Abstract
Examination of differences between primary alcohol and drug abusing adolescents can provide valuable direction to intervention efforts, though little research in this area has been conducted. The current study compared primary alcohol and primary drug abusing runaway adolescents who were randomly assigned to family therapy or treatment as usual. Baseline differences, as well as response to treatment, were examined separately for alcohol and drug use and by gender. Although few baseline differences were found, hierarchical linear modeling indicated that alcohol and drug abusing male and female adolescents responded differently to therapy. Primary drug using males showed poorer alcohol use outcomes than did primary alcohol abusers. Specifically, alcohol use increased for primary drug using males receiving family therapy, while drug use decreased in all groups. Findings suggest that alcohol and drug use outcomes might be improved at treatment planning through consideration of client’s gender and primary alcohol versus drug use.
Keywords: Runaway, Family therapy, Substance abuse, Adolescence
Although some psychosocial treatments for substance abuse problems focus on alcohol problems as distinct from drug problems, most treatments target both groups (Ellingstad, Sobell, Sobell, & Planthara, 2002). Weisner (1992) notes “An accurate picture of the differences and similarities in alcohol and drug treatment populations is lacking….” (p. 431). Although many studies focus on prevalence of use among treatment seeking adolescent and adult populations, few researchers focus on baseline and treatment outcome differences between primary illicit drug (e.g., marijuana dependence and alcohol abuse but not vice versa) and primary alcohol users, especially within adolescent samples.
Given widespread polysubstance use among adolescents (e.g., Martin, Arria, Mezzich, & Bukstein, 1993), an important question is whether the distinction of primary alcohol versus drug use is useful in informing psychosocial intervention efforts. As a step towards addressing this gap in the literature, the current study examined individual and family differences between primary alcohol and primary illicit drug abusing adolescents at baseline and compared the impact of family therapy on alcohol and drug use.
Among adults, research suggests that primary illicit drug users experience more problems than primary alcohol users. Studies report that primary drug users show more severe social and psychological problems in the legal, medical, employment and family domains (Cooke, Kelley, Fals-Stewart, & Golden, 2004; Miller, 1993; Weisner, 1992). Weisner (1992, 1993) compared samples of alcohol versus drug treatment seeking adults and found that clients in alcohol treatment used fewer different drugs than those in drug treatment programs but reported more frequent and heavier drinking. A higher proportion of alcohol compared to drug treatment clients used alcohol in combination with each of nine drug types in the past year. Weisner (1993) found several differences between women and men in alcohol as compared to drug treatment programs, suggesting that attention should be devoted to the differences experienced as a function of gender as well as involvement in drug versus alcohol treatment.
1. Adolescent treatment
No adolescent studies were found that directly compared treatment outcome for primary alcohol versus primary drug abusing adolescents. Also, adolescent studies frequently combined alcohol and drug use into one outcome measure, making conclusions regarding differences in treatment outcome for alcohol and drug use difficult to make. However, studies which reported outcomes separately for alcohol and drug use suggest that illicit drug and alcohol use respond differently to psychosocial treatments.
For example, two studies examining family therapy outcome as compared to individual therapy (Azrin et al., 2001) and group therapy (Santisteban, Coatsworth, Perez-Videl, & Kurtines, 2003) indicated that although illicit drugs were significantly reduced in the experimental interventions, neither the experimental or control interventions significantly reduced alcohol use. Azrin, Donohue, Besalel, Kogan, and Acierno (1994) found that those assigned to behavioral family therapy compared to supportive counseling showed greater reductions in drug use. Although alcohol use was reduced in the family therapy intervention, unlike drug use, alcohol use increased among those assigned to supportive counseling. Overall, findings regarding gender are mixed. Several researchers have noted that females are more likely to reduce their substance use following treatment compared to males (Chung et al., 2003), while other studies find no gender effects (Latimer, Newcomb, Winters, & Stinchfield, 2000).
2. Current study
This study has several goals. First, differences between primary alcohol and drug using youth were examined along individual and family variables at baseline, with the expectation that drug abusing youth would report more problems than alcohol abusing youth. Second, each group’s response to treatment was explored with substance use outcomes examined separately for alcohol and illicit drugs. Although little is available to guide this hypothesis, as noted, primary drug users experience more overall problems than primary alcohol users (Cooke et al., 2004). Also, higher levels of baseline problems and hard core illicit drug use are associated with poorer substance use outcomes (Ellingstad et al., 2002). Finally, given the importance of examining gender differences in alcohol and drug populations (Weisner, 1993) and its potential influence on treatment outcome among adolescents (Colby, Lee, Lewis-Esquerre, Esposito-Smythers, & Monti, 2004), baseline and treatment outcome differences were explored by gender.
3. Methods
3.1. Overview
Data from two randomized trials examining family therapy outcome with an alcohol abusing sample (NIAAA and CSAT grant R01 AA12173) and a drug abusing sample (NIDA grant R29 DA 11590) of runaway adolescents were utilized. The design of the studies differed only in that the primary alcohol problem youth and families were assigned to one of two family therapy conditions, a home-versus office-based approach, and the primary drug abusing sample was assigned only to a home-based approach. Both studies were conducted simultaneously and included a treatment as usual condition through the local runaway shelter. In order to have homogenous treatment groups, only data from those youth assigned to the home-based family therapy in the primary drug and primary alcohol project were compared.
