Abstract
The immunodeficiency, centromeric region instability, and facial anomalies syndrome (ICF) is the only disease known to result from a mutated DNA methyltransferase gene, namely, DNMT3B. Characteristic of this recessive disease are decreases in serum immunoglobulins despite the presence of B cells and, in the juxtacentromeric heterochromatin of chromosomes 1 and 16, chromatin decondensation, distinctive rearrangements, and satellite DNA hypomethylation. Although DNMT3B is involved in specific associations with histone deacetylases, HP1, other DNMTs, chromatin remodelling proteins, condensin, and other nuclear proteins, it is probably the partial loss of catalytic activity that is responsible for the disease. In microarray experiments and real-time RT-PCR assays, we observed significant differences in RNA levels from ICF vs. control lymphoblasts for pro- and anti-apoptotic genes (BCL2L10, CASP1, and PTPN13); nitrous oxide, carbon monoxide, NF-κB, and TNFa signalling pathway genes (PRKCH, GUCY1A3, GUCY1B3, MAPK13; HMOX1, and MAP4K4); and transcription control genes (NR2F2 and SMARCA2). This gene dysregulation could contribute to the immunodeficiency and other symptoms of ICF and might result from the limited losses of DNA methylation although ICF-related promoter hypomethylation was not observed for six of the above examined genes. We propose that hypomethylation of satellite 2at1qh and 16qh might provoke this dysregulation gene expression by trans effects from altered sequestration of transcription factors, changes in nuclear architecture, or expression of noncoding RNAs.
Keywords: Immunodeficiency, constitutive heterochromatin, cancer, DNA methyltransferases, chromosomal rearrangements, DNA demethylation
ICF: Introduction to the syndrome
The immunodeficiency, centromeric region in stability and facial anomalies syndrome (ICF) is a rare recessive disease characterized by targeted chromosome breakage [1]. The majority of cases of ICF that have been studied involve mutations in one of the three main DNA methyltransferase genes, DNMT3B [2–4]. These DNMT3B mutations are usually missense changes within the coding portion of the gene [5–8]. This is the only known genetic disease in humans involving mutations in one of the genes encoding an enzyme that methylates cytosine residues in DNA.
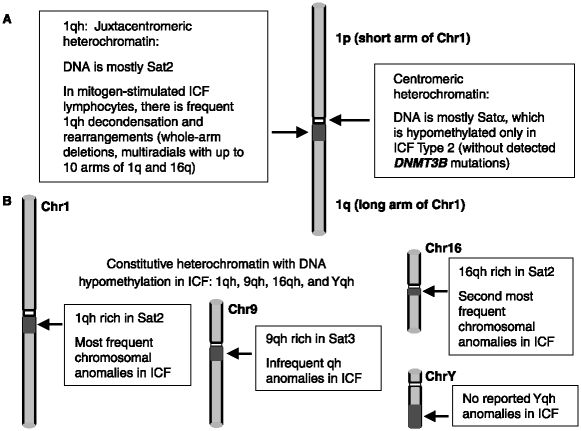
ICF is an immunodeficiency disease that has been described in fewer than 50 patients world-wide [9, 10] since it was first described in the late 1970s [11, 12]. It is diagnosed by immunoglobulin deficiency that is usually seen in the presence of normal B- and T-cell counts, characteristic chromosomal abnormalities in the vicinity of the centromere of certain chromosomes, and, usually, also facial anomalies. The immunodeficiency of ICF patients is largely responsible for their frequent mortality in early childhood. The chromosomal abnormalities are instability that is almost exclusively found in the juxtacentromeric heterochromatin (qh) regions of chromosomes 1 and 16, and sometimes 9 (Figure 1). In addition, all studied ICF tissues and cell cultures display hypomethylation of satellite 2 DNA (Sat2) in 1qh and 16qh, the related satellite 3DNA (Sat3) in 9qh, and, formales, in Yqh satellite DNA [13, 14].
Figure 1.
Hypomethylated DNA in constitutive heterochromatin in ICF. Cartoon illustrating the constitutive heterochromatin regions that display ICF-specific hypomethylation and chromosome abnormalities. Dark gray box, juxtacentromeric (pericentromeric) heterochromatin; white box, centromere.
In this review, we will briefly describe the ICF phenotype, the nature of known ICF-associated mutations in DNMT3B, and why it is likely that ICF is actually due to loss of the enzymatic activity of DNMT3B and not to alterations in its specific protein–protein interactions. The relationships of DNA hypomethylation and chromosome abnormalities in the ICF syndrome and in cancer will also be discussed. Lastly, the question of abnormal gene expression in ICF lymphoblastoid cells will be addressed in some detail with previously unreported data from an expression microarray analysis and an inferred model of how ICF-related DNA hypomethylation leads to the disease.
ICF-linked DNMT3B mutations
DNMT3B overview
ICF patients with DNMT3B mutations [2, 4, 10] are sometimes referred to as exhibiting ICF type 1 disease [7]. These patients are usually compound heterozygotes with various mutations within the gene [5, 6, 10]. In mice, Dnmt3b is an essential gene for normal development [15]. Insertional in activation of Dnmt3b or Dnmt1 results in prenatal death soon after implantation [15]. In murine knock-outs of the third major DNMT gene, Dnmt3a, death is observed several weeks after birth. In humans, if ICF-causing mutations in DNMT3B did not leave residual activity, embryonic lethality would probably result. This residual DNA methylation activity has been observed in vitro [16] and is consistent with results from in vivo mouse models [17]. Therefore, we predict that homozygous null DNMT3B mutations would lead to spontaneous abortions.
Human DNMT3B and murine Dnmt3b (94% identity) and human DNMT3A and murine Dnmt3a (98% identity [18]) have predominant roles in de novo methylation of DNA (methylation of CpG dyads that were symmetrically unmethylated) [19]. These are enzymes are especially important during embryogenesis and gametogenesis [20, 21] although their activity is not limited to these stages in development. DNMT3B and DNMT3A are not redundant in terms of function [22], as validated by the finding that DNMT3B mutations suffice to cause ICF. They differ in expression patterns during murine development [23] although they can interact and stimulate each other's activity [24]. They have some distinct preferences for sequences flanking the CpG dinucleotide and for chromosomal regions [19, 20, 25]. They also differ in relative activity in vitro toward DNA substrates in nucleosomes vs. naked DNA [26]. Complicating analysis of the function of DNMT3B/Dnmt3b and DNMT3A/Dnmt3 a gene products are the numerous isoforms that they encode, which show non-coordinate expression [22]. For example, one of the DNMT3B isoforms is missing conserved motifs in the catalytic domain but evidence suggests that it is still biologically important [27].
DNMT3B mutations in ICF patients (ICF type 1)
ICF type 1 is the only form of ICF whose genetic etiology is known. It involves biallelic DNMT3B mutations [10]. Unless otherwise noted, ICF will denote type 1 in this review. The ICF-linked DNMT3B mutations are often missense mutations and are usually found in the part of the gene encoding the catalytically active C-terminal portion of the protein, namely, one of ten motifs conserved among all cytosine-C5 methyltransferases [1, 2, 4, 5, 10, 15, 28].
The involvement of DNA hypomethylation in the phenotype of ICF is supported at the cytogenetic level. ICF-specific rearrangements in mitogen-treated lymphocytes from patients are the same in frequency, spectrum and chromosomal specificity as those that we found in a normal pro-B lymphoblastoid cell line treated with the DNA methylation inhibitors 5-azacytidine or 5-azadeoxycytidine [29, 30]. The invariant hypomethylation of certain portions of the genome in ICF cells and tissues, most notably Sat2 [1, 13], is also consistent with ICF being due to DNA methylation deficiency.
Noncatalytic functions of DNMT3B
DNMT3B has repressor activity that is independent of its DNA methyltransferase activity [31]. Accordingly, DNMT3B has many specific protein-interaction domains, which are usually outside the C-terminal catalytic domain [32–34]. The specific binding partners of DNMT3B include the other DNA methyltransferases DNMT1 and DNMT3A, histone deacetylases HDAC1 and HDAC2, HP1α, the chromatin remodelling protein hSNF2H, the condensing complex hCAP-C/hCAP-E, and the mitotic chromosome-associated KIF4A [33–35]. DNMT3B is subject to sumoylation [32], which involves addition of a small SUMO protein to alysine residue in a particular protein motif [36]. Sumoylation can affect protein–protein interactions, protein activity and protein localization [37]. The sumoylation and PWWP chromatin targeting domains in the N-terminal half of DNMT3B probably are responsible for intra-nuclear and heterochromatin targeting of the enzyme, respectively [32, 38, 39], which can occur in a cell type-specific manner [31]. Satellite DNA methylation does not appear to be necessary for targeting of Dnmt3b to heterochromatin in murine embryonal stem cells [31] but Sat2 hypomethylation might be involved in the exaggerated targeting of 1qh and 16qhto intranuclear bodies [40], as will be described below.
The only ICF-associated missense mutation outside the catalytic C-terminal half of DNMT3B (S282P) is within the PWWP domain and was found in both DNMT3B alleles in two related ICF patients [28]. The analogous mutation in mouse cells resulted in the loss of detectable targeting to constitutive heterochromatin in interphase and meta-phase [38]. This redistribution could explain the hypomethylation of Sat2 in the juxtacentromeric constitutive heterochromatin of these two ICF patients [28] despite the persistence of methyltransferase activity in vitro [38].
The functional importance of the non-catalytic roles of DNMT3B/Dnmt3b was illustrated by studies of differentiation of rat pheochromocytoma cells (PC12) into neuronal cells. Induction of differentiation in PC12 cells mediated by nerve growth factor was inhibited by antisense or small interfering RNA (siRNA) for Dnmt3b [41]. This inhibition could be largely reversed by transfection with a plasmid encoding Dnmt3b, either wild-type or mutated in the C-terminal catalytic domain so as to inactivate catalytic activity, but not by mutants missing the central ATRX domain or N-terminal PWWP domain. One of the non-catalytic, neuronal differentiation-related targets of the Dnmt3b is the T-cadherin promoter whose activity was repressed by Dnmt3b irrespective of this promoter's methylation status [42].
Generally, mutant DNMT3B proteins from ICF cells are still able to engage in normal protein–protein interactions [34]. One exception is an ICF mutation that altersthe amino-terminal region of DNMT3B's catalytic domain, and, in amouse mutant interferes with acatalysis-enhancing interaction of Dnmt3a and Dnmt3b [17]. The other exceptions are two mutations in the C terminal half of DNMT3B that did not appreciably reduce catalytic activity but did greatly reduce its interaction with Dnmt3L [43] (see below). These exceptions further implicateloss of DNA methylation, and not some other biological activity of DNMT3B, as the upstream molecular defect causing the ICF syndrome.
