Abstract
Methamphetamine/amphetamine (MA)-related morbidity and mortality has been increasing in the United States. MA use is associated with high-risk sexual behavior and syringe-sharing practices. Homeless and marginalized housed persons (H/M) have high rates of substance use and mental health disorders. Little is known about trends of MA use among the H/M. The objective of this study was to quantify increases in MA use among H/M in San Francisco and to determine which demographic and behavioral subgroups have experienced the greatest increases in MA use. We conducted serial cross-sectional population-based studies in three waves: 1996–1997, 1999–2000, and 2003 and studied 2,348 H/M recruited at shelters and lunch lines. The main outcome was self-reported current (30-day) MA use. We found a tripling of current MA use among H/M persons from 1996 to 2003, with a sevenfold increase in smoked MA use. MA use doubled to tripled in most demographic and behavioral subgroups, whereas it quadrupled in those under age 35, and there was a fivefold increase among HIV-infected persons. The increase in MA use among H/M places a vulnerable population at additional increased risk for HIV infection and MA-use related morbidity and mortality. Among HIV-infected H/M, the increase in MA use has important public health implications for the development and secondary transmission of drug-resistant HIV caused by synergistic neurocognitive decline, poor adherence to HIV medications, and increased sexual risk behavior. Clinicians caring for H/M persons should inquire about MA use, refer interested MA users to MA dependence treatment programs and provide targeted HIV sexual risk reduction counseling. For HIV-infected H/M MA users, clinicians should closely monitor adherence to HIV or other chronic medications, to avoid unnecessary morbidity and mortality. Further research is needed to elucidate the most effective prevention and treatment for MA use and dependence among the H/M.
Keywords: Methamphetamine, Amphetamine, Speed, Homeless, Marginally housed, HIV/AIDS
BACKGROUND
Increasing methamphetamine and amphetamine (MA) use-related morbidity and mortality in the United States1 has been widely reported. MA use was first reported in Hawaii and the Western part of the United States where use remains most prevalent; however, MA use has become increasingly prevalent in the Midwest and is spreading eastward.2 Trends have been reported by a variety of sources. From 1991 to 1994, MA-related emergency department (ED) visits and MA-related deaths tripled3 and MA-related ED visits increased from 1995 to 2002 by 54%.4 The number of drug treatment admissions for primary MA use increased almost sixfold from 1993 to 2003.5 Similar increases in the number of MA-related drug treatment admissions have been reported in California from 1992 to 2002.6 Population-based studies of MA are few. Two recent studies reported that 1.4%7 to 2.8%8 used MA in the past year. However, there are no population-based studies reporting on the trends in the prevalence of MA use during the time period from 1991 to present during which MA use-related morbidity and mortality have increased.
MA use is associated with both risky sexual behavior and syringe-sharing practices. MA use is associated with unprotected anal intercourse (UAI),9–11 UAI with HIV-positive or unknown serostatus partners,11–14 increased number of sexual partners,10,11,14,15 sexual disinhibition or impulsivity,9,16,17 sexually transmitted disease (STD) incidence,18,19 and HIV seroconversion20 in MSM. Among heterosexual non-injection drug users, MA use is associated with increased sexual partners, less condom use than non-MA users, sex work, and self-reported history of STDs.21 MA use is associated with receptive syringe sharing and sharing of syringes with multiple partners among IDU.21–23
The homeless and marginally housed (H/M) are a vulnerable population at risk for increased morbidity and mortality.24–27 In particular, H/M have high rates of substance use and mental health disorders28 and may therefore be especially vulnerable to MA use.29 High prevalence of MA use among IDU,9,30–32 MSM33,34 and street youth35 have been reported; however, there have been no population-based reports of trends in MA use in H/M persons.
The goals of this analysis are to describe the recent trends in MA use observed in a population-based study of H/M persons and to determine which demographic and behavioral subgroups of the H/M have experienced the sharpest increases in MA use.
METHODS
Sampling Design
We conducted three waves of cross-sectional studies (1996–1997, 1999–2000, 2003) of adults (aged 18 and older) at homeless service providers in San Francisco, designed to obtain replicable, probability-based, representative samples of the urban indigent.36 The first two waves were conducted at shelters, free meal programs, and single-room occupancy (SRO) hotels, using a multistage cluster sampling with stratification as previously described.37,38 In the third wave, the sampling strategy at shelters and free meal programs remained the same; however, we oversampled non-profit, publicly subsidized SROs with disability as an entry criterion to recruit more HIV-infected individuals for a cohort study. Seventy-one venues were visited, including 13 shelters, eight free meal programs, and 50 SRO hotels. Eligible adults (age 18 and older) completed a structured interview, HIV antibody testing and counseling, and received $10–$20 for participating. All protocols were approved by the Committee on Human Research at University of California, San Francisco.