3.2. Participants
Adolescents were recruited from two Southwestern runaway shelters. Inclusion criteria for adolescents included: (1) between the ages of 12 to 17, (2) had the legal option of returning to a home situation (including foster or other family member), (3) met DSM-IV criteria for an drug or alcohol use disorder, (4) family lived within 60 miles of the research site, and (5) at least one parent or surrogate parent was willing to participate in therapy. In order to be assigned to the drug abusing condition, the youth had to have as their primary drug of abuse a psychoactive substance other than alcohol. In order to be assigned to the alcohol abusing condition, the youth had to have alcohol as their primary drug of abuse. This was determined by their CDISC diagnosis. Identical inclusion criteria were used by Cooke et al. (2004) to differentiate primary alcohol versus drug groups. Adolescents were excluded if there was evidence of unremitted psychosis or other condition, which would impair his or her ability to consent for research participation.
The total sample (N =202) included 113 (56%) females, with an average age of 15.0 years (S.D.=1.4). Reported ethnicity included Anglo (N =67, 33.2%), Hispanic, (N =86, 42.6%), Native American (N =14, 6.9%), African American (N =13, 6.4%), and mixed ethnicity (N =21, 10.4%). On average, youth had run away from home 4.4 times, been arrested 2.2 times, and reported a median annual family income of $20,000. Of those youth assigned to family therapy, 37 were primary alcohol users and 64 were primary drug users. Among the youth in TAU, 42 were primary alcohol abusers and 59 were primary drug abusers. Characteristics of the primary alcohol and primary drug using groups are described below.
Among the primary alcohol abusing sample (N =79), 43 (67%) also met diagnostic criteria for marijuana or other substance abuse or dependence. Overall, 42 (53%) met criteria for alcohol dependence and 28 (35%) met criteria for alcohol abuse. Of the 9 youth who did not meet diagnostic criteria, all showed patterns of problem alcohol use with an average of 39.7% days of alcohol use in the period and an average of 10 standard drinks per drinking episode, and so were included in the project. Overall, primary alcohol abusers drank significantly more standard drinks per drinking occasion (M =9.7, S.D.=6.8) than did primary drug abusers (M =6.7, S.D.=7.2), F(1,201)=8.7, p < 0.05. Primary alcohol users drank alcohol a significantly higher percentage of days in the prior 90 days (M =26.5% of the days, S.D.=24.0) than did primary drug abusers (M =5.3% days, S.D.=1.2), F(1,100)=36.02, p < 0.001.
Among the primary drug abusing sample (N =123), 39 (31%) also met criteria for alcohol abuse or dependence. In sum, 103 (83%) reported marijuana abuse or dependence, 31 (25%) reported other substance abuse or dependence, and 39 (32%) reported alcohol abuse or dependence. Ten youth did not meet CDISC criteria for any substance abuse or dependence, although again, these youth showed problematic patterns of drug use, with an average of 52% days of drug use in the period (and 8.5% days of alcohol use) and were included in the study.
3.3. Procedure and treatment
A project research assistant approached adolescents in the shelter to determine initial eligibility and interest in the project. If the adolescent was eligible and assented to participate in the study, the parent was contacted. Upon parental consent, the interviewer proceeded to administer the Computerized Diagnostic Interview Schedule for Children (CDISC, Shaffer, 1992), sections on drugs, alcohol, and psychosis to determine formal eligibility of the adolescent. Those not passing inclusion criteria during the formal screening were not included in the project and continued with services provided through the shelter. Those meeting the criteria for participation in the study continued with the assessment battery.
Participants were told that the assessment would take up to 3 hours and that they would receive $25 at the completion of the assessment and were paid $50 for each follow-up assessment. Upon completion of the baseline assessment, all youth were randomized to either EBFT (n =101) or TAU (n =101) using a computerized urn randomization program. Assessment interviews were conducted at baseline, 3, 9, and 15 months post-baseline. The follow-up rates for family therapy was: 90/101 (89%) at 3 months, 90/101 (89%) at 9 months, and 85/101 (84%) 15 months. For TAU, the rate was 82/101 (81%) at 3, 9, and 15 months post-baseline.
3.3.1. Therapist training and supervision
Ecologically based family therapy (EBFT) was developed through a stage 1 efficacy trial (Slesnick & Prestopnik, 2005). Therapists received readings including the treatment manual, a 2-day didactic training which including role play exercises, and received intensive ongoing supervision through audiotape session review. Three therapists conducted therapy with 82% of the families. Two therapists were female and master’s level licensed counselors. One male therapist was a bachelor’s level licensed counselor. All had between 2 and 5 years experience in the field. In comparing therapists, one female therapist had significantly more sessions with clients overall (M =12.2, S.D.=5.1) than the other female therapist (M =8.7, S.D.=6.4) and male therapist (M =9.5, S.D.=5.8), F(2,81)=3.2, p < 0.05. However, no overall interactions between therapist and time were found for percent days of alcohol or drug use ( p’s> 0.10; using repeated measures ANOVAs).
Audiotape recordings of all therapy sessions were used for treatment adherence checks by the supervisor and for use in weekly supervision meetings. Thirty EBFT therapy sessions were coded for the occurrence of 10 different EBFT treatment procedures (yes/no). The average number of procedures used during a session was 6.0 (range 1 to 10). Inter-rater reliability for procedure occurrence was κ =0.73.
