Abstract
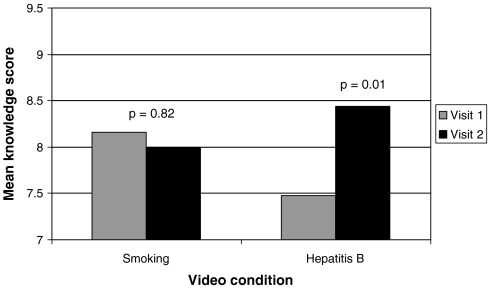
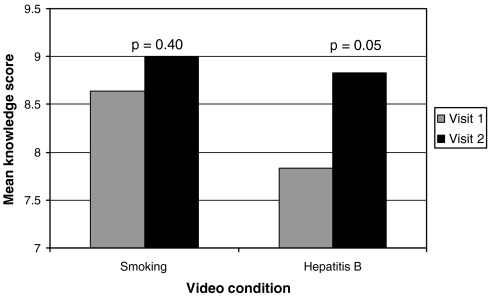
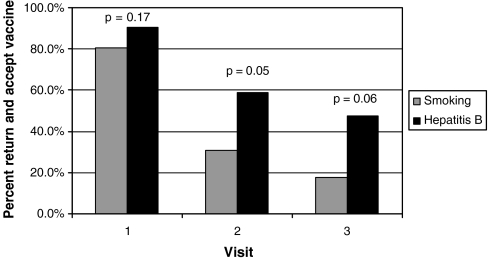
Homeless youth are at increased risk for hepatitis B virus (HBV) infection and HBV vaccine coverage is poor in this group. The purpose of our study was to determine if a shelter-based HBV vaccine program in children and adolescents 2–18 years of age with a randomized controlled trial using a culturally appropriate HBV video could increase HBV vaccine coverage rates. Subjects were randomized to an 8 min HBV video or a control, smoking prevention video. Before exposure to the videos, HBV knowledge, and demographics were assessed in caregivers and adolescents. HBV vaccine no. 1 was offered to all subjects who did not produce a vaccine record; subsequently, an accurate HBV vaccine history was obtained from medical providers. Subjects were asked to return 1 and 3 months after visit 1, HBV vaccine was offered to all with incomplete coverage, and HBV knowledge was reassessed. There were 328 children and adolescents cared for by 170 caregivers enrolled in the study. One hundred and four had incomplete HBV vaccine coverage. Data are reported for all family units with at least one subject needing vaccine. There were 53 children and adolescents randomized to the HBV video vs. 51 to the smoking video. HBV knowledge scores of caregivers improved at Visit no. 2 vs. no. 1 in the HBV video group (p = 0.01) but not in the smoking group (p = 0.82). Similar results were observed for adolescents in the HBV video group (p = 0.05) but not in the smoking group (p = 0.40). Exposure to the HBV video vs the smoking video had a significant effect on return rates for vaccine at Visit no. 2 (59 vs. 31%; p = 0.05) but not at Visit no. 3 (47 vs. 18%, p = 0.06). The shelter-based vaccine program was very effective in increasing HBV coverage rates in the entire group of 328 children and adolescents enrolled in the study, from 68% coverage at baseline to 85% at the conclusion of the study. We conclude that shelter-based HBV vaccine programs can be highly effective in increasing vaccine coverage rates in older children and adolescents. A brief exposure to a culturally appropriate HBV video improves HBV knowledge and may improve return rates for vaccine.
Keywords: Compliance, Educational video, Immunizations, Urban poor, Viral hepatitis
Introduction
Since 1982, the Advisory Committee on Immunization Practices has issued a series of increasingly rigorous hepatitis B vaccination recommendations, culminating in the recommendation in 1999 to vaccinate all persons aged 0 to 18 years who had not been vaccinated previously.1 HBV vaccine coverage rates in the US have risen dramatically over this time period so that 92% of infants and 50–60% of adolescents ages 13–15 years have records indicating that they have been vaccinated.2 In contrast to these excellent HBV vaccine coverage rates for the general population, we have recently reported that only 29% of homeless Baltimore adolescents 13–18 years of age were vaccinated against HBV and only 4% of these subjects had a vaccination card.3 It is discouraging that this problem exists despite the existence of the Vaccines for Children program, which provides publicly purchased vaccine to public and private health care providers for use in children enrolled in Medicaid, Native American or Alaska Native children and children who are uninsured or underinsured.