We included those observations in the current analysis from venues that were visited in at least two out of three waves to ensure consistency across the waves. We excluded observations from SRO hotels because of the oversampling of HIV-infected individuals in the third wave. The resulting sample included 13 shelters and eight free meal programs.
Variables
Sex and Sexual Orientation
We divided the sample into three groups (women, men who identified themselves as heterosexual, and men who identified themselves as ever having sex with men (MSM)). Participants were asked to describe their sexual behavior as straight behavior only, mostly straight behavior, bisexual behavior, mostly gay behavior, or gay behavior only. MSM were defined as having male gender at birth and reporting any behavior other than straight behavior.
Housing Status
We divided the sample into three groups based on self-reported 12-month residential history: literally homeless, marginally housed, and “other housing status.” Literally homeless was defined as reporting spending any night in the prior year living in a shelter, on streets, in a squat, vehicle, park or any other place not meant for sleeping. Marginally housed was defined as reporting living in a single room occupancy hotel or apartment (SRO), board and care apartment and no nights on street or in shelter in the prior year. “Other housing status” individuals did not meet criteria for literally homeless or marginally housed and reported living in one’s own apartment or house, with friends, in jail or prison, in a hospital or a residential drug or alcohol treatment facility in the prior year.
MA Use
In the 1996–1997 wave, participants were asked about amphetamine (“uppers”, “speed”, or “crank”) and methamphetamine (“crystal” or “ice”) together. In the 1999–2000 wave, participants were asked about methamphetamine use, defined as “crystal”, “speed”, “crank”, “glass”, or “ice”. In the 2003 wave, participants were asked about methamphetamine or “speed” use. For this analysis, an affirmative response to any of these terms constituted MA use.
Composite Other Substance Use Variable
We developed a hierarchical composite variable to categorize the type of other substances used by respondents reporting any MA use. Injection drug use (IDU) was defined as injecting heroin, crack, or cocaine. Non-injection drug use (NIDU) was defined as reporting heroin, powder cocaine or crack cocaine use, but not IDU. Heavy alcohol consumption was defined as typically drinking five or more drinks/occasion for men and four or more drinks/occasion for women, and no IDU or NIDU. The last category, no other drug use, was composed of those individuals who did not report any non-MA IDU, NIDU, or heavy alcohol consumption.
Analysis
We report proportions reporting MA use in the prior 30 days, overall and by route of administration (injecting, snorting, smoking), and within demographic subgroups (race, sex/sexual orientation, age, literal homelessness) and behavioral subgroups (other substance use, number of sexual partners, sex in exchange for money or drugs) and by HIV status. We conducted the Mantel–Haenszel Chi-square test for linear trend39 to examine trends, overall and within the subgroups, over the three study waves in this serial-cross sectional study.
The trends (shown in Table 1) we report are statistically significant (p < 0.05) unless otherwise noted. For comparison purposes, we also examined trends in the use of other substances by study wave. In addition, we conducted logistic regression analyses to determine whether trends in MA use were explained by temporal trends in other drug use or in previously observed trends in the population such as increasing age and duration of homelessness.38 We conducted logistic regressions with MA use as the outcome variable, study year as the predictor variable, and demographic and drug use variables as potential confounders, and report the unadjusted and adjusted odds ratios.
TABLE 1.