Stimulation of DNMT3B catalytic activity by interaction with DNMT3L
There is a specific DNMT3L interaction domain located in the C-terminus of Dnmt3b/DNMT3B [44]. DNMT3L is anon-catalytic protein needed for establishment of DNA methylation patterns in the germline, including maternal methylation imprinting and normal levels of methylation of satellite DNA sequences [20]. DNMT3L stimulates the catalytic activity of Dnmt3a and Dnmt3b methyltransferases [45]. This may involve contact of DNMT3B and DNMT3L leading to a changes in the higher-order organization of DNMT3B, just as DNTM3L reorganizes the oligomerization of the DNMT3A2 isoform of DNMT3A [46]. Importantly, two ICF-associated DNMT3B mutations (A766P and R840Q) that result in proteins with approximately wild-type basal methylation activity exhibit decreased association with DNMT3L and a strong decrease in stimulation by DNMT3L [43]. These results implicate interaction of DNMT3B with DNMT3L as critical for normal DNA methylation that is protective against the ICF phenotype.
ICF type 2: Not associated with DNMT3B mutations
About 40% of ICF patients have no mutations in exons of DNMT3B [7, 10]. There might be mutations in the promoter or other transcription control elements or mutations affecting splicing or polyadenylation. However, for several of these ICF patients without detected DNMT3B mutations, the most common isoform of DNMT3B RNA was still observed [7], and for the one patient examined in two putative promoter regions of DNMT3B, no mutations were found [8]. Moreover, mRNA froman ICF patient without detected mutations in DNMT3B was examined by RT-PCR with primers or amplicon sizes specific for several of the DNMT3B RNA splice variants 3B4, 3B3, and3B1 [47]. No evidence for pathogenic alterations in DNMT3B splicing patterns was uncovered.
ICF patients without DNMT3B coding region mutations seem to be derived from a different subtype of the disease. Lymphocytes or fibroblasts from all nine patients in this category displayed hypomethylation in satellite α (centromeric; Figure 1) DNA while all five examined patients who had mutations in DNMT3B did not have the pericentromeric DNA hypomethylation extending into the centromere [7]. ICF patients without mutations in DNMT3B exhibit the same Sat2 hypomethylation and chromosomal anomalies at 1qh and 16qh in mitogen-stimulated cells seen in patients with DNMT3B mutations [8, 13, 14, 48].
Variability of clinical aspects
Immunodeficiency
The immunodeficiency displayed by ICF patients, despite the presence of B cells, results in severe recurrent infections of ten seen in early childhood [49–51]. ICF immunodeficiency is variable ranging from agammaglobulinemia to a mild reduction in immune response [10, 52]. In one study, 27 out of 44 patients presented with agammaglobulinemia although they had B cells in the peripheral blood [10]. All but one of the rest hadhypogammaglobulinemia, one with selective I gA, two with I gM, and one with I gG2 subclass deficiency. Normal percentages of T cells were observed in 36 of 38 ICF patients, the expected stimulation of T-cell proliferation in 25 of 28 tested patients, and CD4+ cells were decreased in only five of 38 patients.
Other symptoms
The dysmorphic facial features of ICF are variable, usually mild [50, 53], and frequent [10]. The typical facial features are abroad flatnasal bridge, hypertelorism (very widely spaced eyes), epicanthic folds and low-set ears. Less frequent but still often associated with the syndrome are micrognathia (small jaw) and macroglossia (protrusion or enlargement of the tongue) [6, 28, 53–56]. Failure to thrive and low birth weight are observed in about half of the patients [10]. Mental retardation and neurologic defects have been seeninabout one-third of the patients [10, 50, 53, 57]. Other congenital abnormalities in ICF are highly variable being observed in one or a few patients. These include bipartite nipples [57], skin pigment changes [12, 57, 58], scleral telangiectasias [57], inguinal hernia and cleft palate [10].
How similar are the Dnmt3b mutant mice to human ICF patients?
Two missense ICF mutations were introduced into both Dnmt3b alleles in mice by homologous loxP/cre-driven recombination [17]. Both affect the catalytic domain in the C-terminal portion of the protein [2, 4]. Three ICF-related transgenic mouse lines were generated that were homozygous for one or the other of these Dnmt3b mutations or the compound heterozygote.
The missense Dnmt3b mutant mice went to term unlike the equivalent Dnmt3b homozygous null mice, which died between 13.5 and 16.5 day post coitum [17]. Most of the missense mutant mice died within 1 day of birth although some survived through to adulthood. Those that survived displayed low birth weight and facial anomalies (shorter nose and wider nasalbridge) reminiscent of the ICF syndrome. Although their immune system was abnormal, the identified abnormality was in the T-cell lineage. One or two days after birth, they had reduced amounts of thymocytes, apparently due to apoptosis, and high levels of fragmented nuclei in the thymus. In contrast, the immunodeficiency of ICF patients only in frequently involves decreased levels of T cells [1, 10] but always is characterized by reduced levels of one or more of the types of immunoglobulins. Normal levels of B cells were observed in these mice as is usually the case for ICF patients.
As described above, only ICF Type 2 patients (who do not display DNMT3B mutations) exhibit hypomethylation of centromeric satellite DNA (Figure 1). The Dnmt3b missense mutant mice displayed hypomethylation of murine minor satellite DNA, which is centromeric, as well as of major satellite DNA, which is juxtacentromeric [17]. No mention was made in this study of chromosomal rearrangements. However, in an earlier report from this group, aneuploidy, polyploidy and numerous breaks and fusions in chromosomes were observed in murine embryonic fibroblasts with double knockout of Dnmt3b [59]. This is very different from the chromosomal abnormalities in ICF, which do not include aneuploidy or polyploidy, and are localized almost exclusively to the juxtacentromeric heterochromatin of only afew chromosomes, those with long regions of Sat2 [1, 14] (see below). Therefore, the DNA hypomethylation and chromosomal abnormalities in mice with Dnmt3b mutations or derived cell cultures is more extensive (including centromeric as well as juxtacentromeric DNA) than in the DNMT3B-mutant ICF syndrome in humans, even when comparing the same DNMT3B mutations, and the nature of the immune dysfunction is different. These differences between species in a disease that most prominently affects satellite DNA-rich heterochromatin are not surprising. Mice do not have Sat2- or Sat3-like sequences in their genome, where so much of the ICF DNA hypomethylation is concentrated [60]. Moreover, murine chromosomes are acrocentric, rather than mostly metacentric, as for human chromosomes, including those harbouring most of the Sat2 or Sat3 DNA. At the end of this review, we will discuss our hypothesis that Sat2 hypomethylation plays an indirect causative role in ICF.
ICF DNA hypomethylation and relationship to cancer
ICF DNA hypomethylation
Juxtacentromeric satellite DNA in normal somatic tissues is generally highly methylated [61]. The hypomethylation of satellite DNA sequences in ICF cells at 1qh, 9qh, 16qh, and Y qh appears to be an invariant characteristic of ICF as detected by Southern blot analysis with CpG methylation-sensitive restriction endonucleases and by immunocytochemistry with anti-m5C antibodies [13, 14, 60]. By bisulfite based genomic sequencing, Sat2 in ICF lymphoblastoid cell lines (LCLs) and fibroblast cell strains was found to have aboutone-third the methylation of analogous controls [62]. The controls had an average of 69% methylation of CpG dinucleotides. By hairpin genomic sequencing, we recently showed that normal somatic tissues have averages of 81, 12 and 7% symmetrically methylated, symmetrically unmethylated and hemimethylated CpG dyads, respectively (C. Shao, M. Lacey, and M. Ehrlich, submitted).
In addition to Sat2 and Sat3, satellite DNA at Yqh is hypomethylated in ICF cells [13, 60]. A nother class of ICF-hypomethylated heterochromatic sequences is in facultative heterochromatin, the inactive X chromosome of females(Xi) [60, 63, 64]. Hypomethylation of examined CpG islands on the X chromosome has been found in some, but notall, ICF patients on their Xi [1, 51, 63]. ICF-related Yqh and Xi hypomethylation is unlikely to be of biological significance because no gender-specific differences in symptoms have been reported for this disease, and, for Xi genes, the hypomethylation is often inconsistent from patient to patient. Analysis of methylation of imprinted genes in ICF has not revealed any gene region with consistent hypomethylation among examined patients [52]. Therefore, these gene regions too are unlikely to contribute to the ICF phenotype.
By HPLC analysis of DNA digests, we demonstrated that the hypomethylation of the genome in ICF involves only arather small percentage of the 5-methylcytosine residues, namely 7% hypomethylation in brain DNA [14]. W e confirmed that the methylation abnormality of ICF is confined to asmall fraction of the genome by two-dimensional electrophoresis of restriction digests of DNA from four ICF vs. four control LCLs [65]. Only 13 of the approximately one thousand spots displayed consistent ICF-specific differences, and all but one of these was derived from NBL2 and D4Z4t and emrepeats. These repeats are dissimilar from each other and from Sat2 or Sat3 in sequence, G + C content, and chromosomal location (acrocentric, subtelomeric, or juxtacentromeric) despite their common ICF hypomethylation [65–67]. That only alimited amount of consistent DNA demethylation is associated with ICF, and mostly in DNA repeats, should be taken into account in models of how DNMT3B mutation gives rise to the disease.
Sperm DNA hypomethylation: Similarities with ICF and cancer DNA hypomethylation
Normal human sperm display shypomethylation in juxtacentromeric Sat2 and Sat3, subtelomeric D4Z4 arrays, and acrocentric chromosomal NBL2 sequences as do ICF cells and somatic tissues [13, 61, 62, 65, 66]. Unlike ICF Type 1, but like Type 2 and a very high percentage of cancers, sperm also displays hypomethylation of centromeric Satα sequences [68, 69]. Sat2, D4Z4, and NBL2 exhibit less methylation in purified normal sperm than do ICF cells [14, 67] (unpub.data).
In mice, juxtacentromeric (major satellite) and centromeric (minor satellite) repeats are hypomethylated in both oocytes and sperm [70]. Imprinted genes and high-copy interspersed repeats are differentially methylated in sperm vs. oocyte DNA [71, 72]. Accordingly, there are differences in the prevalence of transcripts for Dnmt3b, Dnmt3a, Dnmt1, Dnmt1s (a Dnmt1 splice variant), and Dnmt3L during the course of gametogenesis in the male vs. the female germline [21].
Given the involvement of DNMT3B in the ICF syndrome and ICF-linked hypomethylation of the above described tandem repeats, it is clear that this enzyme is necessary during development for normal methylation of these sequences in human somatic cells. The low but appreciable levels of methylation in these repeats in ICF somatic cells, which are higher than those of sperm, might be due to either DNMT3A and/or residual DNMT3B activity. The restructuring of chromatin composition during spermatogenesis [73] might inhibit access of satellite DNA and other large tandem repeats to DNMT3B or facilitate access to as yet uncertain DNA demethylation machinery [74, 75] so as to explain the low levels of methylation of these sequences in sperm.
Frequent increases in methylation of some DNA sequences and decreases in methylation of others are seen in a wide variety of cancers [61]. There is often more hypomethylation than hypermethylation of DNA during carcinogenesis, leading to a net decrease in the genomic 5-methylcytosine content [76]. A lthough the exact methylation changes between different cancers of the same type are not the same, there are cancer type-specific differences in the frequency of hypermethylation or hypomethylation of certain genomic sequences. These opposite types of DNA methylation changes appear to be mostly independent of one another, although they may arise because of a similar abnormality leading to long-lasting epigenetic instability in cancers [77]. Evidence of hypermethylation of some DNA sequences in ICF has been sought but has not been found. Therefore, unlike cancers, ICF DNA has exhibited only hypomethylation.