The poor HBV vaccine coverage in the homeless adolescents is particularly concerning because rates of HBV infection (either present or past) in homeless subjects are much higher than in the general population (9–17% for homeless adolescents)4–6 and 30% for homeless adults7,8 vs. 1.8% of US children and 4.9% of adults.9 Published strategies to increase acceptance of vaccines in general include multi-component interventions with client reminders, education, incentives, and free vaccine.10 Clearly, the existence of free vaccine alone is not sufficient to achieve optimal HBV vaccine coverage in our population of homeless children and adolescents in Baltimore.3 A recent critique of 225 studies of 17 interventions to improve vaccination coverage in children and adolescents served as the basis for recommendations by the Task Force on Community Preventive Services.10 This review concluded that there was strong scientific evidence that the following interventions were effective: client reminders, reducing out-of-pocket costs for vaccinations, home visits, and multi-component interventions including education. However, the contribution of individual components to the overall effectiveness of the interventions could not be attributed. Whether or not incentives and educational efforts could actually increase vaccine coverage in the problematic pediatric homeless population, characterized by many barriers to effective medical care,11 is not known.
The purpose of our study was to determine if a shelter-based program with a multi-component intervention including reminders, incentives, and free vaccine could improve HBV vaccine coverage compared to baseline rates in children and adolescents 2–18 years of age and to perform a randomized controlled trial to determine if a culturally appropriate educational session with an HBV video could increase HBV vaccine coverage rates compared to a comparable session with a control video on smoking prevention.
Methods
Study Design
Details regarding the method of recruitment into the study, characteristics of the homeless shelters and transitional houses where the study was done, visit schedule, and the means of ascertaining the HBV vaccine history have been previously published.3 In the month between visit nos. 1 and 2 the vaccine history was researched by the study nurse and research assistant for all children whose caregivers did not produce vaccination records. Healthcare providers were contacted by phone and/or fax and the Baltimore Immunization Registry Program and the school database of the Baltimore City Health Department were reviewed.
In brief, at visit no. 1, after informed consent was obtained from the caregiver or independent teen (18 years of age and not living with a caregiver), family units (caregiver with one or more children 2–12 years of age and/or adolescents 13–18 years of age) were randomized to one of two culturally appropriate educational videos. Each enrollment visit to each shelter was randomized, in order to include as many sites as possible with diverse populations, duration of stay, size, and geographical locations. If more than one family unit was enrolled at a site, then all family units enrolled at the site at that time were exposed to the same video. The videos were Respect Yourself/Protect Yourself by the Hepatitis Foundation International (to instruct the subject about hepatitis B infection and the importance of HBV vaccine) and Bilal’s Dream, by the American Lung Association (to instruct the subject about the deleterious health consequences of cigarette smoking). Both of these videos featured African American children and adolescents and were selected as a culturally appropriate tool because 88% of the homeless caregivers in the study were African American.3
Demographic information and HBV vaccine history were then obtained by interview of caregivers and adolescents. A laptop-based questionnaire (ACASI-automated, computer-assisted self inventory)12 was used to assess HBV vaccine attitudes and knowledge as well as potentially sensitive information about drug and alcohol use and to screen for depression using the Center for Epidemiologic Studies Depression (CES-D) short form.13 The rationale for doing depression screening was that severe depression might interfere with the caregiver’s interest and/or ability to obtain HBV vaccine coverage for the child/children cared for. Subsequently, family units were shown one of the two 8-min videos; after the video presentation the research nurse reviewed the contents of the video with a 5-min Power Point summary and encouraged the subjects to ask questions to increase their understanding of the information presented. The families were given the Vaccine Information Sheet for Hepatitis B Vaccine. HBV vaccine was offered to all children and adolescents whose caregivers did not produce a vaccination record proving completion of three doses of vaccine.