MA use in the homeless and marginally housed in San Francisco in the past month; by route of administration and by demographic and behavioral subgroups
| Characteristic | Wave 1 n/total (%) | Wave 2 n/total (%) | Wave 3 n/total (%) | P value for trenda | Wave 3/Wave 1 ratio |
|---|---|---|---|---|---|
| MA Use by Route of Administration | |||||
| All routes | 66/1152 (5.7) | 62/678 (9.1) | 78/518 (15.1) | <0.001 | 2.6 |
| Snorted /Inhaled | 23/1152 (2.0) | 23/672 (3.4) | 23/518 (4.4) | 0.004 | 2.2 |
| Smoked | 12/1152 (1.0) | 26/672 (3.9) | 37/518 (7.1) | <0.001 | 6.9 |
| Injected | 45/1152 (3.9) | 41/672 (6.1) | 48/518 (9.3) | <0.001 | 2.4 |
| Any MA use by Demographic Subgroup | |||||
| Age | |||||
| ≤34 | 22/251 (8.8) | 17/106 (16.1) | 32/97 (33.0) | <0.001 | 3.8 |
| 35–49 | 35/662 (5.3) | 39/423 (9.2) | 35/261 (13.4) | <0.001 | 2.5 |
| ≥50 | 9/237 (3.8) | 5/14 (3.6) | 11/159 (6.9) | 0.17 | 1.8 |
| Sex/Sexual Orientation | |||||
| Female | 8/245 (3.3) | 6/171 (3.5) | 9/100 (9.0) | 0.04 | 2.8 |
| Male, not MSM | 30/681 (4.4) | 26/376 (6.9) | 32/284 (11.3) | 0.001 | 2.6 |
| MSM | 27/220 (12.3) | 30/128 (23.4) | 37/134 (27.6) | 0.002 | 2.3 |
| Race | |||||
| Caucasian | 35/415 (8.4) | 35/232 (15.1) | 42/175 (24.0) | <0.001 | 2.9 |
| African-American | 15/563 (2.7) | 16/347 (4.6) | 12/221 (5.4) | 0.05 | 2.0 |
| Other | 16/171 (9.4) | 10/97 (10.3) | 24/119 (20.2) | 0.009 | 2.2 |
| HIV status | |||||
| Negative | 62/1045 (5.9) | 47/591 (8.0) | 65/457(14.2) | <0.001 | 2.4 |
| Positive | 4/92 (4.4) | 14/81 (17.3) | 13/60 (21.7) | 0.0013 | 5.0 |
| Housing Status b | |||||
| Other Housing Status | 5/76 (6.6) | 5/37 (13.5) | 2/36 (5.6) | 0.936 | 0.9 |
| Marginally Housed | 5/108 (4.6) | 2/57 (3.5) | 3/35 (8.6) | 0.484 | 1.9 |
| Literally Homeless | 56/968 (5.8) | 55/584 (9.4) | 73/447 (16.3) | <0.001 | 2.8 |
| Literally Homeless >1 year | |||||
| No | 22/429 (5.1) | 13/188 (6.9) | 15/127 (11.8) | 0.03 | 2.3 |
| Yes | 44/717 (6.1) | 48/479 (10.0) | 62/388 (16.0) | <0.001 | 2.6 |
| Any MA use by Behavioral Subgroup | |||||
| Other Substance Use Past Month | |||||
| Injection drug use c | 29/110 (26.4) | 28/86 (32.6) | 28/64 (43.8) | 0.02 | 1.7 |
| Non-injection drug used | 11/276 (4.0) | 10/197 (5.1) | 20/131 (15.3) | 0.001 | 3.8 |
| Heavy drinking e | 7/173 (4.1) | 4/92 (4.4) | 12/78 (15.4) | 0.003 | 3.8 |
| No other drug use | 19/593 (3.2) | 20/303 (6.6) | 18/245 (7.4) | 0.006 | 2.3 |
| Sex Partners in Past Year | |||||
| None | 8/288 (2.8) | – | 7/126 (5.6) | 0.16 | 2.0 |
| 1–2 | 25/469 (5.3) | – | 18/158 (11.4) | 0.009 | 2.1 |
| 3 or more | 30/386 (7.8) | – | 53/227 (23.4) | <0.001 | 3.0 |
| Sex Exchange in Past Year | |||||
| No | 49/1036 (4.7) | – | 58/436 (13.3) | <0.001 | 2.8 |
| Yes | 13/99 (13.1) | – | 18/60 (30.0) | 0.01 | 2.3 |
a SAS Mantel–Haenszel Chi-square for Trend
b Literally homeless defined as living in a shelter, on streets, in a squat, vehicle, park or any other place not meant for sleeping at least one night in the prior year. Marginally housed was defined as living in a single room occupancy hotel or apartment (SRO), board and care apartment and no nights on street or in shelter. “Other housing status” individuals did not meet criteria for literally homeless or marginally housed and reported living in one’s own apartment or house, with friends, in jail or prison, in a hospital or a residential drug or alcohol treatment facility in the prior year.
cHeroin, crack, cocaine or any injection drugs
dHeroin, crack, cocaine but no injection
e≥5 drinks/occasion for men, ≥4 drinks/occasion for women but no other drugs
RESULTS
Overall, we conducted 2,553 interviews at the 10 venues that were sampled in at least two of the three waves in the time period from 1996–2003. We excluded 39 observations that were missing MA use data and 166 interviews for persons seen more than once per study wave, leaving a total of 2,348 observations for this analysis.