ICF chromosomal rearrangements and relationship to rearrangements in cancer
ICF-type chromosomal rearrangements
Diagnosis of ICF usually involves cytogenetic detection of chromosome rearrangements targeted to Sat2-rich 1qh and 16qh [9, 53] (Figure 1). Standard metaphase analysis of mitogen-stimulated lymphocytes from peripheral blood of ICF patients reveals predominantly chromosome breaks, whole-arm deletions, multi-branched chromosomes with upto ten arms of Chr1 and/or Chr16, and, less frequently, translocations, and isochromosomes (usually containing two 1q arms fused in the juxtacentromeric region) [1, 53]. Frequently, there is decondensation in 1qh or 16qh in ICF LCLs or stimulated lymphocytes [14, 78]. This decondensation is probably related to the shift in replication timing of Sat2 from mostly G2/M and very late in S phase and towards more of the Sat2 replicating in S phase, including in intermediate stages of S phase [62].
The decondensation of 1qh and 16qh in ICF lymphoblastoid cells is likely to be critical to the ICF-type rearrangements in these regions. Indirect evidence for more frequent somatic paring of 1qh and 16qh in ICF lymphocytes than in control lymphocytes was reported [79]. In ICF LCLs, multiradials composed of arms of both Chr1 and Chr16 had been shown to be favoured over homologous associations [14]. We had proposed that those multiradials represent unresolved Holliday junctions. In collaboration with David Gisselsson, we analyzed chromosome dynamics at mitosis and the frequency of genomic imbalances in ICF LCLs [80]. Consistent with our model, the results suggest that illegitimate recombination of heterochromatic sequences at interphase due to increased 1qh and 16qh associations in ICF LCLs leads to severe perturbations at mitosis.
DNMT3B co-localizes throughout mitosis with components of the chromosome condensation machinery (hSNF2H, KIF4A, hCAP-C, and hCAPG) in HeL a cells [35]. These proteins were associated with Sat2 and rDNA in interphase as determined by chromatin immunoprecipitation of a control LCL, although the extent of association was not quantitated. In ICF LCL s, one of these proteins, hSNF2H, was tested for its association with DNMT3B and found to still coprecipitate with the mutant DNMT3B [34]. Nonetheless, these proteins and HP1, which is highly concentrated in G2-phase ICF lymphoblasts in an anomalous giant nuclear body containing Sat2 DNA [40], might have a role in the ICF-specific chromosomal abnormalities at 1qh and 16qh.
Because a DNMT inhibitor can give distinctive ICF-like rearrangements in apro-B-cell line, including multiradial chromosomes [29, 30] and can cause decondensation of constitutive heterochromatin [81], it is likely that ICF-linked Sat2 hypomethylation contributes to the ICF-associated 1qh and 16qh abnormalities. Other studies of human lymphocytes and B-cell lines also support a relationship of DNA hypomethylation per se and ICF-type chromosomal abnormalities [82, 83] as does the association of juxtacentromeric DNA demethylation and chromosome rearrangements in cancer (see below). Nonetheless, hypomethylation of satellite DNA in constitutive heterochromatin in ICF cells does not suffice to promote rearrangements because the long 9qh region (Figure 1) with its Sat3 hypomethylation in ICF only very infrequently displays rearrangements in mitogen-stimulated lymphocytes from ICF patients [9, 14]. The even longer Yqh region (Figure 1), which also is hypomethylated in ICF cells [13], has not been reported to be susceptible to rearrangement in ICF cells.
Moreover, the cell type and cell growth conditions influence the association of rearrangements with Sat2 hypomethylation. While Sat2-hypomethylated chorionic villus cultures have an increased frequency of these rearrangements, they are only seen in a very low percentage of the metaphases in cultures at low passage numbers [84]. That frequency increases dramatically at higher passages. In ICF cells, the frequency of chromosomal rearrangement sat1qh and 16qh depends on cell growth [1, 9]. In vitro mitogen stimulation of lymphocytes greatly increases the development of these aberrant chromosomes independent of its role in inducing cycling. A much higher frequency of juxtacentromeric (pericentromeric) rearrangements of Chr1 and Chr16 per metaphase is seen 72 or 96h after mitogen stimulation of ICF lymphocytes than at 48h, although the frequent abnormal decondensation of 1qh and 16qh can be observed in metaphases at 48 h [12, 53, 85]. The rearrangements observed in mitogen-stimulated ICF lymphocytes and in untreated ICF LCLs may occur in vivo, but at a very low rate, as deduced from studies of micronucleus formation in unstimulated bone marrow and lymphocytes from ICF patients [53, 58, 86]. The viability of ICF patients and cell-type specificity of the disease, mostly an immunodeficiency disease, indicates that a generalized breakdown in 1qh and 16qh chromatin stability is not manifest throughout the tissues of ICF patients.
Relationship of chromosomal rearrangements in ICF to similar rearrangements in cancer
ICF-type chromosome rearrangements have been seen in cancers [87]. Chr1/Chr16 multiradial chromosomes, which are expected to be very short-lived structures [14], and decondensation in Sat2-rich 1qh have been observed in multiple myeloma and hepatocellular carcinomas [88, 89]. In urothelial carcinomas and glioblastomas, there is evidence for an association of DNA hypomethylation with juxtacentromeric chromosomal rearrangements [90, 91]. Unbalanced Chr1 and Chr16 juxtacentromeric rearrangements are over represented in a wide variety of cancers [92]. The unbalanced nature of these rearrangements could foster tumorigenesis by resulting changes in copy number of oncogenes or tumor suppressor genes [61]. Studies of mice with genetically engineered DNA hypomethylation due to hypomorphic mutations in Dnmt1 provide further evidence that DNA hypomethylation can predispose to chromosome rearrangements [93].
Cancer incidence in ICF patients
Studies from DNA-hypomethylated mice give evidence of a causal relationship between genomic hypomethylation and cancer, but only certain types of cancer [77, 94]. Although ICF had not been associated with cancer, fewer than 50 patients (mostly children) have been identified. Their usually very short average lifespan would preclude detection of a cancer predisposition that was not very high and did not result in tumors rather quickly. However, recently an ICF patient of 7 years was reported to have Hodgkin lymphoma [95], and previously an unrelated ICF patient was described as having an adrenocortical adenoma [8]. The normal or heightened DNA damage response observed in ICF lymphocytes [96] might help explain why tumors have not been found more frequently in ICF patients compared to patients with shortlife expectancies due to several other rare chromosomal in stability syndromes [97].
Altered gene expression in ICF lymphoblastoid cells
Overview of ICF microarray expression analyses
Because ICF patients can have very large decreases in specific serum immunoglobulins despite the usually normal levels of B cells [5, 10], transcriptional dysregulation in B cells or both B and T cells is likely to be the predominant cause of their immunodeficiency. We showed that ICF LCLs have plentiful surface IgM and normal IgM RNA levels [5] despite extremely low levels of serum IgM. Therefore, the immune defect in ICF occurs at a step prior to class switching. It was suggested that peripheral blood-derived B cells and BLCLs in ICF patients may display an altered expression pattern only as result of being less mature than their normal counterparts [98]. However, the absence of detectable IgM in serum from 12 out of 45 patients [10] indicates an intrinsic defect in B cells in ICF patients. Moreover, the differences in the expression patterns of ICF LCLs compared to control LCLs described below argue for more than just a loss of maturity of B cells. For example, we found significant differences in RNA levels in ICF vs. control LCLs for some genes expressed only in mature B cells, others known to be expressed mainly in the T-cell lineage, and yet others with no known or expected relationship to lymphogenesis.
We did two microarray expression experiments on ICF and control LCLs. They involved B-cell lines from ICF patients with known and diverse DNMT3B mutations and from controls, including phenotypically normal parents of the patients. In the first study, total RNA (cRNA) from ICF LCLs derived from five different patients and five control LCLs were examined on oligonucleotide arrays for ∼8400 genes (Affyarray HuGene FL, Affymetrix) [5]. The fold change (FC) was determined, namely, the relative RNA signal levels in ICF vs. control or control vs. ICF. About 0.3% of the genes were found to be up- or down-regulated at a significance level (two-sample t-test) of P < 0.05 and FC > 2.0 or P < 0.01 and FC > 1.5. In the second experiment, eight ICF and seven control LCLs, including five and two from the first study, respectively, were analyzed on oligonucleotides arrays representing >33,000 genes (Affyarray U133A and B arrays). In this analysis, ∼1% of the genes showed an FC > 2 (up- or down-regulation) and P < 0.01 for ICF-specific differences in RNA levels. Dysregulation involved 120 probesets that were down-regulated and 229 up-regulated.
The summary data for 20 of these genes of interest from the second experiment are shown in Tables I and II. Nine were also found to be dysregulated in the first microarray experiment and eight were similarly up- or down-regulated in two different probe sets in the second experiment. By quantitative real-time RT-PCR (qRT-PCR), we verified that the following RNAs were overexpressed in eight ICF LCLs compared to eight control LCLs: the transcription factor NR2F2 (COUP-TFII); SMARCA2 (BRM), encoding a SNF2 subunit of a chromatin remodelling complex; PRKCH and PTPN13 (FAP-1), which regulate apoptosis; GUCY1B3 and GUCY1A3, which encode the two subunits of a soluble guanylate cyclase, and CD44 and CKLF, which are implicated in the later stages of B-cell development. Although the terms up- or down-regulation are used, a caveat is that differences in post-transcriptional processing are sometimes responsible for changes in the steady-state levels of RNA, the parameter monitored in these studies.
Table I.
