Abstract
Fortification of foods and advice on sensible sun exposure are urgently needed
At the turn of the 20th century more than 80% of children living in the industrialised cities of the Western hemisphere had rickets.1 2 Rickets became extremely rare in the United Kingdom, Europe, and United States after it was realised that exposure to ultraviolet light was the major source of vitamin D, and after the fortification of milk and other foods with vitamin D.2 At least a billion people worldwide are estimated to be vitamin D deficient, mainly because of inadequate exposure to sunlight and inadequate fortification of food with vitamin D.1 3 4 5
Skin pigmentation absorbs ultraviolet light, thereby reducing vitamin D production; this can be a problem for certain racial groups who now live in the Northern hemisphere. Human breast milk contains very little vitamin D and women with vitamin D deficiency provide no vitamin D for their infant. Such infants will be at high risk of developing rickets if they are exclusively breast fed. Rickets is the most overt sign of severe vitamin D deficiency in Europe—around 1-5% of children with vitamin D deficiency have skeletal signs of rickets and probably 10-25% of adults with vitamin D deficiency have symptomatic osteomalacia.
Vitamin D deficiency causes secondary hyperparathyroidism and increases destruction of the skeleton by precipitating or exacerbating osteopenia and osteoporosis.1 3 Raised parathyroid hormone concentrations induce phosphaturia and hypophosphataemia; this causes a mineralisation defect of the osteoid (osteomalacia). Unlike osteoporosis, which is a painless disease, rickets and the adult counterpart osteomalacia can cause non-specific aches and pains in bones and muscles, and severe muscle weakness.1 6 7
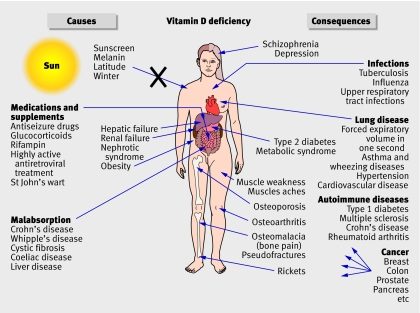
In the accompanying lesson of the week, Sievenpiper and colleagues present two cases of severe vitamin D deficiency where the classic causes (figure ) and clinical consequences were misdiagnosed as fibromyalgia, chronic fatigue syndrome, or degenerative arthritis.1 6 7 8 Sievenpiper and colleagues note that severe secondary hyperparathyroidism causes osteoclastogenesis, which can look like isolated lytic lesions in the skeleton and can be misdiagnosed as metastatic disease8 or even Paget’s disease. The proximal muscle weakness reported by the authors is a common feature of vitamin D deficiency, 1 6 7 8 which can be misdiagnosed as multiple sclerosis or amyotrophic lateral sclerosis.1
Causes and consequences of vitamin D deficiency
So what are the beneficial effects of vitamin D? People who live at higher latitudes, have vitamin D deficiency, or lack exposure to the sun have an increased risk of many cancers (figure).1 3 4 5 Increasing the intake of vitamin D to 1000 IU a day reduces the risk of colorectal cancer and many other deadly cancers by 30-50%.1 3 4 5 Vitamin D deficiency is also linked to cardiovascular disease. After adjusting for standard cardiovascular risk factors, one study found that the risk for the first cardiovascular event was 62% higher in people with vitamin D deficiency.9 Vitamin D deficiency has also been associated with autoimmune diseases, infectious diseases, and schizophrenia (figure).1 5 9 10
Vitamin D has so many health benefits because all tissues have vitamin D receptors.1 3 4 5 Vitamin D controls (directly or indirectly) more than 200 genes that regulate calcium and bone metabolism, modulate innate immunity, control cell growth and maturation, regulate the production of insulin and renin, induce apoptosis and inhibit angiogenesis.1 4 5 9 10 Skin, brain, colon, breast tissue, and macrophages can produce 1,25-dihydroxyvitamin D.1 4 5 9 10 Once produced, 1,25-dihydroxyvitamin D carries out its biological function(s) within the cell and then induces its own destruction.1 25-Hydroxyvitamin D concentrations (the measure of vitamin D status) vary greatly with the season.1 3 4 5
Excessive exposure to sunlight causes an estimated annual loss of 1.6 million disability adjusted life years (DALYs)—0.1% of the total global disease burden in the year 2000. This compares with the loss of about 3.3 billion DALYs from bone disease caused by vitamin D deficiency as a result of too little exposure to sunlight.11 These figures do not take into account the other potential health benefits of sun exposure and vitamin D sufficiency in reducing other chronic diseases, which account for 9.4% of total global disease burden. Notably, non-melanoma skin cancers occur on the most sun exposed areas, such as the face and hands, whereas most melanomas occur on the areas least exposed to the sun.12 Intermittent and occupational sun exposure has been found to reduce the risk of malignant melanoma.1 4 5 12
How should vitamin D deficiency be diagnosed and treated? Serum calcium concentrations are usually normal in people with vitamin D deficiency and 1,25-dihydroxyvitamin D values are normal or raised. The only way to know a person’s vitamin D status is to measure serum 25-hydroxyvitamin D concentrations. Sievenpiper and colleagues provided appropriate aggressive treatment of vitamin D deficiency with 300 000 IU of intramuscular vitamin D3 monthly or 10 000 IU of oral vitamin D2 daily.8 Vitamin D2 (50 000 IU) once a week for eight weeks will correct vitamin D deficiency.1 To maintain vitamin D sufficiency, 50 000 IU of vitamin D2 twice a month or 1000-2000 IU of vitamin D3 a day is usually sufficient.1 3 4 5
Vitamin D intoxication is an extremely rare event and occurs from inadvertent or intentional vitamin D poisoning. Concentrations of 25-hydroxyvitamin D of 75-150 nmol/l are recommended for health. Vitamin D intoxication occurs when concentrations are greater than 375 nmol/l.