3.3.2. Ecologically based family therapy
The home-based family therapy used an ecological approach and is described in detail in Slesnick and Prestopnik (2005). Briefly, preliminary intervention with the family consists of preparing parents and adolescents to come together to talk about issues that may have initiated the runaway episode, and extensive engagement strategies are employed (Slesnick, Meyers, Meade, & Segelken, 2000). Dysfunctional interactions corresponding to the development and continuation of problem behaviors are targeted utilizing communication and problem-solving skills training. Both individual and family sessions are utilized for dealing with substance use in an overt way. Throughout treatment, family members receive assistance obtaining community services such as medical care or job training. On average, families completed 10.0 sessions (S.D.=6.0) and the number of completed sessions did not differ between the primary alcohol (M =9.5) and drug group (M =10.4), F(1,99)=0.53, p > 0.05.
3.3.3. Treatment as usual
Adolescents who were randomized into TAU received informal meetings with staff and crisis counselors as well as service linkage/case management. Each shelter had one master’s level, licensed, counselor. Counselors were supervised by the respective shelter’s clinical director both of whom were Master’s level licensed professional counselors. Case managers were bachelor’s level professionals with a range of educational backgrounds including social work and psychology and were supervised by the crisis counselors. Adolescents in our study were in the shelter an average of 9 days (S.D.=16.0) at the pretreatment assessment and 15 days (S.D.=21.5) at the 3-month follow-up assessment, which did not differ between treatment groups.
Some adolescents received treatment outside our program. At pretreatment, the average number of outside (non-EBFT) treatment sessions was 3.4 (S.D.=12.4), which did not differ between treatment groups. At the 3-month follow-up, the average number of outside treatment sessions was 2.5 (S.D.=5.7), which also did not differ between groups. Although it is likely that many of these reported outside treatment sessions were with shelter staff, the assessment did not differentiate treatments with shelter staff and treatments not with shelter staff.
3.4. Materials
Three domains of interest were assessed: family functioning, substance use, and individual problem behaviors. The assessment included both clinician assisted and self-report questionnaires.
3.4.1. Diagnostic status
Shaffer’s Computerized Diagnostic Interview Schedule for Children (CDISC, 1992) is a computerized instrument consisting of 263 items measuring the criteria for DSM-IV diagnoses. It has demonstrated excellent inter-rater reliability of 97% with clinicians agreeing with the diagnosis of CDISC (Wolfe, Toro, & McCaskill, 1999).
3.4.2. Demographic measures
A demographic questionnaire designed to characterize and compare participants was administered.
3.4.3. Family measures
The Conflict Tactic Scale (CTS, Straus, 1979) was administered to measure the occurrence of several methods of conflict resolution (reasoning, verbal aggression, and physical violence) used by the youth and primary caretaker. The measure has shown good internal consistency with Cronbach’s α of 0.83 (Yoder, 1999) in a clinical sample.
The Parental Bonding Instrument (PBI, Parker, Tupling, & Brown, 1979) consists of 25 items designed to measure youth’s perceived attitudes of parental bonding and overprotection. Reliability and validity have been established in both clinical and non-clinical samples (Klimidis, Minas, & Ata, 1992).
The Family Environment Scale (FES, Moos & Moos, 1986) is a commonly used and well-standardized family assessment instrument. It is comprised of 90 true–false items and consists of 10 subscales, which measure social–environmental characteristics of families. Internal consistencies have ranged from 0.61 to 0.78 and test–retest reliabilities from 0.73 to 0.86. Conflict and Cohesion subscales were used to assess family disturbance as these two areas of functioning have been shown to predict negative communication exchanges in delinquent families (Mas, 1986).
3.4.4. Substance use
The Form 90, developed for NIAAA funded Project Match (Miller & DelBoca, 1994), was the primary measure of quantity and frequency of drug and alcohol use. This measure uses a combination of the timeline follow-back method (Sobell & Sobell, 1992) and grid averaging (Miller & Marlatt, 1984). This tool has shown excellent test–retest reliability for indices of drug use in major categories (Westerberg, Tonigan, & Miller, 1998) including with runaway substance abusing adolescents (Slesnick & Tonigan, 2004) with κ’s for different drug classes ranging from 0.74 to 0.95. Percent days of alcohol and drug use was the primary dependent measure used in this study. To address problem consequences associated with drug use, the POSIT (Rahdert, 1991) was utilized. Support for the psychometric properties of the POSIT, including convergent and discriminant validity, have been reported by McLaney, Delboca, and Babor (1994).
3.4.5. Individual problem behaviors
The National Youth Survey Delinquency Scale (NYSDS, Elliot & Huizinga, 1983) is a structured interview used as a measure of delinquent behavior. Internal consistency alphas range between 0.65 and 0.92, and criterion correlations between self-report and police or parent data approach 0.40 (Moffitt, 1989). The Youth Self-Report (YSR) of the parent-reported Child Behavior Checklist (CBCL, Achenbach & Edelbrock, 1982) is a 120-item scale, which provides factor scores for internalizing, externalizing as well as total behavior problems.