Immune system-related genes with significant differences in RNA levels in ICF vs. control lymphoblasts.
| Microarray dataa | qRT-PCR datab | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Abbreviated gene name | Ref seq. ID or other ID | Chrom. location | Description | Array expt. no. | Mean for ICF | Mean for controls | FC | P-value from t-test | FC | P-value from t-test |
| IGHG3 | M87789 | 14q32.33 | Immunoglobulin heavy constant gamma 3 | 1 | 291 | >18,600 | −60 | 0.004 | NA | |
| 211647_x_at | Ig rearranged mu-chain gene V-N-D-N-J-region, complete cds | 2 | 62 | 8765 | −100 | 2 × 10−8 | ||||
| NT5E (CD73) | NM_002526 | 6q14-q21 | 5′-Nucleotidase, ecto; hydrolyzes extracellular nucleotides; intracellular signalling, lymphocyte proliferation, activation, and cell cohesion; much greater activity in mature than immature B and T cells | 2 | 377 | 158 | +2.4 | 0.005 | NA | |
| MAP4K4 | NM_145687 | 2q11.2 | Mitogen-activated protein kinase kinase kinase kinase 4; role in T-cell antigen-mediated responses, in cell motility, and in TNF-α/JNK and p53 signalling pathways | 2 | 890 | 14 | +18 | 0.001 | NA | |
| CASP1 | NM_033292 | 11q22.3 | Caspase 1, apoptosis-related cysteine peptidase (interleukin 1, beta, convertase); in B cells, activation of NF-κB and MAPK14 | 2 | 961 | 333 | +3.0 | 0.009 | NA | |
| CD27 | NM_001242 | 12p13 | Tumor necrosis factor receptor; family, member 7 (TNFRSF7); T-cell and B-cell proliferation response to antigens; somatically mutated, germinal center, memory, and plasma cells | 1 | 1439 | 2890 | −2.0 | 0.04 | NA | |
| 2 | 1552 | 3081 | −2.0 | 0.03 | ||||||
| ITGB2 (CD18) | NM_000211 | 21q22.3 | Integrin, beta 2 (complement component 3 receptor 3 and 4 subunit); cell surface adhesion receptor involved in B-cell differentiation and homing | 2 | 1046 | 357 | +2.9 | 0.03 | NA | |
| CD44 | NM_000610 | 11p13 | CD44 antigen; attachment to endothelial cells and homing to peripheral lymphoid organs and sites of inflammation; naïve and memory B cells, not on germinal center B cells | 2 | 4651 | 1438 | +3.2 | 0.005 | +3.5 | 0.01 |
| CD40 | NM_001250 | 20q12-q13.2 | Tumor necrosis factor receptor superfamily, member 5; interaction with its T-cell ligand needed for B-cell proliferation, differentiation, isotype switching, humoral memory response; mature B cells | 2 | 1460 | 487 | +3.0 | 0.01 | NA | |
| CKLF | NM_016326 | 16q22.1 | Chemokine-like factor; chemotaxis; upregulated in activated T cells but not in B cells; very high expression in testes | 2 | 1599 | 351 | +4.6 | 0.003 | +3.3 | 0.03 |
The first [5] and second experiments on ICF vs. control B-cell lines were done similarly on HuGene FL and HG-U133 microarrays, respectively (Affymetrix). The ICF LCLs for Expt. #2 were those in Expt. #1 (only one of the two ICF B stocks) with three additional LCLs, patients 1 and 3 from one study [29] and patient 5 from another [6]. The control LCLs for Expt. #2 were from the mothers and fathers of patient ICF B and C and AG15022 and AG14953 (Coriell Institute). A positive fold change (FC) denotes RNA overexpression in ICF and is the mean signal for ICF divided by that for the controls for that probe set. A negative FC indicates underexpression in ICF and is the negative of the mean signal for controls divided by that for ICF. P-values are for two-sample t-tests to evaluate the significance of ICF-associated increases or decreases in mean RNA levels relative to the controls. For IGHG3, PRKCH, CD44, and CKLF, another probe set in the microarray gave similar results in Expt. #2 (not shown);
Real-time quantitative RT-PCR (MyIQ Cycler and iQ SYBR Green Supermix, Bio-Rad) was done on all the ICF LCL samples used for Expt. #2 and 6–12 control LCLs (including additional B-cell lines) that were prepared from random hexanucleotide or oligo(dT)-primed cDNA. Primers were designed for the HG-U133 microarray probe regions and optimal annealing temperatures for PCR were determined by gradient PCR. The data were normalized to those from GAPDH. The fold change is described as for the microarray data. The P-values are for the differences in the mean RNA levels using log-transformed data. NA, not assayed.
Table II.
More genes with significantly altered RNA levels in ICF vs. control lymphoblasts.
| Microarray dataa | qRT-PCR dataa | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Gene symbol | Ref seq. ID | Chrom. location | Description | Array expt. no. | Mean for ICF | Mean for controls. | FC | P-value from t-test | FC | P-value from t-test |
| PRKCH | NM_006255 | 14q22-q23 | Protein kinase C, eta; calcium-independent and phospholipid-dependent; a PRKCH cleavage product is implicated in apoptosis in pro-B cells but expression in T cells is much higher than in B cells; expression correlated with NO production | 1 | 379 | 100 | +3.8 | 0.04 | ||
| 2 | 2301 | 170 | +13.6 | 0.003 | +6.5 | 0.04 | ||||
| GUCY1A3 | NM_000856 | 4q32.1 | Guanylate cyclase 1, soluble, alpha 3; heterodimerizes with beta subunit to give an enzyme (sGC) strongly activated by NO | 1 | 233 | 101 | +2.3 | 0.03 | ||
| 2 | 1193 | 417 | +2.9 | 7 × 10−5 | +6.8 | 4 × 10−6 | ||||
| GUCY1B3 | NM_000857 | 4q32.1 | Guanylate cyclase 1, soluble, beta 3; heme-containing subunit of sGC; MAPK13 is a downstream effector and HMOX1 is upstream | 1 | 1316 | 292 | +4.5 | 0.007 | ||
| 2 | 3759 | 782 | +4.8 | 0.001 | +10.6 | 1 × 10−5 | ||||
| HMOX1 | NM_002133 | 22q13.1 | Heme oxygenase (decycling) 1; ubiquitious transcriptionally inducible stress protein; degrades heme; generates CO for anti-proliferative effects on T cells | 1 | 577 | 2353 | −4.1 | 0.03 | ||
| 2 | 864 | 1559 | −1.8 | 0.009 | NA | |||||
| MAPK13 | NM_002754 | 6p21.31 | Mitogen-activated protein kinase 13; stress activated kinase; activated by PRKCH during regulation of keratinocyte differentiation; downstream in the sGC pathway; is pro-apoptotic; implicated in antigen-meidated T-cell responses | 2 | 388 | 104 | +3.7 | 0.006 | NA | |
| PTPN13 | NM_080683 | 4q21.3 | Protein tyrosine phosphatase, non-receptor type 13 (APO-1/CD95 (Fas)-associated phosphatase); both anti- and pro-apoptic effects; IκBα is a substrate; high expression in placenta and testis | 1 | 271 | 41 | +2.7 | 0.02 | ||
| 2 | 623 | 53 | +12 | 1 × 10−7 | +5.0 | 0.02 | ||||
| BCL2L10 | NM_020396 | 15q21.2 | BCL2-like 10 (apoptosis facilitator); both anti- and pro-apototic | 2 | 560 | 184 | +3.0 | 0.002 | NA | |
| CNN3 | NM_001839 | 1p22-p21 | Calponin 3, acidic; actin-binding protein; low expression in leukocytes | 1 | 407 | 80 | +4.1 | 0.008 | NA | |
| 2 | 1046 | 357 | +2.9 | 0.03 | ||||||
| SLC1A1 | NM_004170 | 9p24 | Solute carrier family 1 (neuronal/epithelial high affinity glutamate transporter) | 1 | 137 | 237 | −1.7 | 0.001 | NA | |
| 2 | 716 | 1493 | −2.1 | 0.007 | NA | |||||
| NR2F2 | NM_021005 | 15q26.2 | Nuclear receptor subfamily 2, group F, member 2; COUP-TFII; negative post transcriptional regulator of MYOD1 | 2 | 824 | 91 | +9.0 | 0.003 | +2.9 | 0.005 |
| SMARCA2 | NM_003070 | 9p24.3 | SWI/SNF related, matrix associated, subfamily a, member 2; BRM; chromatin remodelling | 2 | 2814 | 1250 | +2.1 | 0.002 | +3.3 | 0.004 |
See the footnotes to Table I. Two probe sets each for GUCY1B3, CNN3, SMARCA2, and BCL2L10 in microarray Expt. #2 gave similar results.
Twelve genes with significant differences from the microarray data between ICF and control LCLs were then tested by RT-PCR. Only one of these did not exhibit RT-PCR results concordant with the micro-array results (data not shown). In addition, one gene, RGS1, which displayed ICF-specific changes in its RNA levels only in the first microarray experiment, did not show significant differences in RNA levels in ICF vs. control LCLs by qRT-PCR (data not shown). Some other genes also displayed significant differences in RNA levels between ICF and control LCLs only in the first experiment [5]. However, the microarray for the first experiment was smaller, the gene annotation was much less thorough, and the probe sets were different from those in the second experiment (usually 20 oligonucleotides per set in the first experiment and 11 in the second). These factors and the absence of some of the probe sets or the apparently poorer hybridization of others can explain why some of the genes that appeared to be significantly dysregulated in ICF LCLs compared to controlLCLs in the first array experiment were not seen as dysregulated in the second.
In view of the extreme scarcity of ICF patients and their median age of 8 years at death [10], we examined Epstein Barr virus-transformed B-cell lines rather than lymphocytes. The activation associated with this transformation might hide some in vivo defects in B-cell activation in ICF patients and only asubset of B cells will be transformed. Nonetheless, we found much consistency in LCLs from eight unrelated patients and new insights into transcriptional regulation of the immune system.
Genes with lymphocyte functions that had altered RNA levels in ICF LCLs
The most dramatic difference in RNA levels in ICF vs. control LCLs was seen for IGHG3 (Table I). This was expected based upon results given results from the patient sera and surface immunoglobulin expression [5]. The second largest difference in RNA levels in disease compared to control LCLs in Table I or II was observed for MAP4K4, which has been implicated in antigen-mediated T-cell activation [99] but not in B-cell function. This ubiquitously expressed kinase participates in the JNK/TNF-α and p53 signalling pathways and can be controlled at the level of transcription [100–102]. The maximum microarray signal for MAP4K4 in the control LCLs in the second microarray experiment was 46 while, with the exception of one LCL (ICF K), the ICF LCLs had much higher signals (371, 2893, 295, 291, 1856, 348 and 1060). MAP4K4 seems to have abroad role in fostering cell migration [103]. A nother gene whose RNA was upregulated in ICF vs. control LCLs was NT5E, which was found to be expressed mostly in B cells, rather than T cells, and usually only after isotype switching [104].
CD27, which plays a key role in T-cell memory and in the stimulation of B cells to produce immunoglobulins [105], had lower mRNA levels in ICF LCLs relative to control LCLs (Table I). This is consistent with ICF immune dysfunction. The ability of peripheral blood-derived B cells (CD19+) to express cell-surface CD27 after stimulation [98] makes the down-regulation of its RNA in ICF lymphoblastoid cells unlikely to be causally involved in ICF immunodeficiency. While CD40, CD44, CKLF and ITGB2 (CD18) mRNAs were significantly upregulated in ICF vs. control LCLs, their positive functions in lymphogenesis [106–112] make them unlikely candidates for active players in the immunodeficiency of ICF patients. Some gene candidates for interfering with later stages of B-cell differentiation or activation did not display significant differences in RNA levels in ICF vs. control LCLs in the microarray analysis, namely, BTK, PRDM1, PAX5, IRF4, BCL6, XBP1, BACH2 and MAPBPIP.
Cell death or growth arrest genes that had altered RNA levels in ICFLCLs
Genes involved in cell death or arrest of the cell cycle may be important contributors to the immune dysfunction of ICF patients. CASP1, BCL2L10, PTPN13, HMOX1, MAPK13 and PRKCH, which displayed ICF-specific differences in their RNA levels, might be involved in abnormal regulation of apoptosis or cell cycle arrest in lymphoid cells in ICF patients (Tables I and II). However, major decreases in numbers of lymphocytes are not usually found to be associated with ICF. Low levels of T cells are present in only half of ICF patients and the levels of B cells are even less likely to be lower than normal in ICF patients and are never undetectable [1, 9]. Nonetheless, too much cell death induced by B-cell activation just in the later stages of B-cell development could lead to the loss of plasma cells and decreased serum immunoglobulin without compromising total levels of B cells.
