Abstract
There is a dearth of research that examines the impact of family systems therapy on problems among sexually and/or physically abused youth. Given this void, differential outcome and predictors of substance use change were evaluated for abused, as, compared with nonabused, runaway adolescents who were randomly assigned to family therapy or treatment as usual Abused adolescents reported lower family cohesion at baseline, although both abused and nonabused adolescents showed similar substance use reductions. Utilizing hierarchical linear modeling, we found that substance use changed with change in cohesion over time. These findings link change in family functioning to change in adolescent substance use, supporting family systems theory. Findings suggest that a potent target of intervention involves focus on increasing positive communication interactions.
INTRODUCTION
The National Child Abuse and Neglect Data System (NCANJDS) reported that in 2002 an estimated 1,800,000 referrals were made alleging child abuse or neglect to state and local child protective services agencies. Of these referrals, 896,000 children were determined to be victims of child abuse by the Child Protective Services (CPS) agencies. Even with this high number of youth and families affected by abuse, the consensus within the literature is that there are few rigorousty designed treatment evaluation studies for maltreated youth (Cohen & Mannarino, 1998; James & Mennen, 2001; Stevenson, 1999). Several researchers have noted that treatment efforts are still in the early stage of development, and more attention is needed for identifying effective interventions (Finkelhor & Berliner 1995; Kolko, 1996; Swenson & Spratt, 1999). To that end, this study examined substance abuse treatment] outcome and its predictors among physically and/or sexually abused adolescents.
It has been suggested that there is no special sexually abused children’s syndrome or symptom characteristic of a majority of such children (Finkelhor & Berliner, 1995; Kendall-Tackett, Williams, & Finkelhor, 1993). Physical and/or sexual abuse affects diverse sets of youth with a wide range of ages, backgrounds, and associated symptom presentations. Problem behavior patterns vary by age as well, with running away or substance use typical of older children and nightmares and anxiety more typical of younger children (Finkelhor & Berliner, 1995).
Stevenson (1999) and Beutler and Hill (1992) suggest that the lack of a specific childhood abuse syndrome and the diversity of those affected calls into question whether specific therapies are required for abuse or whether treatment should focus on the presenting symptoms rather than on child abuse specifically. These authors question whether therapy should focus on the youth’s history of physical and/or sexual abuse or on issues, such as depression or substance abuse, that prompt treatment seeking. Finkelhor and Berliner (1995) conclude that, because of the diversity among abused children and families, it is unlikely that any one therapy will be effective for all children and families. These researchers note that treatment evaluation with a homogeneous group with similar symptoms allows an intervention to be systematically administered and evaluated. This study included a relatively homogeneous group of physically and/or sexually abused adolescents as they had run away from home and were substance abusing.
Child Sexual and Physical Abuse
Finkelhor and Berliner (1995) reviewed 29 studies examining treatment outcome with sexually abused children and adolescents. Of these, five published studies used an experimental design in which children were randomly assigned to a treatment condition; only two of the studies (Baker, 1987; Monck et al, 1994) included adolescent participants. In both studies, client outcomes improved with treatment, though outcomes were similar across conditions.
More recently, Cohen and colleagues (Cohen, Deblinger, Mannarino, & Steer, 2004; Cohen & Mannarino, 1998, 2000) compared the efficacy of trauma-focused, cognitive-behavioral therapy (TF-CBT) and child-centered therapy for treating posttraumatic stress disorder and other emotional/behavioral problems in children aged 8 to 14 years who had a history of sexual abuse. These researchers found that those children and parents assigned to the TF-CBT, as compared to those assigned to the child-centered therapy, demonstrated greater improvement along many dimensions, such as depression, behavior problems, abuse-related distress/attributions and parenting practices.
Compared with studies on child sexual abuse, even fewer studies have examined treatment with physically abused children (James & Mennen, 2001). Milner and Chilamkurti (1991) noted that parental aggression, parental distress, and family conflict are risk factors for childhood physical abuse. Given the role of parents in the abuse of their children, most treatment-outcome research has focused on treatment of the parent, excluding the family or child. However, comprehensive treatment targeting multiple systems has the advantage over individual treatment models through addressing the many needs of children and their families (Swenson & Spratt, 1999).
A review of the treatment literature notes that most of the treatment outcome studies examining childhood physical abuse were conducted in the 1980s with few new studies identified. Only five randomized trials were identified by James and Mennen (2001), and of these none included adolescents. However, Kolko (1996) compared a family therapy (FT) intervention with a cognitive-behavioral treatment (CBT) and routine community care for 55 physically maltreated children between 6 and 13 years old. Both CBT and FT were associated with less violence and externalizing behavior, parental distress and abuse risk, and family conflict as well as higher cohesion. All three conditions showed time effects across many areas of functioning.
Runaways
Rotheram-Borus (1991) notes that the lack of a supportive family may be the largest factor associated with adolescent running away. Several researchers have noted that childhood abuse increases the likelihood that a youth will run away from home (Kaufman & Widom, 1999; Sullivan & Knutson, 2000). Runaway youth frequently cite physical and sexual abuse, family violence, and/or high conflict among family members as reasons for leaving home (Lindsey, Kurtz, Jarvis, Williams, & Nackerud, 2000). In fact, between 21% and 60% of these youth report being sexually abused, whereas between 16% and 40% report physical abuse (Molnar, Shade, Kral, Booth, & Watters, 1998; Tyler & Cauce, 2002). Sullivan and Knutson (2000) found in their sample that neglect was not significantly associated with running away. Leaving home may be more related to a traumatogenic influence than it is a consequence of lack of supervision (Sullivan & Knutson, 2000).
Some evidence suggests that childhood abuse affects treatment outcome among runaways. Examining data from the Runaway/Homeless Youth Management Information System reveals that adolescents who used runaway shelter services nationwide in 1997, and who reported abuse by parents (N = 14,419), were less likely to reunify following a runaway episode (Thompson, Kost, & Pollio, 2003), although completing services through a runaway shelter increased the likelihood of the youth returning home. Kaliski, Rubinson, Lawrence, and Levy (1990) noted that the abused runaway adolescent’s focus on present survival outweighed major concerns for the future, thereby obstructing new behaviors fjrom being learned and practiced.
One gap in our knowledge of runaway and homeless youth is in the treatment realm. A search in the available databases (including Academic Search Premiere, Psychinfo, Medline, ERIC, Social Services Abstracts) indicates that comprehensive intervention for this group that addresses family issues, substance use, social stability, and physical and mental health issues has received little attention. Given the high risk for continuing health and social problems within this group, research focus on intervention efforts is considered to be an important endeavor.
Substance Abuse
Many studies note high levels of substance abuse among runaways and those with a history of childhood abuse. In fact, childhood abuse may be a factor in the development of substance abuse (Dembo et al., 1988). Both abused adolescents and adults in treatment for substance use report greater substance abuse problems than do nonabused individuals who are also in substance abuse treatment (Westermeyer, Wahmanhom, & Thuras, 2001). Compared to non-sexually abused peers, adolescents in treatment for substance abuse who reported prior sexual abuse also showed more severe substance use and an earlier onset of drug and alcohol use. Within an adult sample receiving substance abuse treatment, those reporting childhood physical abuse showed greater severity of substance use, a more morbid course of substance use problems, and more lifetime treatment in adulthood (Westermeyer et al., 2001). Given the potential role of childhood abuse on severity of substance use and its treatment, more research is needed to identify factors associated with treatment outcome in this group in order to better tailor and develop effective interventions.
Similarly, runaway youth report higher levels of substance abuse than do their nonrunaway peers (Koopman, Rosario, & Rotheram-Borus, 1994) with two studies reporting that nearly 70% of their sample of runaway youth met criteria of an alcohol or drug diagnosis (Baer, Ginzler, & Peterson, 2003; Kipke, Montgomery, Simon, & Iverson, 1997). Runaway youth and their families are characterized by high levels of family distress and family reunification is associated with greater adolescent adjustment and lower substance use (Van Leeuwen et al., 2004).
In a recent review of treatments for adolescent substance abuse problems, 15 studies met criteria for inclusion into the review (see Vaughn & Howard, 2004), thus, relatively few controlled trials on substance abuse treatment with adolescents have been conducted. Several literature reviews conclude that family therapy is an especially effective intervention for treating adolescent sub stance abuse when compared with non-family based interventions (Liddle, 2004; Ozechowski & Liddile, 2000). Recent clinical trials consistently report that more drug-abusing adolescents enter, engage in and remain in family therapy longer than in other modalities, and that family therapy produces significant reductions in pre- to posttreatment substance use (Latimer, Winters, D’Zurilla, & Nichols, 2003; Liddle et al, 2001; Santisteban, Perez-Vidal, Coatsworth, & Kurtines 2003; Waldron, Slesnick, Brody, Turner, & Peterson, 2001).
Our Study
In addition to providing preliminary support for treatment efforts with this population, the childhood abuse treatment outcome studies to date highlight the need for increased focus on adolescent treatment, which is especially salient given that more than one-third of childhood physical and sexual abuse cases involve adolescents (US Department of Health and Human Services, 1998). Also, CBT has been the dominant intervention utilized (Cohen, Deblinger, & Mannarino, 2004; Kolko, 1996), with only two studies examining FT (Kolko, 1996; Monck et al., 1994). Family therapy has received little attention in the treatment of adolescents with a history of physical and sexual abuse, even though much research points to the powerful role of the family on treatment outcome for adolescent problem behaviors (Liddle, 2004).