Both Engerix-B (GlaxoSmithKline; 10 μg in 0.5 ml) and Recombivax HB (Merck; 5 μg in 0.5 ml) in 0.5 ml were used over the course of the study and were given via the intramuscular route in the deltoid or anterolateral thigh. It should be noted that a condensed 3 month schedule was done in this study in recognition of the reality that homeless shelters in Baltimore generally have short stays, ranging from 30 to 90 days. At each visit, families were instructed to return to their medical provider in 6–12 months for the fourth HBV vaccine as recommended by the Center for Disease Control if there is not a 4 month interval in between the first and third vaccine.14
At the conclusion of visit no. 1, children, adolescents, and caregivers were screened for hepatitis C virus (anti-HCV) antibody, using a finger-stick testing system (detailed results of the hepatitis C screening are being reported separately). In this paper, HCV screening results are reported for the two video groups since HCV infection of the caregiver might conceivably affect attitude toward HBV vaccine coverage for the caregiver’s children. In addition to the videos, other interventions which might increase return rates and acceptance of HBV vaccine were as follows: caregivers were paid $10 and children, adolescents, and caregivers were given gift packages containing cosmetics for the adults and candy and toothbrushes for the children. Caregivers were also given reminder cards with the date of the next appointment in a card pouch which could be worn as a necklace.
All families were instructed to return in 1 month for visit no. 2, in which the second HBV vaccine dose was given if the vaccine history (researched in between visit nos. 1 and 2) demonstrated that it was indicated. They were also given the anti-HCV test results at visit no. 2. At this visit, vaccine attitudes and knowledge were again assessed, and the second vaccine was administered. Only those families in whom there was at least one subject needing the third vaccine were instructed to return in 2 months (3 months from visit no. 1) Caregivers were paid $10 and given reminder cards; both they and their children and adolescents were given gifts as in visit 1. At visit no. 3 HBV vaccine attitudes and knowledge were again assessed and the third HBV vaccine given if indicated Caregivers were then paid $30 and children, adolescents and caregivers were given gift packages.
HBV Knowledge Questionnaire
There were ten true/false questions, as follows: (1) Hepatitis B can cause cirrhosis. (2) Hepatitis B is found mainly in urine. (3) Hepatitis B always makes you feel sick. (4) Only one hepatitis B shot is needed to protect a person against hepatitis B. (5) A person can die from hepatitis B. (6) A person can get hepatitis B from sharing cups and other utensils. (7) A person can get hepatitis B from unprotected sex. (8) A person can get hepatitis B from drugs and needles. (9) A person can get hepatitis B from hugging. (10) Newborns can get hepatitis B from their mothers.
Statistics
Analyses were conducted to examine the association of video condition with three dependent variables that were expected to be affected by the video. Vaccine coverage was defined as receiving all three vaccine shots needed by the end of each visit (coded 1) vs. not receiving all three required shots by the end of each visit (coded 0). Children who dropped out of the study before completing the series were assumed to have not completed the vaccine series. Summary descriptive statistics for vaccine coverage are provided, indicating how many children completed the entire three-shot series by the end of each visit. Completing vaccine coverage by the end of the study (i.e., by the end of visit 3) was of primary interest, therefore hypothesis tests were done using completion rates at the end of visit 3 only. Return and accept a shot was defined as accepting a shot that was needed at each visit (coded 1) vs. not accepting the shot that was needed (coded 0); if a child failed to return for a visit when a shot was needed, this was considered non-acceptance. Vaccine acceptance is distinct from vaccine coverage because it was possible to accept a shot that was needed at a given visit without completing the entire three-shot series during that visit. Finally, HBV knowledge score was computed for visits 1 and 2; it ranged from 0 (no correct answers) to 10 (all correct answers).
Data management and analysis were performed using SAS v9.1 (SAS Institute, Cary, NC). Separate analyses were conducted for caregivers and children and adolescents. The seven independent teens were always included with the adolescents. All analyses of the child and adolescent data adjusted for the fact that there were multiple children and/or adolescents within the same families as well as repeated measurements for individual children and adolescents (visits 1, 2 and 3); this was done using mixed models and design effect models (SAS PROCs NLMIXED and SURVEYLOGISTIC for dichotomous variables, and MIXED and SURVEYREG for continuous variables). Analyses of caregiver characteristics at baseline did not involve a clustered data structure; therefore, Fisher’s exact test (dichotomous variables) or t tests (continuous variables) were used. With the exception of descriptive statistics for completion rates at each visit, all statistical analyses focused on differences between the video conditions. Analyses of the association of video condition with the dependent variables (defined above) took into account video condition, visit and the condition-by-visit interaction. Because the impact of video condition was of primary interest and participants were randomized to video conditions, other adjustment variables were not included. Secondary analyses taking further adjustment variables into account were not attempted due to the small sample size of children needing shots. All analyses of the impact of video condition utilized mixed models; the direct likelihood technique enabled unbiased estimation of video condition effects in the presence of some missing data for the dependent variables at visits 2 and 3.15,16 Examination of residual distributions indicated that the models were reasonably consistent with statistical assumptions. A p value of <0.05 was considered statistically significant.