CASP1 (Table I) is a cytokine involved in a variety of inflammatory processes, including the proteolytic maturation of the inactive precursor of the inflammatory cytokines interleukin-1 (IL1) and IL18 [113]. It is pro-apoptotic in various cell types and may be associated with IgA deficiency and increased apoptosis in B cells [114]. Therefore, the observed increased levels of CASP1 RNA in ICF vs. control LCLs are consistent with the heightened susceptibility of ICF lymphoid cells to apoptosis [80, 86, 115, 116]. Over-expression of CASP1 RNA in ICF cells could also perturb NF-κB signalling pathway simpacting expression of other genes (see below). Underexpression of RNA for the anti-apoptotic HMOX1 stress protein and overexpression of MAPK13 and PRKCH RNA in ICF vs. control LCLs (Table II) might also contribute to pro-apoptotic tendencies of ICF lymphoid cells.
There was significantly more BCL2L10 RNA in ICF LCLs compared to control LCLs (Table II). This widely expressed member of the BCL2 family has a polypeptide structure compatible with both pro-and anti-apoptotic effects depending on the cell type and conditions [117]. It appears to be a negative regulator of cell death in humanglioma cells provoking them to exit from the cell cycle [118]. While ICF LCLs were hypersensitive to γ gradiation compared to controls, we demonstrated that this was mostly due to irreversible growth inhibition, secondarily to non-apoptotic cell death, and thirdly to apoptosis [96]. All three of these types of responses to irradiation were significantly more frequent for ICF cells than for control cells despite the functional cell cycle checkpoints in ICF cells.
Given that the main anti-proliferative response of ICF LCLs to γ radiation was not apoptosis, it is noteworthy that PTPN13, a gene with anti-apoptotic effects was overexpressed in mRNA from ICF vs. control LCLs (Table II). This protein tyrosine phosphatase interacts with diverse proteins including the cell death FAS protein [119]. The interaction with FAS decreases the export of FAS to the cell surface and there by opposes the FAS pro-apoptotic activity. PTPN13 may suppress pro-apoptotic signalling also through another interactive partner, a neurotrophin receptor [120]. However, as for BCL2L10, an opposite pro-apoptotic role for PTPN13 has also been reported [121], in this case, involving dephosphorylation of the insulin receptor substrate-1. Northern blotting revealed very strong signals for PTPN13 RNA inplacenta and testes (both tissues with considerable DNA hypomethylation [61, 122]), as well as for kidney; moderate signals in lung and ovary; weak signals in heart, brain and pancreas; and almost nodetectable signal in leukocytes [123]. With the much more sensitive RTPCR assay, PTPN13 RNA was detected in T cells and was found to be decreased upon IL-2 activation although it was more abundantin CD45RO+ memory T cells than in CD45RA + naive T cells [124].
Overlapping upregulation of RNA for kinases and NO or CO signal pathway members
The microarray results suggest that overlapping signal transduction pathways may be critical for the immune dysfunction of the ICF syndrome (Tables I and II). One of these involves the a forementioned CASP1 and PTPN13, whose RNAs were upregulated in ICF vs. control LCLs. In addition to its catalytic function, CASP1 has anon-catalytic role, as activator in B cells of NF-κB and p38MAPK, the MAPK family that includes MAPK13 [125]. An increase in NF-κB signalling is also predicted from increased PTPN13 RNA, because the corresponding protein phosphatase has as one of its substrates IκBα, which inhibits NF-κB [126]. In addition, NF-κB upregulates PTPN13 transcription [119] and plays a critical role in lymphocyte development and function [127, 128].
Another signalling pathway with ICF-specific differences in RNA for several of its members is the carbon monoxide (CO) pathway (Table II). HMOX1, which displayed ICF-specific decreases in RNA levels, catabolizes heme and there by releases gaseous CO, which is responsible for its anti-apoptotic effects [129]. This pathway also involves downstream activation of NF-κB, which, in turn, by promoter interactions, activates transcription from a subset of NF-κB-dependent anti-apoptotic genes [129–131]. Among the diverse effects of CO signalling, it seems to be a modulator of autoimmunity [129].
Another link to the NF-κB signal pathways among the ICF-overexpressed RNAs involves the above mentioned protein kinase C family member, PRKCH. This calcium-independent, serine-and threonine-specific enzyme is activated by diacylglycerol to phosphorylate a wide range of cellular proteins and there by influence many aspects of physiology [132–135]. Un likely most protein kinase C isoforms, transcription of PRKCH is highly tissue specific. Its expression primarily, but not exclusively, in epithelial tissues is probably due to an enhancer, a silencer and trans-acting factors [136]. In skin, PRKCH is associated with terminal differentiation of keratinocytes. Genetic polymorphisms in PRKCH are implicated in increasing the risk of rheumatoid arthritis and cerebral infarction [135, 137]. Overexpression of PRKCH may play a role in tumor progression through downstream ERK and ELK effectors [132]. PRKCH RNA was overexpressed 4- to 14-fold in ICF vs. control LCLs as seen in both microarray experiments and qRTPCR (Table II). It is implicated as a pro-apoptotic protein in early B-cell development [138]. PRKCH RNA was reported to be induced upon lymphocyte activation but was present at much lower levels in B cells than in T cells, whether resting or activated [137]. A mong the processes subject to its regulation, PRKCH helps control the activation of NF-κB upon lipopolysaccharide induction of primary rat astrocytes [133]. PRKCH activity can result in the production of nitric oxide (NO), another important signalling gas, via the inducible nitric oxide synthetase gene (iNOS) [134].
The widespread signalling molecule NO is, in turn, related to GUCY1A3 and GUCY1B3, whose RNAs were upregulated in ICF compared to control LCLs as determined in both microarrays and by qRT-PCR (Table II). GUCY1A3 and GUCY1B3 are the two subunits of the soluble guanylate cyclase (sGC), a heme protein that is a major sensor for NO, thereby regulating diverse physiological processes, [129]. Proliferation of Thelper (Th) 1 cells is controlled by NO levels [139]. Although GUCY1A3 and GUCY1B3 are very close together on 4q32.1, they may not be regulated in a fully coordinate manner [140], as is consistent with our data (Table II). Their heterodimeric products GC is strongly stimulated by NO and weakly stimulated by CO. The NO and CO pathways intersect in various ways at the protein level, including that decreased HOX1 in ICF vs. control LCLs could lead to less HOX1-mediated degradation of the hemeprosthetic group necessary for the GUCY1B3 subunit of sGC [141]. Another pathway intersection of the genesin Tables I and II is that MAPK13 has a prominent role as a downstream enzyme in the sGC signalling pathway [129]. ICF-related overexpression of RNAs for MAPK13 and the two sGC subunits is consistent with their interrelated functioning in cell growth arrest.
Some of the genes in Tables I and II that exhibited ICF-related changes in RNA levels in the B lymphoblastoid cells are much more closely associated with T cells than with B cells. This might reflect coordinate dysregulation in the B-cell and T-cell lineages. For those genes, it might be that only dysregulation in T cells is relevant to the disease or that the role of these genes in B cells is insufficiently appreciated. Alternatively, these changes might contribute to the pathology of ICF because of inappropriate expression of T-cell specific genes in the B-cell lineage.
Dysregulation of genes that may help explain non-immune symptoms of ICF
While the significantly altered RNA levels for some proteins in ICF vs. control LCLs, such as the CNN actin-binding protein, might have no biological consequences, others may be a factor in the nonimmune symptoms of ICF. Although we examined RNA only in BLCLs, abnormal RNA levels in the lymphoid cell lineage might be found in other lineages too and altered regulation in lymphocytes can sometimes mirror more physiologically important dysregulation in a very different tissue [142]. Overexpression of PTPN13 RNA in ICF LCLs (Table II) might pertain to neurological findings in ICF patients because high levels of PTPN13 in fetal brain and its ability to bind to the neurotrophin receptor implicate this protein in controlling neuronal cell death [120, 143]. One of the neurological abnormalities in ICF is seizures, which was reported in three of 45 patients [10]. SLC1A1, a neuronal protein involved in transporting glutamate that is protective against seizures and neuronal death [144], was significantly underexpressed at the RNA level in ICF LCLs relative to control LCLs (Table II). In addition, the observed BCL2L10 RNA dysregulation may be involved in ICF-related neurological disturbances because BCL2L10 mRNA increases appreciably from a very low level during in vitro differentiation of rat astrocytes [145]. Moreover, GUCY1B3 and iNOS are associated with each other in certain areas of the hippocampus in mice [146] and CASP1 overexpression has been linked to cognitive impairment with aging [147].
Upregulation of PRKCH (Table II) may explain a perplexing finding reported in one study of two unrelated ICF patients, both of whom displayed bipartite nipples [57]. PRKCH is implicated in upregulation of many epithelial tissues, including the mammary gland in rats [148]. These associations might account for the occasional specific finding of bipartite nipples in ICF patients.
ICF-associated upregulation of RNA for the chromatin remodelling protein SMARCA2 might impact 1qh and 16qh decondensation. SMARCA2 (BRM) is an important modulator of chromatin assembly [149]. It could also have disparated own stream effects through its impact on transcriptional regulation, DNA repair and homologous recombination.
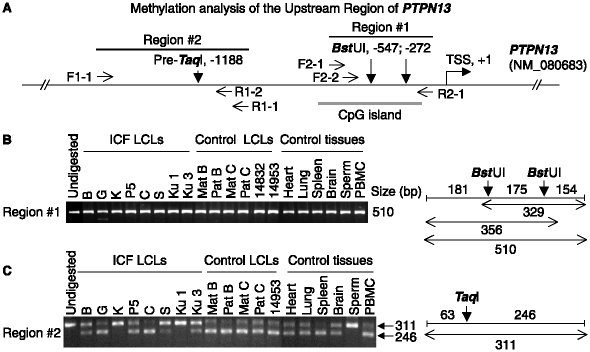
Lack of detectable methylation changes in the promoter regions of examined ICF-upregulated genes
We recently examined methylation of five genes with qRT-PCR-confirmed ICF-associated upregulation of their RNA, namely, GUCY1A3, PTPN13, NR2F2, SMARCA2 and CKLF (Tables I and II). Their 5′ gene region (for GUCY1A3) or upstream regions (for the other genes) were assayed for methylation in ICF and control LCLs as well as in several normal tissues by combined bisulfite restriction analysis (COBRA). COBRA allows quantitation of DNA methylation levels at restriction endonuclease sites in a given DNA sequence that is amplified by PCR [150]. Genes with up-regulation of RNA were chosen because of the frequent association of DNA hypomethylation in promoters with transcription [151]. By COBRA, we saw no consistent ICF-specific differences in DNA methylation in the examined regions despite their ICF-related increases in the levels of the corresponding mRNAs (Figure 2 and data not shown). This was similar to our previous finding for GUCY1B3 in ICF cells [5]. Almost all of the immediate upstream regions were constitutively unmethylated. There were various amounts of partial methylation in their further upstream sequences but no correlations between methylation and RNA levels amongindividual LCLs. Therefore, the differential mRNA levels for these genes in ICF vs. control LCLs could not be explained by differences in methylation in or near their promoters. A caveat in this analysis is that only the top gene in an ICF-activated transcription pathway might have ICF-specific promoter hypomethylation.