This study evaluated the relative contribution of individual and family factors expected to predict substance use at treatment outcome among abused runaway youth who received FT. Based on the literature reviewed, our expectations were as follows: (1) Abused (compared with nonabused runaway) youth would show more severe problems on variables considered to affect treatment outcome (individual and family problems) at baseline (Harrison, Fulkerson, & Beebe, 1997); (2) abused youth would show poorer substance use outcome than would nonabused youth (Westermeyer et al., 2001). Differences associated with change within and between the abused and nonabused groups were explored in order to identify predictors of substance use outcome for this specific group. Findings may then inform future intervention efforts as identification of specific targets for change can enhance the potential for positive treatment outcome.
METHOD
Overview
In this study we utilized data from two treatment outcome studies examining family therapy outcome with an alcohol-abusing sample (National Institute on Alcohol Abuse and Alcoholism [NIAAA] and Center for Substance Abuse Treatment [CSAT] grant R01 AA12173) and a drug-abusing sample (National Institute on Drug Abuse [NIDA] grant R29 DA 11590) of runaway adolescents. The design of these two studies was similar except for the fact that the alcohol-problem youth and families were assigned to one of two family therapy conditions (a home- vs. office-based approach), and the drug-abusing sample was assigned only to a home-based approach. Both studies included a treatment-as-usual condition through the local runaway shelter. For the purposes of this study, the two family therapy conditions in the alcohol study were collapsed and only data from those assigned to family therapy were examined, because individual and family change among those assigned to family therapy was the primary focus.
Abuse Definition
Keeping Children and Families Safe Act (National Clearinghouse on Child Abuse and Neglect Information, 2004) defines child physical abuse as physical injury (from minor bruises to severe fractures or death) as a result of punching, beating, kicking, biting, shaking, throwing, stabbing, choking, burning, or otherwise harming a child. Sexual abuse includes activities by a parent or caretaker, such as fondling a child’s genitals, penetration, incest, rape, sodomy, indecent exposure, and exploitation through prostitution or production of pornographic materials. This study used similar definitions, and abuse was self-reported by the adolescent. In reference to sexual abuse, youth were asked, “Has anyone ever touched you sexually in a way that made you feel uncomfortable OR hurt you OR was against your will?” and for physical abuse they were asked, “Has anyone ever hurt you physically—enough to leave marks or bruises or burns?”
Participants
Adolescents were recruited from two Southwestern runaway shelters. Inclusion criteria included: (1) between the ages of 12 and 17; (2) had the legal option of returning to a home situation (including foster or other family member); (3) adolescent met Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, 2000) criteria for a psychoactive substance use disorder; (4) family lived within 60 miles of the research site; and (5) at least one parent or surrogate parent was willing to participate in therapy. Adolescents were excluded if (1) there was evidence of unremitted psychosis or other condition that would impair his or her ability to consent for research participation, or (2) if current investigation of abuse or other condition (e.g., ward of the state) precluded the ability to conduct family therapy.
Sample Characterization
Participants included 242 adolescents recruited from two local runaway shelters. A total of 137 (57%) were female and 105 (43%) were male. The mean age at the time of intake was 14.99 (SD = 1.38 years). The average annual family income reported was $26,536 with a range of $0 to $190,000. Among the adolescents, 92 (41%) identified themselves as being Hispanic, 81 (34%) Anglo, 18 (7%) Native American, 15 (6%) African American, and 25 (12%) “Other” or mixed ethnicity. On average, adolescents first left home at 13.5 years (SD = 3.5 years) with a range of 10–17 years. A total of 151 (62%) reported having been arrested with an average of 2.60 (SD = 5.22) arrests. A majority of youth (154 [64%]) reported the experience of either physical or sexual abuse. Out of this subgroup a total of 31 (20%) had experienced both forms of abuse. The demographic details of abused and nonabused participants are listed in Table 1. In summary, more females, adolescents, abused adolescents reported more runaway episodes, having lived in a foster compared with males, reported a history of abuse. Compared with nonabused adolescents, abused adolescents reported more runway episodes, having lived in a foster or group home, and to have had a history of at least one suicide attempt, no differences were found for the other demographic characteristics. Please refer to Table 1 for demographic information on the abused and nonabused respondents in the two experimental groups. Again, a greater number of females reported childhood abuse in both the groups. No other significant differences were found.
Table 1.
Comparison of Demographics of Abused and Nonabused Respondents in the Experimental Groups
| Family therapy | Treatment as usual | |||
|---|---|---|---|---|
| Abused (n = 84) | Not abused (n = 57) | Abused (n = 70) | Not abused (n = 31) | |
| Gender N (%) | ||||
| Female | 54 (64.3%)* | 26 (45.6%)* | 46 (65.7%)** | 11 (35.5%)** |
| Male | 30 (35.7%)* | 31 (54.4%)* | 24 (34.3%)** | 20 (64.5%)** |
| Ethnicity N (%) | ||||
| Hispanic | 36 (43%) | 24 (42.1%) | 30 (42.9%) | 12 (38.7%) |
| Anglo | 28 (33.3%) | 17 (29.8%) | 25 (35.7%) | 11 (35.5%) |
| Native American | 18 (9.5%) | 6 (10.5%) | 3 (4.3%) | 1 (3.2%) |
| African American | 6 (7.1%) | 5 (8.8%) | 2 (2.9%) | 2 (6.5%) |
| Mixed ethnicity | 6 (7.1%) | 5 (8.8%) | 10 (14.3%) | 5 (15.1%) |
| Other Characteristics | ||||
| Currently enrolled in school N (%) | 45 (53.6%) | 33 (57.9%) | 32(45.7%) | 13 (41.9%) |
| Primary caretaker education level M (SD) | 12.3 (±3.6) | 12.9 (±3.9) | 13.1 (±3.4) | 12.2 (±3.2) |
| Annual family income M (SD) | $26,198 (±$25,550) | $29,656(±$38,831) | $27,341(±$28,983) | $19,642 (±$21,134) |
| Ever in foster home N (%) | 19 (22.6%) | 7 (12.3%) | 35 (50%) | 10 (32.3%) |
| Ever in group home N (%) | 24 (28.6%) | 10 (17.5%) | 34 (48.6%) | 11 (35.5%) |
| Ever in juvenile detention N (%) | 39 (46.4%) | 23 (40.4%) | 27 (38.6%) | 18 (58.1%) |
| Ever in jail overnight N (%) | 26 (31%) | 15 (26.3%) | 20 (28.6%) | 14 (45.2%) |
| Ever ward of state N (%) | 19 (22.6%) | 8 (14%) | 29 (41.4%) | 10 (32.3%) |
| Ever arrested N (%) | 53 (63.1%) | 32 (56.1%) | 43 (61.4%) | 23 (74.2%) |
| Number of times arrested M (SD) | 3.4 (±6.8) | 1.5 (±1.9) | 2.9 (±5.8) | 1.8 (±1.8) |
| Number of times runaway M (SD) | 4.0 (±5.3) | 2.7 (±2.9) | 5.6 (±11.3) | 5.9 (±17.71) |
| Ever attempted suicide | 36 (42.9%) | 15 (26.3%) | 31 (44.3%) | 9 (29.0%) |
| Percent Days of Substance Use in the Last 90 Days M (SD) | ||||
| Drugs | 40.96 (±35.3) | 43.19 (±33.9) | 39.41 (±34.2) | 49.17 (34.3) |
| Alcohol | 15.8 (±19.7) | 16.8 (±23.9) | 11.1 (±12.5) | 18.19 (±24.3) |
| Drugs and alcohol | 47.1(±32.7) | 48.4 (±32.5) | 44.3 (±31.9) | 54.77 (±32.6) |
p < 0.05.
p < 0.01.
Procedure and Treatment
A project research assistant approached adolescents in the shelter to determine initial eligibility and interest in the project. If the adolescent was eligible and assented to have their parents contacted and to participate in the study, the parent was contacted. Upon parental consent, the youth’s assessment was then conducted, and the youth and family were randomly assigned to FT or treatment as usual (TAU). The interviewer then proceeded to administer the Computerized Diagnostic Interview Schedule for Children (CDISC; Shaffer, 1992) sections on drugs, alcohol, and psychosis to determine formal eligibility of the adolescent. Those who did not pass quick-screen or meet the inclusion criteria during the formal screening were excluded from the study. Those meeting the criteria for participation in the study continued with the assessment battery.
Participants were told that the assessment would take up to 3 hours and that they would receive $25 at the completion of the assessment. Following completion of the assessment battery, 141 youths were randomly assigned to FT and 101 to TAU through the shelter. All clients were followed at 3, 9, and 15 months postintake and were paid $50 for each follow-up assessment. Most follow-up assessments were conducted in the youth’s home; otherwise, youths were transported to the research site for their appointment by the project research assistant. The follow-up rates for those assigned to family therapy were as follows: 124/141 (88%) at 3 months postintake, 116/141 (82%) at 9 months postintake, and 115/141 (81%) at 15 months postintake. The follow-up rates for TAU were: 79/101 (78%) at 3 months, 82/101 (81%) at 6 months, and 83/101 (82%) at 15 months.