4. Results
In order to examine differences between the primary alcohol and primary drug participants as well as to examine differences between males and females a 2 (gender)× 2 (condition×primary alcohol or primary drug)×2 (TAU or treatment) MANOVA was performed for individual and family variables assessed at baseline. There were overall main effects for gender [ F(12,179) = 2.95, p < 0.001], condition [F(12,179)=10.03, p < 0.001], and treatment versus control group [F(12,179)=2.98, p < 0.001]. There were no significant interaction effects. Post-hoc t-tests revealed several variables had significantly different means. For gender, there was a significant difference between males and females for YSR internalizing, PBI overprotection and care, and BDI scores. The means and standard deviations and t-test results of the variables of interest are presented in Table 1 for males and females, Table 2 for the two conditions, and Table 3 for the treatment versus control groups. For the primary alcohol and the primary drug conditions, there were significant differences in the use of drugs and use of alcohol, and delinquency. For the treatment versus control group, there were significant differences in number of homeless days and delinquency scores.
Table 1.
Post-hoc t-test results comparing males and females on the individual and family variables at baseline
| Males
|
Females
|
t-value | |||
|---|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | ||
| Homeless days | 62.53 | 36.04 | 58.65 | 38.16 | 0.73 |
| Drug use | 47.13 | 23.71 | 40.87 | 34.52 | 1.27 |
| Alcohol use | 13.69 | 19.51 | 13.59 | 19.09 | 0.036 |
| Conflict | 4.95 | 2.41 | 5.51 | 2.56 | −1.57 |
| Cohesion | 4.64 | 2.58 | 4.00 | 2.43 | 1.79 |
| Internalizing | 15.02 | 8.44 | 22.12 | 11.45 | −4.89*** |
| Externalizing | 25.96 | 9.35 | 27.20 | 11.51 | −0.82 |
| Bond OV | 17.64 | 9.06 | 20.33 | 9.00 | −2.10* |
| Bond care | 22.23 | 8.43 | 19.72 | 8.46 | 2.09* |
| Delinquency | 406.95 | 652.11 | 293.08 | 871.88 | 1.02 |
| BDI | 9.23 | 7.68 | 15.96 | 11.32 | −4.79*** |
p < 0.05.
p < 0.001.
Table 2.
Post-hoc comparison t-tests for primary alcohol- and primary drug-treated participants
| Primary alcohol
|
Primary drug
|
t-value | |||
|---|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | ||
| Homeless days | 60.0 | 36.34 | 60.6 | 37.89 | −0.11 |
| Drug use | 35.63 | 33.22 | 48.76 | 34.72 | −2.66** |
| Alcohol use | 26.53 | 24.00 | 5.36 | 8.01 | 9.04*** |
| Conflict | 5.07 | 2.55 | 5.38 | 2.48 | −0.84 |
| Cohesion | 4.61 | 2.59 | 4.07 | 2.45 | 1.48 |
| Internalizing | 19.06 | 10.73 | 18.95 | 10.90 | 0.07 |
| Externalizing | 27.31 | 10.90 | 26.23 | 10.44 | 0.70 |
| Bond OV | 18.00 | 9.38 | 19.88 | 8.88 | −1.43 |
| Bond care | 21.83 | 8.85 | 20.18 | 8.26 | 1.34 |
| Delinquency | 524.46 | 1121.27 | 226.86 | 413.72 | 2.67** |
| BDI | 12.78 | 10.17 | 13.11 | 10.59 | −0.22 |
p < 0.01.
p < 0.001.
Table 3.
Post-hoc comparison t-tests for the treatment versus control groups at baseline
| Control
|
Treatment
|
t-value | |||
|---|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | ||
| Homeless days | 49.51 | 41.22 | 71.21 | 29.07 | −4.32*** |
| Drug use | 42.41 | 34.32 | 44.84 | 35.12 | −0.49 |
| Alcohol use | 13.29 | 17.19 | 13.98 | 21.14 | −0.25 |
| Conflict | 5.35 | 2.54 | 5.17 | 2.48 | 0.52 |
| Cohesion | 4.31 | 2.61 | 4.25 | 2.43 | 0.18 |
| Internalizing | 19.63 | 11.50 | 18.35 | 10.08 | 0.83 |
| Externalizing | 26.32 | 10.17 | 26.99 | 11.07 | −0.44 |
| Bond OV | 18.10 | 9.52 | 20.17 | 8.60 | −1.62 |
| Bond care | 20.09 | 9.06 | 21.57 | 7.92 | −1.23 |
| Delinquency | 530.41 | 1044.61 | 156.09 | 264.79 | 3.49** |
| BDI | 12.24 | 10.45 | 13.72 | 10.36 | −1.01 |
p < 0.01.
p < 0.001.
In order to examine differences in the response to treatment for use of alcohol and use of drugs, Hierarchical Linear Modeling (HLM, Raudenbush & Bryk, 2002) using the HLM5 (Raudenbush, Bryk, Cheong, & Congdon, 2001) computer software program was used. HLM provides advantages over other repeated measures analyses. First, it allows each individual to have a change trajectory rather than simply using an average change across the individuals. This is level 1 of the model and represents that variability in change over time among the individuals in the sample. Once this variability is established, then other variables can be used to try to predict or explain that variability. This is considered level 2 of the model and includes individual characteristics at baseline, as well as treatment group. In the analyses for this project, the HLM models included: level 1, the alcohol use or drug use scores for baseline and the three follow-up time points, and level 2, gender, condition, treatment versus control group, and the individual and family variables hypothesized to impact outcomes. Two series of model tests were performed: one for alcohol use and one for drug use.