Sample Characteristics
The sample was predominantly male (78%), included a plurality of African Americans (48%), was middle-aged (median age 42.5,) and were mostly literally homeless (85%). Current (past 30 days) alcohol and substance use was high: 29% drank alcohol heavily, 14% injected drugs, 32% used crack cocaine, and 9% used MA.
Overall MA Trends and Trends by Route of Administration
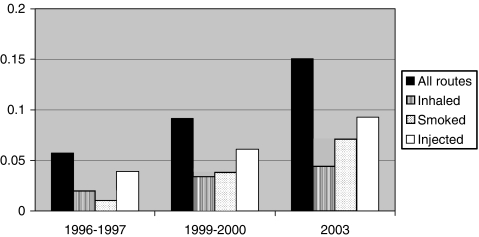
The number of respondents who reported any MA use almost tripled from 5.7% in 1996–1997 to 15.1% in 2003 (Table 1, Figure 1). Injection was the most commonly reported route of MA administration, ranging from 3.9% in 1996–1997 to 9.3% in 2003. The proportions of respondents who reported snorting and injecting MA each approximately doubled, and the proportion of respondents who reported smoking MA increased sevenfold from 1% in 1996–1997 to 7.1% in 2003. The median number of days of MA use in the prior month was 2 (IQR 1–5) in 1996–1997 and 3 (IQR 1–7) in 2003 (p value .62).
FIGURE 1.
Proportion of homeless and marginally housed adults reporting MA use in the prior 30 days, overall and by route of administration, 1996–2003.
Trends in Other Substances
We examined trends in the use of other drugs and heavy alcohol use to determine whether there was a concomitant decrease in the use of these substances. From 1996–1997 to 2003, the proportion that reported heroin use in the prior month increased from 9.3% to 11.6% (p = .08); crack cocaine use increased from 29.5% to 32.6% (p = .06); and powder cocaine use increased from 4.0% to 6.8% (p = .02) (data not shown). Stable proportions of the sample, 29.6% and 27.8% (p = .56), reported heavy drinking in the 1996–1997 and 2003 samples respectively (data not shown.)
MA Trends by Demographic Characteristic
Current MA use was highest in the youngest age group, with 8.8% of those under age 35 reporting current MA use in the 1996–1997 wave. Compared to older age groups, MA use in those under age 35 increased the most, with MA use quadrupling to 33% in 2003. A greater proportion of MSM (12.3%) reported current MA use than women (3.3%) and heterosexual men (4.4%) in the first wave; MA use more than doubled in each of these groups. Among Caucasians, the proportion reporting MA use tripled from 8.4% to 24.0%, whereas among African Americans the proportion reporting MA use doubled from 2.7% to 5.4%. Among literally homeless respondents, there was a threefold increase in the proportion reporting MA use (Table 1).
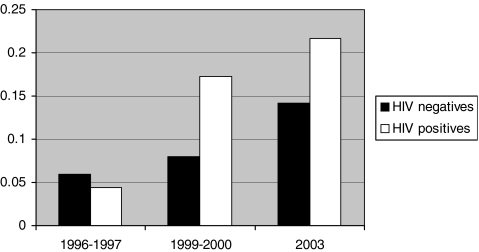
MA Trends among HIV-infected Respondents
The proportion of HIV-infected respondents reporting MA use increased fivefold from 4.4% to 21.7%; this was the greatest overall increase in MA use of any of the subgroups examined (Table 1, Figure 2).
FIGURE 2.
Proportion of HIV-uninfected and HIV-infected homeless and marginally housed adults reporting MA use in the prior 30 days, 1996–2003.
MA Use among Users of Other Substances
Among IDU, the proportion reporting MA use in the 1996–1997 wave was 26.4%, whereas it was 4% in NIDU and those who reported heavy alcohol consumption. The proportion of IDU who reported MA use doubled over the three waves, whereas the proportion reporting MA use among NIDU and heavy drinkers quadrupled over the three waves. MA use doubled in those reporting no other substance use.
