover, it is also likely that social support, life stressors, and family history of psychiatric comorbidity are indicators of positive outcome for MDD across various treatment modalities and may also increase the chances of spontaneous response. Therefore, in the absence of a placebo or an active control, the demographic and clinical features identified may be thought of as good prognostic predictors of outcome independent of treatment modality. Despite these limitations, the current study does provide additional support for the hypothesis that easy to identify patient factors may be able to significantly improve the quality of patient care by increasing physician efficiency when prescribing anti-depressant medications. These clinical predictors, although not prescriptive, can assist in treatment planning and aid with patient education regarding potential outcomes. Of the three clinical predictors identified (living status, total length of illness, and family history of depression), living status appears to be the most promising mediator of treatment outcome. Future study of clinical predictors of treatment response for emerging antidepressant medications should include social features, such as living status and an assessment of the quality of relationships, in addition to the commonly used demographic and illness features in predictor analyses.
Acknowledgments
This report was supported in part by a contract from Bristol Myers Squibb and funded in part by NIMH grants (1UO1 MH61562-01A2 MHT) (R01MH064062-01A2 MHT) and Lydia Bryant Test Professorship in Psychiatric Research (MHT). The authors appreciate the assistance of Melissa Haldeman and the administrative support of Eric Nestler, Professor and Chairman, Department of Psychiatry, University of Texas Southwestern Medical Center.
References
- [AHCPR] Agency for Health Care Policy and Research. Depression in primary care: volume 2. Treatment of major depression. Clinical practice guideline nr 5. AHCPR publication nr 93-0551. Rockville, MD: AHCPR; 1993. [Google Scholar]
- Akiskal HS. Factors associated with incomplete recovery in primary depressive illness. J Clin Psychiatry. 1982;43:266–71. [PubMed] [Google Scholar]
- Aliapoulous J, Zisook S. Tricyclic antidepressants medications. In: Goodnick PJ, editor. Predictors of treatment response in mood disorders. Clinical practice. Washington: American Psychiatric Pr; 1996. pp. 1–36. [Google Scholar]
- Andrews G, Tennant C, Hewson DM, et al. Life event stress, social support, coping style and risk of psychological impairment. J Nerv Dis. 1978;166:307–16. doi: 10.1097/00005053-197805000-00001. [DOI] [PubMed] [Google Scholar]
- Aneshensel CS, Stone JD. Stress and depression. Arch Gen Psychiatry. 1982;39:1392–6. doi: 10.1001/archpsyc.1982.04290120028005. [DOI] [PubMed] [Google Scholar]
- [APA] American Psychiatric Association. Diagnostic and statistical manual of mental disorders – Fourth edition (DSM-IV) Washington: APA; 1994. [Google Scholar]
- Baldwin DS, Hawley CJ, Abed RT, et al. A multicenter double-blind comparison of nefazodone and paroxetine in the treatment of outpatients with moderate-to-severe depression. J Clin Psychiatry. 1996;57(Suppl 2):46–52. [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychology research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bielski RJ, Friedel RO. Predictors of tricyclic antidepressant response: a critical review. Arch Gen Psychiatry. 1976;33:1479–89. doi: 10.1001/archpsyc.1976.01770120083009. [DOI] [PubMed] [Google Scholar]
- Brown GW, Adler Z, Bifulco A. Life events, difficulties and recovery from chronic depression. Br J Psychiatry. 1988;152:487–98. doi: 10.1192/bjp.152.4.487. [DOI] [PubMed] [Google Scholar]
- Brugha TS, Bebbington PE, MacCarthy B, et al. Gender, social support and recovery from depressive disorders: a prospective clinical study. Psychol Med. 1990;20:147–56. doi: 10.1017/s0033291700013325. [DOI] [PubMed] [Google Scholar]
- Brugha TS, Bebbington PE, Stretch DD, et al. Predicting the short-term outcome of first episodes and recurrences of clinical depression: a prospective study of life events, difficulties, and social support networks. J Clin Psychiatry. 1997;58:298–306. doi: 10.4088/jcp.v58n0703. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–57. [PubMed] [Google Scholar]
- Cohn CK, Robinson DS, Roberts DL, et al. Responders to antidepressant drug treatment: a study comparing nefazodone, imipramine, and placebo in patients with major depression. J Clin Psychiatry. 1996;57(Suppl 2):15–18. [PubMed] [Google Scholar]