Therapist training and supervision
Therapists received readings including the treatment manuals, a 2-day didactic training, which included roleplay exercises, and received intensive, ongoing supervision through audiotape session review by the principal investigator. To equate groups on therapist characteristics, each therapist was trained to provide both the home- and office-based treatment. Several therapists conducted the family therapy, but four therapists conducted therapy with the majority of the youth (84%). Therapists included three females and one male. Therapist ethnicities included Anglo (n = 3) and Hispanic (n = 1). All therapists were master’s-level, licensed counselors with between 2 and 5 years’ experience in the field. Therapist differences were investigated. The number of completed treatment sessions differed significantly (F = 3.3; p < 0.05). However, no overall interactions between therapist and time were found for substance use (all/p >.10; using repeated-measures analysis of variance).
Audiotape recordings of all therapy sessions were used for treatment adherence checks by the supervisor and for use in supervision meetings. The therapists and supervisor met weekly, and during these meetings selected portions of audiotapes were reviewed, feedback was provided, and problems were discussed. The supervisor ensured that the core elements of systemic family therapy were being utilized by the therapists, especially relational statements, reframes and roleplays and the avoidance of blame on individuals.
Family therapy
In this project, two manualized, ecologically focused, family systems-based therapies were offered; one provided in the office (Alexander & Parsons, 1982) and one in the home (Slesnick & Prestopnik, 2005). These two treatment models are similar in focus, though different in context (home vs. office). For example, the goal of each treatment was to alter dysfunctional family patterns that contribute to substance abuse, running away, and related individual problem behaviors. Another goal was for youth and parents to become more confident and competent in their ability to communicate needs and expectations. Families were guided from an intrapersonal to interpersonal interpretation of problems utilizing interpretations, questions, and reframes that have relational bases. The interventions were nonconfrontational, and the therapist set a nonhostile, nonjudgmental tone for sessions. Other intervention strategies included cognitive-behavioral techniques, which were utilized to interrupt problem behavior patterns so that new skills could be taught, practiced, and applied outside the therapy context. In addition to communication and parenting skills training, ecologically focused family therapy includes a wide range of behavioral, cognitive, and environmental interventions (such as meetings with teachers and probation officers), depending on the family’s needs. Both treatment interventions focused specifically on reducing runaway behavior. Most session time focused on reducing negative, and increasing positive, attributions and expectations among family members, as well as improving communication and problem-solving skills. Intensity of focus on substance abuse depended on the adolescent’s comfort with the topic. Up to 16 family sessions were offered, and sessions averaged 60 minutes.
Treatment as usual
Those adolescents who were randomly assigned to TAU received services that the shelter normally provided. These services included talking with counselors on staff, crisis intervention, and assistance with placement. On average, youth stayed at the shelter 9 days (SD = 15) at pretreatment and 15 days (SD = 22) at the first follow-up. At the first follow-up, youth in TAU reported receiving an average of 3 (SD = 5.5) outside therapy sessions, whereas those in FT reported 1.7 (SD = 5.2) outside therapy sessions, which did not differ between groups, F(1, 202) = 2.65, p > 0.05.
Measures
Three domains of interest were assessed: family functioning, substance use, and individual problem behaviors. The assessment included both clinician assisted and self-report questionnaires. Those youth having difficulty completing the self-report questionnaires were offered assistance from the interviewer, and they were given the option of completing the assessment in one sitting or in two shorter sessions on separate days.
Diagnostic status
Shaffer’s (1992) CDISC is a computerized instrument developed specifically to diagnose children and adolescents based on DSM-IV criteria. It has demonstrated excellent interrater reliability of 97% with clinicians agreeing with the diagnosis of CDISC (Wolfe, Toro, & McCaskill, 1999). The interview was administered to youths by the research assistant.
Demographic measures
A demographic questionnaire designed to characterize and compare participants was administered. Measures included age, gender, self-identified ethnicity, information about parents and siblings, self-reported physical and sexual abuse, number of runaway episodes, economic information, education level, grade point average, suicidality, and arrest history.
Family measures
The Conflict Tactic Scale (CTS; Straus, 1979) was implemented to measure the occurrence of several methods of conflict resolution used by the youth and primary caretaker. Three subscales were used (reasoning, verbal aggression, and physical violence), with each subscale separately scored to understand the methods used in conflict resolution. The measure has shown good internal consistency with Cronbach’s alpha of.83 (Yoder, 1999) in a clinical sample. The reliability coefficient for this sample ranged from 0.76 to 0.83.
The Parental Bonding Instrument (PBI; Parker, Tupling, & Brown, 1979) consists of 25 items designed to measure youths’ perceived attitudes of parental bonding and overprotection during the period of time in which the youth lived in the home. Reliability and validity have been established in both clinical and nonclinical samples (Klimidis, Minas, & Ata, 1992; Parker, 1983). Cronbach’s alpha for this sample ranged from 0.79 to 0.89.
The Family Environment Scale (FES; Moos & Moos, 1986) is comprised of 90 true-false items and consists of 10 subscales, which measure social-environmental characteristics of families (Cohesion, Expressivity, Conflict, Independence, Achievement-Orientation, Cultural-Religious Emphasis, Organization, and Control). Internal consistencies have ranged from.61 to.78 and test-retest reliabilities from.73 to.86. Conflict and Cohesion subscales were used to assess family disturbance as these two areas of functioning have been shown to predict negative communication exchanges in delinquent families (Mas, 1986). The reliability coefficient for this sample was 0.77 for the cohesion subscale and 0.66 for the conflict subscale.
Substance use
The Form 90, developed for NIAAA-funded Project Match (Miller & Del Boca, 1994), was the primary measure of quantity and frequency of drug and alcohol use. This measure uses a combination of the timeline follow-back method (Sobell & Sobell, 1992) and grid averaging (Miller & Marlatt, 1984). This tool has shown excellent test-retest reliability for indices of drug use in major categories (Tonigan, Miller, & Brown, 1997; Westerberg, Miller, & Tonigan, 1999), including with runaway, substance-abusing adolescents (Slesnick & Tonigan, 2004) with kappas for different drug classes ranging from.74 to.95. Percent days of alcohol and drug use (in the prior 90 days) was the primary dependent measure used in this study. To address problem consequences associated with drug use, the Problem Oriented Screening Instrument for Teenagers (POSIT, Rahdert, 1991) was utilized. Support for the psychometric properties of the POSIT, including convergent and discriminant validity, have been reported by McLaney, DelBoca, and Babor (1994). The reliability coefficient for this sample was 0.85.
Individual problem behaviors
The National Youth Survey Delinquency Scale (NYSDS; Elliott & Huizinga, 1983) is a structured interview used as a measure of delinquent behavior. It includes five subscales: General theft, crimes against persons, index offenses, drug sales and total delinquency. The NYSDS is a structured interview that has displayed adequate test-retest and criterion validity (Elliott & Huizinga, 1983). Cronbach’s alpha for this sample was 0.65.
The Youth Self-Report (YSR) is the parallel instrument for the parent-reported Child Behavior Checklist (CBCL; Achenbach & Edelbrock, 1982). The YSR is a 120-item, self-report questionnaire that provides factor scores for internalizing, externalizing, as well as total behavior problems. The measure is highly reliable and effectively discriminates between children referred to clinics for problem behavior and nonclinic children. The reliability coefficients for this sample ranged from 0.62 to 0.88.
RESULTS
Data Analysis Strategy
There were at least two areas of interest in this data. First, comparing the baseline means on the variables hypothesized to affect outcomes for those who were abused and those who were not was of interest. Second, evaluation of whether different outcomes on substance abuse were found among those who were abused compared with those who were not was conducted.
To investigate differences at baseline among those who reported either physical or sexual abuse, those who reported both, and those who reported no abuse, a multivariate analysis of variance (MANOVA) was performed to estimate the significance of differences in the means among these three groups on the different factors: treatment factors (number of other diagnoses), family factors (bonding, violence, cohesion and conflict), and individual factors (depression, consequences of substance use, delinquency, internalizing and externalizing behaviors). We also wanted to make sure that the TAU group did not exhibit baseline differences from the FT-treated group even though the assignment was randomized. Given the number of variables and their likely correlation, a MANOVA was selected. The main effect for abuse was significant in the multivariate tests (Wilks Lambda =.75; F[28, 428] = 2.31; p < 001). There was also a main effect for treatment group (Wilks Lambda =.86; F[14, 214] = 2.3; p <.001). In the tests for between-subjects effects the following contributed to the overall main effect for abuse: FES conflict and cohesion, internalizing; CTS violence by the parent to the adolescent and by the adolescent to the parent; bonding, depression, and other diagnoses. In the tests for between-subjects effects for the treatment groups, only the delinquency total score contributed to the overall main effect.
In post hoc Scheffe procedures, several variables showed significant differences among the abuse groups. For FES conflict, those who experienced both types of abuse had significantly higher conflict scores than those who experienced no abuse. Those who experienced no abuse had significantly higher scores on FES cohesion than those who experienced either kind of abuse and those who experienced both types of abuse. Those who experienced only one kind of abuse had significantly higher cohesion scores than those who experienced both types of abuse. The only two variables that did not show significant differences among the three abuse groups were bonding overprotection, and consequences of substance use. These differences are noted in Table 2.
Table 2.