4.1. Alcohol use
The first model to be tested was the unconditional model or the unrestricted model that examines the variability in alcohol use scores. In this model the coefficient for alcohol use was 8.68 (t =9.77, p < 0.001). This can be interpreted as the average percent days of alcohol use across all participants and over all time points. One piece of this analysis that is of particular interest is how much of the variability in alcohol use can be attributed to the individual. This is known at the intraclass correlation and in this analysis indicated that about 53% of the variability in alcohol use scores could be attributed to the individual. This is the amount of variance available to predict. The second model tested was the random coefficients model, in which time was added to the model to explain some of the variability in alcohol use scores at level 1. The results of these model tests are presented in Table 4. The coefficient for alcohol use in this model was 12.09 (t =10.10, p < 0.001), which can be interpreted as the baseline alcohol use score. The coefficient for the slope due to time, or change in alcohol use over time was −2.27 (t =−5.87, p < 0.001) indicating that on average alcohol use decreased from baseline over the follow-up period. Both intercepts [χ2(196)=970.76, p < 0.001] and the slopes [χ2(196)=355.17, p < 0.001] had significant variation as well, suggesting that not all individuals had the same baseline score for alcohol use, nor did all individual change in the same way. About 27% of the variance in alcohol use scores could be accounted for by time.
Table 4.
HLM results for the models testing change in alcohol use
| Unconditional
|
Random coefficients
|
Model 1
|
||||
|---|---|---|---|---|---|---|
| Coefficient (S.E.) | t-value | Coefficient (S.E.) | t-value | Coefficient (S.E.) | t-value | |
| Intercept | 8.68 (0.89) | 9.75*** | 12.09 (1.19) | 10.10*** | 41.08 (5.23) | 7.85*** |
| Gender | – | – | 0.55 (2.05) | 0.27 | ||
| Control | – | – | −0.91 (2.06) | −0.44 | ||
| Primary group | – | – | −17.92 (2.46) | −7.28*** | ||
| Slope | – | −2.27 (0.38) | −5.87*** | −9.66 (1.68) | −5.75*** | |
| Gender | – | – | −1.79 (0.69) | −2.59** | ||
| Control | – | – | 1.69 (0.70) | 2.40** | ||
| Primary group | – | – | 4.68 (0.81) | 5.74*** | ||
| Random effects
| ||||||
| Variance component | Variance component | Variance component | ||||
|
| ||||||
| Intercept | 128.07 | 226.18 | 152.97 | |||
| Slope | – | 13.27 | 7.37 | |||
| Level 1 | 112.23 | 81.74 | 81.74 | |||
| Deviance | 6289.76 | 6202.33 | 6111.22 | |||
| # of parameters | 2 | 4 | 4 | |||
p ≤ 0.01.
p < 0.001.
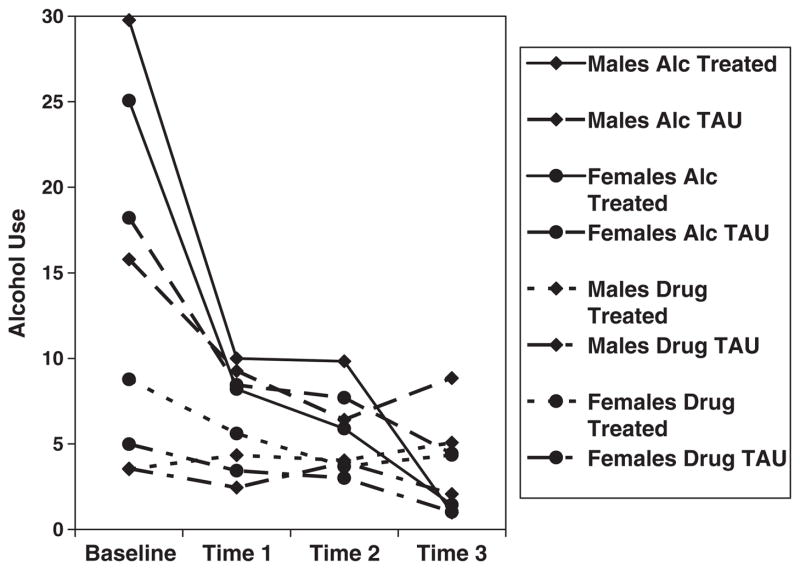
The next model test was used to examine differences between the primary alcohol versus drug groups, treatment groups and gender, to determine if any of these variables could explain the variability in intercepts and slopes at level 1 (model 1 in Table 4). The coefficient for alcohol use in this model was 41.08 (t =10.64, p < 0.001). This can be interpreted as the average alcohol use score for males being treated in the primary alcohol condition. In this model, condition (−17.92, p < 0.001) was a significant predictor of the intercept for alcohol use, suggesting that those in the primary alcohol treatment group had higher alcohol use scores than those in the primary drug treatment group as would be expected. For the slope due to time, gender (−1.79, t =−2.59, p < 0.01), condition (4.68, t =5.74, p < 0.001), and treatment versus control group (1.69, t =2.40, p < 0.05) were significant predictors. The effects of gender, condition and control group status are depicted in Fig. 1. The use of alcohol decreased more in the primary alcohol treatment group, while it may have increased slightly for the males in the primary drug treatment group. These variables accounted for 32% of the variability in the intercepts and 44% of the variability in slopes for this sample.
Fig. 1.
Graphic depiction of the effects gender, treatment condition, and control group overtime for alcohol use.
