Abstract
Objective
Treatment for localized carcinoma of the prostate (PCa) is frequently associated with decrements in sexual functioning and satisfaction. Given the highly interpersonal nature of these decrements, interpersonal problems (such as interpersonal sensitivity) may affect recovery of sexual functioning after PCa treatment by interfering with physician and partner communication and through distorted cognitions surrounding sexual dysfunction. The objective of the present study was to determine the effect of interpersonal sensitivity on several treatment indicators, including response to a group based psychosocial intervention.
Methods
Participants were 101 older men recovering from radical prostatectomy and were enrolled in a randomized controlled trial of a 10-wk group-based cognitive behavioral stress management (CBSM) intervention. Measures included the Inventory of Interpersonal Problems (IIP) and the Sexual Functioning subscale of the UCLA quality of life measure.
Results
At baseline, interpersonal sensitivity was related to a belief linking sexual dysfunction to core male identity (r = .29, p < .05). Using hierarchical regression, we found that (a) the CBSM intervention was effective in promoting sexual recovery in all participants and that (b) this effect was moderated by interpersonal sensitivity, such that individuals with higher levels of interpersonal sensitivity made larger improvements in sexual functioning in response to CBSM.
Conclusions
CBSM was effective for improving sexual function after radical prostatectomy. Individuals with higher levels of interpersonal sensitivity were more likely to perceive sexual dysfunction as a threat to masculine identity and made larger gains in the CBSM intervention. Results and relevance to the older male cancer patient are discussed from the perspective of interpersonal theory.
Keywords: CBSM, interpersonal sensitivity, interpersonal theory, prostate cancer, radical prostatectomy
Introduction
Interpersonal Sensitivity
The importance of a supportive social environment in the promotion of health and well-being is one of the best documented effects in health psychology.1 Although there are exceptions2, in general individuals with greater quality of social support tend to live longer and experience better quality of life across a range of medical conditions (see Uchino, 2006 for a review).3
As a corollary to the above, there is also evidence that for certain individuals the social network can be a source of strife and distress2,4. Given the reciprocal nature of human interactions and the expectation for shared support in relationships, much research has documented the negative impact of maladaptive interpersonal traits on social support.5,6,7 One such trait is interpersonal sensitivity†. In the context of personality dysfunction research, interpersonal sensitivity is used to describe a problematic interpersonal style characterized by being “too sensitive” to others, a tendency to perceive and elicit criticism and a chronic perception of rejection and abandonment.8 In its more extreme form, interpersonal sensitivity is associated with Avoidant and Borderline personality disorders.8,9
One model used to explain the impact of interpersonal sensitivity on an individual’s social environment comes from Interpersonal Theory.10 This theoretical and clinical approach is based on the observation that we create the quality of our own social networks through our own interpersonal reactions and perceptions.10,11 From this perspective, individuals with high levels of pathological personality traits (such as interpersonal sensitivity) hold to rigid self-concepts and work to confirm these concepts by evoking certain stereotyped responses from others.11–13 For these individuals, the majority of social interactions confirm the belief that others are rejecting and critical,14 bolstering an already rigid and maladaptive interpersonal style.15 High levels of interpersonal sensitivity may thereby degrade the quality of an individual’s social support network directly (i.e., by creating interpersonal conflict) and indirectly (i.e., by diminishing the perception of social support where it does exist). This indirect path may be especially important for men recovering from cancer, given recent evidence that perceived social support may be as or more important than objective social support in reducing distress in medical populations.16,17
Interpersonal Sensitivity and Psychological Interventions
Although there are clear distinctions to be made between perceptions of social support and those of cohesion/alliance in a group treatment setting, it is reasonable to expect that the same maladaptive personality traits might manifest in both areas. That is, given that interpersonal sensitivity is theorized to cause problems in an individual’s social environment, one would expect that the same trait would be associated with decrements in therapeutic alliance and group cohesion, and thereby in the effectiveness of group-based and individual interventions. However, while this certainly appears to be true in diagnosable Axis II conditions,18–25 literature describing the effect of subclinical interpersonal problems such as interpersonal sensitivity on treatment outcomes is considerably less clear. For example, it has been suggested that while certain kinds of personality dysfunction (particularly dominant or hostile styles) negatively impact group climate and attendance,26,27 other styles (particularly more submissive and avoidant styles) are related to a greater sense of working therapeutic alliance and an enhanced perception of group altruism.28–30 There is also evidence suggesting that personality dysfunction is associated with better treatment outcome in supportive and cognitive-behavioral interventions,31–32 particularly when considered in the context of presenting distress.33 Taken together, these data suggest that while many diagnosable Axis II conditions interfere with treatment efficacy, a certain degree of avoidant or submissive personality characteristics (of the kind associated with interpersonal sensitivity) may actually serve to augment benefit from interventions via a number of pathways (discussed in detail in the discussion section).
Psychological Interventions for Men Recovering from Prostate Cancer Treatment
Prostate carcinoma (PCa) is the most common solid tumor malignancy in American men, and results in nearly 30,000 deaths annually.34 Whereas risk factors for PC are not clearly understood, the disease is clearly related to aging, as more than 70% of all cases occur in men over 65.34 Although surgical removal of the prostate gland is associated with a high 10 year survival rate in localized cases (93%),34 sexual dysfunction is a common and often enduring side effect of this treatment.35–37 In one major survey, 85% of patients reported experiencing some erectile dysfunction within the last 6 months even 4.3 years after treatment, and 61% reported moderate or extreme distress relating to this dysfunction.35 Prior work has indicated that psychological interventions directed at psychoeducation or teaching stress management skills can improve aspects of quality of life in men recovering from PCa treatment.38–39 Less is known about how these interventions affect physical recovery—including recovery of sexual functioning—after medical treatments are completed. The present study addressed this gap and also tested the role of interpersonal sensitivity as a possible moderator of intervention effects.
