Abstract
Decisions concerning the use of intravenous fluids and antibiotics in terminally ill patients are regularly made by hospital doctors, but there is little record of staff attitudes and current practice in Britain. A questionnaire was therefore distributed to 833 Welsh hospital doctors, citing the case of a hypothetical terminally ill patient and asking questions about medical management. Of the 448 (54%) doctors who replied, 346 (77%) had managed a similar patient recently. Intravenous fluids would be administered by 238 (53%), with 206 of these (87%) resiting the cannula as required and 62 (26%) resorting to a central venous line if there was no alternative. With increasing age and seniority doctors become conservative in their approach. Nearly all claimed that 'ensuring the patient's comfort' was the reason for their decision. Only 72 (16%) would use antibiotics if the patient became pyrexial. The results suggest that British doctors are divided in their approach to the medical management of terminally ill patients and there is a need for greater discussion and training so that all the issues involved are fully appreciated.
Full text
PDF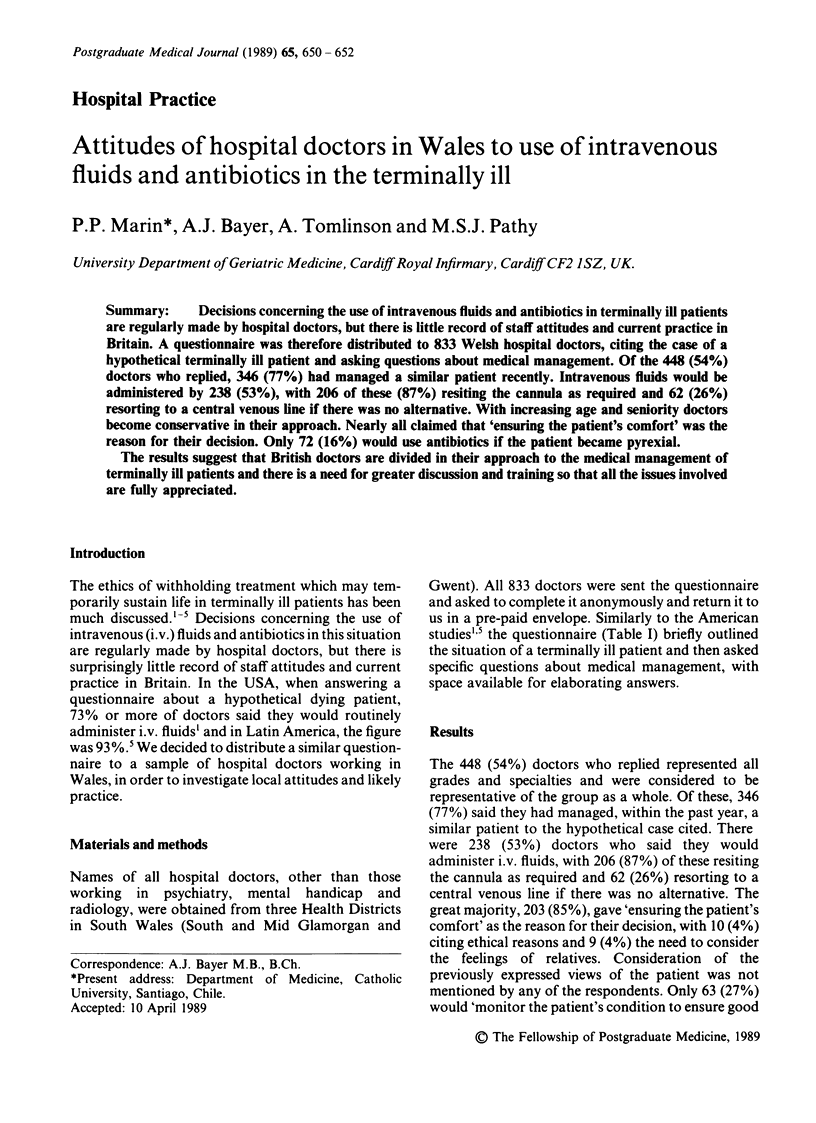

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Micetich K. C., Steinecker P. H., Thomasma D. C. Are intravenous fluids morally required for a dying patient? Arch Intern Med. 1983 May;143(5):975–978. [PubMed] [Google Scholar]
- Wanzer S. H., Adelstein S. J., Cranford R. E., Federman D. D., Hook E. D., Moertel C. G., Safar P., Stone A., Taussig H. B., van Eys J. The physician's responsibility toward hopelessly ill patients. N Engl J Med. 1984 Apr 12;310(15):955–959. doi: 10.1056/NEJM198404123101505. [DOI] [PubMed] [Google Scholar]