Results
There were 328 children and adolescents (including 7 independent teens) and 170 adult caregivers enrolled in the study. Of the adult caregivers, 69% were 31 years old or greater, 87% were African American, and 95% were female. Thirty-nine percent were single, 26% were married, and 35% were separated, divorced, or widowed. Twelve percent were currently employed. Thirty-five percent earned $5,000 or less, 23% $5–10,000, and 11% >$10,000 annually. Forty-two percent had not completed high school. Thirty-six percent were responsible for three or more children and/or adolescents and 64% for 1–2 children and /or adolescents. There were 52% who were living in a shelter, 39% in transitional housing, and 9% in other housing. The following characteristics were reported by caregivers and adolescents, respectively: alcohol use at least once/week, 7 and 14%; cocaine/crack last 6 months, 17 and 14%; heroin last 6 months, 12 and 14%; and ever injected street drugs, 17 and 14%.
HBV vaccine acceptance and rates of completion of three doses of vaccine in various age groups is shown in Table 1. The vaccine coverage rate for the whole group increased from 68% at baseline to 85% at the conclusion of the study. The group showing the most dramatic improvement was the 13–18 year age group in which HBV vaccine coverage increased from 31% at baseline to 68%. One hundred three children and adolescents who were given vaccine at visit no. 1 were later shown to have had full HBV vaccine coverage at baseline. There were a total of 244 vaccinations in the study, so 103/244 (42%) were given vaccine unnecessarily.
TABLE 1.
Vaccine acceptance and completion rates by homeless Baltimore children and adolescents (of those who needed it at study entry)
| Age group | Visit 1 | Visit 2 | Visit 3 | |||
|---|---|---|---|---|---|---|
| Accept n (%) | Complete n (%) | Accept n (%) | Complete n (%) | Accept n (%) | Complete n (%) | |
| 2–5 years | 8/13 (62) | 6/13 (46) | 2/7 (29) | 0/7 (0) | 2/7 (29) | 2/7 (29) |
| 6–9 years | 10/11 (91) | 5/11 (45) | 2/6 (33) | 0/6 (0) | 1/6 (17) | 1/6 (17) |
| 10–12 years | 32/37 (86) | 9/37 (24) | 11/28 (39) | 1/28 (4) | 9/27 (33) | 9/27 (33) |
| 13–18 years | 39/43 (91) | 9/43 (21) | 19/34 (56) | 2/34 (6) | 12/32 (38) | 12/32 (38) |
| Total | 89/104 (86) | 29/104 (28) | 34/75 (45) | 3/75 (4) | 24/72 (33) | 24/72 (33) |
Of the 104 children and adolescents who needed the vaccine at Visit 1, 89 accepted it. There were seven who declined a shot because they mistakenly believed that the child had already completed the vaccine series and an additional eight who needed it but rejected it. Of the latter, two caregivers did not believe their child was at risk for HBV, four children refused to cooperate and two said they preferred to get it from their own doctor. Acceptance rates were highest in the 13 to 18-year group (91% at the baseline visit). Overall, 89/104 (86%) accepted one or more vaccines and 54% completed the HBV vaccine series.