Present Study
The present study had three primary aims. First, we tested the effects of a 10-week, group based Cognitive-Behavioral Stress Management (CBSM) program in promoting sexual functioning in a group of older men recovering from localized PCa. This intervention (discussed below) targeted a variety of issues surrounding recovery from PCa. In terms of sexual dysfunction, the CBSM intervention was designed to: (a) provide practical information regarding treatment options for erectile dysfunction, (b) broaden definitions of sexuality to include options other than intercourse, (c) give participants a safe and supportive environment to address their concerns about sexuality and sexual function, (d) provide participants with skills to effectively discuss sexual dysfunction with partners and (e) train participants to challenge distorted cognitions surrounding problems with sexual performance. We hypothesized that the CBSM intervention would be associated with larger improvements in sexual functioning than would occur in a control condition.
As a second aim, we sought to evaluate interpersonal sensitivity as a moderator of this intervention. Although there are few studies describing interpersonal sensitivity in PCa, this variable may be particularly salient in this population for a number of reasons. From a purely practical perspective, the demands associated with PCa treatment require effective interpersonal communication with one’s physician and partner and reliance on a social network to provide tangible and emotional support. For individuals high in interpersonal sensitivity, the ability to effectively communicate about such sensitive topics without suspiciousness, guardedness or fear of rejection may be lacking. Moreover, treatment for localized PCa requires placing considerable trust in other people (such as one’s medical team), especially given the consequences of treatment failure. For individuals high in interpersonal sensitivity, placing total trust in others may generate considerable anxiety. These speculations are supported by recent data suggesting that individuals with poorer interpersonal relationships tend to react to PCa diagnosis and treatment with more self-blame40 and greater distress when seeking support from others.41
In terms of the impact of interpersonal sensitivity on the efficacy of the CBSM intervention, one recent study demonstrated that certain negative baseline indicators traditionally associated with interpersonal problems (i.e., low self-esteem and depression) were predictive of larger treatment gains in a psychoeducational intervention for men recovering from localized PCa.42 Further, we have previously demonstrated that interpersonal sensitivity is related to poorer sexual function (r = −.28), deficits in perceived partner support (r = −.37) and poorer doctor-patient communication (r = −.27).43 Given the clear need for intervention suggested by these findings, as well as literature showing that a degree of interpersonal dysfunction may be helpful in group interventions,33 we hypothesized that a CBSM approach emphasizing recovery of sexual function (e.g., sexual-aid education and partner communication) would be more effective for individuals reporting higher levels of interpersonal sensitivity.
As a third aim, we sought to understand the impact of interpersonal sensitivity on the perception that sexual dysfunction is a threat to masculine identity. Treatment for prostate cancer may generate schematic challenges, such as the need to separate one’s sexual functioning from representations of masculinity and self-worth. Given the interpersonal theory conceptualization that the core of interpersonal pathology is an inflexibility in one’s core schemas and an inability to alter self-representations to match environmental demands, we hypothesized that higher levels of interpersonal sensitivity would be associated with a greater tendency to see sexual dysfunction as a threat to core masculine identity.
Method
Sample
Participants were 101 men who had undergone radical prostatectomy for localized (i.e. Stage I or II) PCa. Participants were recruited for the study through a combination of methods including distribution of study flyers, urologist referral, and through access to the Florida Cancer Data System, a cancer registry maintained by the Florida Department of Health.
Following initial contact, participants were introduced to the study and asked to complete an initial inclusion/exclusion screen via telephone. Participants were then excluded if they had a prior history of cancer or had received treatment more than 18 months ago. Because PCa is primarily a disease of older men, and given that younger men with PCa tend to have different concerns than their older counterparts (e.g., greater likelihood of metastatic disease) the CBSM intervention described below was designed and tailored for men at or above retirement age. Participants were therefore excluded if they were < 45 year old to ensure the appropriateness of the intervention to the study participants.
If participants met these initial criteria, they were scheduled for a follow-up screening in a face-to-face interview. This screening assessed for other exclusion criteria including reading level (less than 9th grade), cognitive impairment, and active psychiatric symptoms including panic attacks, post-traumatic stress disorder, suicidal ideation, psychosis or substance dependence in the past 3 months. This assessment included the Folstein Mini-Mental Status Examination (>23)44 and the Structured Clinical Interview for the DSM-IV.45 Participants who met all inclusion criteria were provided with an opportunity to ask questions about the study and signed an IRB approved informed consent form.
Following screening and informed consent procedures, participants completed the baseline assessment battery. They were then randomly assigned to either the experimental (10-week group) or control (one-day seminar) condition. The procedure for randomization is described in detail below. The one-day control seminar was scheduled approximately 6 weeks into the 10-week course of the experimental condition. Experimental participants were then reassessed within 2–3 weeks of completion of the 10-week intervention, while control participants were reassessed 7–8 weeks after the one-day seminar to ensure parallel time periods between baseline and post intervention assessments.
As reported in a previous publication from this sample,43 121 men completed the baseline assessment. Of these, 101 completed the post-intervention assessment, yielding an attrition rate of 16.6%. These 101 were included in all subsequent analyses.
Participants in the present study were primarily non-Hispanic White (43%) or Hispanic (38%) followed by Black (18%). Participants were an average of 60.3 years old (SD = 4.9), primarily married or partnered (78%), had an average of 14 years of formal education (SD = 3.3) and earned an average of $52,000 annually (SD = $41,000). The average time since treatment was 9.1 months (SD = 4.9), and the average time since diagnosis was 12.5 months (SD = 6.7).
Experimental condition
The 10-week Cognitive-Behavioral Stress Management (CBSM) intervention for Prostate Cancer46 was a modified version of a protocol originally designed by Antoni et al and used with other chronic illness populations (e.g., breast cancer, HIV and Chronic Fatigue Syndrome).47 CBSM groups were composed of 4–6 participants and met once each week for 2 hours, which included 90-minutes of didactic instruction and discussion and 30 minutes of relaxation training. The intervention was generally designed to buffer distress by providing participants with effective coping and stress-management techniques as well as with practical information regarding PCa and recovery. The 10-week time-frame was designed to allow for the delivery of a theory-guided and manualized comprehensive stress management intervention that targeted issues salient to this population through the delivery of relaxation exercises, as well as cognitive, behavioral and interpersonal skills to cope with illness-related disruption and other relevant stressors. Participants were encouraged to engage one another in discussion regarding their experience with cancer, and weekly between-session homework exercises were assigned to elaborate on session material. As discussed earlier, sexual dysfunction was a major area of emphasis. Other content areas included assertive communication, anger management, rational thought replacement, utilization of social support, doctor-patient communication and active coping. All CBSM groups were led by master's level clinical psychology students and/or Ph.D. level licensed clinical psychologists trained in the CBSM protocol, and were videotaped and reviewed to monitor treatment fidelity.