Means and Standard Deviations of the Treatment Variables for Those Who Did Not Report Abuse (n = 76), Those Who Reported Either Type of Abuse (n = 88) and Those Who Reported Both Types of Abuse (n = 39) in the Family-Therapy-Treated Group (n = 119) and Treatment-as-Usual Group (n = 84)*.
| Family-therapy treated group | Treatment-as-usual group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No abuse | Either type | Both types | No abuse | Either type | Both types | |||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Treatment factors | ||||||||||||
| Number of drugs | .48 | .74 | .54 | .61 | .47 | .51 | .51 | .50 | .40 | .49 | .50 | .61 |
| Number of diagnoses | .87 | 1.26 | 1.11 | 1.51 | 1.61 | 1.53 | 1.06 | 1.13 | .64 | 1.05 | 2.47 | 2.34a |
| Consequences | 5.87 | 3.64 | 5.90 | 4.06 | 6.47 | 5.11 | 5.55 | 3.73 | 5.21 | 3.81 | 8.27 | 4.49 |
| Number of sessions | 9.52 | 6.12 | 8.59 | 6.4 | 8.30 | 6.94 | na | na | na | |||
| Individual factors | ||||||||||||
| Delinquency | 82.17 | 167.80 | 197.27 | 291.66 | 130.50 | 175.50 | 369.80 | 578.90 | 539.70 | 782.10 | 606.6 | 732.90b,d |
| Externalizing | 27.19 | 10.79 | 27.82 | 9.86 | 28.38 | 10.61 | 26.37 | 7.87 | 23.73 | 10.65 | 31.05 | 13.09 |
| Internalizing | 17.53 | 9.49 | 19.78 | 10.64 | 19.38 | 8.64 | 18.82 | 11.03 | 15.27 | 10.05 | 26.11 | 12.58a |
| Family factors | ||||||||||||
| Bonding care | 23.78 | 6.18 | 20.66 | 8.27 | 14.85 | 9.52 | 21.58 | 8.71 | 21.83 | 9.42 | 15.77 | 8.75a |
| Bonding overprotection | 21.02 | 7.52 | 19.05 | 10.29 | 20.28 | 8.27 | 15.17 | 8.05 | 17.54 | 8.41 | 21.88 | 10.59 |
| Aggression youth | .39 | .20 | .47 | .24 | .50 | .21 | .31 | .23 | .35 | .23 | .48 | .28b |
| Aggression parent | .31 | .23 | .40 | .24 | .49 | .20 | .32 | .27 | .30 | .23 | .40 | .30b |
| Violence youth | .06 | .07 | .09 | .08 | .10 | .13 | .06 | .10 | .06 | .07 | .13 | .13a |
| Violence parent | .06 | .09 | .15 | .12 | .18 | .17 | .06 | .10 | .09 | .13 | .17 | .14c |
| Cohesion | 4.91 | 2.35 | 3.58 | 2.3 | 3.71 | 2.49 | 4.65 | 2.63 | 4.81 | 2.64 | 3.55 | 2.70c |
| Conflict | 4.89 | 2.00 | 5.90 | 2.50 | 5.76 | 2.75 | 4.96 | 2.27 | 5.00 | 2.66 | 5.94 | 2.73b |
Listwise deletion for missing data;
Both-Types group different than the other two groups (p < 05);
Both-Types group different than the No-Abuse group (p < .05);
No-Abuse group different than the other two groups (p < .05);
Family-Treatment group different than the Treatment-as-Usual group (p < .05).
na = not applicable.
In summary, those adolescents who reported abuse did appear to have different means on some of the variables that were hypothesized to affect treatment outcomes. The next step was to assess whether those who reported abuse and those who did not showed differences in outcomes compared with those in treatment and those in the TAU group. To assess these differences hierarchical linear modeling (HLM, Raudenbush & Bryk, 2002) with the HLM 5 software (Raudenbush, Bryk, Cheong, & Congdon, 2002) was used to estimate the model for change in substance use over the course of treatment and follow-up. Hierarchical linear modeling allows the researcher to take into account the “nesting” of the data. In this instance we have substance abuse measures at baseline, 3 months, 9 months and 15 months postbaseline. These across-time data is nested in individuals (each individual contributes 4 data points). Hierarchical linear modeling allows for the possibility that baseline substance abuse is different for each individual and that change in substance abuse across time may also be different. Other analyses only provide central tendencies (i.e., means) for the baseline and the change. Thus, Level 1 for this model was substance use for all individuals in the sample at each of the four time points. Level 2 variables included the presence or absence of abuse, treatment group, and all the predictor factors (treatment, family, individual) that were hypothesized to affect the outcomes of treatment. To test the impact of family variables on treatment outcome we entered this set of variables last so that the other variables believed to affect treatment outcomes would be tested and thus controlled for in previous steps. Thus, the final step in creating a model to predict the baseline level of substance abuse and the change in substance abuse was the addition of the family variables.
The first step in an HLM analysis is to estimate an unconditional model, in this case this is a model that allows the baseline of substance use to vary between and among individuals without including time. This is the unconditional model presented in Table 3. The coefficient for substance use in this model is 34.06, which can be interpreted as the average percent days of substance use (within the prior 90 days) across all subjects and all time points. This value was significantly different than zero (t = 20.34; p <.001) and there was significant variability in the baseline scores between subjects, χ2(232) = 906.27, p <.001. From this model, the intraclass correlation can also be calculated (Luke, 2004). The intraclass correlation allows the researcher to gauge how much of the variability lies at level 2, which in this case is the individual. Thus, about 42% of the variability in substance use over all time points is between the individuals in the sample. If this percentage were low, it would not make sense to continue the analysis. Given that this number is fairly substantial, it suggests that there may be predictors of this variability, and this may lead to areas for intervention.
Table 3.
Hierarchical Linear Modeling Analysis results: Parameter Estimates and Model Fit for Substance Use Over Time for Family-Therapy-Treatment Group, Treatment-as-Usual Group and Abused versus Not Abused
| Unconditional
|
Model 1
|
Model 2
|
||||
|---|---|---|---|---|---|---|
| Fixed effects | Coef. | t-value | Coef. | t-value | Coef. | t-value |
| Intercept | 34.06 | 20.34*** | 50.79 | 19.90*** | 51.12 | 9.55*** |
| Treatment group | 3.99 | ns | ||||
| Abuse group 1 | −4.68 | ns | ||||
| Abuse group 2 | −3.06 | ns | ||||
| Slope (time) | −6.68 | −8.12*** | −5.42 | −2.96** | ||
| Treatment group | −3.73 | −2.21* | ||||
| Abuse group 1 | 1.50 | ns | ||||
| Abuse group 2 | 1.15 | ns | ||||
|
| ||||||
| Random effects | Variance Component | χ2 | Variance Component | χ2 | Variance Component | χ2 |
|
| ||||||
| Intercept | 488.08 | 906.27*** | 772.28 | 470.49*** | 783.30 | 467.76*** |
| Slope | 58.47 | 367.43*** | 56.52 | 357.98*** | ||
| Level 1 | 671.75 | 500.84 | 500.84 | |||
ns = not significant
p < .05.
p < .01.
p < .001.
The next step in the HLM analysis was to add a predictor for variation in substance use at level 1. In this instance, the model estimates the effect of time on substance use. This is labeled as Model 1 in Table 3. The intercept in this model was 50.79 (t = 19.90; p <.001) and can be interpreted as the average baseline percent days of substance use in this sample. The coefficient for the slope or change over time was −6.68 (t = −8.12; p <.001) suggesting that on average substance use decreased over time. There was significant variability in the slopes among the individuals, and time accounted for about 25% of the variance in substance use. These models at level 1 suggest that on average substance abuse decreased over time, but there was variability in that change, and the baseline values were also variable. This suggests that not only do we need to understand what variables affect treatment on average, but also what may affect treatment at the individual variability level. In other words, we need to understand why some of these adolescents changed and how much they changed as well as why some of these adolescents did not change or change as much.
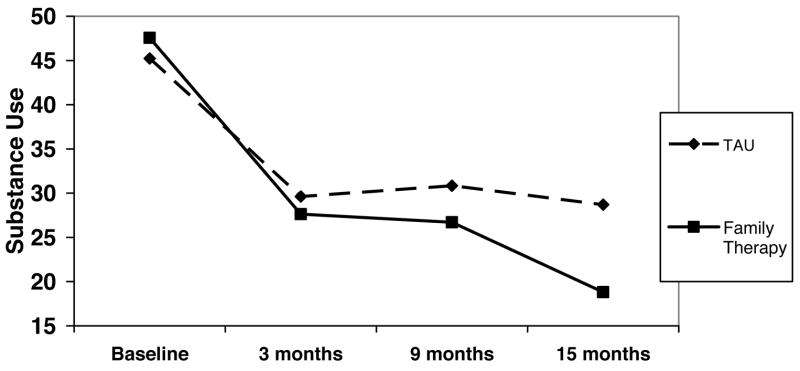
The next step was to assess whether the FT group or the control group (TAU) differed in terms of their baseline on substance abuse or their change in substance abuse over time (Model 2 in Table 3). There were no differences at baseline, but there was a significant difference in change in substance abuse for the treatment versus the control group (t = −2.21; p <.05). Treatment or control group explained about 5% of the variability in change in substance abuse over time. Although both groups showed a decrease in substance abuse, the group that received family therapy showed more of a decrease in substance abuse (see Figure 1). Given this, the two groups were separated to determine what might account for some of the change in substance use for those abused and those not abused.
Figure 1.
Change in substance use between Treatment-as-Usual group and Family-Therapy-Treatment group.