Figure 2.
Analysis of DNA methylation upstream of PTPN13. Representative COBRA analysis for DNA methylation of a gene that had RNA upregulated in ICF vs. control LCLs. DNA samples had been modified with bisulfite and amplified by PCR with primers at the indicated positions as previously described [5]. The PCR products could be cleaved by TaqI or BstUI only if they had been methylated at the CpG dinucleotide in the indicated sites in genomic DNA; the pre-TaqI site, CCGA, would be converted to aTaqI site, TCGA, upon bisulfite treatment and PCR if it was Cm5 CGA in genomic DNA. (A) Diagram of the 5′PTPN region showing the transcription start site (TSS) [123] at Chr4 87,734,909 (hg18, UCSC database), the 5′ CpG island (−701 to −150), and PCR primers; positions are given relative to the TSS. (B) and (C), electrophoresis gels stained with ethidium bromide and visualized for fluorescent bands from the PCR products (−628 to −119 and −1250 to −940) digested with Bst UI or Taq I. PBMC, peripheral blood mononuclear cells; ICF LCLs are described in the legend to Table I, with the addition of another control LCL (AG14832, Coriell Institute). Sizes are given in bp for the expected and obtained restriction products.
Hypothesis: The relationship of DNMT3B mutations to the ICF phenotype
Methylation analysis of various genes [51, 52, 63, 64] (Figure 2), and whole-genome restriction analysis [65] have revealed consistent hypomethylation only in tandem DNA repeats (including satellite DNA) and X-linked sequences in Xi. However, unconventional genes, whose broad biological influence has been appreciated only recently (especially micro RNA and anti-sense RNA genes) [152], were not specifically examined. While a critical gene that is hypomethylated specifically in ICF cells may have been missed, we favour a different explanation for the connection of selective DNA hypomethylation to the ICF syndrome. We propose that the pathogenicity of DNMT3B mutations in ICF patients is due to the hypomethylation of constitutive heterochromatin. This same explanation can be applied to patients with ICF type 2, who have no detected DNMT3B mutations but do exhibit the characteristic hypomethylation of juxtacentromeric satellite DNA [7]. Because no gender bias has been reported for ICF, our proposal for the involvement of satellite DNA is limited to the long juxtacentromeric heterochromatin butnot Yqh (Figure 1) nor the facultative heterochromatin of Xi. We favour the involvement of Sat2-containing 1qh and 16qh over Sat3-containing 9qh (Figure 1) because of the more frequent cytogenetic abnormalities in the former regions.
Evidence is mounting that constitutive heterochromatin is biologically important and not just an inert filler in the genome, as many previously thought. In fission yeast and drosophila, transcription of non-coding RNA is important for the establishment of constitutive heterochromatin [153–155]; these organisms have little or no methylation of their DNA [16]. Some, but not all, of various tested normal or cancer samples andhalf of ICF LCLs that we analyzed for Sat2 RNA were positive by RT-PCR (which included controls for DNA contamination) and by assays for RNA polymerase engagement [156]. However, these signals were very low and we did not see the large increase in Sat2 transcripts upon heat shock [156] that is found for 9qh Sat3 transcripts [157].
Besides constitutive heterochromatin yielding non-coding transcripts that might affect expression of protein-coding genes, its intranuclear location may help organize chromatin throughout the nucleus so as to modulategene expression in trans [85]. Evidence for this phenomenon has been reported in the lymphoid lineage [158, 159]. The intranuclear distribution of centromeres in lymphoid cells is distinct for the cell type and stage of differentiation and involves genes associated with lymphogenesis [160]. The importance of the spatial location of chromatin in the nucleus is illustrated by the finding that much gene expression occurs in transcription factories that are specific for different functional groups of genes [161]. Hypomethylation of 1qh, 9qh, and 16qh satellite DNA might influence the distribution of these heterochromatic regions in the nucleus during certain stages in lymphogenesis or lymphocyte activation and there by affect expression from genes on other chromosomes.
Recently, one dramatic change in positioning of hypomethylated constitutive heterochromatin specifically in ICF lymphoblasts and lymphocytes has been described. It is the formation of agiant promyelocytic leukemia (PML) type nuclear body that correlated with under condensed 1qh or 16qh, but not 9qh, in a large percentage of ICF G2 nuclei [39, 40]. All three isoforms of HP1 as well as SP100, SUMO-1, transcription factors CBP and DAXX, the DNA helicase BLM, and the SWI-SNF remodelling protein ATRX co-localize in this single nuclear body. M uch smaller PML-type bodies containing these proteins are observed in G2-phase nuclei of normal cells but the association of 1qh Sat2 DNA with these normal bodies is less frequent than for the giant PML nuclear body in ICF lymphocytes and LCLs. This abnormal concentration of satellite DNA heterochromatin and nuclear proteins in ICF G2-stage lymphoid cells has been proposed to be linked to undercondensation and chromosomal abnormalities at 1qh and 16qh [40]. However, it might also reflect an abnormal distribution of chromatin proteins in interphase that could influence expression of genes else where in the genome.
There are more and more examples of transcription control proteins that bind selectively to constitutive heterochromatin [162–168]. Furthermore, there is evidence that the binding of at least some of these transcription factors to the highly repetitive DNA of constitutive heterochromatin sequesters these proteins in a reversible manner so as to modulate expression of sets of genes [5, 168–172]. Methylation of satellite DNA can dramatically alter binding of certain transcription control proteins to DNA, in general [173] or constitutive heterochromatin [174], in particular. Therefore, pathogenic dysregulation of a subset of genes in ICF might be due to altered transcription factor binding to satellite DNA in response to its disease-related hypomethylation. This would be a new type of DNA methylation control of gene expression in trans mediated by chromatin acting as a dynamic reservoir for storage and possibly delivery of transcription modulatory proteins, which in the case of ICF, might explain the life-threatening immunodeficiency.
Acknowledgments
This research was supported in part by NIH grant CA 81506 and Louisiana Cancer Research Consortium grant.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- [1].Ehrlich M. The ICF syndrome, a DNA methyltransferase 3B deficiency and immunodeficiency disease. Clin Immunol. 2003;109:17–28. doi: 10.1016/s1521-6616(03)00201-8. [DOI] [PubMed] [Google Scholar]
- [2].Hansen RS, Wijmenga C, Luo P, Stanek AM, Canfield TK, Weemaes CM, Gartler SM. The DNMT3B DNA methyltransferase gene is mutated in the ICF immunodeficiency syndrome. Proc Natl Acad Sci USA. 1999;96:14412–14417. doi: 10.1073/pnas.96.25.14412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Okano M, Takebayashi S, Okumura K, Li E. Assignment of cytosine-5 DNA methyltransferases Dnmt3a and Dnmt3b to mouse chromosome bands 12A2-A3 and 2H1 by in situ hybridization. Cytogenet Cell Genet. 1999;86:333–334. doi: 10.1159/000015331. [DOI] [PubMed] [Google Scholar]
- [4].Xu G, Bestor TH, Bourc'his D, Hsieh C, Tommerup N, Hulten M, Qu S, Russo JJ, Viegas-Péquignot E. Chromosome instability and immunodeficiency syndrome caused by mutations in a DNA methyltransferase gene. Nature. 1999;402:187–191. doi: 10.1038/46052. [DOI] [PubMed] [Google Scholar]
- [5].Ehrlich M, Buchanan K, Tsien F, Jiang G, Sun B, Uicker W, Weemaes C, Smeets D, Sperling K, Belohradsky B, et al. DNA methyltransferase 3B mutations linked to the ICF syndrome cause dysregulation of lymphogenesis genes. Hum Mol Gen. 2001;10:2917–2931. doi: 10.1093/hmg/10.25.2917. [DOI] [PubMed] [Google Scholar]
- [6].Wijmenga C, Hansen RS, Gimelli G, Bjorck EJ, Davies EG, Valentine D, Belohradsky BH, van Dongen JJ, Smeets DF, van den Heuvel LP, et al. Genetic variation in ICF syndrome: Evidence for genetic heterogeneity. Hum Mutat. 2000;16:509–517. doi: 10.1002/1098-1004(200012)16:6<509::AID-HUMU8>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- [7].Jiang YL, Rigolet M, Bourc'his D, Nigon F, Bokesoy I, Fryns JP, Hulten M, Jonveaux P, Maraschio P, Megarbane A, et al. DNMT3B mutations and DNA methylation defect define two types of ICF syndrome. Hum Mutat. 2005;25:56–63. doi: 10.1002/humu.20113. [DOI] [PubMed] [Google Scholar]
- [8].Kubota T, Furuumi H, Kamoda T, Iwasaki N, Tobita N, Fujiwara N, Goto Y, Matsui A, Sasaki H, Kajii T. ICF syndrome in a girl with DNA hypomethylation but without detectable DNMT3B mutation. Am J Med Genet. 2004;129A:290–293. doi: 10.1002/ajmg.a.30135. [DOI] [PubMed] [Google Scholar]
- [9].Ehrlich M, Jackson K, Weemaes C. Immunodeficiency, centromeric region instability, facial anomalies syndrome (ICF) Orphanet J Rare Dis. 2006;1:2. doi: 10.1186/1750-1172-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Hagleitner M, Lankester A, Maraschio P, Hulten M, Fryns J, Schuetz C, Gimelli G, Davies E, Gennery A, Belohradsky B, et al. Clinical spectrum of immunodeficiency, centromeric instability and facial dysmorphism (ICF-syndrome) J Med Genet. 2007 doi: 10.1136/jmg.2007.053397. [DOI] [PubMed] [Google Scholar]