One-day seminar condition
Participants assigned to the control condition met once for 4 hours, and were provided with the same manual and instructed in the same stress management techniques as were participants in the experimental condition. Control participants were encouraged to practice stress management and relaxation techniques on a daily basis. Parallel to the experimental condition, groups consisted of 4–6 participants and were co-led by master's level clinical psychology students and/or Ph.D. level licensed clinical psychologists trained in the CBSM protocol.
Randomization procedure
Twenty-two cohorts ranging from 6 to 18 participants were recruited throughout the study period. Participants were assigned to the experimental or control conditions following one of three randomization procedures depending on the size of the recruited cohort, in order to assure that each intervention group consisted of at least 4 to 6 participants. In three cohorts consisting of greater than 12 participants, we conducted a 1:1 (1 experimental to 1 control) randomization procedure. A 2:1 (2 experimental to 1 control) randomization was conducted in cohorts consisting of six to 12 participants (3 cohorts). Finally, in the majority of our cohorts (14 cohorts), all participants were included in a group and the group randomly assigned to either the experimental or control condition by flipping a coin.
Measures
Health and sociodemographic measures
Demographics and clinical variables were assessed by interview. Because comorbid health problems have been shown to relate to sexual function in this population48 a modified version of the Charlson Comorbidities Index (CCI)49 was also included in the assessment battery. This version contained the original 19 categories of the Charlson, with the exception that the “any tumor” category was modified to ask only about non-skin, prostate, or bladder cancers (i.e., to avoid confounding with the diagnosis of PCa present in the sample).
Sexual functioning and concern
Sexual functioning was assessed using the sexual functioning subscale of the University of California, Los Angeles Prostate Cancer Index Composite (UCLA-PCI).50 This subscale asks participants to rate their sexual desire and ability over the past 4 weeks. Items assess sexual desire as well as erectile quality and frequency. Response items range from very poor (0) to very good (4), and are subsequently recoded to reflect an overall percentage of sexual functioning (i.e., 0–100%). The UCLA-PCI has been widely used in the prostate cancer literature51,52 and demonstrates adequate internal consistency (α = .81) in the present sample.
Concern about sexual functioning (CASF) was assessed using a 4-item measure that asked participants to rate their agreement with statements linking sexual function to masculine identity. These include "It’s important to me to fulfill my sexual role as a man" and "If a man isn’t satisfying his partner sexually, he can't possibly feel good about himself." The CASF is designed for use in men with cancer, and is based theoretically on the Concern About Appearance subscale of the Measure of Body Apperception (MBA) created by C. Carver and utilized in studies of women with breast cancer.53–54 Although the MBA was originally designed and tested in a population of women, the items used here have been modified in respect to gender, and we would expect that the questions utilized in the CASF have face validity for men. In the present sample, the CASF demonstrated acceptable internal consistency (α = .79).
Interpersonal sensitivity
Interpersonal sensitivity was assessed using the 47-item Inventory of Interpersonal Problems, Personality Disorder version (IIP-PD).8 The IIP-PD consists of five subscales (interpersonal ambivalence, interpersonal sensitivity, aggression, need for social approval and lack of sociability) culled from the original 127-item Inventory of Interpersonal Problems.55 The IIP-PD asks participants to rate the extent to which they agree or disagree to statements describing interpersonal problems. Response items are Strongly Agree (4), Agree (3), Neutral (2), Disagree (1) Strongly Disagree (0). As a unifactorial measure, the IIP-PD has demonstrated strong predictive validity in diagnosing DSM-IV Axis II pathology.9,56 In the present sample, the interpersonal sensitivity subscale demonstrated strong internal consistency (α = .81).
Design and statistics
The present study was a 2×2, randomized, repeated measures design with 2 levels of the intervention condition (experimental or control) and 2 time points (baseline and post-intervention).
Interpersonal sensitivity and baseline measures
Baseline correlations between interpersonal sensitivity and sexual functioning variables in this sample are presented elsewhere.43 Briefly, in this prior study from the same sample, interpersonal sensitivity was negatively associated with pre-intervention sexual function outcomes.
In the present study, bivariate correlation was used to test the hypothesis that interpersonal sensitivity was associated with a greater tendency to link sexual dysfunction to core masculine identity (i.e, at baseline).
Control variables
In order to minimize demographic confounds, baseline demographic, medical, and health measures were correlated with post intervention sexual functioning. These variables included age, time since diagnosis, time since treatment, use of medications (separate analyses were performed for use [Y/N] of antihypertensives, analgesics, blood glucose regulators, antidepressants, and sedatives/hypnotics), medical comorbidities, income, education and ethnicity (white, black, Hispanic). Only age (r= −.22, p < .05), medical comorbidities (r= −.25, p < .05) and use of sexual aids such as Viagra or vacuum pump in the past 4 weeks (dummy coded as yes/no; r = .20, p < .05) were significantly related to post-intervention sexual functioning, and were controlled for in the regression analyses described below.
Interpersonal sensitivity as a moderator of the intervention
Hierarchical multiple regression was used to determine the relationship between post intervention sexual functioning and intervention condition. We then tested the interaction of intervention condition and interpersonal sensitivity in predicting post intervention sexual functioning after adding relevant covariates. Moderation was tested as per guidelines described by G. Holmbeck.57 In this approach, all predictor variables were centered prior to analysis, and an intervention by interpersonal sensitivity interaction term was created using the centered data. After entering control variables, main effects for intervention and interpersonal sensitivity were entered, followed by their interaction. Following significance of the interaction term, two new variables describing high and low interpersonal sensitivity were created by subtracting or adding (respectively) one SD from the interpersonal sensitivity mean. Separate regression slopes were then computed for the effect of CBSM on post intervention sexual function for each of these two interpersonal sensitivity groups (i.e. high and low). These slopes were then evaluated individually for statistical significance.57
Data screening
Prior to centering data or analysis, we tested predictor and outcome variables for normality and for outliers (>3 SD from the mean). We then tested for multicolinearity among predictor variables in the moderated regression analyses.