Family Therapy Treatment Group
The HLM 5 software (Raudenbush et al, 2002) provides an exploratory analysis option to test for potentially significant predictor variables. Given the number of potential variables at level 2, it was decided to use this exploratory function for predicting the baselines and then the changes in percent days of use. Each group of predictor variables was entered to see which variables had potential and which did not. The first group was considered the treatment factor group; it included number of sessions, number of other diagnoses at baseline, number of drugs used, and consequences of drug use. The only variables that were potentially significant within this group were number of drugs used at baseline and consequences of drug use. The second factor included individual variables (internalizing and externalizing, and delinquency). None of these variables were potentially significant in explaining the baseline of substance use. The same was true for the abuse factor (either physical or sexual, both or none reported) or the family factor (violence, conflict, cohesion, and bonding). That is, none of the variables hypothesized to affect treatment outcome, other than number of drugs used and consequences of drug use, was significant in predicting percent days of substance use at baseline. Thus, the final model for the baseline (Model 2 in Table 4) included number of drugs used (t = 4.7; p <.001) and consequence of drug use (t = 3.45; p <.01). These two variables accounted for about 48% of the variability in percent days of use at baseline.
Table 4.
Hierarchical Linear Modeling Analysis Results: Parameter Estimates and Model Fit for Substance Use Over Time for Family-Therapy-Treatment Group
| Unconditional
|
Model 1
|
Model 2
|
Model 3
|
|||||
|---|---|---|---|---|---|---|---|---|
| Fixed effects | Coef. | t-value | Coef. | t-value | Coef. | t-value | Coef. | t-value |
| Intercept | 32.15 | 14.06*** | 51.68 | 14.23*** | 51.68 | 16.54*** | 51.68 | 17.01*** |
| Treatment factors | ||||||||
| Consequences | 1.57 | 3.45** | 1.75 | 3.63** | ||||
| Number of drugs | 17.88 | 4.70*** | 29.81 | 5.77*** | ||||
| Abuse | ns | |||||||
| Individual factors | ns | |||||||
| Family factors | ns | |||||||
| Slope (time) | −7.81 | −7.36*** | −7.81 | −7.36*** | −7.81 | −7.82*** | ||
| Treatment factors | ||||||||
| Number of diagnoses | −.91 | −2.13* | ||||||
| Number of drugs | −5.2 | −3.73*** | ||||||
| Abuse | ns | |||||||
| Individual factors | ns | |||||||
| Family factors | ||||||||
| Cohesion | −.70 | −2.74** | ||||||
|
| ||||||||
| Random effects | Variance Compone nt | χ2 | Variance Component | χ2 | Variance Component | χ2 | Variance Component | χ2 |
|
| ||||||||
| Intercept | 455.56 | 443.60*** | 826.73 | 247.60*** | 430.08 | 83.33*** | 372.38 | 173.25*** |
| Slope | 35.75 | 158.68** | 35.82 | 158.70** | 21.96 | 140.32* | ||
| Level 1 | 645.22 | 485.81 | 485.76 | 486.2 | ||||
ns = not significant
p <.05.
p <.01.
p <.001.
With these variables included for the intercept, the next step was to determine which of the variables of interest had potential for explaining variability in the change in substance use due to treatment. For the treatment factor, number of drugs and number of diagnoses other than substance abuse or dependence had significant potential to sexplain variability in the change in substance use over time. The individual factors including reports of abuse were not significant. The only other variable that was a potentially significant predictor of the change in substance use was family cohesion. These three variables were included in Model 3 in Table 4. Family cohesion (t = −2.74; p <.01), number of diagnoses other than substance-related ones at time 1 (t = −2.13; p <.05), and number of drugs used at baseline (t = −3.73; p <.001) were all significant predictors of change in substance use due to treatment and at follow-up. These three variables accounted for about 39% of the variability in change in substance use across time between the individuals in the sample. With each step in this model-building procedure deviance decreased, which suggests an increase in fit. Graphic depictions of the relationships among cohesion, number of drugs used, and change in substance use across time can be seen in Figure 2 (to create the groups for number of drugs used and cohesion, a mean split was used).
Figure 2.
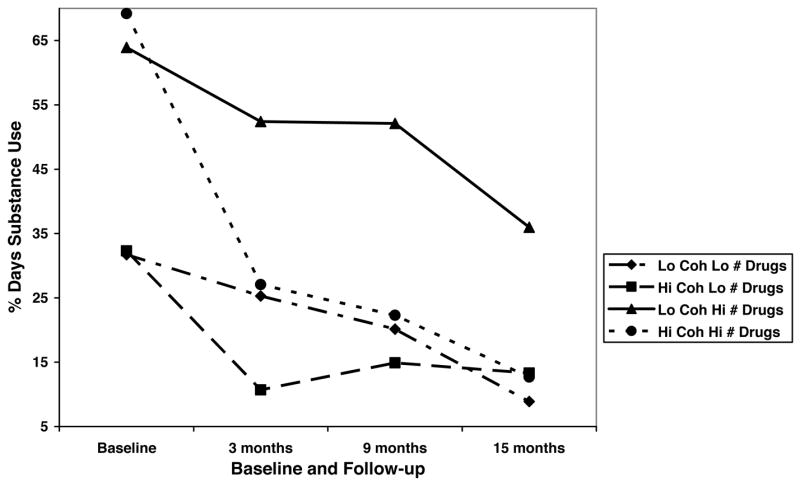
Number of drugs and cohesion in relation to substance use over time for Family-Therapy-Treatment group.
Given the findings from the HLM analyses, several questions remain, one of which is whether change in cohesion varies with change in substance use over the course of treatment and follow-up and whether this covariation is different for those who report abuse and those who do not.
Another HLM analysis was performed, but cohesion became the “dependent” measure. To capture whether change in substance use covaried with change in cohesion a reliability of change index (RCI) was created for substance use subtracting time-4 substance use from time-1 substance use, then dividing this by the standard error of the difference (Jacobson, Follette, & Ravensdorf, 1984). An RCI of 1.96 or greater suggests a reliable change. In this instance a positive number indicates decrease in substance use, and a negative number indicates increase in substance use over time.
In the HLM analysis, cohesion at the four time points was used at level 1, whereas the abuse variable and change in substance use variable were used at level 2. The unconditional model indicated that the overall average for cohesion between individuals and across the four time points was 5.1 (t = 24.8; p <.001). The results of these model tests are reported in Table 5. The intraclass correlation suggested that individual accounted for about 48% of the variability in cohesion across time. In the model in which time is entered to account for change in cohesion, the coefficient for cohesion was 4.33 (t = 18.01; p <.001), which can be interpreted as the baseline level of cohesion across individuals. The coefficient for the slope was.51 ( t= 5.45; p <.001), which suggests that cohesion increased over time. The variability in baseline scores and change over time were also significant in this model. Time accounted for about 31% of the variability in cohesion.
Table 5.
Hierarchical Linear Modeling Analysis Results: Parameter Estimates and Model Fit for Cohesion Over Time for Family-Therapy-Treatment Group
| Unconditional
|
Model 1
|
Model 2
|
Model 3
|
|||||
|---|---|---|---|---|---|---|---|---|
| Fixed effects | Coef. | t-value | Coef. | t-value | Coef. | t-value | Coef. | t-value |
| Intercept | 5.1 | 24.92*** | 4.33 | 18.01*** | 5.0 | 18.02*** | 5.0 | 17.92*** |
| Abuse1 | −1.2 | −3.04** | −1.2 | −3.04** | ||||
| Abuse2 | −1.18 | −1.91 | −1.18 | −1.91 | ||||
| Change in use | .04 | 3.08** | .02 | 1.14 | ||||
| Slope (Time) | .51 | 5.45*** | .51 | 5.45*** | .51 | 5.58*** | ||
| Abusel | ns | |||||||
| Abuse2 | ns | |||||||
| Change in use | .018 | 2.10* | ||||||
|
| ||||||||
| Random effects | Variance Component | χ2 | Variance Component | χ2 | Variance Component | χ2 | Variance Component | χ2 |
|
| ||||||||
| Intercept | 3.31 | 468.56*** | 4.10 | 337.07*** | 3.59 | 300.98*** | 3.53 | 296.60*** |
| Slope | .41 | 180.91*** | .40 | 180.93*** | .37 | 172.91 | ||
| Level 1 | 3.50 | 2.40 | 2.40 | 2.40 | ||||
ns = not significant
p < .05.
p < .01.
p < .001.
In the next step, the two abuse variables were entered. We dummy coded the abuse variable as: 1, 0 for physical abuse; 0, 1 for sexual abuse; 1, 1 for both types of abuse; and 0, 0 for neither type of abuse. The change in substance use score was also used at level 2 to explain the variability in cohesion at baseline. The first abuse variable (which was coded 1 for either type of abuse and 0 for no abuse) was a significant predictor of the variability in cohesion (−1.20; t = −3.04; p <.01). The change in substance use score was also predictive of the variability in the intercept (.049; t = 2.74; p <.01). These variables explained 12% of the variability in baseline scores. This would suggest that change in substance use covaried with the baseline level of cohesion, but that the intercept in cohesion was also different for those who reported either type of abuse than for those who did not report abuse. The finding that change in substance abuse covaried with the variability in baseline suggests that the baseline level of cohesion matters for change in substance abuse. The coefficient was negative, suggesting that lower levels of cohesion at baseline were associated with greater decreases in substance abuse. In other words, those with lower levels of cohesion may have responded more to treatment than did those with higher levels of cohesion.
Finally, the intercepts and slopes as outcomes model were tested, using the abuse and change in substance use variables to explain both the intercepts and the slopes of cohesion scores. Only the change in substance use variable (.018; t = 2.1; p < 05) was significantly predictive of the changes in cohesion scores, not the abuse variables. This suggests that change in cohesion and change in substance abuse covary. The coefficient is positive, which suggests that as cohesion increased, substance abuse decreased. These variables accounted for about 7.5% of the variability in the change of cohesion. The relationships among abuse, change in substance use, and cohesion across time are graphically depicted in Figure 3.