The demographics of the 76 caregivers of the 104 children and adolescents who needed HBV vaccine are shown in Table 2; the profile of the 37 caregivers in the HBV video group was similar to that of the 39 caregivers in the Smoking video group. Because the previously reported historical HBV vaccine coverage group in this population had shown a significant age effect,3 the children and adolescents were grouped according to age (Table 3). There were no age differences between video groups. Mean baseline HBV knowledge scores of the caregivers were similar in the two video groups; scores did not differ between the 22 adolescents in the HBV video group and the 21 adolescents in the Smoking video group. Exposure to the HBV video improved HBV knowledge scores in both caregivers (Figure 1) and adolescents (Figure 2). Exposure to the HBV video was associated with increased return rates for HBV vaccine at visit no. 2 with a trend to increased return rates for HBV vaccine at visit no. 3 (p = 0.06; Figure 3). Of the 104 children and adolescents who needed HBV vaccine at the beginning of the study, 62.3% (33/53) of the HBV video group completed the HBV vaccine series by the end of the study vs. 45.1% (23/51) of the Smoking video group, p = 0.16. Neither visit 1 nor visit 2 HBV knowledge scores, nor changes in knowledge scores between visits 1 and 2, were associated with completion of the vaccine series by the end of the study (p’s > 0.50). In addition, HBV knowledge was not associated with rates of returning to accept vaccine shots at each visit (p > 0.90).
TABLE 2.
Demographics of homeless Baltimore caregivers in both educational video groups
| Variable | HBV video | Smoking video | P valuea |
|---|---|---|---|
| N | 37 | 39 | |
| Female | 97.3% (36/37) | 92.3% (36/39) | 0.61 |
| African American | 86.5% (32/37) | 89.7% (35/39) | 0.73 |
| Single | 35.1% (13/37) | 30.8% (12/39) | 0.81 |
| Not educated past 11th grade | 37.8% (14/37) | 43.6% (17/39) | 0.65 |
| Biological mother | 97.1% (33/34) | 92.1% (35/38) | 0.62 |
| Responsible for 4 or more children | 29.7% (11/37) | 28.2% (11/39) | 1.00 |
| Lived on streets last 6 months | 10.8% (4/37) | 20.5% (8/39) | 0.35 |
| Employed | 16.2% (6/37) | 12.8% (5/39) | 0.75 |
| Financial assistance | 86.5% (32/37) | 87.2% (34/39) | 1.00 |
| Income ≤0K | 54.1% (20/37) | 69.2% (27/39) | 0.24 |
| Anti-HCV+ | 27.0% (10/37) | 18.9% (7/37) | 0.58 |
| Ever injected street drugs | 12.1% (4/33) | 11.4% (4/35) | 1.00 |
| Heroin last 6 months | 8.8% (3/34) | 13.2% (5/38) | 0.71 |
| Cocaine last 6 months | 14.7% (5/34) | 21.1% (8/38) | 0.55 |
| Alcohol 1–7 times/week | 8.8% (3/34) | 7.9% (3/38) | 1.00 |
| Depression score | 5.1 ± 0.6 (34) | 6.1 ± 0.9 (38) | 0.39 |
aFisher’s exact test for binary variables and t test for continuous variables (n)
TABLE 3.
Child and adolescent demographics according to video groups
| Variable | HBV video | Smoking video | P valuea |
|---|---|---|---|
| N | 53 | 51 | |
| Mean age | 11.3 ± 0.5 | 11.2 ± 0.6 | 0.86 |
| Age category | |||
| 2–5years | 11.3% (6/53) | 13.7% (7/51) | 0.74 |
| 6–9years | 11.3% (6/53) | 9.8% (5/51) | 0.79 |
| 10–12years | 35.8% (19/53) | 35.3% (18/51) | 0.95 |
| 13–18years | 41.5% (22/53) | 41.2% (21/51) | 0.97 |
| Female | 47.2% (25/53) | 60.8% (31/51) | 0.20 |
| African American | 90.6% (48/53) | 88.2% (45/51) | 0.74 |
aWald chi-square (binary outcomes) or t test (continuous outcomes) after adjustment of standard errors for design effects to account for clustering of children in families.
FIGURE 1.
Mean HBV knowledge scores in Caregivers for visits 1 and 2 according to Video Condition. (Smoking video, n = 38 at visit 1 and 25 at visit 2; Hepatitis B video, n = 34 at visit 1 and 26 at visit 2).
FIGURE 2.
Mean HBV knowledge scores in Adolescents during visits 1 and 2 according to video condition (Smoking video, n = 19 at visit 1 and 11 at visit 2; Hepatitis B video, n = 18 at visit 1 and 14 at visit 2).
FIGURE 3.
HBV vaccine acceptance rates by children and adolescents who watched a Hepatitis B video vs. those who watched a Smoking video (Smoking video, n = 51, 36 and 34 at visits 1, 2 and 3, respectively; Hepatitis B video, n = 55, 39 and 38 at visits 1, 2 and 3, respectively).