All predictor and outcome variables met the assumption of normality as indicated by skewness < 1.5 and kurtosis < 2.0. No outliers were detected on any measure.
To test assumptions of regression, post-intervention sexual function was regressed on baseline sexual function, CBSM intervention status and interpersonal sensitivity (entered as a single block). Examination of the residual scatterplot suggested linearity and homoscedasticity (e.g., the points were clustered evenly along the 0 line in a roughly rectangular fashion). Multicollinearity was assessed using the Tolerance cut-off value of 0.1. All Tolerance values were >.60 (i.e., for baseline sexual function, the CBSM intervention, and interpersonal sensitivity before centering).
Results
Attrition analyses
As reported in a previous publication from this sample,43 121 men completed the baseline assessment. Of these, 101 completed the post-intervention assessment, yielding an attrition rate of 16.6%. Individuals who completed the post-intervention assessments did not differ from those who completed only the pre-intervention assessment on measures of income, age, time since diagnosis or treatment, education or sexual function (all p’s > .15).
Randomization analyses
At baseline, participants assigned to the experimental (CBSM) condition did not vary from those in the control condition in terms of education, income, baseline sexual function, time since diagnosis, time since radical prostatectomy, or baseline interpersonal sensitivity. Individuals in the control condition did report more medical comorbidity than did those in the experimental condition (Charlson Index = 1.7 vs. 1.0; t = 2.2, p < .05). However, this difference appeared to be driven by a single individual in the control condition with a Charlson score that was >3.5 SD from the mean. As described above, this variable was controlled for in all regression analyses. These data are presented in Table I.
Table I.
Baseline Characteristics by Experimental Condition
| Mean | SD | t | |||
|---|---|---|---|---|---|
| Exp (n=60) | Con (n=41) | Exp (n=60) | Con (n=41) | ||
| Interpersonal sensitivity | 31.1 | 29.5 | 6.9 | 6.4 | 1.2ns |
| Baseline sexual function | 26.1 | 19.2 | 22.5 | 15.6 | 1.7ns |
| Medical comorbidities | 1.0 | 1.7 | 1.5 | 1.7 | −2.2* |
| Age | 60.6 | 59.9 | 4.8 | 5.6 | .75ns |
| Years of education | 14.3 | 13.9 | 2.9 | 3.6 | .77ns |
| Months since diagnosis | 13.2 | 13.9 | 7.6 | 5.7 | −.56ns |
| Months since radical prostatectomy | 9.4 | 10.7 | 5.3 | 4.9 | −1.2ns |
| Income (thousands) | 53.7 | 54.3 | 42.0 | 40.0 | −.74ns |
= p < .05
Sample Characteristics
Participants in this sample had a mean modified CCI of 1.3 (SD = 1.7), with the majority reporting comorbid connective tissue disease (24%), followed by peripheral vascular disease (15%) and diabetes (10%). These scores are generally consistent with those reported in other studies of men with localized prostate cancer.58,59
Mean sexual function at baseline for the entire sample was 23.8% (SD = 20.6%). Regarding desire, 38.7% of participants rated their level of sexual desire as "very poor" or "poor," while 35% rated desire as "fair" to "good." Similarly, a majority (58.5%) of participants rated their ability to reach orgasm as "very poor" or "poor" while only 32.1% indicated "fair" or "good" orgasmic functioning. Eighty-eight percent of participants rated their ability to have an erection as "very poor" or "poor," while only 4.7% rated their ability as "good" or “very good.” Despite these reported decrements, only 25% of participants reported attempting to improve sexual function over the past four weeks via medication, implant or vacuum pump.
Interpersonal Sensitivity and Baseline Measures
Bivariate correlation analysis indicated that baseline interpersonal sensitivity was a significant correlate of concern about sexual function (r = .29, p < .05), such that individuals higher in interpersonal sensitivity were more likely to see sexual dysfunction as a threat to masculine identity.
Intervention Effects and Moderation by Interpersonal Sensitivity
In a hierarchical regression model controlling for baseline sexual functioning, age, medical comorbidities and use of sexual aids, CBSM group assignment was a significant predictor of post intervention sexual functioning (β = .14, p < .05; see Table II and Figure I). By way of comparison, those in the experimental condition made a 37.4% improvement in sexual functioning score over the 10-weeks, while those in the control condition improved by only 11.5%.
Table II.
Effect of CBSM on Sexual Functioning
| Step | Variable | β | p | R2 | R2Δ | F for R2Δ | p for R2Δ |
|---|---|---|---|---|---|---|---|
| 1 | Age | −0.01 | ns | .57 | .57 | 44.47 | <.01 |
| Comorbidities | −0.09 | ns | |||||
| Baseline sexual functioning | 0.73 | <.01 | |||||
| Use of sexual aids (Y/N) | 0.10 | ns | |||||
| 2 | CBSM group assignment | 0.15 | <.05 | .59 | .02 | 5.03 | <.05 |
F (5,97) = 34.39, p < .01.
Figure I.