MA Use and Sexual Risk Behavior
The proportion reporting MA use doubled from 1996 to 2003 among those reporting one to two sexual partners in the past year and tripled among respondents reporting three or more sexual partners in the past year. The increase in MA use in those who reported no sexual partners was not statistically significant.
MA Trends Adjusted for Substance Use and Demographic Trends
In logistic regression analyses of the trends in MA use, the trends persisted after adjustment for age, sex/sexual orientation, race/ethnicity, duration homeless, heavy alcohol consumption, heroin use, powder cocaine use, and crack cocaine use. The odds ratio of MA use for each successive calendar year compared to the prior year were 1.19 (95% CI 1.13–1.25) in the unadjusted model, and the odds ratio decreased only slightly 1.17 (95% CI 1.11–1.25) in the model adjusted for the potential confounders listed above.
DISCUSSION
We found a tripling in the proportion of persons reporting MA use from 1996 to 2003 in a population-based sample of H/M adults in San Francisco. The route of MA administration that had the greatest increase was smoking. We found increases in MA use (by all routes of administration) in almost all demographic and behavioral subgroups, with the greatest increases in HIV-infected respondents, young adults under age 35, non-injection drug users, heavy drinkers, and those reporting three or more sex partners in the past year. The median days of MA use reported was low and did not change significantly, suggesting that a greater proportion of H/M is using MA but that most are not MA dependent. The increase in MA use was not offset by decreases in the use of other drugs, or other temporal trends in the population. Although previous studies have shown increases in MA use in MSM and in IDU, this is the first study to quantify increases in MA use in a population-based sample of H/M persons.
We note several precautions in interpreting these findings. First, our results from a population of H/M individuals may not be generalizeable to other populations. However, the overall trends we observed are consistent with trends in drug treatment and ED admissions.3–5,29 Second, we relied on self-report of MA use, but we have no reason to suspect that the proportion overreporting MA use would systematically increase over time. Third, the terms used for MA on the study instruments changed over time; however, the definition became progressively narrower over the study waves, and therefore most likely led to an underestimate in the increase in MA use. Fourth, we did not collect dependency scale or other detailed data about patterns and severity of MA use. Last, the study design was a series of cross-sectional surveys. Although increasing proportions of HIV-infected individuals and persons with multiple sex partners reported MA use, we are unable to determine whether increased MA use resulted in increased sexual risk behavior and HIV infection or whether those already infected with HIV or with higher numbers of sex partners became more likely to use MA.
Despite these limitations, our findings have significant health implications for H/M persons, a vulnerable population at risk for increased morbidity and mortality.24–27 MA use fuels impulsive sexual risk behavior and behavioral disinhibition.9–17,20,23 The sharp increases in all demographic and behavioral subgroups, but particularly among the young and the sexually active, place already vulnerable H/M persons at further increased risk for sexual acquisition of HIV infection20 and drug-resistant HIV.40 In addition, H/M persons using MA are at risk for long-term adverse health sequelae of MA use: including cardiovascular,41,42 oral health complications,43–45 as well as increased risk of traumatic injuries46 and violent death.41 MA use also adds additional risk of neurocognitive impairment, depression, dementia, and psychosis10,41 to those in a population with already high levels of psychiatric morbidity and substance use disorders.24–27 We suggest clinicians caring for H/M individuals inquire specifically about MA use and MA use in association with sex during clinic visits and emphasize HIV sexual risk reduction counseling messages for H/M individuals reporting MA use with sex. Clinicians and service providers in the Northeast should be particularly alert to possible increases in MA use in the H/M population.
HIV-infected persons were the demographic subgroup with the highest overall (fivefold) increase in MA use. Increases in MA use among already HIV-infected H/M has important public health consequences such as the development of drug-resistant HIV because of the possible synergistic risk of neurocognitive decline47 and poor adherence to HIV medications,48 and increased sexual risk behavior and secondary sexual transmission of drug-resistance HIV.40 Clinicians should closely monitor HIV-infected H/M MA users for adherence to HIV and other chronic medications and should provide interventions such as pillboxes or pharmacy support programs to improve adherence to HIV and other chronic medications and avoid unnecessary morbidity and mortality.
MA users who seek treatment for MA dependence have been shown to reduce MA use and sexual risk behaviors through the Matrix Model, an outpatient stimulant dependence treatment program.49–52 Health care providers should be aware of MA dependence treatment options in their communities and refer interested MA users.