- [11].Hulten M. Selectivesomatic pairing and fragility at 1q12 in a boy with common variable immunodeficiency. Clin Genet. 1978;14:294. [Google Scholar]
- [12].Tiepolo L, Maraschio P, Gimelli G, Cuoco C, Gargani GF, Romano C. Multibranched chromosomes 1, 9, and 16 in a patient with combined IgA and IgE deficiency. Hum Genet. 1979;51:127–137. doi: 10.1007/BF00287166. [DOI] [PubMed] [Google Scholar]
- [13].Jeanpierre M, Turleau C, Aurias A, Prieur M, Ledeist F, Fischer A, Viegas-Pequignot E. An embryonic-like methylation pattern of classical satellite DNA is observed in ICF syndrome. Hum Mol Genet. 1993;2:731–735. doi: 10.1093/hmg/2.6.731. [DOI] [PubMed] [Google Scholar]
- [14].Tuck-Muller CM, Narayan A, Tsien F, Smeets D, Sawyer J, Fiala ES, Sohn O, Ehrlich M. DNA hypomethylation and unusual chromosome instability in cell lines from ICF syndrome patients. Cytogen Cell Genet. 2000;89:121–128. doi: 10.1159/000015590. [DOI] [PubMed] [Google Scholar]
- [15].Okano M, Bell DW, Haber DA, Li E. DNA methyltransferases Dnmt3a and Dnmt3b a reessential for de novo methylation and mammalian development. Cell. 1999;98:247–257. doi: 10.1016/s0092-8674(00)81656-6. [DOI] [PubMed] [Google Scholar]
- [16].Gowher H, Jeltsch A. Molecular enzymology of the catalytic domains of the Dnmt3a and Dnmt3b DNA methyltransferases. J Biol Chem. 2002;277:20409–20414. doi: 10.1074/jbc.M202148200. [DOI] [PubMed] [Google Scholar]
- [17].Ueda Y, Okano M, Williams C, Chen T, Georgopoulos K, Li E. Roles for Dnmt3b in mammalian development: Amouse model for the ICF syndrome. Development. 2006;133:1183–1192. doi: 10.1242/dev.02293. [DOI] [PubMed] [Google Scholar]
- [18].Xie S, Wang Z, Okano M, Nogami M, Li Y, He WW, Okumura K, Li E. Cloning, expression and chromosome locations of the human DNMT3 gene family. Gene. 1999;236:87–95. doi: 10.1016/s0378-1119(99)00252-8. [DOI] [PubMed] [Google Scholar]
- [19].Jeltsch A. Molecular enzymology of mammalian DNA methyltransferases. Curr Top Microbiol Immunol. 2006;301:203–225. doi: 10.1007/3-540-31390-7_7. [DOI] [PubMed] [Google Scholar]
- [20].Kato Y, Kaneda M, Hata K, Kumaki K, Hisano M, Kohara Y, Okano M, Li E, Nozaki M, Sasaki H. Role of the Dnmt3 family in de novo methylation of imprinted and repetitive sequences during male germcell development in the mouse. Hum Mol Genet. 2007;16:2272–2280. doi: 10.1093/hmg/ddm179. [DOI] [PubMed] [Google Scholar]
- [21].Lucifero D, La Salle S, Bourc'his D, Martel J, Bestor TH, Trasler JM. Coordinate regulation of DNA methyltransferase expression during oogenesis. BMC Dev Biol. 2007;7:36. doi: 10.1186/1471-213X-7-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Turek-Plewa J, Jagodzinski PP. The role of mammalian DNA methyltransferases in the regulation of gene expression. Cell Mol Biol Lett. 2005;10:631–647. [PubMed] [Google Scholar]
- [23].Feng J, Chang H, Li E, Fan G. Dynamic expression of de novo DNA methyltransferases Dnmt3a and Dnmt3b in the central nervous system. J Neurosci Res. 2005;79:734–746. doi: 10.1002/jnr.20404. [DOI] [PubMed] [Google Scholar]
- [24].Li JY, Pu MT, Hirasawa R, Li BZ, Huang YN, Zeng R, Jing NH, Chen T, Li E, Sasaki H, et al. Synergistic function of DNA methyltransferases Dnmt3a and Dnmt3b in the methylation of Oct 4 and Nanog. Mol Cell Biol. 2007 doi: 10.1128/MCB.01380-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Suetake I, Miyazaki J, Murakami C, Takeshima H, Tajima S. Distinct enzymatic properties of recombinant mouse DNA methyltransferases Dnmt3a and Dnmt3b. J Biochem (Tokyo) 2003;133:737–744. doi: 10.1093/jb/mvg095. [DOI] [PubMed] [Google Scholar]
- [26].Takeshima H, Suetake I, Shimahara H, Ura K, Tate S, Tajima S. Distinct DNA methylation activity of Dnmt3a and Dnmt3b towards naked and nucleosomal DNA. J Biochem (Tokyo) 2006;139:503–515. doi: 10.1093/jb/mvj044. [DOI] [PubMed] [Google Scholar]
- [27].Weisenberger DJ, Velicescu M, Cheng JC, Gonzales FA, Liang G, Jones PA. Role of the DNA methyltransferase variant DNMT3b3 in DNA methylation. Mol Cancer Res. 2004;2:62–72. [PubMed] [Google Scholar]
- [28].Shirohzu H, Kubota T, Kumazawa A, Sado T, Chijiwa T, Inagaki K, Suetake I, Tajima S, Wakui K, Miki Y, et al. Three novel DNMT3B mutations in Japanese patients with ICF syndrome. Am J Med Genet. 2002;112:31–37. doi: 10.1002/ajmg.10658. [DOI] [PubMed] [Google Scholar]
- [29].Hernandez R, Frady A, Zhang X-Y, Varela M, Ehrlich M. Preferential induction of chromosome 1 multibranched figures and whole-arm deletions in a human pro-B cell line treated with 5-azacytidine or 5-azadeoxycytidine. Cytogenet Cell Genet. 1997;76:196–201. doi: 10.1159/000134548. [DOI] [PubMed] [Google Scholar]
- [30].Ji W, Hernandez R, Zhang X-Y, Qu G, Frady A, Varela M, Ehrlich M. DNA demethylation and pericentromeric rearrangements of chromosome 1. Mutation Res. 1997;379:33–41. doi: 10.1016/s0027-5107(97)00088-2. [DOI] [PubMed] [Google Scholar]
- [31].Bachman KE, Rountree MR, Baylin SB. Dnmt3a and Dnmt3b are transcriptional repressors that exhibit unique localization properties to heterochromatin. J Biol Chem. 2001;276:32282–32287. doi: 10.1074/jbc.M104661200. [DOI] [PubMed] [Google Scholar]
- [32].Kang ES, Park CW, Chung JH. Dnmt3b, de novo DNA methyltransferase, interacts with SUMO-1and Ubc9 through its N-terminal region and is subject to modification by SUMO-1. Biochem Biophys Res Commun. 2001;289:862–868. doi: 10.1006/bbrc.2001.6057. [DOI] [PubMed] [Google Scholar]
- [33].Kim GD, Ni J, Kelesoglu N, Roberts RJ, Pradhan S. Co-operation and communication between the human maintenance and de novo DNA (cytosine-5) methyltransferases. EMBO J. 2002;21:4183–4195. doi: 10.1093/emboj/cdf401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Geiman TM, Sankpal UT, Robertson AK, Zhao Y, Zhao Y, Robertson KD. DNMT3B interacts with hSNF2H chromatin remodeling enzyme, HDACs1 and 2, and components of the histone methylation system. Biochem Biophys Res Commun. 2004;318:544–555. doi: 10.1016/j.bbrc.2004.04.058. [DOI] [PubMed] [Google Scholar]
- [35].Geiman TM, Sankpal UT, Robertson AK, Chen Y, Mazumdar M, Heale JT, Schmiesing JA, Kim W, Yokomori K, Zhao Y, et al. Isolation and characterization of a novel DNA methyltransferase complex linking DNMT3B with components of the mitotic chromosome condensation machinery. Nucleic Acids Res. 2004;32:2716–2729. doi: 10.1093/nar/gkh589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Gill G. SUMO and ubiquitin in the nucleus: Different functions, similar mechanisms? Genes Dev. 2004;18:2046–2059. doi: 10.1101/gad.1214604. [DOI] [PubMed] [Google Scholar]
- [37].Heun P. SUM Organization of the nucleus. Curr Opin Cell Biol. 2007;19:350–355. doi: 10.1016/j.ceb.2007.04.014. [DOI] [PubMed] [Google Scholar]
- [38].Ge YZ, Pu MT, Gowher H, Wu HP, Ding JP, Jeltsch A, Xu GL. Chromatin targeting of de novo DNA methyltransferases by the PWWP domain. J Biol Chem. 2004;279:25447–25454. doi: 10.1074/jbc.M312296200. [DOI] [PubMed] [Google Scholar]
- [39].Luciani JJ, Depetris D, Usson Y, Metzler-Guillemain C, Mignon-Ravix C, Mitchell MJ, Megarbane A, Sarda P, Sirma H, Moncla A. PML nuclear bodies are highly organised DNA–protein structures with a function in heterochromatin remodelling at the G2 phase. J Cell Sci. 2006;119:2518–2531. doi: 10.1242/jcs.02965. [DOI] [PubMed] [Google Scholar]
- [40].Luciani JJ, Depetris D, Missirian C, Mignon-Ravix C, Metzler-Guillemain C, Megarbane A, Moncla A, Mattei MG. Subcellular distribution of HP1 proteins is altered in ICF syndrome. Eur J Hum Genet. 2005;13:41–51. doi: 10.1038/sj.ejhg.5201293. [DOI] [PubMed] [Google Scholar]
- [41].Bai S, Ghoshal K, Datta J, Majumder S, Yoon SO, Jacob ST. DNA methyltransferase 3b regulates nerve growth factor-induced differentiation of PC12 cells by recruiting histone deacetylase 2. Mol Cell Biol. 2005;25:751–766. doi: 10.1128/MCB.25.2.751-766.2005. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [42].Bai S, Ghoshal K, Jacob ST. Identification of T-cadherin as a novel target of DNA methyltransferase 3B and its role in the suppression of nerve growth factor-mediated neurite outgrowth in PC12 cells. J Biol Chem. 2006;281:13604–13611. doi: 10.1074/jbc.M513278200. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [43].Xie ZH, Huang YN, Chen ZX, Riggs AD, Ding JP, Gowher H, Jeltsch A, Sasaki H, Hata K, Xu GL. Mutations in DNA methyltransferase DNMT3B in ICF syndrome affect its regulationby DNMT3L. Hum Mol Genet. 2006;15:1375–1385. doi: 10.1093/hmg/ddl059. [DOI] [PubMed] [Google Scholar]
- [44].Margot JB, Ehrenhofer-Murray AE, Leonhardt H. Inter-actions with in the mammalian DNA methyltransferase family. BMC Mol Biol. 2003;4:7. doi: 10.1186/1471-2199-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Suetake I, Shinozaki F, Miyagawa J, Takeshima H, Tajima S. DNMT3L stimulates the DNA methylation activity of Dnmt3a and Dnmt3b through adirect interaction. J Biol Chem. 2004;279:27816–27823. doi: 10.1074/jbc.M400181200. [DOI] [PubMed] [Google Scholar]
- [46].Kareta MS, Botello ZM, Ennis JJ, Chou C, Chedin F. Reconstitution and mechanism of the stimulation of de novo methylation by human DNMT3L. J Biol Chem. 2006;281:25893–25902. doi: 10.1074/jbc.M603140200. [DOI] [PubMed] [Google Scholar]