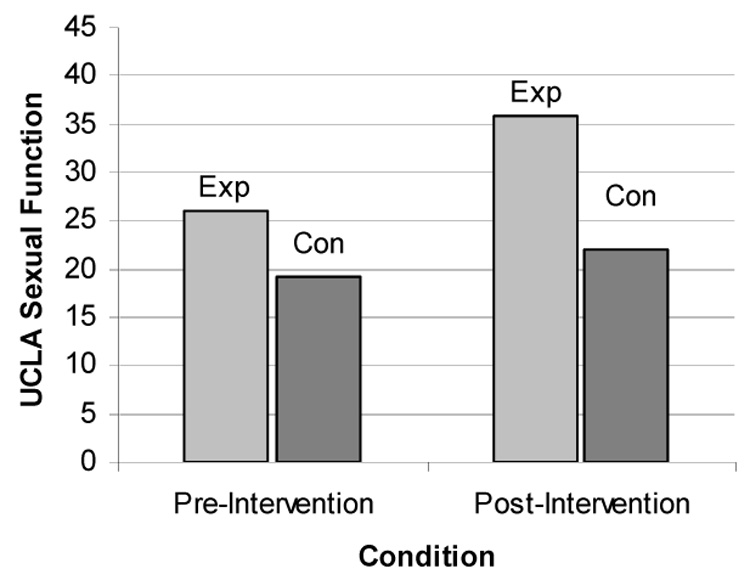
Effect of CBSM on Sexual Functioning
We next tested a moderated regression model in which personality dysfunction and CBSM group assignment were entered as main effects, followed by their interaction. The overall model accounted for 61% of the variance in post intervention sexual functioning (F [7,94] = 24.43, p < .001; see Table III). The interaction factor was significant (β = .19, p < .05) and accounted for an additional 2.3% of the variance in post intervention sexual functioning after control variables and the main effects of personality dysfunction and CBSM group assignment.
Table III.
Moderation of CBSM by Interpersonal Sensitivity
| Step | Variables | β | p | R2 | R2Δ | F for R2Δ | p for R2Δ |
|---|---|---|---|---|---|---|---|
| 1 | Age | 0.01 | ns | 0.59 | 0.59 | 34.80 | <.01 |
| Comorbidities | −0.07 | ns | |||||
| Baseline sexual functioning | 0.73 | <.01 | |||||
| Use of sexual aids (Y/N) | 0.09 | ns | |||||
| 2 | Interpersonal Sensitivity | 0.14 | <.05 | 0.62 | .03 | 4.17 | <.05 |
| CBSM group assignment | 0.14 | <.05 | |||||
| 3 | Interpersonal Sensitivity | 0.19 | <.05 | 0.64 | .02 | 6.04 | <.05 |
| X CBSM group assignment | |||||||
F (7,94) = 24.43, p < .01.
Post-hoc regression analyses indicated that for men higher in interpersonal sensitivity, those assigned to the CBSM intervention showed larger pre-post change in sexual functioning (Pre M = 19.4, SD = 17.4 ; Post M = 43.4, SD = 34.2) vs. controls (Pre M = 21.8, SD = 13.8; Post M = 22.4, SD = 17.7), β = .29, p < .01. For individuals with lower levels of personality dysfunction, the relationship between CBSM group assignment and post intervention sexual functioning was not significant (β = .03, p > .70), with no difference in pre-post changes between experimental (Pre M = 31.2, SD = 28.1; Post M = 33.6, SD = 32.2) and control (Pre M = 25.4, SD = 11.6; Post M = 25.2, SD = 15.0) groups. Therefore, while all participants improved slightly over time, participants with higher levels of interpersonal sensitivity appear to be particularly responsive to the effect of CBSM intervention. These data are presented visually in Figure II.
Figure II.
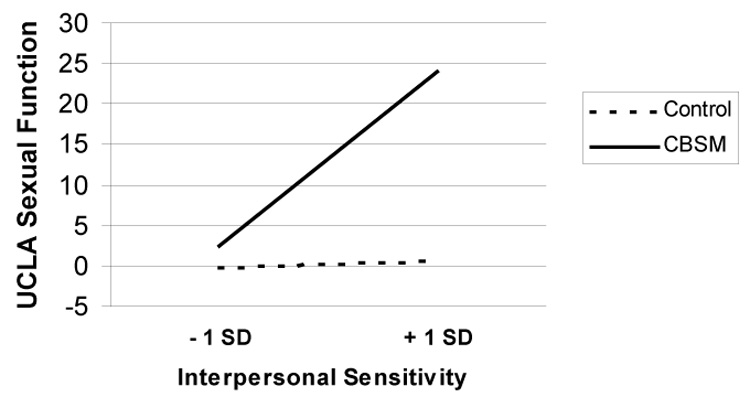
Change in Sexual Functioning by CBSM Assignment and Level of Interpersonal Sensitivity
Discussion
To our knowledge, this is the first study to investigate the role of interpersonal sensitivity in a group-based psychosocial intervention for men recovering from prostate cancer. Consistent with studies of personality traits in medical populations60 as well as our own work,43 we found that higher levels of interpersonal sensitivity at baseline were associated with a tendency to perceive sexual dysfunction as a threat to core masculinity. As hypothesized, the CBSM intervention was effective in promoting recovery of sexual functioning for all participants. However, consistent with some prior work33,42 we found that interpersonal sensitivity at baseline moderated the efficacy of the CBSM intervention, such that men beginning the study with higher levels of interpersonal sensitivity showed the greatest gains in sexual functioning after the intervention period.
Whereas the finding that individuals with interpersonal problems are more likely to interpret sexual dysfunction as a threat to their sense of masculinity is somewhat intuitive, our finding of enhanced intervention efficacy for these individuals requires some elaboration. It is plausible that individuals who are willing to report interpersonal sensitivity are demonstrating insight into the fact that some of their problems have interpersonal sources. They may have more room for improvement in key outcome variables, preventing a ceiling effect that may exist in comparison groups.33 Further, we found that that interpersonal sensitivity was positively associated with the CASF scale, suggesting that men with significant interpersonal sensitivity are more likely to see sexual dysfunction as threatening to a core sense of male identity. With sexual dysfunction, this identity becomes threatened, and an individual's coping resources may be strained or overwhelmed. This may lead them to avoid or deny issues relating to sexual ability and desire. For these men, a group setting with appropriate modeling from less dysfunctional participants and education regarding options for treatment would serve to (a) provide the practical information these participants were avoiding, (b) normalize feelings of anxiety surrounding a perceived loss of male status and (c) model appropriate partner communication regarding sexual dysfunction, thereby decreasing performance anxiety associated with sexual intimacy. The exposure to interpersonal situations in a controlled environment may also be corrective for interpersonally sensitive individuals, in that a group leader may be able to direct attention to their tendency to elicit negative reactions from other group members and challenge distorted interpretations of group interactions. By doing so, the therapist (and other group members) may serve to interrupt the “self-fulfilling prophecies” theorized to exist in these individuals13 and thereby improve their ability to effectively communicate needs and feelings. This effect may be particularly salient as it relates to sexual functioning, as improvement depends not only on physical changes but also on effective interpersonal and partner communication.61
Clearly, this study is preliminary and has limitations. Although we suspect that participants who were high in interpersonal sensitivity may have modeled the approaches of more functional members, we did not measure group process variables directly, and can therefore only speculate as to their importance. A more detailed assessment of group climate would have provided us with better information. Also, the fact that we did not assess the sexual partners of participants gave us only half the picture in terms of sexual activity and communication. Although several researchers have already moved in this direction,62,63 further work incorporating measures of personality dysfunction along with partner perceptions could help to elucidate these relationships. Since we did not perform mid-intervention assessments or monitor homework completion, we are unable to make statements regarding the necessary “dose” of CBSM to promote change in sexual function. Also, our use of the Charlson Index to measure medical comorbidities may not have been ideal given this measure’s intended use as a predictor of mortality after hospitalization. Finally, while our control condition was designed to provide participants with the same information as was given to those in the experimental condition, the difference in contact with other participants and clinicians (4 hours vs. 20 hours) is a threat to the validity of comparisons to the control group.