- Costello CG. Social factors associated with depression: a retrospective community study. Psychol Med. 1982;12:329–39. doi: 10.1017/s0033291700046663. [DOI] [PubMed] [Google Scholar]
- Cox DR. Regression models and life tables. J R Stat Soc. 1972;334:187–220. [Google Scholar]
- Coyne JC, Thompson R, Palmer SC. Marital quality, coping with conflict, marital complaints, and affection in couples with a depressed wife. J Fam Psychol. 2002;16:26–37. doi: 10.1037//0893-3200.16.1.26. [DOI] [PubMed] [Google Scholar]
- Croughan JL, Secuda SK, Katz MM, et al. Sociodemographic and prior clinical course characteristics associated with treatment response in depressed patients. J Psychiatric Res. 1988;22:227–37. doi: 10.1016/0022-3956(88)90008-8. [DOI] [PubMed] [Google Scholar]
- Crowther JH. The relationship between depression and marital maladjustment. A descriptive study. J Nerv Ment Dis. 1985;173:227–31. doi: 10.1097/00005053-198504000-00004. [DOI] [PubMed] [Google Scholar]
- Danish University Antidepressant Group. Citalopram: clinical effect profile in comparison with clomipramine. A controlled multicenter study. Psychopharmacology (Berl) 1986;90:131–8. doi: 10.1007/BF00172884. [DOI] [PubMed] [Google Scholar]
- Danish University Antidepressant Group. Paroxetine: a selective serotonin reuptake inhibitor showing better tolerance but weaker antidepressant effect than clomipramine in a controlled multicenter study. J Affect Disord. 1990;18:289–99. doi: 10.1016/0165-0327(90)90081-i. [DOI] [PubMed] [Google Scholar]
- Dean A, Lin N. The stress-buffering role of social support. Problems and prospects for systematic investigation. J Nerv Ment Dis. 1977;165:403–17. doi: 10.1097/00005053-197712000-00006. [DOI] [PubMed] [Google Scholar]
- Ensel WM. The role of age in the relationship of gender and marital status to depression. J Nerv Ment Dis. 1982;170:536–43. doi: 10.1097/00005053-198209000-00004. [DOI] [PubMed] [Google Scholar]
- Esposito K, Goodnick P. Predictors of response in depression. Psychiatr Clin North Am. 2003;26:353–65. doi: 10.1016/s0193-953x(02)00104-1. [DOI] [PubMed] [Google Scholar]
- Ezquiaga E, Garcia A, Bravo F, et al. Factors associated with outcome in major depression: a 6-month prospective study. Soc Psychiatry Psychiatr Epidemiol. 1998;33:552–7. doi: 10.1007/s001270050093. [DOI] [PubMed] [Google Scholar]
- Friedman RA, Parides M, Baff R, et al. Predictors of response to desipramine in dysthymia. J Clin Psychopharmacol. 1995;15:280–3. doi: 10.1097/00004714-199508000-00007. [DOI] [PubMed] [Google Scholar]
- George LK, Blazer DG, Hughes DC, et al. Social support and the outcome of major depression. Br J Psychiatry. 1989;154:478–85. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- Goering PN, Lancee WJ, Freeman SJ. Marital support and recovery from depression. Br J Psychiatry. 1992;160:76–82. doi: 10.1192/bjp.160.1.76. [DOI] [PubMed] [Google Scholar]
- Goodwin FK. Predictors of antidepressant response. Bull Minninger Clin Spring. 1993;57:146–60. [PubMed] [Google Scholar]
- Greenhouse JB, Kupfer DJ, Frank E, et al. Analysis of time to stabilization in the treatment of depression biological and clinical correlates. J Affect Disord. 1987;13:259–66. doi: 10.1016/0165-0327(87)90045-0. [DOI] [PubMed] [Google Scholar]
- Hagerty BM, Williams BA. The effects of sense of belonging, social support, conflict, and loneliness on depression. Nurs Res. 1999;48:215–19. doi: 10.1097/00006199-199907000-00004. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol, Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–96. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Klerman GL, Andreasen NC, et al. Psycho-social predictors of chronicity in depressed patients. Br J Psychiatry. 1986;148:648–54. doi: 10.1192/bjp.148.6.648. [DOI] [PubMed] [Google Scholar]
- Hoencamp E, Haffmans PM, Duivenvoorden H, et al. Predictors of (non-) response in depressed outpatients treated with three-phase sequential medication strategy. J Affect Disord. 1994;31:235–46. doi: 10.1016/0165-0327(94)90099-x. [DOI] [PubMed] [Google Scholar]
- Hooley JM, Teasdale JD. Predictors of relapse in unipolar depressives: expressed emotion, marital distress, and perceived criticism. J Abnorm Psychol. 1989;98:229–35. doi: 10.1037//0021-843x.98.3.229. [DOI] [PubMed] [Google Scholar]
- Hunkeler EM, Meresman JF, Hargreaves WA, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Arch Fam Med. 2000;9:700–8. doi: 10.1001/archfami.9.8.700. [DOI] [PubMed] [Google Scholar]