However, the Matrix Model is an intensive, 16-week cognitive behavioral psychotherapy intervention that may not be successful in the H/M population. Further research is needed to elucidate the most effective prevention and treatment interventions for MA use and dependence as well as reduction of sexual risk behaviors among the H/M. Attention should be focused on adapting successful MA dependence treatment interventions for this vulnerable population with unique needs.
Acknowledgment
MD-D is supported by T-32 MH19105. DRB supported by NIH K-24 AA015287. JH supported by NIH K01 DA023365. The research was supported by NIH R01 MH54907. The funding agencies had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Financial Disclosures None of the authors report any financial relationships or other conflicts of interest.
Footnotes
Das-Douglas and Bangsberg are with the Department of Medicine, Division of Infectious Diseases, University of California, San Francisco, CA, USA; Das-Douglas, Bangsberg, and Hahn are with the Epidemiology and Prevention Interventions Center, Department of Medicine, San Francisco General Hospital, University of California, San Francisco, CA, USA; Das-Douglas and Bangsberg are with the Center for AIDS Prevention Studies, University of California, San Francisco, CA, USA; Colfax is with the Epidemiology Section, AIDS Office, San Francisco Department of Public Health, San Francisco, CA, USA; Moss is with the Epidemiology and Biostatistics, University of California, San Francisco, USA.
References
- 1.Methamphetamine use dates to post-WWII era. Drug little-known risk factor in early AIDS days. AIDS Alert. 2002;17(10):125–127. [PubMed]
- 2.SAMHSA. Methamphetamine Use, Abuse, and Dependence: 2002, 2003, and 2004. Washington D.C.: SAMSHA; 2005.
- 3.Increasing morbidity and mortality associated with abuse of methamphetamine—United States, 1991–1994. MMWR Morb Mortal Wkly Rep. 1995;44(47):882–886. [PubMed]
- 4.Treatment Episode Data Set (TEDS). Highlights—2003. National Admissions to Substance Abuse Treatment Services. DASIS Series: S-27. 2005 (DHHS Publication No. (SMA) 05-4043). Available at: http://wwwdasis.samhsa.gov/teds03/2003_teds_highlights.pdf. Accessed on August 14, 2007.
- 5.Roberts DL, Ball J. Amphetamine and Methamphetamine Emergency Department Visits, 1995–2002 The Drug Abuse Warning Network. The DAWN Report. July 2004. Available at: http://dawninfo.samhsa.gov/old_dawn/pubs_94_02/shortreports/files/DAWN_tdr_amphetamine.pdf. Accessed on August 14, 2007.
- 6.Brecht ML, Greenwell L, Anglin MD. Methamphetamine treatment: trends and predictors of retention and completion in a large state treatment system (1992–2002). J Subst Abuse Treat. 2005;29(4):295–306. [DOI] [PubMed]
- 7.Johnston LD, O’Malley PM, Bachman JG. Monitoring the Future: National Survey Results on Drug Use, 1975–2002, Volume II: College Students & Adults Ages 19–40. National Institute on Drug Abuse; 2002.