Despite these limitations we believe that this research is unique in several ways. First, this is one of the first reports that a group-based CBSM intervention can be used to effectively target sexual recovery in men treated for PCA. Although the mechanism of change is not clear, we can speculate that a combination of education in the use of sexual aids, training in effective communication and other stress management skills, and the normalizing environment of the group all played a role. Second, this work is the first to apply interpersonal theory constructs to the problem of medically induced sexual dysfunction. Interpersonal theory seems a particularly appropriate template for discussing these issues, given the interpersonal nature of sexual activity. We also believe that these data add to a growing literature supporting the “targeting” of psychosocial interventions such as CBSM towards individuals who are both at highest risk for negative outcome and the most likely to benefit from group treatment. In our study, these men were those highest in interpersonal sensitivity, a trait associated with lower levels of sexual quality of life that did not improve without intervention. Finally, while these data replicate other work demonstrating the detrimental influence of personality problems in medical settings, they also emphasize the potential applicability of group interventions in improving care for these individuals.
Future work could focus on interventions that blend group support with partner involvement, targeted at groups most likely to show benefit (i.e., those highest in interpersonal sensitivity or other negative baseline treatment indicators). Additional areas for research include determining the best timing for these interventions in the cancer treatment experience, illuminating the psychosocial and biobehavioral mechanisms that might explain these effects, and determining whether the effects might generalize to other treated cancer patients (e.g., women undergoing treatment for breast cancer) via similar or different mechanisms.
Acknowledgments
This study was supported by National Cancer Institute grant 1P50CA84944.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
For clarity, we note that the term “interpersonal sensitivity” is also used in communication and developmental literature to describe the ability to accurately perceive the needs, motives and mood states of others and to make correct social judgments based on non-verbal cues. This concept is distinct from our use of the term.
References
- 1.Berkman L. Social support, social networks, social cohesion and health. Social Work in Health Care. 2000;31:3–14. doi: 10.1300/J010v31n02_02. [DOI] [PubMed] [Google Scholar]
- 2.Tilden V, Galyen R. Cost and conflict: The darker side of social support. Western Journal of Nursing Research. 1987;9:9–18. doi: 10.1177/019394598700900103. [DOI] [PubMed] [Google Scholar]
- 3.Uchino B. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 4.Sandler I, Barrera M. Toward a multimethod approach to assessing the effects of social support. American Journal of Community Psychology. 1984;12:37–52. doi: 10.1007/BF00896927. [DOI] [PubMed] [Google Scholar]
- 5.DeLongis A, Holtzman S. Coping in context: The role of stress, social support, and personality in coping. Journal of Personality. 2005;73:1–24. doi: 10.1111/j.1467-6494.2005.00361.x. [DOI] [PubMed] [Google Scholar]
- 6.Dehle C, Landers J. You can’t always get what you want, but can you get what you need? Personality traits and social support in marriage. Journal of Social and Clinical Psychology. 2005;24:1051–1076. [Google Scholar]
- 7.Cutrona C, Hessling RM, Suhr JA. The influence of husband and wife personality on marital social support interactions. Personal Relationships. 1997;4:379–393. [Google Scholar]
- 8.Pilkonis P, Kim Y, Prioietti M, Barkham M. Scales for personality disorders developed from the inventory of interpersonal problems. Journal of Personality Disorders. 1996;10:355–369. [Google Scholar]
- 9.Stern B, Kim Y, Trull R, Scarpa A, Pilkonis P. Inventory of Interpersonal Problems personality disorder scales: Operating characteristics and confirmatory factor analysis in nonclinical samples. Journal of Personality Assessment. 2000;74:459–471. doi: 10.1207/S15327752JPA7403_9. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan HS. The interpersonal theory of psychiatry. New York (NY): Norton; 1953. [Google Scholar]
- 11.Kiesler DJ. Contemporary interpersonal theory and research: personality, psychopathology, and psychotherapy. New York (NY): John Wiley & Sons; 1996. [Google Scholar]
- 12.Leary T. Interpersonal diagnosis of personality; a functional theory and methodology for personality evaluation. Oxford (UK): Ronal Press; 1957. [Google Scholar]
- 13.Kiesler DJ. An interpersonal communication analysis of relationship in psychotherapy. Psychiatry: Journal for the Study of Interpersonal Processes. 1979;42:299–311. doi: 10.1080/00332747.1979.11024034. [DOI] [PubMed] [Google Scholar]
- 14.Wachtel P. Psychoanalysis and behavior therapy. New York (NY): Basic Books; 1977. [Google Scholar]
- 15.Pincus A. The interpersonal circumplex and the interpersonal theory: Perspectives on personality and its pathology. In: Strack S, Lorr M, editors. Differentiating Normal and Abnormal Personality. New York (NY): Springer; 1994. pp. 114–136. [Google Scholar]
- 16.Serovich J, Kimberly J, Mosack K, Lewis T. The role of family and friend social support in reducing emotional distress among HIV-positive women. AIDS Care. 2001;13:335–341. doi: 10.1080/09540120120043982. [DOI] [PubMed] [Google Scholar]