Figure 3.
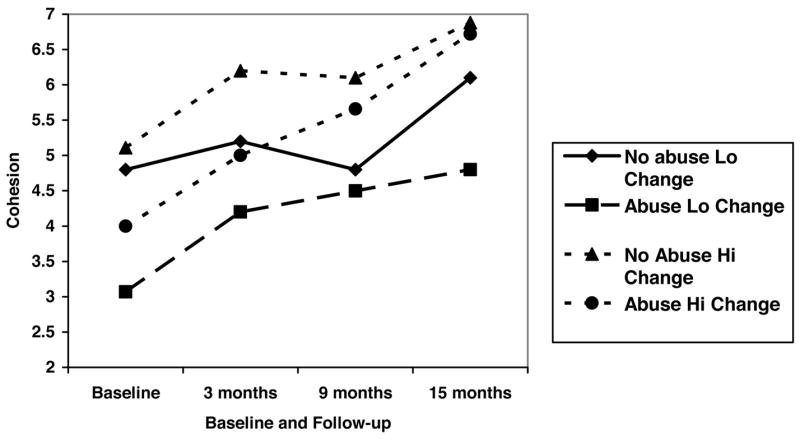
Reports of either type of abuse or none, change in substance use and change in cohesion over time for Family-Therapy-Treatment group only.
Control Group: Treatment as Usual
Using the results from the treated group, we tested the same set of models with the treatment as usual group. It should be noted that the HLM program used 99 participants’ data for the treated group and 99 participants’ data for the control group models. The results of these model tests are reported in Tables 6 and 7. The coefficient for drug use in the unconditional model was 37.12 for the TAU group, and there was significant variability in the baseline scores, χ2(98) = 388.10, p <.001. When time was added to the level-1 model, the coefficient for substance use was 48.33 (t = 12.48; p <.001), and the slope or change in substance use over time was −4.48 (t = −3.28; p <.001). There was significant variability in slopes as well, χ2(98) = 169.66, p <.001 As in the models that explained variability in baseline scores and changes in percent days of use in the treatment group, only the number of drugs used explained variability in baseline scores on substance abuse for the TAU group (t = 4.62; p <.001), but not the consequences due to drug use. In the final intercepts and slopes as outcomes model (Model 3 in Table 6), only number of drugs used at baseline significantly predicted both intercept and change in substance use; cohesion did not explain any of the variability in change in substance use in the TAU group. In the model that explored the covariation of change in cohesion and change in substance abuse for the TAU group (Table 7), cohesion scores significantly changed over time, but that change was not predicted by change in substance use.
Table 6.
Hierarchical Linear Modeling Analysis Results: Parameter Estimates and Model Fit for Substance Use Over Time for Treatment-as-Usual Group
| Unconditional
|
Model 1
|
Model 2
|
Model 3
|
|||||
|---|---|---|---|---|---|---|---|---|
| Fixed effects | Coef. | t-value | Coef. | t-value | Coef. | t-value | Coef. | t-value |
| Intercept | 37.12 | 14.11*** | 48.33 | 12.48*** | 48.98 | 13.77*** | 48.98 | 14.32*** |
| Treatment factors | ||||||||
| Consequences | .23 | ns | .20 | ns | ||||
| Number of drug | 24.05 | 5.23*** | 38.50 | 5.51*** | ||||
| Slope (time) | −4.48 | −3.38*** | −4.93 | −3.35*** | −4.93 | −3.56*** | ||
| Treatment factors | ||||||||
| Number of diagnoses | −.05 | ns | ||||||
| Number of drugs | −8.22 | −3.14** | ||||||
| Family factors | ||||||||
| Cohesion | −.20 | ns | ||||||
|
| ||||||||
| Random effects | Variance Component | χ2 | Variance Component | χ2 | Variance Component | χ2 | Variance Component | χ2 |
|
| ||||||||
| Intercept | 517.22 | 388.10*** | 692.84 | 182.21*** | 224.40 | 104.21** | 178.62 | 98.69 |
| Slope | 78.61 | 169.66** | 69.61 | 134.80** | 55.72 | 121.31** | ||
| Level 1 | 698.89 | 537.53 | 558.26 | 557.46 | ||||
ns = not significant
p < .05.
p < .01.
p < .001.
Table 7.
Hierarchical Linear Modeling Analysis Results: Parameter Estimates and Model Fit for Cohesion Over Time for Treatment-as-Usual Group
| Unconditional
|
Model 1
|
Model 2
|
||||
|---|---|---|---|---|---|---|
| Fixed effects | Coef. | t-value | Coef. | t-value | Coef. | t-value |
| Intercept | 5.2 | 23.63*** | 4.30 | 15.88*** | 4.43 | 8.85*** |
| Abuse1 | .04 | ns | ||||
| Abuse2 | −.54 | ns | ||||
| Change in use | .02 | ns | ||||
| Slope (time) | .60 | 5.46*** | .60 | 3.29*** | ||
| Abuse 1 | −.08 | ns | ||||
| Abuse2 | .13 | ns | ||||
| Change in use | .02 | ns | ||||
|
| ||||||
| Random effects | Variance Component | χ2 | Variance Component | χ2 | Variance Component | χ2 |
|
| ||||||
| Intercept | 2.54 | 251.88*** | 3.32 | 187.65*** | 3.46 | 184.17*** |
| Slope | .30 | 108.85** | .30 | 103.27** | ||
| Level 1 | 3.99 | 2.89 | 2.89 | |||
ns = not significant
p <.05.
p <.01.
p <.001.
In addition, we investigated whether change in cohesion scores were different for the TAU and FT-treated groups. The slopes were virtually identical. However, it should be noted that, change in cohesion was related to change in substance use in the family therapy treated group but not in the TAU group. So, although family cohesion scores changed for the better in both groups, that change was only related to better outcomes in the FT- treated group.
DISCUSSION
Researchers report that abused youth, compared with nonabused, have more severe substance use problems (Harrison et al., 1997) and respond more poorly to substance abuse treatment (Westermeyer et al., 2001). Yet, to date, few formal treatment evaluation studies have been conducted to address substance abuse and related problems among this group, and some have called for more evaluation of family involved interventions (Pelcovitz et al., 2000; Swenson & Spratt, 1999). This study evaluated family therapy outcome for substance using runaway youth, a majority of whom reported physical and/or sexual abuse.
Our first hypothesis, that abused compared with nonabused youth would show more severe individual and family problems at baseline, was partially supported. Abused adolescents, compared with nonabused, reported lower cohesion, less parental care and more severe conflict resolution tactics that involved violence from parents. Thus, even among a sample of runaway youth with relatively severe family situations, abused adolescents reported even less parent care and family cohesion than did nonabused adolescents. This finding is consistent with a large body of research on child physical and sexual abuse (e.g., Finkelhor & Berliner, 1995). For example, Pelcovitz et al. (2000) examined 99 abused and 99 nonabused adolescents to determine the relationship between family functioning and physical abuse. Abused adolescents perceived their families as less adaptable, cohesive, and balanced compared with nonabused adolescents. Both fathers and mothers were viewed as less caring.
However, abused adolescents did not show significantly different levels of substance use at pretreatment from nonabused adolescents. Regardless of abuse status, the only significant predictors of substance abuse at baseline were number of different drugs used and drug use consequences. This finding is contrary to earlier research reporting higher substance use among adolescent physical and sexual abuse victims (Harrison et al., 1997). One possibility for the difference is that those youth who might not otherwise seek substance abuse treatment services were engaged into treatment while at a runaway shelter and may have different substance use patterns than those found in other treatment samples. Moreover, runaway youth in general show significantly higher rates of substance use and problems than do nonrunaway youth (Forst & Crim, 1994). In fact, Beitchman, Zucker, Hood, DaCosta, and Akman (1991) and Kendall-Tackett et al. (1993) conclude that differences in symptoms between abused and nonabused groups are often not found in clinical samples.
The second hypothesis, that abused compared with nonabused adolescents would show poorer substance use outcome, was not supported. Pretreatment level of cohesion, along with number of different drugs used and drug use consequences, predicted change in substance use, but abuse status did not. However, this finding suggests that change in substance use can be more limited for those adolescents who report lower family cohesion and a higher number of different drugs used at pretreatment. The clinical implication is then to intervene to increase family cohesiveness and address the issues associated with multiple drug use and its consequences. This finding alone does not link change in cohesion to change in substance use; thus, further analysis was conducted.
Of interest then was the relationship between abuse, change in family cohesion, and change in substance use. Abuse and change in substance use explained the variability in cohesion at baseline. Moreover, substance use changed with changes in cohesion, although change in cohesion did not differ between those who reported abuse and those who did not. These findings have at least three implications. First, the intervention was equally effective for abused and nonabused adolescents on improving family and individual outcomes. No family therapy studies were identified that compared treatment outcomes for abused versus nonabused youth. Although not an FT trial, Naar-King, Silvern, Ryan, and Sebring (2002) compared abused and nonabused adolescents who received at least one month of inpatient treatment for internalizing and externalizing behavior problems. These researchers assessed 187 adolescents ages 12 to 17: 67% were classified as physically or sexually abused; 10% were sexually abused only; 32% were physically abused only; and 25% were both sexually and physically abused. Of interest is that those with histories of sexual abuse alone did not differ from the nonabused group, although physical abuse alone was associated with higher PTSD symptoms. Although the findings from our study suggest that therapeutic focus on presenting symptoms, rather than on abuse specifically, may be effective (Beutler & Hill, 1992; Stevenson, 1999), more research is needed to determine whether specific interventions that focus directly on abuse issues are necessary, and in which cases such focus would be necessary. For example, Allers and Benjack (1992) note that unless the core residual abuse issues are also addressed in a safe, psychotherapeutic setting, during periods of high stress, the survivor will quickly return to self-defeating and self-destructive coping patterns (i.e., substance use). Similarly, Cohen, Deblinger, and Mannarino (2004) found that focus on trauma issues among children with PTSD leads to greater improvement in several problem areas as compared with an intervention without such focus.