Discussion
Overall, our multi-component shelter-based vaccine program was highly successful in increasing HBV vaccine coverage in the homeless Baltimore children and adolescents studied. The randomized controlled trial demonstrated that the use of a brief educational session with a culturally appropriate video about HBV added to the effects of the other interventions to increase HBV knowledge among caregivers and adolescents. There was an insignificant trend toward a positive effect on vaccine acceptance rates in this relatively small study. It is particularly noteworthy that vaccine acceptance by the adolescents was excellent. These subjects are at increased risk for HBV infection and historically they have the lowest HBV coverage of all subjects in the pediatric age group.
Although there have been many studies in the urban poor as to how to improve vaccination rates in general, no studies have focused specifically on improvement of HBV vaccine coverage among homeless children and adolescents. Only one study addressed the impact of vaccination programs at child care centers.17 No studies were identified regarding educational materials other than printed materials, no studies focused on improving HBV vaccine coverage, and no study investigated means of increasing vaccine acceptance by adolescents. In contrast, several groups have reported successful strategies in increasing HBV vaccine coverage in high-risk adult populations, including counseling,18 free HBV serologic testing and vaccine,19 and linking HBV vaccine to a syringe exchange program offered in mobile health care services.20
Our study of homeless children and adolescents was unique in three ways: (1) it focused on a shelter-based vaccine program and (2) it included educational materials in addition to printed materials and (3) it included evaluation of strategies to increase vaccine coverage in adolescents. The HBV video used in our study (Respect Yourself–Protect Yourself—Teens Talk to Teens About Liver Wellness) had been developed to target adolescents but had never been evaluated in a prospective controlled trial. The primary focus of this video was to alert young adults to the importance of their liver. The second most important message was about viral hepatitis, drugs, and alcohol, and how they can damage the liver and impact negatively on one’s life. The overall goal of the video was to encourage children and adolescents to take responsibility for their own healthcare and adopt healthy lifestyle behaviors. It is interesting that HBV knowledge scores themselves did not correlate with HBV vaccine acceptance rates nor with return rates although exposure to the HBV video, HBV Power Point presentation and discussion was associated with higher HBV vaccine acceptance rates at visit 2 and a trend (p = 0.06) to higher acceptance rates at Visit 3. Thus, it may be that the general emphasis on the importance of protecting oneself against HBV and the time spent by the study nurse discussing the negative health impact of HBV had a greater impact than the specific knowledge points addressed in the video.
We believe this type of approach to empower youth to take a proactive approach to healthy life-styles is particularly relevant for the homeless, given the multiple barriers to medical care they often face.21,22 However, since the approach used in this study was toward family units, it is not clear whether the youth, the caregivers, or both were involved in the decisions to return and to accept vaccine. In the past, more homeless families than housed poor families were uninsured.23 Homeless families are much less likely to report a regular provider for preventive care and are more likely to use emergency departments or clinics rather than private offices for both preventive care and sick care.23 More recently, it has been reported that, even in times of economic prosperity and welfare reform, >40% of one cohort of homeless adults lacked health insurance.24 All of these barriers have the potential for having a negative impact on HBV vaccine coverage for the children and adolescents living in these families.
One of the major barriers to HBV vaccine coverage of homeless youth is the unstable, transient nature of the population. This transiency makes it difficult to accomplish in this population the vaccine schedules recommended by the Advisory Committee on Immunization Practices (ACIP) for all children and adolescents.14 For children 1–10 years, the following schedules are acceptable: 0, 1, and 6 months; 0, 2, and 4 months; and 0, 1, 2, and 12 months. For adolescents 11–19 years there are seven different acceptable schedules, the most important element being a minimum of 4 months between the initial and final dose. Thus, the accelerated schedule we used in this study, of 0, 1, and 3 months would be consistent with ACIP recommendations only if the children and adolescents followed through with the recommendation of a booster at 12 months. It is somewhat reassuring that there are at least two reports of accelerated HBV vaccine schedules of 0, 10 and 21 days resulting in >90% seropositivity 12 months after the initial dose.25,26 It is also worth noting that longer-than-recommended intervals between HBV vaccine doses do not reduce final concentrations of antibody.27
Thus, one limitation of our study was that our vaccine schedule was dictated by the practicality of what we thought we could achieve in the homeless population. Another limitation is that, since we employed a multi-component intervention in our study, it was not possible to analyze the individual impact on vaccine coverage of the various strategies we used. These included free vaccines, shelter-based vaccine delivery, reminder pouches, cash incentives and gift packets, reduction of out of pocket expenses for our families, and even the service of performing anti-HCV testing and its impact on return rates. An additional limitation is that the comparisons of variables between the arms of the study (e.g., Smoking video vs. HBV video) involved small numbers of subjects. Furthermore, there were no provisions made to prevent subjects from memorizing the HBV video. A final limitation was that the transient nature of the homeless population did not permit follow-up serology.