- 17.Newsom J, Schulz R. Social support as a mediator in the relation between functional status and quality of life in older adults. Psychology and Aging. 1996;11:34–44. doi: 10.1037/0882-7974.11.1.34. [DOI] [PubMed] [Google Scholar]
- 18.Reich J. The effects of Axis II disorders on the outcome of treatment of anxiety and unipolar depressive disorders: A review. Journal of Personality Disorders. 2003;17:387–405. doi: 10.1521/pedi.17.5.387.22972. [DOI] [PubMed] [Google Scholar]
- 19.Reich J, Vasile R. Effect of Personality Disorders on the Treatment Outcome of Axis I Conditions: An Update. The Journal of Nervous and Mental Disease. 1993;181:475–484. doi: 10.1097/00005053-199308000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Reich J, Green A. Effects of personality disorders on outcome of treatment. Journal of Nervous and Mental Disease. 1991;179:74–82. doi: 10.1097/00005053-199102000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Baer L, Jenike A. Personality disorders in obsessive compulsive disorder. Psychiatric Clinics of North America. 1992;15:803–812. [PubMed] [Google Scholar]
- 22.Marchland A, Goyer L, Dupuis G, Mainguy N. Personality disorders and the outcome of cognitive-behavioural treatment of panic disorder with agoraphobia. Canadian Journal of Behavioral Science. 1998;30:14–23. [Google Scholar]
- 23.Prudic J, Olfson M, Marcus S, Fuller R, Sackeim H. Effectiveness of electroconvulsive therapy in community settings. Biological Psychiatry. 2004;55:301–312. doi: 10.1016/j.biopsych.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 24.Faravelli C, Albanesi G. Agoraphobia with panic attacks: One year prospective follow-up. Comprehensive Psychiatry. 1987;28:481–487. doi: 10.1016/0010-440x(87)90013-7. [DOI] [PubMed] [Google Scholar]
- 25.Chambless DL, Renneberg B, Goldstein AJ, Gracely E. MCMI-diagnosed personality disorders among agoraphobic outpatients: Prevalence and relationship to severity and treatment outcome. Journal of Anxiety Disorders. 1992;6:193–212. [Google Scholar]
- 26.Kivlighan D, Angelone E. Interpersonal problems: Variables influencing participant's perception of group climate. Journal of Counseling Psychology. 1992;39:468–472. [Google Scholar]
- 27.MacNair-Semands R. Predicting attendance and expectations for group therapy. Group Dynamics: Theory, Research, and Practice. 2002;6:219–228. [Google Scholar]
- 28.Paivio S, Bahr L. Interpersonal problems, working alliance, and outcome in short-term psychotherapy. Psychotherapy Research. 1998;8:392–407. [Google Scholar]
- 29.Muran J, Segal Z, Samstag L, Crawford C. Patient pretreatment interpersonal problems and therapeutic alliance in short-term cognitive therapy. Journal of Consulting and Clinical Psychology. 1994;62:185–190. doi: 10.1037//0022-006x.62.1.185. [DOI] [PubMed] [Google Scholar]
- 30.MacNair-Semands R, Lese K. Interpersonal problems in the perception of therapeutic factors in group therapy. Small Group Research. 2000;31:158–174. [Google Scholar]
- 31.Schauenburg H, Kuda M, Sammet I, Strack M. The influence of interpersonal problems and symptom severity on the duration and outcome of short-term psychodynamic psychotherapy. Psychotherapy Research. 2000;10:133–146. doi: 10.1080/713663670. [DOI] [PubMed] [Google Scholar]
- 32.Rice A. Interpersonal problems of persons with personality disorders and group outcomes. International Journal of Group Psychotherapy. 2003;53:155–175. doi: 10.1521/ijgp.53.2.155.42813. [DOI] [PubMed] [Google Scholar]
- 33.Mohr D, Beutler L, Engle D, et al. Identification of patients at risk for nonresponse and negative outcome in psychotherapy. Journal of Consulting and Clinical Psychology. 1990;58:622–628. doi: 10.1037//0022-006x.58.5.622. [DOI] [PubMed] [Google Scholar]
- 34.American Cancer Society. Cancer Facts & Figures 2006. Atlanta (GA): American Cancer Society; 2006. [Google Scholar]
- 35.Schover L, Fouladi R, Warneke C, et al. Defining sexual outcomes after treatment for localized prostate carcinoma. Cancer. 2002;95:1773–1785. doi: 10.1002/cncr.10848. [DOI] [PubMed] [Google Scholar]
- 36.Matthew A, Goldman A, Trachtenberg J, Robinson J, Horsburgh S, Currie K, Ritvo P. Sexual dysfunction after radical prostatectomy: Prevalence, treatments, restricted use of treatments and distress. Journal of Urology. 2005;174:2105–2110. doi: 10.1097/01.ju.0000181206.16447.e2. [DOI] [PubMed] [Google Scholar]
- 37.Hu J, Elkin E, Pasta D, et al. Predicting quality of life after radical prostatectomy: Results from CaPSURE. Journal of Urology. 2004;171:703–708. doi: 10.1097/01.ju.0000107964.61300.f6. [DOI] [PubMed] [Google Scholar]
- 38.Penedo FJ, Molton IR, Dahn J, Shen JB, Kinsinger DP, Traeger L, Siegel S. A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: Development of stress management skills improves quality of life and benefit finding. Annals of Behavioral Medicine. 2006;31:261–270. doi: 10.1207/s15324796abm3103_8. [DOI] [PubMed] [Google Scholar]
- 39.Lepore S, Helgeson V, Eton D, Schulz R. Improving quality of life in men with prostate cancer: A randomized controlled trial of group education interventions. Health Psychology. 2003;22:443–452. doi: 10.1037/0278-6133.22.5.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ptacek JT, Pierce GR, Ptacek JJ. The social context of coping with prostate cancer. Journal of Psychosocial Oncology. 2002;20:61–80. doi: 10.1300/J077v25n02_03. [DOI] [PubMed] [Google Scholar]