Although the health benefits of vitamin D sufficiency are clear, awareness of the dangers of vitamin D deficiency is lacking. People with vitamin D deficiency have no obvious symptoms until it is so severe that they develop osteomalacia; this is often misdiagnosed as fibromyalgia, so many doctors may not be aware of the problem. Public health campaigns that emphasise the insidious consequences of vitamin D deficiency on health are therefore needed. Regulatory health agencies also need to provide recommendations for sensible sun exposure, especially for ethnic minorities. They should also implement aggressive fortification of foods—supplementation should be increased from 100 IU per serving to at least 200 IU. The US, Canada, Sweden, and Finland already fortify milk with vitamin D but this policy should be extended to Europe. More foods, such as pasta, other dairy products, and orange juice should be fortified.
Competing interests: MFH receives research support from the UV Foundation, National Dairy Council, and National Institutes of Health.
Provenance and peer review: Commissioned; not externally peer reviewed.
References
- 1.Holick MF. Vitamin D deficiency. N Engl J Med 2007;357:266-81. [DOI] [PubMed] [Google Scholar]
- 2.Hess AF, Unger LJ. The cure of infantile rickets by sunlight. JAMA 1921;77:39-41. [Google Scholar]
- 3.Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr 2006;84:18-28. [DOI] [PubMed] [Google Scholar]
- 4.Grant WB, Garland CF. The association of solar ultraviolet B (UVB) with reducing risk of cancer: multifactorial ecologic analysis of geographic variation in age-adjusted cancer mortality rates. Anticancer Res 2006;26:2687-99. [PubMed] [Google Scholar]
- 5.Moan J, Porojnicu AC, Dahlback A, Setlow RB. Addressing the health benefits and risks, involving vitamin D or skin cancer, of increased sun exposure. Proc Natl Acad Sci 2008;105:668-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Plotnikoff GA, Quigley JM. Prevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal pain. Mayo Clin Proc 2003;78:1463-70. [DOI] [PubMed] [Google Scholar]
- 7.Erkal MZ, Wilde J, Bilgin Y, Akinci A, Demir E, Bodeker RH, et al. High prevalence of vitamin D deficiency, secondary hyperparathyroidism and generalized bone pain in Turkish immigrants in Germany: identification of risk factors. Osteoporos Int 2006;17:1133-40. [DOI] [PubMed] [Google Scholar]
- 8.Sievenpiper JL, McIntyre EA, Verrill M, Quinton R, Pearce SHS. Unrecognised severe vitamin D deficiency. BMJ 2008. doi: 10.1136/bmj.39555.820394.B [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang TJ, Pencina MJ, Booth SL, Jacques PF, Engelsson E, Lanier K, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation 2008;117:503-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adams JS, Hewison M. Unexpected actions of vitamin D: new perspectives on the regulation of innate and adaptive immunity. Nat Clin Pract Endocrinol Metab 2008;4:80-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lucas RM, McMichael AJ, Armstrong BK, Smith WT. Estimating the global disease burden due to ultraviolet radiation exposure. Int J Epidemiol 2008 Feb 14 [Epub ahead of print]. [DOI] [PubMed]
- 12.Kennedy C, Bajdik CD, Willemze R, de Gruijl FR, Bavinck JN. The influence of painful sunburns and lifetime of sun exposure on the risk of actinic keratoses, seborrheic warts, melanocytic nevi, atypical nevi and skin cancer. J Invest Dermatol 2003;120:1087-93. [DOI] [PubMed] [Google Scholar]