Second, the results provide support to the theoretical framework guiding family systems therapy. That is, improvement in individual functioning, such as substance use, is assumed to be related to change in family interaction patterns targeted by the intervention. Until recently, researchers had concluded that although FT improves substance use problems among adolescents, evidence for its impact on family interaction variables proved more elusive. This study adds to more recent findings (Huey et al., 2000; Liddle et al., 2001) in which connections between change in family functioning and specific adolescent problem behaviors have begun to be identified.
Finally, as FES cohesion measures perceived commitment, help and support that family members provide for one another, it follows that these are important targets of the FT intervention. In fact, couples research has shown that the presence of positivity, rather than the lack of negativity, predicts greater relationship satisfaction and better marital outcomes (Gottman, Coan, Swanson, & Carrere, 1998).
Although decreasing conflict and addressing dysfunctional interaction patterns are integral to change, increasing the presence of positive interactional behaviors may be of key importance to sustaining improved individual and family functioning.
Several limitations should be addressed. First, results are based solely upon the youths’ self-reports of both their own and their families’ functioning. Parent perspective and observational methods would provide a rich source of data and would likely provide even greater elucidation on the mechanisms of change. Second, a longer follow-up period could provide more information on the generalization of change over time, as few treatment outcome studies extend their treatment follow-up beyond 1 year. Third, although Hispanics were overrepresented in this sample, other minority groups were underrepresented which limits generalizability. Moreover, runaway adolescents and families in other regions of the country might differ from those in the Southwest. The primary disadvantage of evaluation within homogeneous groups is loss of generalizability and the need for studies to be replicated with diverse subpopulations of abused youth.
Clinical Implications
In all, there are several clinical implications of this research. First, clinical intervention focused on increasing positive interaction may be integral to improvement, especially for runaway youth with a history of childhood abuse who reported lower cohesion levels at baseline as compared with their non-abused peers. Therapists may need to identify and increase behaviors in which family members support one another. Communication skills training and decreasing negative attributions and blame is likely insufficient, as reduction of negative attributions/interaction patterns does not imply an automatic increase in positive interactions. The family-systems-based intervention employed in this study was not developed specifically for adolescents with a history of childhood abuse. Abused adolescents improved similarly to nonabused adolescents in many areas, suggesting that mandatory focus on childhood abuse issues is not required to achieve successful outcomes. However, sensitivity to the needs of youth with trauma histories is necessary to determine the direction of the intervention. An adolescent who reports trauma symptoms, and one who wishes to discuss his or her trauma, is likely to benefit from a trauma-focused intervention. Other adolescents with childhood abuse will not report such symptoms, and they are likely, for instance, to identify their greatest need as improving their relationship with other family members.
Conclusion and Future Direction
Firm conclusions have not been reached regarding the most effective techniques for treating abused children given that many studies have not used adequate controls and many have included small sample sizes. The population served through this program reflects clinical reality in that these youth have multiple problems and present for associated services through agencies (e.g., shelters) that are less prepared to address their complex needs. Involvement of the family in treatment for abused children is supported by this study and others (Deblinger, Lippmann, & Steer, 1996; Kolko, 1996; Monck et al., 1994). Research needs to examine the relationship between relational positivity or cohesiveness, conflict resolution, and outcome among couples versus family groups. According to marital theory, Driver and Gottman (2004) contend that conflict resolution may be a path to increased positivity in that most couples therapies focus on communication and conflict resolution. Future studies will need to examine whether this holds true for family therapy interventions as well.
Acknowledgments
This work has been supported by NIDA grant (R29 DA 11590) and NIAAA and CSAT grant (R01 AA12173).
References
- Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist and Child Behavior Profile. Burlington, VT: Child Psychiatry, University of Vermont; 1982. [Google Scholar]
- Alexander JR, Parsons BV. Functional family therapy: Principles and procedures. Carmel, CA: Brooks/Cole; 1982. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington DC: American Psychiatric Association; 2000. [Google Scholar]
- Allers CT, Benjack KJ. Connections between child abuse and HIV infection. Journal of Counseling and Development. 1991;70:309–313. [Google Scholar]
- Baer JS, Ginzler JA, Peterson PL. DSM-IV alcohol and substance abuse and dependence in homeless youth. Journal of Studies on Alcohol. 2003;64(5):5–14. doi: 10.15288/jsa.2003.64.5. [DOI] [PubMed] [Google Scholar]
- Baker CR. A comparison of individual and group therapy as treatment of sexually absued adolescent females. Dissertation Abstract International. 1987;47(10B):4319–4320. [Google Scholar]
- Beitchman HJ, Zucker JK, Hood EJ, DaCosta AG, Akman D. A review of the short-term effects of child sexual abuse. Child Abuse and Neglect. 1991;15:537–556. doi: 10.1016/0145-2134(91)90038-f. [DOI] [PubMed] [Google Scholar]
- Beutler EL, Hill EC. Process and outcome research in the treatment of adult victims of childhood sexual abuse: Methodological issues. Journal of Consulting and Clinical Psychology. 1992;60:204–212. doi: 10.1037//0022-006x.60.2.204. [DOI] [PubMed] [Google Scholar]
- Cohen AJ, Mannarino PA. Interventions for sexually abused children: Initial treatment outcome findings. Child Maltreatment. 1998;3(1):17–26. [Google Scholar]
- Cohen AJ, Mannarino PA. Predictors of treatment outcome in sexually abused children. Child Abuse and Neglect. 2000;24:983–994. doi: 10.1016/s0145-2134(00)00153-8. [DOI] [PubMed] [Google Scholar]
- Cohen AJ, Deblinger E, Mannarino A. Trauma-focused cognitive-behavioral therapy for sexually abused children. Psychiatric Times. 2004;21:52–53. [Google Scholar]
- Cohen AJ, Deblinger E, Mannarino A, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:393–402. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deblinger E, Lippmann J, Steer R. Sexually abused children suffering posttraumatic stress symptoms: Initial treatment outcome findings. Child Maltreatment. 1996;1:310–321. [Google Scholar]
- Dembo R, Williams L, Wish E, Dertke M, Berry E, Getreu A, Washburn M, Schmeidler J. The relationship between physical and sexual abuse and illicit drug use: A replication among a new sample of youths entering a juvenile detention center. International Journal of Addictions. 1988;23:1101–1123. doi: 10.3109/10826088809056189. [DOI] [PubMed] [Google Scholar]
- Driver JL, Gottman JM. Daily marital interactions and positive affect during marital conflict among newlywed couples. Family Process. 2004;43:301–314. doi: 10.1111/j.1545-5300.2004.00024.x. [DOI] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D. Social class and delinquent behavior in a national youth panel. Criminology: An Interdisciplinary Journal. 1983;21:149–177. [Google Scholar]
- Finkelhor D, Berliner L. Research on the treatment of sexually abused children: A review and recommendations. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1408–1423. doi: 10.1097/00004583-199511000-00007. [DOI] [PubMed] [Google Scholar]
- Forst ML, Crim D. A substance use profile of delinquent and homeless youths. Journal of Drug Education. 1994;24:219–231. doi: 10.2190/K7VM-P8KN-P2FD-W9C3. [DOI] [PubMed] [Google Scholar]
- Gottman J, Coan J, Swanson C, Carrere S. Predicting marital happiness and stability from newlywed interactions. Journal of Marriage and the Family. 1998;60:5–22. [Google Scholar]
- Harrison PA, Fulkerson JA, Beebe T. Multiple substance use among adolescent physical and sexual abuse victims. Child Abuse and Neglect. 1997;21:529–539. doi: 10.1016/s0145-2134(97)00013-6. [DOI] [PubMed] [Google Scholar]
- Huey SJ, Henggeler SW, Brondino MJ, Pickrel SG. Mechanisms of change in multisystemic therapy: Reducing delinquent behavior through therapist adherence and improved family and peer functioning. Journal of Consulting and Clinical Psychology. 2000;68:451–467. [PubMed] [Google Scholar]
- Jacobson NS, Follette WC, Ravensdorf D. Psychotherapy outcome research: Methods for reporting variability and evaluating clinical significance. Behavior Therapy. 1984;15:336–352. [Google Scholar]
- James S, Mennen F. Treatment outcome research: How effective are treatments for abused children? Child and Adolescent Social Work Journal. 2001;18(2):73–95. [Google Scholar]
- Kaliski EM, Rubinson L, Lawrence L, Levy SR. AIDS, runaways, and self-efficacy. Family and Community Health. 1990;13:60–67. [Google Scholar]