The final step in the HLM analysis was to explore which of the individual and family variables believed to impact treatment outcomes were significant predictors of the variability in alcohol use at baseline and change in alcohol use. HLM5 has an exploratory function in which it tests whether each variable entered separately could predict variability. In the model for slope, all of the individual and family variables were entered. Only the consequences due to use of substances held promise as a predictor of some of the variability, no other variable reached significance. However, when consequences were entered into the model with gender, condition, and control group, it was no longer a significant predictor. None of the hypothesized variables were determined to be significant predictors of the variability in intercepts or baseline alcohol use in this sample.
4.2. Drug use
The same procedures were used to test models for the use of drugs over the follow-up period. The first model to be tested was the unconditional model or the unrestricted model that examines the variability in drug use scores. In this model, the coefficient for drug use was 31.75 (t =17.34, p < 0.001). This can be interpreted as the average percent days of drug use across all participants and over all time points. The intraclass correlation derived from this analysis indicated that about 41% of the variability in drug use scores could be attributed to the individual. The second model tested was the random coefficients model, in which time was added to the model to explain some of the variability in drug use scores at level 1. The results of these model tests are presented in Table 5. The coefficient for drug use in this model was 40.20 (t =17.59, p < 0.001), which can be interpreted as the average baseline drug use score for all participants. The coefficient for the slope due to time, or change in drug use over time was −5.63 (t =−5.98, p < 0.001) indicating that on average drug use decreased from baseline over the follow-up period. Both intercepts [χ2(196)=550.61, p < 0.001] and the slopes [χ2(196)=326.17, p < 0.001] had significant variation as well. About 24% of the variance in drug use scores could be accounted for by time.
Table 5.
HLM results for the models testing change in drug use
| Unconditional
|
Random coefficients
|
Model 1
|
||||
|---|---|---|---|---|---|---|
| Coefficient (S.E.) | t-value | Coefficient (S.E.) | t-value | Coefficient (S.E.) | t-value | |
| Intercept | 31.75 (1.83) | 17.34*** | 40.20 (2.28) | 17.59*** | 24.44 (8.27) | 2.95** |
| Gender | – | – | −8.12 (4.54) | −1.78 | ||
| Control | – | – | −1.41 (4.45) | −0.31 | ||
| Primary group | – | – | 13.02 (4.51) | 2.88** | ||
| Slope | – | −5.63 (0.94) | −5.98*** | −1.70 (3.35) | −0.50 | |
| Gender | – | – | −.81 (1.85) | −0.44 | ||
| Control | – | – | 3.24 (1.84) | 1.75 | ||
| Primary group | – | – | 5.74*** | −3.17 (1.86) | −1.70 | |
| Random effects
| ||||||
| Variance component | Variance component | Variance component | ||||
|
| ||||||
| Intercept | 490.20 | 665.75 | 626.88 | |||
| Slope | – | 69.96 | 67.05 | |||
| Level 1 | 693.62 | 525.66 | 525.66 | |||
| Deviance | 7649.78 | 7585.42 | 7545.12 | |||
| # of parameters | 2 | 4 | 4 | |||
p < 0.001.
p ≤ 0.01.
The next model test was used to examine differences between the primary alcohol versus drug groups, treatment groups and gender, to see if any of these variables could explain the variability in intercepts and slopes at level 1 (model 1 in Table 5). The coefficient for drug use in this model was 24.08 (t =10.64, p < 0.001). This can be interpreted as the average drug use score for males being treated in the primary alcohol condition. In this model, condition (13.02, p < 0.01) was a significant predictor of the intercept for drug use, suggesting that those in the primary alcohol treatment group had lower drug use scores than those in the primary drug treatment group as would be expected. For the slope due to time, none of the variables were significant. That is, even though drug use decreased over the time period, it did not appear to matter if the participant was in the primary alcohol or primary drug treatment condition, or in the control group, or male or female.
The final step in the HLM analysis was to explore which of the individual and family variables believed to impact treatment outcomes were significant predictors of the variability in intercepts and slopes. In the exploratory analysis for the intercept of drug use, externalizing behaviors and consequences of substance use were potentially significant predictors. When entered into the model, only externalizing behaviors were significant predictors of the intercept for drug use (0.34, t =2.10, p < 0.05). In the exploratory step for the slope, none of the variables of interest were potentially significant predictors of the slope.
It should be noted that the means on alcohol use and substance use at the last follow-up were different than the baseline means and varied among the treatment conditions and gender. These are presented in Table 6.
Table 6.
Means (standard deviations) for % of days using drugs or alcohol for males and females within treatment groups at 15 months post-baseline
| % Days use | TAU
|
EBFT
|
||
|---|---|---|---|---|
| Males | Females | Males | Females | |
| Alcohol treatment group | ||||
| Drugs | 37.23 (44.2) | 19.92 (26.32) | 15.22 (32.59) | 5.61 (13.15) |
| Alcohol | 7.67 (8.37) | 4.61 (8.02) | 0.74 (1.57) | 1.64 (3.45) |
| Drug treatment group | ||||
| Drugs | 30.32 (36.46) | 24.20 (36.89) | 21.85 (28.33) | 21.80 (25.66) |
| Alcohol | 7.49 (17.33) | 1.20 (2.12) | 4.86 (8.11) | 4.68 (6.42) |
5. Discussion
Few studies have examined differences between the primary drug and primary alcohol problem adolescent populations even though as Weisner (1992) notes, alcohol and drugs carry different meanings and values which affect treatment strategies and outcome. Identification of differences might be very useful for informing intervention strategies with adolescent groups.