- Joyce PR, Paykel ES. Predictors of drug response in depression. Arch Gen Psychiatry. 1989;46:89–99. doi: 10.1001/archpsyc.1989.01810010091014. [DOI] [PubMed] [Google Scholar]
- Katz MM, Koslow SH, Maas JW, et al. The timing, specificity and clnical prediction of tricylic drug effects in depression. Psychol Med. 1987;17:297–309. doi: 10.1017/s0033291700024831. [DOI] [PubMed] [Google Scholar]
- Keller MB, Klerman GL, Lavori PW. Long-term outcomes of episodes of major depression: clinical and public significance. J Am Med Assoc. 1984;252:788–92. [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Mueller TL, et al. Time to recovery, chronicity, and levels of psychopathology in major depression. A 5-year prospective follow-up of 431 subjects. Arch Gen Psychiatry. 1992;49:809–16. doi: 10.1001/archpsyc.1992.01820100053010. [DOI] [PubMed] [Google Scholar]
- Kocsis JH. New issues in the prediction of antidepressant response. Psychopharmacol Bull. 1990;26:49–53. [PubMed] [Google Scholar]
- Kocsis JH, Mason BJ, Frances AJ, et al. Prediction of response of chronic depression to imipramine. J Affect Disord. 1989;17:255–60. doi: 10.1016/0165-0327(89)90008-6. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, et al. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59:877–83. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Myers JK, Lindenthal JJ, Pepper MP. Life events, social integration and psychiatric symptomatology. J Health Soc Behav. 1975;16:421–7. [PubMed] [Google Scholar]
- Nierenberg AA. Predictors of response to antidepressants general principals and clinical implications. Psychiatr Clin North Am. 2003;26:345–52. doi: 10.1016/s0193-953x(02)00105-3. [DOI] [PubMed] [Google Scholar]
- Pande AC, Sayler ME. Severity of depression and response to fluoxetine. Int Clin Psychopharmacol. 1993;8:243–5. doi: 10.1097/00004850-199300840-00006. [DOI] [PubMed] [Google Scholar]
- Reimherr FW, Chouinard G, Cohn CK. Antidepressant efficacy of sertraline: a double-blind, placebo- and amitriptyline-controlled, multicenter comparison study in outpatients with major depression. J Clin Psychiatry. 1990;51(Suppl B):18–27. [PubMed] [Google Scholar]
- Rush AJ, Giles DE, Schlesser MA, et al. The inventory for depressive symptomatology (IDS): preliminary findings. Psychiatry Res. 1986;18:65–87. doi: 10.1016/0165-1781(86)90060-0. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, et al. The inventory of depressive symptomatology (IDS): psychometric properties. Psychol Med. 1996;26:477–86. doi: 10.1017/s0033291700035558. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Roffwarg HP, Giles DE, et al. Psychobiological predictors of antidepressant drug response. Pharmacopsychiatria. 1983;16:192–4. doi: 10.1055/s-2007-1019497. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria for a selected group of functional disorders. New York: New York State Psychiatric Institute; 1977. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, et al. The structured clinical interview for DSM-III-R (SCID) I: history, rationale, and description. Arch Gen Psychiatry. 1992;49:624–9. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Tomaszewska W, Peselow ED, Barouche F, et al. Antecedent life events, social supports and response to antidepressants in depressed patients. Acta Psychiatr Scand. 1996;94:352–7. doi: 10.1111/j.1600-0447.1996.tb09872.x. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Rush AJ, Crismon ML, et al. The Texas Medication Algorithm Project (TMAP): clinical results for patients with major depressive disorder. Arch Gen Psychiatry. 2004;61:669–80. doi: 10.1001/archpsyc.61.7.669. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Rush AJ, Pan JY, et al. Which depressed patients respond to nefazodone and when? J Clin Psychiatry. 2001;62:158–63. doi: 10.4088/jcp.v62n0304. [DOI] [PubMed] [Google Scholar]
- Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting. JAMA. 2002;288:2836–45. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Vallejo J, Gasto C, Catalan R, et al. Predictor of antidepressant treatment outcome in melanchol: psychosocial, clinical, and biological indicators. J Affect Disord. 1991;21:151–62. doi: 10.1016/0165-0327(91)90036-r. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiatry. 1976;33:1111–15. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Shea T, Pilkonis PA, et al. Gender, type of treatment, dysfunctional attitudes, social support, life events, and depressive symptoms over naturalistic follow-up. Am J Psychiatry. 1996;153:1021–7. doi: 10.1176/ajp.153.8.1021. [DOI] [PubMed] [Google Scholar]