- Kaufman GJ, Widom SC. Childhood victimization, running away, and delinquency. Journal of Research in Crime and Delinquency. 1999;36:347–370. [Google Scholar]
- Kendall-Tackett AK, Williams ML, Finkelhor D. Impact of sexual abuse on children: A review and synthesis of recent empirical studies. Psychological Bulletin. 1993;113:164–180. doi: 10.1037/0033-2909.113.1.164. [DOI] [PubMed] [Google Scholar]
- Kipke MD, Montgomery SB, Simon TR, Iverson EF. Substance abuse disorders among runaways and homeless youth. Substance Use and Misuse. 1997;32:969–986. doi: 10.3109/10826089709055866. [DOI] [PubMed] [Google Scholar]
- Klimidis S, Minas IH, Ata AW. The PBI-BC: A brief current form of the parental bonding instrument for adolescent research. Comprehensive Psychiatry. 1992;33:374–377. doi: 10.1016/0010-440x(92)90058-x. [DOI] [PubMed] [Google Scholar]
- Kolko JD. Individual cognitive behavioral treatment and family therapy for physically abused children and their offending parents: A comparison of clinical outcomes. Child Maltreatment. 1996;1:322–342. [Google Scholar]
- Koopman C, Rosario M, Rotheram-Borus MJ. Alcohol and drug use and sexual behaviors placing runaways at risk for HIV infection. Addictive Behaviors. 1994;19:95–103. doi: 10.1016/0306-4603(94)90055-8. [DOI] [PubMed] [Google Scholar]
- Latimer WW, Winters CK, D’Zurilla T, Nichols M. Integrated family and cognitive-behavioral therapy for adolescent substance abusers: A stage I efficacy study. Drug and Alcohol Dependence. 2003;71:303–318. doi: 10.1016/s0376-8716(03)00171-6. [DOI] [PubMed] [Google Scholar]
- Liddle AH. Family-based therapies for adolescents alcohol and drug use: Research contributions and future research needs. Addiction. 2004;99(Suppl 2):76–92. doi: 10.1111/j.1360-0443.2004.00856.x. [DOI] [PubMed] [Google Scholar]
- Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional family therapy for adolescent drug abuse: Results of a randomized clinical trial. American Journal of Drug Alcohol Abuse. 2001;27:651–688. doi: 10.1081/ada-100107661. [DOI] [PubMed] [Google Scholar]
- Lindsey WE, Kurtz PD, Jarvis S, Williams RN, Nackerud L. How runaway and homeless youth navigate troubled waters: Personal strengths and resources. Child and Adolescent Social Work Journal. 2000;17(2):115–141. [Google Scholar]
- Luke DA. Multilevel modeling. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- Mas CH. Unpublished doctoral dissertation. University of Utah; Salt Lake City, UT: 1986. Attribution styles and communication patterns in families of juvenile delinquents. [Google Scholar]
- McLaney MA, DelBoca FK, Babor TF. A validation study of the Problem Oriented Screening Instrument for Teenagers (POSIT) Journal of Mental Health. 1994;3:363–376. [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form-90 family of instruments. Journal of Studies on Alcohol. 1994;(Supplement No 12):112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Marlatt GA. Manual for the comprehensive drinker profile. Odessa, FL: Psychological Assessment Resources; 1984. [Google Scholar]
- Milner SJ, Chilamkurti C. Physical child abuse perpetrator characteristics: A review of literature. Jurnal of Interpersonal Violence. 1991;6:345–366. [Google Scholar]
- Molnar EB, Shade BS, Kral HA, Booth ER, Watters KJ. Suicidal behavior and sexual/physical abuse among street youth. Child Abuse and Neglect. 1998;22:213–222. doi: 10.1016/s0145-2134(97)00137-3. [DOI] [PubMed] [Google Scholar]
- Monck E, Sharland E, Bentovim A, Goodall G, Hyde C, Lewin B. Child sexual abuse: A descriptive and treatment outcome study. London: HMSO; 1994. [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale manual. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- Naar-King S, Silvern L, Ryan V, Sebring D. Type and severity of abuse as predictors of psychiatric symptoms in adolescence. Journal of Family Violence. 2002;17:133–149. [Google Scholar]
- National Child Abuse and Neglect Data System. Child maltreatment. 2002 Retrieved on November 2, 2004, from http://www.acf.hhs.gov/programs/cb/publications/cmreports.htm.
- National Clearinghouse on Child Abuse and Neglect Information. What is child abuse and neglect? 2004 Retrieved on November 2, 2004, from http://nccanch.acf.hhs.gov/pubs/factsheets/whatiscan.cfm.
- Ozechowski TJ, Liddle HA. Family-based therapy for adolescent drug abuse: Knowns and unknowns. Clinical Child and Family Psychology Review. 2000;3:269–298. doi: 10.1023/a:1026429205294. [DOI] [PubMed] [Google Scholar]
- Parker G. Parental overprotection: A risk factor in psychosocial development. New York: Grune & Stratton; 1983. [Google Scholar]
- Parker G, Tupling H, Brown LB. A parental bonding instrument. British Journal of Medical Psychology. 1979;52:1–10. [Google Scholar]
- Pelcovitz D, Kaplan JS, Ellenberg A, Labruna V, Salzinger S, Mandel F, Weiner M. Adolescent physical abuse: Age at time of abuse and adolescent perception of family functioning. Journal of Family Violence. 2000;15:375– 389. [Google Scholar]
- Rahdert E. DHHS Publication No. (ADM) 91–1735. Rockville, MD: National Institute on Drug Abuse; 1991. The adolescent assessment and referral system manual. [Google Scholar]
- Raudenbush SW, Bryk A. Hierarchical linear models. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon R. HLM 5. Chicago: Scientific Software International; 2002. [Google Scholar]
- Rotheram-Borus MJ. The risky business of adolescence: How to help teens stay safe. Select Committee on Children, Youth and Families. U.S. House of Representatives; Washington, DC: 1991. June 17, 1991, Testimony at hearing. [Google Scholar]
- Santisteban DA, Perez-Vidal A, Coatsworth JD, Kurtines WM. Efficacy of Brief Strategic Family Therapy in modifying Hispanic adolescent behavior problems and substance use. Journal of Family Psychology. 2003;17:121–133. doi: 10.1037/0893-3200.17.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D. The Diagnostic Interview Schedule for Children—2.3 Version. New York: Columbia University; 1992. [Google Scholar]
- Slesnick N, Prestopnik JL. Ecologically-based family therapy outcome with substance abusing runaway adolescents. Journal of Adolescence. 2005;28:277–298. doi: 10.1016/j.adolescence.2005.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Tonigan JS. Assessment of alcohol and other drugs used by runaway youths: A test-retest study of the Form 90. Alcoholism Treatment Quarterly. 2004;22(2):21–34. doi: 10.1300/J020v22n02_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back. In: Litten R, Allen J, editors. Measuring alcohol consumption. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Stevenson J. The treatment of the long term sequelae of child abuse. Journal of Clinical Psychology and Psychiatry. 1999;40:89–111. [PubMed] [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics (CT) Scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Sullivan MP, Knutson FJ. The prevalence of disabilities and maltreatment among runaway children. Child Abuse and Neglect. 2000;24:1275–1288. doi: 10.1016/s0145-2134(00)00181-2. [DOI] [PubMed] [Google Scholar]
- Swenson CC, Spratt GE. Identification and treatment of child physical abuse through medical and mental health collaborations. Children’s Health Care. 1999;28:123–139. [Google Scholar]
- Thompson JS, Kost AK, Pollio ED. Examining risk factors associated with family reunification for runaway youth: Does ethnicity matter? Family Relations. 2003;52:296–304. [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: An instrument for assessing alcohol treatment outcome. Journal of Studies on Alcohol. 1997;58:358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Tyler AK, Cauce MR. Perpetrators of early physical and sexual abuse among homeless and runaway adolescents. Child Abuse and Neglect. 2002;26:1261–1274. doi: 10.1016/s0145-2134(02)00413-1. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services, National Center on Child Abuse and Neglect, Child Maltreatment 1996. Reports from the states to the National Child Abuse and Neglect Data System. Washington, DC: US Government Printing Office; 1998. [Google Scholar]
- Van Leeuwen JM, Hopfer C, Hooks S, White R, Petersen J, Pirkopf J. A snapshot of substance abuse among homeless and runaway youth in Denver, Colorado. Journal of Community Health. 2004;29:217–229. doi: 10.1023/b:johe.0000022028.50989.aa. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Howard MO. Adolescent substance abuse treatment: A synthesis of controlled evaluations. Research on Social Work Practice. 2004;14:325–335. [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. Journal of Consulting and Clinical Psychology. 2001;69:802–813. [PubMed] [Google Scholar]
- Westerberg VS, Miller WR, Tonigan JS. Reliability of the Form 90D: An instrument for quantifying drug use. Substance Abuse. 1999;19:179–189. doi: 10.1080/08897079809511386. [DOI] [PubMed] [Google Scholar]
- Westermeyer J, Wahmanholm K, Thuras P. Effects of childhood physical abuse on course and severity of substance abuse. American Journal on Addictions. 2001;10:101–110. doi: 10.1080/105504901750227769. [DOI] [PubMed] [Google Scholar]
- Wolfe SM, Toro PA, McCaskill P. A comparison of homeless and matched housed adolescents on family environment variables. Journal of Research on Adolescence. 1999;9:53–66. [Google Scholar]
- Yoder KA. Comparing suicide attemptors, suicide ideators, and non-suicide homeless and runaway adolescents. Suicide and Life Threatening Behaviors. 1999;29:25–36. [PubMed] [Google Scholar]