Our first hypothesis was not supported. In general, unlike studies with adults (Cooke et al., 2004; Miller, 1993; Weisner, 1992), the findings did not show that primary drug abusing youth reported more individual and family problems compared to primary alcohol abusing youth at baseline. This may reflect sociocultural and legal norms. That is, alcohol is an illicit drug for youth between the ages of 12 and 17. As such, adolescents are likely to experience similar negative consequences for alcohol use as they are for drug use, both socially and legally. Adults may legally purchase and possess alcohol and may experience fewer negative consequences associated with its use, as compared to drugs. Since the two samples of youth in this study were polydrug users, which is representative of adolescent substance users in general (Martin et al., 1993), those who drink alcohol but do not use other drugs or vice versa might show different behavioral correlates and would provide a cleaner test of our first hypothesis.
The second hypothesis was supported. Alcohol use compared to drug use responded differently to the intervention depending upon whether an individual was a primary alcohol or drug user and male or female. Drug use was significantly reduced regardless of gender, treatment, or being a primary alcohol or drug user. However, primary alcohol users showed statistically and clinically significant reductions in frequency of alcohol use (from 28% days to 1% days of use, a 97% reduction) when assigned to the family treatment as compared to those assigned to TAU (who showed a 76% reductions from 25% days of use to 6% days of use); primary drug using males in treatment showed a 32% increase in alcohol use (from 3.3% days to 4.8% days).
This study highlights the need to assess alcohol and drugs separately. Possibly, primary drug abusing males substitute alcohol for drugs when receiving treatment, but future research will need to more fully examine this finding. The clinical implication is that primary drug abusing males may need special attention in intervention efforts on coping and problem solving skills so that alcohol use does not replace reductions in drug use behavior.
Although this study has several strengths including nearly equal representation of males and females, follow-up assessments to 15 months post-baseline, and a randomized design with a control group, several limitations need to be considered. Participants were runaway youth whose family, individual and substance use problems are often more severe than non-runaway youth (Koopman, Rosario, & Rotheram-Borus, 1994). The findings may not generalize to non-runaway youth or those youth within different parts of the country who may experience different sociocultural pressures. Since this was an add-on study, those who received EBFT in general received more treatment and therapist contact than those who received TAU without EBFT. Possibly, the greater therapist contact (and not EBFT) is responsible for outcome. Although findings suggest that EBFT is efficacious, a larger clinical trial comparing EBFT with a viable control condition will be necessary to more fully explore the unique impact of family therapy on outcome among this population.
Determination of factors predicting differences in treatment responsiveness of alcohol versus drug use within different treatment modalities, client populations, and settings is still needed. This study provides some direction for future research examining differences between alcohol and drug use treatment responsiveness through considering primary drug of abuse and gender. Potentially, as Colby et al. (2004) note, future research needs to test the efficacy of treatments that include separate modules for addressing alcohol and other drugs versus those that use a “one size fits all” approach.
Acknowledgments
This work has been supported by NIDA grant (R29 DA 11590) and NIAAA and CSAT grant (AA12173).
References
- Achenbach TM, Edelbrock CS. Manual for the child behavior checklist and child behavior profile. Burlington, VT: Child Psychiatry, University of Vermont; 1982. [Google Scholar]
- Azrin NH, Donohue B, Besalel VA, Kogan ES, Acierno R. Youth drug abuse treatment: A controlled outcome study. Journal of Child and Adolescent Substance Abuse. 1994;3:1–16. [Google Scholar]
- Azrin NH, Donohue B, Teichner GA, Crum T, Howell J, DeCato LA. A controlled evaluation and description of individual-cognitive problem solving and family-behavior therapies in dually-diagnosed conduct-disordered and substance-dependent youth. Journal of Child and Adolescent Substance Abuse. 2001;11:1–43. [Google Scholar]
- Chung T, Martin CS, Grella CE, Winters KC, Abrantes AM, Brown SA. Course of alcohol problems in treated adolescents. Alcoholism: Clinical and Experimental Research. 2003;27:253–261. doi: 10.1097/01.ALC.0000053009.66472.5E. [DOI] [PubMed] [Google Scholar]
- Colby SM, Lee CS, Lewis-Esquerre J, Esposito-Smythers C, Monti PM. Adolescent alcohol misuse: Methodological issues for enhancing treatment research. Addiction. 2004;99(2):47–62. doi: 10.1111/j.1360-0443.2004.00854.x. [DOI] [PubMed] [Google Scholar]
- Cooke CG, Kelley ML, Fals-Stewart W, Golden J. A comparison of the psychosocial functioning of children with drug-versus alcohol-dependent fathers. The American Journal of Drug and Alcohol Abuse. 2004;30(4):695–710. doi: 10.1081/ada-200037530. [DOI] [PubMed] [Google Scholar]