- 8.Iritani BJ, Hallfors DD, Bauer DJ. Crystal methamphetamine use among young adults in the USA. Addiction. 2007;102(7):1102–1113. [DOI] [PubMed]
- 9.Mansergh G, Colfax GN, Marks G, Rader M, Guzman R, Buchbinder S. The Circuit Party Men’s Health Survey: findings and implications for gay and bisexual men. Am J Public Health. 2001;91(6):953–958. [DOI] [PMC free article] [PubMed]
- 10.Shoptaw S, Peck J, Reback CJ, Rotheram-Fuller E. Psychiatric and substance dependence comorbidities, sexually transmitted diseases, and risk behaviors among methamphetamine-dependent gay and bisexual men seeking outpatient drug abuse treatment. J Psychoactive Drugs. 2003;35(Suppl 1):161–168. [DOI] [PubMed]
- 11.Schwarcz S, Scheer S, McFarland W, et al. Prevalence of HIV infection and predictors of high-transmission sexual risk behaviors among men who have sex with men. Am J Public Health; 2007;97(6):1067–1075 (Jun). [DOI] [PMC free article] [PubMed]
- 12.Colfax G, Coates TJ, Husnik MJ, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J Urban Health. 2005;82(Suppl 1):i62–i70. [DOI] [PMC free article] [PubMed]
- 13.Colfax G, Vittinghoff E, Husnik MJ, et al. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 15 2004;159(10):1002–1012. [DOI] [PubMed]
- 14.Wong W, Chaw JK, Kent CK, Klausner JD. Risk factors for early syphilis among gay and bisexual men seen in an STD clinic: San Francisco, 2002–2003. Sex Transm Dis. 2005;32(7):458–463. [DOI] [PubMed]
- 15.Hirshfield S, Remien RH, Walavalkar I, Chiasson MA. Crystal methamphetamine use predicts incident STD infection among men who have sex with men recruited online: a nested case-control study. J Med Internet Res. 29 2004;6(4):e41. [DOI] [PMC free article] [PubMed]
- 16.Semple SJ, Zians J, Grant I, Patterson TL. Impulsivity and methamphetamine use. J Subst Abuse Treat. 2005;29(2):85–93. [DOI] [PubMed]
- 17.Semple SJ, Zians J, Grant I, Patterson TL. Methamphetamine use, impulsivity, and sexual risk behavior among HIV-positive men who have sex with men. J Addict Dis. 2006;25(4):105–114. [DOI] [PubMed]
- 18.Hirshfield S, Remien RH, Humberstone M, Walavalkar I, Chiasson MA. Substance use and high-risk sex among men who have sex with men: a national online study in the USA. AIDS Care. 2004;16(8):1036–1047. [DOI] [PubMed]
- 19.Chesney MA, Koblin BA, Barresi PJ, et al. An individually tailored intervention for HIV prevention: baseline data from the EXPLORE Study. Am J Public Health. 2003;93(6):933–938. [DOI] [PMC free article] [PubMed]
- 20.Plankey MW, Ostrow DG, Stall R, et al. The Relationship Between Methamphetamine and Popper Use and Risk of HIV Seroconversion in the Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr. 1 2007;45(1):85–92. [DOI] [PMC free article] [PubMed]
- 21.Molitor F, Truax SR, Ruiz JD, Sun RK. Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. West J Med. 1998;168(2):93–97. [PMC free article] [PubMed]
- 22.Lorvick J, Martinez A, Gee L, Kral AH. Sexual and injection risk among women who inject methamphetamine in San Francisco. J Urban Health. 2006;83(3):497–505. [DOI] [PMC free article] [PubMed]
- 23.Gibson DR, Leamon MH, Flynn N. Epidemiology and public health Consequences of methamphetamine use in California’s Central Valley. J Psychoact Drugs. 2002;34(3):313–319. [DOI] [PubMed]
- 24.Kushel MB, Hahn JA, Evans JL, Bangsberg DR, Moss AR. Revolving doors: imprisonment among the homeless and marginally housed population. Am J Public Health. 2005;95(10):1747–1752. [DOI] [PMC free article] [PubMed]
- 25.Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92(5):778–784. [DOI] [PMC free article] [PubMed]
- 26.Cheung AM, Hwang SW. Risk of death among homeless women: a cohort study and review of the literature. CMAJ. 2004;170(8):1243–1247. [DOI] [PMC free article] [PubMed]
- 27.Hwang SW. Mortality among men using homeless shelters in Toronto, Ontario. JAMA. 2000;283(16):2152–2157. [DOI] [PubMed]
- 28.Breakey WR, Fischer PJ, Kramer M, et al. Health and mental health problems of homeless men and women in Baltimore. JAMA. 1989;262(10):1352–1357. [DOI] [PubMed]