One of the goals of the US Health and Human Services for Healthy People in 2010 is to “reduce to zero cases per 100,000 hepatitis B rates in persons aged <25 years (except perinatal infection”.1 To achieve this goal it will be necessary to target HBV vaccine coverage efforts at high-risk pediatric populations such as homeless children and adolescents. Investigators at Yale20 recently demonstrated it was feasible to increase HBV vaccine coverage in adult injection drug users attending a syringe exchange site. There were 77% of the vaccine-eligible subjects who completed two vaccines, and 66% completed three vaccines. Correlates of completing all three vaccinations included being homeless (OR 1.98, 95% CI = 1.14–12.27).
Our experience suggests that shelter-based programs targeted at older children and adolescents have the potential of significantly increasing HBV vaccine coverage in this high-risk population.
Acknowledgment
Yvette Bowser and Yvonne Barnes for data management, Ed Hirschorn of Maryland Vaccines for Children for provision of vaccines, Joseph Bareta for statistical advice, Shaina Ashe and Aileen Staples for research assistance, Margaret Wilson for expert secretarial assistance, Betty Schulze RN CPNP and Joanne Manzo RN CPNP of Healthcare for the Homeless for introducing us to the shelters, (the Center for Disease Control for providing partial support for the development of the Hepatitis B video) Paul Wockenfuss and the Saint James Social Ministries for gift donations, shelter managers who made the study possible and the caregivers and their children who enrolled in the study. The research was supported by a grant from NIH/NIDA RO1 DA13743.
References
- 1.Centers for Disease Control and Prevention. Update recommendations to prevent hepatitis B virus transmission—United States. MMWR Morb Mortal Wkly Rep. 1999;48:33–34. [PubMed]
- 2.Center for Diseases Control. Viral Hepatitis B: Frequently Asked Questions. Available at http://www/cdc/gov/ncidod/diseases/hepatitis/b/faqb.htm. Accessed on 12/8/2006.
- 3.Schwarz K, Garrett B, Lamoreux J. Hepatitis B vaccination rate of homeless children in Baltimore. J Pediatr Gastroenterol Nutr. 2006;41(2):225–229. [DOI] [PubMed]
- 4.Beech BM, Myers L, Beech DJ, Kernick NS. Human immunodeficiency syndrome and hepatitis B and C infections among homeless adolescents. Semin Pediatr Infect Dis. 2003;14(1):12–19 Jan. [DOI] [PubMed]
- 5.Moses S, Mestery K, Kaita KD, Minuk GY. Viral hepatitis in a Canadian street- involved population. Can J Public Health. 2002;93(2):123–128 Mar-Apr. [DOI] [PMC free article] [PubMed]
- 6.Roy E, Haley N, Lemire N, et al. Hepatitis B virus infection among street youths in Montreal. Can Med Assoc J. 1999;161(6):689–693 Sep 21. [PMC free article] [PubMed]
- 7.Klinkenberg WD, Caslyn RJ, Morse GA et al. Prevalence of human immunodeficiency virus, hepatitis B, and hepatitis C among homeless persons with co-occurring severe mental illness and substance use disorders. Compr Psychiatry. 2003;44(4):293–302 Jul-Aug. [DOI] [PubMed]
- 8.Gelberg L, Robertson MJ, Leake B, et al. Hepatitis B among homeless and other impoverished US military veterans in residential care in Los Angeles. Public Health. 2001;115(4):286–291 Jul. [DOI] [PubMed]
- 9.McQuillan GM, Coleman PJ, Kruszon-Moran D, et al. Prevalence of hepatitis B virus infection in the United States: the National Health and Nutrition Examination Surveys, 1976 through 1994. Am J Public Health. 1999;89:14–18. [DOI] [PMC free article] [PubMed]