- Ellingstad TP, Sobell LC, Sobell MB, Planthara P. Drug treatment outcome methodology (1993–1997): Strengths, weaknesses, and comparison to the alcohol field. Addictive Behaviors. 2002;27:319–330. [PubMed] [Google Scholar]
- Elliot DS, Huizinga D. Social class and delinquent behavior in a national youth panel. Criminology: An Interdisciplinary Journal. 1983;21:149–177. [Google Scholar]
- Klimidis S, Minas IH, Ata AW. The PBI-BC: A brief current form of the parental bonding instrument for adolescent research. Comprehensive Psychiatry. 1992;33:374–377. doi: 10.1016/0010-440x(92)90058-x. [DOI] [PubMed] [Google Scholar]
- Koopman C, Rosario M, Rotheram-Borus MJ. Alcohol and drug use and sexual behaviors placing runaways at risk for HIV infection. Addictive Behaviors. 1994;19:95–103. doi: 10.1016/0306-4603(94)90055-8. [DOI] [PubMed] [Google Scholar]
- Latimer WW, Newcomb M, Winters KC, Stinchfield RD. Adolescent substance abuse treatment outcome: The role of substance abuse problem severity, psychosocial, and treatment factors. Journal of Consulting and Clinical Psychology. 2000;68(4):684–696. [PubMed] [Google Scholar]
- Martin CS, Arria AM, Mezzich AC, Bukstein OG. Patterns of polydrug use in adolescent alcohol abusers. American Journal of Drug and Alcohol Abuse. 1993;19(4):511–521. doi: 10.3109/00952999309001639. [DOI] [PubMed] [Google Scholar]
- Mas CH. Doctoral Dissertation. University of Utah; Salt Lake City, UT: 1986. Attribution styles and communication patterns in families of juvenile delinquents. [Google Scholar]
- McLaney MA, Delboca FK, Babor TF. A validation study of the Problem Oriented Screening Instrument for Teenagers (POSIT) Journal of Mental Health. 1994;3:363–376. [Google Scholar]
- Miller WR. Alcoholism: Toward a better disease model. Psychology of Addictive Behaviors. 1993;7(2):129–136. [Google Scholar]
- Miller WR, DelBoca FK. Measurement of drinking behavior using the Form-90 family of instruments. Journal of Studies on Alcohol. 1994;12(2):112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Marlatt GA. Manual for the comprehensive drinker profile. Odessa, FL: Psychological Assessment Resources; 1984. [Google Scholar]
- Moffitt TE. Accommodating self-report methods to a low-delinquency culture: Experience from New Zealand. In: Klein MW, editor. Cross-national research in self-reported crime and delinquency. Norwell, MA: Kluwer Academic; 1989. pp. 43–66. [Google Scholar]
- Moos RH, Moos BS. Family environment scale manual. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- Parker G, Tupling H, Brown LB. A parental bonding instrument. British Journal of Medical Psychology. 1979;52:1–10. [Google Scholar]
- Rahdert E. DHHS Publication (ADM) 91-1735. Rockville, MD: National Institute on Drug Abuse; 1991. The adolescent assessment and referral system manual. [Google Scholar]
- Raudenbush SW, Bryk A. Hierarchical linear models. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon R. HLM 5. Chicago, IL: Scientific Software International; 2001. [Google Scholar]
- Santisteban DA, Coatsworth JD, Perez-Videl A, Kurtines WM. Efficacy of brief strategic family therapy in modifying Hispanic adolescent behavior problems and substance use. Journal of Family Psychology. 2003;17(1):121–133. doi: 10.1037/0893-3200.17.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D. The Diagnostic Interview Schedule for Children—2.3 Version. New York: Columbia University; 1992. [Google Scholar]
- Slesnick N, Meyers RJ, Meade M, Segelken DH. Bleak and hopeless no more: Engagement if reluctant substance-abusing runaway youth and their families. Journal of Substance Abuse Treatment. 2000;19(3):215–222. doi: 10.1016/s0740-5472(00)00100-8. [DOI] [PubMed] [Google Scholar]
- Slesnick N, Prestopnik J. Dual and multiple diagnosis among substance using runaway youth. American Journal of Drug and Alcohol Abuse. 2005;31(1):179–201. doi: 10.1081/ADA-200047916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Tonigan JS. Assessment of alcohol and other drugs used by runaway youths: A test–retest study of the Form 90. Alcoholism Treatment Quarterly. 2004;22(2):21–34. doi: 10.1300/J020v22n02_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The conflict tactics (CT) scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Weisner C. A comparison of alcohol and drug-treatment clients—are they from the same population? American Journal of Drug and Alcohol Abuse. 1992;18:429–444. doi: 10.3109/00952999209051040. [DOI] [PubMed] [Google Scholar]
- Weisner C. The epidemiology of combined alcohol and drug use within treatment agencies: A comparison by gender. Journal of Studies on Alcohol. 1993;54:268–274. doi: 10.15288/jsa.1993.54.268. [DOI] [PubMed] [Google Scholar]
- Westerberg VS, Tonigan JS, Miller WR. Reliability of Form 90D: An instrument for quantifying drug use. Substance Abuse. 1998;19(4):179–189. doi: 10.1080/08897079809511386. [DOI] [PubMed] [Google Scholar]
- Wolfe SM, Toro PA, McCaskill PA. A comparison of homeless and matched housed adolescents on family environment variables. Journal of Research on Adolescence. 1999;9:53–66. [Google Scholar]
- Yoder KA. Comparing suicide attempters, suicide ideators, and nonsuicidal homeless and runaway adolescents. Suicide and Life-Threatening Behavior. 1999;29:25–36. [PubMed] [Google Scholar]