- 29.Wenzel SL, Ebener PA, Koegel P, Gelberg L. Drug-abusing homeless clients in California’s substance abuse treatment system. J Psychoactive Drugs. 1996;28(2):147–159. [DOI] [PubMed]
- 30.Mattison AM, Ross MW, Wolfson T, Franklin D. Circuit party attendance, club drug use, and unsafe sex in gay men. J Subst Abuse. 2001;13(1–2):119–126. [DOI] [PubMed]
- 31.Halkitis PN, Green KA, Mourgues P. Longitudinal investigation of methamphetamine use among gay and bisexual men in New York City: findings from Project BUMPS. J Urban Health. 2005;82(Suppl 1):i18–i25. [DOI] [PMC free article] [PubMed]
- 32.Semple SJ, Patterson TL, Grant I. A comparison of injection and non-injection methamphetamine-using HIV positive men who have sex with men. Drug Alcohol Depend. 2004;76(2):203–212. [DOI] [PubMed]
- 33.Newmeyer JA. The prevalence of drug use in San Francisco in 1987. J Psychoactive Drugs. 1988;20(2):185–189. [DOI] [PubMed]
- 34.Newmeyer JA. Patterns and trends of drug use in the San Francisco Bay Area. J Psychoact Drugs. 2003;35(Suppl 1):127–132. [DOI] [PubMed]
- 35.Fairbairn N, Kerr T, Buxton JA, Li K, Montaner JS, Wood E. Increasing use and associated harms of crystal methamphetamine injection in a Canadian setting. Drug Alcohol Depend. 11 2007;88(2–3):313–316. [DOI] [PMC free article] [PubMed]
- 36.Burnam M, Koegel P. Methodology for obtaining a representative sample of homeless persons. Eval. Rev. 1988;12:117–152. [DOI]
- 37.Robertson MJ, Clark RA, Charlebois ED, et al. HIV seroprevalence among homeless and marginally housed adults in San Francisco. Am J Public Health. 2004;94(7):1207–1217. [DOI] [PMC free article] [PubMed]
- 38.Hahn JA, Kushel MB, Bangsberg DR, Riley E, Moss AR. BRIEF REPORT: the aging of the homeless population: fourteen-year trends in San Francisco. J Gen Intern Med. 2006;21(7):775–778. [DOI] [PMC free article] [PubMed]
- 39.Mantel N. Chi-square tests with one degree of freedom: extensions of the Mantel-Haenszel procedure. J Am Stat Assoc. 1963;58:690–700. [DOI]
- 40.Colfax GN, Vittinghoff E, Grant R, Lum P, Spotts G, Hecht FM. Frequent methamphetamine use is associated with primary non-nucleoside reverse transcriptase inhibitor resistance. AIDS. 2007;21(2):239–241. [DOI] [PubMed]
- 41.Meredith CW, Jaffe C, Ang-Lee K, Saxon AJ. Implications of chronic methamphetamine use: a literature review. Harv Rev Psychiatr. 2005;13(3):141–154. [DOI] [PubMed]
- 42.Maxwell JC. Emerging research on methamphetamine. Curr Opin Psychiatry. 2005;18(3):235–242. [DOI] [PubMed]
- 43.Curtis EK. Meth mouth: a review of methamphetamine abuse and its oral manifestations. Gen Dent. 2006;54(2):125–129; quiz 130. [PubMed]
- 44.Saini T, Edwards PC, Kimmes NS, Carroll LR, Shaner JW, Dowd FJ. Etiology of xerostomia and dental caries among methamphetamine abusers. Oral Health Prev Dent. 2005;3(3):189–195. [PubMed]
- 45.Williams N, Covington JS, 3rd. Methamphetamine and meth mouth: an overview. J Tenn Dent Assoc. 2006;86(4):32–35. [PubMed]
- 46.Tominaga GT, Garcia G, Dzierba A, Wong J. Toll of methamphetamine on the trauma system. Arch Surg. 2004;139(8):844–847. [DOI] [PubMed]
- 47.Rippeth JD, Heaton RK, Carey CL, et al. Methamphetamine dependence increases risk of neuropsychological impairment in HIV infected persons. J Int Neuropsychol Soc. 2004;10(1):1–14. [DOI] [PubMed]
- 48.Reback CJ, Larkins S, Shoptaw S. Methamphetamine abuse as a barrier to HIV medication adherence among gay and bisexual men. AIDS Care. 2003;15(6):775–785. [DOI] [PubMed]
- 49.Obert JL, McCann MJ, Marinelli-Casey P, et al. The matrix model of outpatient stimulant abuse treatment: history and description. J Psychoact Drugs. 2000;32(2):157–164. [DOI] [PubMed]
- 50.Rawson RA, Marinelli-Casey P, Anglin MD, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction. 2004;99(6):708–717. [DOI] [PubMed]
- 51.Rawson RA, Gonzales R, Brethen P. Treatment of methamphetamine use disorders: an update. J Subst Abuse Treat. 2002;23(2):145–150. [DOI] [PubMed]
- 52.Rawson RA, Huber A, Brethen P, et al. Status of methamphetamine users 2–5 years after outpatient treatment. J Addict Dis. 2002;21(1):107–119. [DOI] [PubMed]