- 10.Briss PA, Rodewald LE, Hinman AR, et al. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. Am J Prev Med. 2000;18(1S):97–140. [DOI] [PubMed]
- 11.Klein JD, Woods AH, Wilson KM, et al. Homeless and runaway youths’ access to health care. J Adolesc Health. 2000;5:331–339. [DOI] [PubMed]
- 12.Bloom DE. Technology, experimentation, and the quality of survey data. Science. 1998;5365:847–848. [DOI] [PubMed]
- 13.Clark CH, Mahony JS, Clark DJ, et al. Screening for depression in a hepatitis C population: the reliability and validity of the Center for Epidemiologic Studies Depression Scale (CES-D). J Adv Nurs. 2002;40:361–369. [DOI] [PubMed]
- 14.Mast EE, Margolis HS, Fiore AE, et al. Advisory Committee on Immunization Practices (ACIP) part I: Immunization of infants, children, and adolescents. MMWR Recomm Rep. 2005 Dec 23;54(RR-16):1–31. Erratum in: MMWR Morb Mortal Wkly Rep. 2006 Feb 17;55(6):158–9. Division of Viral Hepatitis, National Center for Infectious Diseases. USA. [PubMed]
- 15.Beunckens C, Molenberghs G, Kenward MG. Direct likelihood analysis versus simple forms of imputation for missing data in randomized clinical trials. Clin Trials. 2005;2:379–386. [DOI] [PubMed]
- 16.Molenberghs G, Verbeke G. Models for discrete longitudinal data. New York: Springer Verlag; 2005.
- 17.O’Mara LM, Isaacs S. Evaluation of registered nurses follow-up on the reported immunization status of children attending child care centres. Can J Public Health. 1993;84:124–127. [PubMed]
- 18.Koblin BA, Xu G, Lucy D, et al. Hepatitis B infection and vaccination among high-risk noninjection drug-using women: Baseline data from the UNITY study. Sex Transm Dis. 2007;34:917–922. [DOI] [PubMed]
- 19.Ompad DC, Galea S, Wu Y, et al. Acceptance and Completion of hepatitis B vaccination among drug users in New York City. Commun Dis Public Health. 2004;7(4):294–300 Dec. [PubMed]
- 20.Altice FL, Bruce RD, Walton MR, Buitrago MI. Adherence to hepatitis B virus vaccination at syringe exchange sites. J Urban Health. 2005;82(1):151–161. [DOI] [PMC free article] [PubMed]
- 21.DuPlessis HM, Cora-Bramble D, American Academy of Pediatrics Commitee on Community Health. Providing Care for Immigrant, Homeless, and Migrant Children. Pediatrics. 2005;115:1095–1100. [DOI] [PubMed]
- 22.Simms MD. Medical care of children who are homeless or in foster care. Curr Opin Pediatr. 1998;10:486–490. [DOI] [PubMed]
- 23.Wood D, Valdez RB. Barriers to medical care for homeless families compared with housed poor families. Am J Dis Child. 1991;145(10):1109–1115. [DOI] [PubMed]
- 24.O’Toole TP, Gibbon JL, Seltzer D, Hanusa BH, Fine MJ. Urban homelessness and poverty during economic prosperity and welfare reform: changes in self-reported comorbidities, insurance, and sources for usual care, 1995–1997. J Urban Health. 2002;79(2):200–210. [DOI] [PMC free article] [PubMed]
- 25.Bosnak M, DIkici B, Bosnak V, Haspolat K. Accelerated hepatitis B vaccination schedule in childhood. Pediatr Int. 2002;44(6):663–665. [DOI] [PubMed]
- 26.Nothdurft HD, Dietrich M, Zudkerman JN, et al. A new accelerated vaccination schedule for rapid protection against hepatitis A and B. Vaccine. 2002;20(7–8):1157–1162. [DOI] [PubMed]
- 27.Hadler SC, Margolis HS. Hepatitis B immunization: vaccine types, efficacy and indications for immunization. In: Remington JS, Swartz MN, editors. Curr Clin STop Infect Dis 1992;12:282–308. [PubMed]