- 41.Zakowski SG, Harris C, Krueger N, Laubmeier KK, Garrett S, Flanigan R, et al. Social barriers to emotional expression and their relations to distress in male and female cancer patients. British Journal of Health Psychology. 2003;8:271–286. doi: 10.1348/135910703322370851. [DOI] [PubMed] [Google Scholar]
- 42.Helgeson V, Eton D, Lepore S. Moderators of the benefits of psychoeducational interventions for men with prostate cancer. Health Psychology. 2006;25:348–354. doi: 10.1037/0278-6133.25.3.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Siegel S, Molton I, Penedo F, Llabre M, Kinsinger D, et al. Interpersonal sensitivity, partner support, patient-physician communication and sexual functioning in men recovering from prostate carcinoma. Journal of Personality Assessment, in press. doi: 10.1080/00223890701629847. (in press) [DOI] [PubMed] [Google Scholar]
- 44.Folstein M, Folstein S, McHugh P. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 45.First M, Spitzer M, Gibbon M, Williams J. Structured clinical interview for the DSM-IV axis I disorders. New York (NY): Biometrics Research, New York State Psychiatry Research; 1996. [Google Scholar]
- 46.Penedo F, Dahn J, Antoni M, Schneiderman N. Cognitive-Behavioral Stress Management for Men Recovering from Prostate Cancer. 2002 doi: 10.1002/cncr.11894. Unpublished treatment manual. [DOI] [PubMed] [Google Scholar]
- 47.Antoni M, Baggett L, Ironson G, et al. Cognitive-behavioral stress management buffers distress responses and immunologic changes following notification of HIV-1 seropositivity. Journal of Consulting and Clinical Psychology. 1991;5:906–915. doi: 10.1037//0022-006x.59.6.906. [DOI] [PubMed] [Google Scholar]
- 48.Dahn J, Penedo F, Gonzalez J, Esquiabro M, Antoni M, Roos B, Schneiderman N. Sexual functioning and quality of life after prostate cancer treatment: Considering sexual desire. Urology. 2004;63:273–277. doi: 10.1016/j.urology.2003.09.048. [DOI] [PubMed] [Google Scholar]
- 49.Charlson M, Pompei P, Ales K, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Disease. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 50.Litwin M, Hays R, Fink A, et al. The UCLA prostate cancer index: Development, reliability, and validity of a health-related quality of life measure. Medical Care. 1998;36:1002–1012. doi: 10.1097/00005650-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 51.Ishihara M, Suzuki H, Akakura K, Komiya A, Imamoto T, Tobe T, Ichikawa T. Baseline health-related quality of life in the management of prostate cancer. International Journal of Urology. 2006;13:920–925. doi: 10.1111/j.1442-2042.2006.01441.x. [DOI] [PubMed] [Google Scholar]
- 52.Karakiewicz P, Kattan M, Tanquay S, Elhilali M, Bazinet M, Scardino P, Aprikan A. Cross-cultural validation of the UCLA prostate cancer index. Urology. 2003;61:302–307. doi: 10.1016/s0090-4295(02)02245-8. [DOI] [PubMed] [Google Scholar]
- 53.Carver C, Pozo-Kaderman C, Price A, Noriega V, Harris S, et al. Concern about aspects of body image and adjustment to early stage breast cancer. Psychosomatic Medicine. 1998;60:168–174. doi: 10.1097/00006842-199803000-00010. [DOI] [PubMed] [Google Scholar]
- 54.Petronis V, Carver C, Antoni M, Weiss S. Investment in body image and psychosocial well-being among women treated for early stage breast cancer: Partial replication and extension. Psychology and Health. 2002;18:1–13. [Google Scholar]
- 55.Horowitz L, Rosenberg S, Baer B, Ureno G, Villasenor V. Inventory of interpersonal problems: Psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology. 1998;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- 56.Kim Y, Pilkonis P, Barkham M. Confirmatory factor analysis of the personality disorder subscales from the Inventory of Interpersonal Problems. Journal of Personality Assessment. 1997;69:284–296. doi: 10.1207/s15327752jpa6902_3. [DOI] [PubMed] [Google Scholar]
- 57.Holmbeck G. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- 58.Sweat S, Bergstalh E, Slezak J, Blute M, Zincke H. Competing risk analysis after radical prostatectomy for clinically nonmetastatic prostate adenocarcinoma according to clinical Gleason score and patient age. Journal of Urology. 2002;168:525–529. [PubMed] [Google Scholar]
- 59.Froehner M, Kock R, Litz R, Oehlschlaeger S, Wirth M. Which conditions contributing to the Charlson score predict survival after radical prostatectomy? Journal of Urology. 2004;171:697–699. doi: 10.1097/01.ju.0000108138.36333.09. [DOI] [PubMed] [Google Scholar]
- 60.Taylor M, Deary J, Frier M, Gold A. Psychosocial factors and diabetes-related outcomes following diagnosis of Type 1 diabetes in adults: The Edinburgh Prospective Diabetes Study. Diabetic Medicine. 2003;20:135–146. doi: 10.1046/j.1464-5491.2003.00887.x. [DOI] [PubMed] [Google Scholar]
- 61.Juraskova I, Butow P, Robertson R, Sharpe L, McLeod C, Hacker N. Post-treatment sexual adjustment following cervical and endometrial cancer: A qualitative insight. Psycho-Oncology. 2003;12:267–279. doi: 10.1002/pon.639. [DOI] [PubMed] [Google Scholar]
- 62.Soloway C, Soloway M, Kim S, Kava B. Sexual, psychological and dyadic qualities of the prostate cancer ‘couple’. British Journal of Urology International. 2005;95:780–785. doi: 10.1111/j.1464-410X.2005.05400.x. [DOI] [PubMed] [Google Scholar]
- 63.Manne S, Babb J, Pinover W, Horowitz E, Ebbert J. Psychoeducational group intervention for wives of men with prostate cancer. Psycho-Oncology. 2004;13:37–46. doi: 10.1002/pon.724. [DOI] [PubMed] [Google Scholar]