- [47].Kloeckener-Gruissem B, Betts DR, Zankl A, Berger W, Gungor T. A new and a reclassified ICF patient without mutations in DNMT3B and its interacting proteins SUMO-1 and UBC9. Am J Med Genet A. 2005;136:31–37. doi: 10.1002/ajmg.a.30767. [DOI] [PubMed] [Google Scholar]
- [48].Miniou P, Jeanpierre M, Bourc'his D, Coutinho Barbosa AC, Blanquet V, Viegas-Pequignot E. Alpha-satellite DNA methylation in normal individuals and in ICF patients: Heterogeneous methylation of constitutive heterochromatin in adult and fetal tissues. Hum Genet. 1997;99:738–745. doi: 10.1007/s004390050441. [DOI] [PubMed] [Google Scholar]
- [49].Howard PJ, Lewis IJ, Harris F, Walker S. Centromeric instability of chromosomes 1 and 16 with variable immune deficiency: A new syndrome. Clin Genet. 1985;27:501–505. doi: 10.1111/j.1399-0004.1985.tb00239.x. [DOI] [PubMed] [Google Scholar]
- [50].Gimelli G, Varone P, Pezzolo A, Lerone M, Pistoia V. ICF syndrome with variable expression in sibs. J Med Gen. 1993;30:429–432. doi: 10.1136/jmg.30.5.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Hansen RS, Stoger R, Wijmenga C, Stanek AM, Canfield TK, Luo P, Matarazzo MR, D'Esposito M, Feil R, Gimelli G, et al. Escape from gene silencing in ICF syndrome: Evidence for advanced replication time as amajor determinant. Hum Mol Genet. 2000;9:2575–2587. doi: 10.1093/hmg/9.18.2575. [DOI] [PubMed] [Google Scholar]
- [52].Schuffenhauer S, Bartsch O, Stumm M, Buchholz T, Petropoulou T, Kraft S, Belohradsky B, Meitinger T, Wegner R. DNA, FISH and complementation studies in ICF syndrome; DNA hypomethylation of repetitive and single copy loci and evidence for atrans acting factor. Hum Genet. 1995;96:562–571. doi: 10.1007/BF00197412. [DOI] [PubMed] [Google Scholar]
- [53].Smeets DFCM, Moog U, Weemaes CMR, Vaes-Peeters G, Merkx GFM, Niehof JP, Hamers G. ICF syndrome: A new case and review of the literature. Hum Genet. 1994;94:240–246. doi: 10.1007/BF00208277. [DOI] [PubMed] [Google Scholar]
- [54].Ausio J, Levin DB, De Amorim GV, Bakker S, Macleod PM. Syndromes of disordered chromatin remodeling. Clin Genet. 2003;64:83–95. doi: 10.1034/j.1399-0004.2003.00124.x. [DOI] [PubMed] [Google Scholar]
- [55].Maraschio P, Zuffardi O, Dalla Fior T, Tiepolo L. Immunodeficiency, centromeric heterochromatin instability of chromosomes 1, 9, and 16, and facial anomalies: The ICF syndrome. J Med Genet. 1988;25:173–180. doi: 10.1136/jmg.25.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Turleau C, Cabanis M-O, Girault D, Ledeist F, Mettey R, Puissant H, Marguerite P, de Grouchy J. Multibranched chromosomes in the ICF syndrome: Immunodeficiency, centromeric instability, and facial anomalies. Am J Med Genet. 1989;32:420–424. doi: 10.1002/ajmg.1320320331. [DOI] [PubMed] [Google Scholar]
- [57].Franceschini P, Martino S, Ciocchini M, Ciuti E, Vardeu MP, Guala A, Signorile F, Camerano P, Franceschini D, Tovo PA. Variability of clinical and immunological phenotypein immunodeficiency–centromericinstability–facial anomalies syndrome. Report of two new patients and review of the literature. Eur J Pediatr. 1995;154:840–846. doi: 10.1007/BF01959794. [DOI] [PubMed] [Google Scholar]
- [58].Fasth A, Forestier E, Holmberg E, Holmgren G, Nordenson I, Soderstrom T, Wahlstrom J. Fragility of the centromeric region of chromosome 1 associated with combined immunodeficiency in siblings: A recessively inherited entity? Acta Paediatr Scand. 1990;79:605–612. doi: 10.1111/j.1651-2227.1990.tb11524.x. [DOI] [PubMed] [Google Scholar]
- [59].Dodge JE, Okano M, Dick F, Tsujimoto N, Chen T, Wang S, Ueda Y, Dyson N, Li E. Inactivation of Dnmt3b in mouse embryonic fibroblasts results in DNA hypomethylation, chromosomal instability, and spontaneous immortalization. J Biol Chem. 2005;280:17986–17991. doi: 10.1074/jbc.M413246200. [DOI] [PubMed] [Google Scholar]
- [60].Miniou P, Jeanpierre M, Blanquet V, Sibella V, Bonneau D, Herbelin C, Fischer A, Niveleau A, Viegas-Pequignot ET. Abnormal methylation pattern in constitutive and facultative (X in active chromosome) heterochromatin of ICF patients. Hum Mol Genet. 1994;3:2093–2102. doi: 10.1093/hmg/3.12.2093. [DOI] [PubMed] [Google Scholar]
- [61].Ehrlich M. DNA methylation in cancer: Too much, but also too little. Oncogene. 2002;21:5400–5413. doi: 10.1038/sj.onc.1205651. [DOI] [PubMed] [Google Scholar]
- [62].Hassan KM, Norwood T, Gimelli G, Gartler SM, Hansen RS. Satellite 2 methylation patterns in normal and ICF syndrome cells and association of hypomethylation with advanced replication. Hum Genet. 2001;109:452–462. doi: 10.1007/s004390100590. [DOI] [PubMed] [Google Scholar]
- [63].Bourc'his D, Miniou P, Jeanpierre M, Molina Gomes D, Dupont J, De Saint-Basile G, Maraschio P, Tiepolo L, Viegas-Pequignot E. Abnormal methylation does not prevent X inactivation in ICF patients. Cytogenet Cell Genet. 1999;84:245–252. doi: 10.1159/000015269. [DOI] [PubMed] [Google Scholar]
- [64].Hansen RS. X inactivation-specific methylation of LINE-1 elements by DNMT3B: Implications for the Lyon repeat hypothesis. Hum Mol Gen. 2003;12:2559–2567. doi: 10.1093/hmg/ddg268. [DOI] [PubMed] [Google Scholar]
- [65].Kondo T, Comenge Y, Bobek MP, Kuick R, Lamb B, Zhu X, Narayan A, Bourc'his D, Viegas-Pequinot E, Ehrlich M, et al. Whole-genome methylation scan in ICF syndrome: Hypomethylation of non-satellite DNA repeats D4Z4 and NBL2. Hum Mol Gen. 2000;9:597–604. doi: 10.1093/hmg/9.4.597. [DOI] [PubMed] [Google Scholar]
- [66].Tsien F, Sun B, Hopkins NE, Vedanarayanan V, Figlewicz D, Winokur S, Ehrlich M. Hypermethylation of the FSHD syndrome-associated D4Z4 repeat in normal somatic tissues and FSHD lymphoblastoid cell lines but not in ICF lymphoblastoid cell lines. Mol Gen Metab. 2000;74:322–331. doi: 10.1006/mgme.2001.3219. [DOI] [PubMed] [Google Scholar]
- [67].Nishiyama R, Qi L, Lacey M, Ehrlich M. Both hypomethylation and hypermethylation in a 0.2-kb region of a DNA repeat in cancer. Mol Cancer Res. 2005;3:617–626. doi: 10.1158/1541-7786.MCR-05-0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Narayan A, Ji W, Zhang X-Y, Marrogi A, Graff JR, Baylin SB, Ehrlich M. Hypomethylation of pericentromeric DNA in breast adenocarcinomas. Int J Cancer. 1998;77:833–838. doi: 10.1002/(sici)1097-0215(19980911)77:6<833::aid-ijc6>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- [69].Qu G, Dubeau L, Narayan A, Yu M, Ehrlich M. Satellite DNA hypomethylation vs. overall genomic hypomethylation in ovarian epithelial tumors of different malignant potential. Mutat Res. 1999;423:91–101. doi: 10.1016/s0027-5107(98)00229-2. [DOI] [PubMed] [Google Scholar]
- [70].Sanford J, Forrester L, Chapman V, Chandley A, Hastie N. Methylation patterns of repetitive DNA sequences in germ cells of Mus musculus. Nucleic Acids Res. 1984;12:2823–2836. doi: 10.1093/nar/12.6.2823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Sanford JP, Clark HJ, Chapman VM, Rossant J. Differences in DNA methylation during oogenesis and spermatogenesis and their persistence during early embryogenesis in the mouse. Genes Dev. 1987;1:1039–1046. doi: 10.1101/gad.1.10.1039. [DOI] [PubMed] [Google Scholar]
- [72].Howlett SK, Reik W. Methylation levels of maternal and paternal genomes during preimplantation development. Development. 1991;113:119–127. doi: 10.1242/dev.113.1.119. [DOI] [PubMed] [Google Scholar]
- [73].Govin J, Escoffier E, Rousseaux S, Kuhn L, Ferro M, Thevenon J, Catena R, Davidson I, Garin J, Khochbin S, et al. Pericentric heterochromatin reprogramming by new histone variants during mouse spermiogenesis. J Cell Biol. 2007;176:283–294. doi: 10.1083/jcb.200604141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Kress C, Thomassin H, Grange T. Active cytosine demethylation triggered by anuclear receptor involves DNA strand breaks. Proc Natl Acad Sci USA. 2006;103:11112–11117. doi: 10.1073/pnas.0601793103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Yamazaki T, Yamagata K, Baba T. Time-lapse and retrospective analysis of DNA methylation in mouse preimplantation embryos by live cell imaging. Dev Biol. 2007;304:409–419. doi: 10.1016/j.ydbio.2006.12.046. [DOI] [PubMed] [Google Scholar]
- [76].Gama-Sosa MA, Slagel VA, Trewyn RW, Oxenhandler R, Kuo KC, Gehrke CW, Ehrlich M. The 5-methylcytosine content of DNA from human tumors. Nucleic Acids Res. 1983;11:6883–6894. doi: 10.1093/nar/11.19.6883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Ehrlich M. Cancer-linked DNA hypomethylation and its relationship to hypermethylation. Curr Top Microbiol Immunol. 2006;310:251–274. doi: 10.1007/3-540-31181-5_12. [DOI] [PubMed] [Google Scholar]
- [78].Sumner AT. Scanning electron microscopy of mammalian chromosomes from prophase to telophase. Chromosoma. 1991;100:410–418. doi: 10.1007/BF00337519. [DOI] [PubMed] [Google Scholar]
- [79].Maraschio P, Cortinovis M, Dainotti E, Tupler R, Tiepolo L. Interphase cytogenetics of the ICF syndrome. Ann Hum Genet. 1992;56:273–278. doi: 10.1111/j.1469-1809.1992.tb01152.x. [DOI] [PubMed] [Google Scholar]
- [80].Gisselsson D, Shao C, Tuck-Muller C, Sogorovic S, Palsson E, Smeets D, Ehrlich M. Pericentromeric chromosomal abnormalities in hypomethylated sequences of ICF syndrome cells at interphase, metaphase, and anaphase. Chromosoma. 2005;114:118–126. doi: 10.1007/s00412-005-0343-7. [DOI] [PubMed] [Google Scholar]
- [81].Haaf T. The effects of 5-azacytidine and 5-azadeoxycytidine on chromosome structure and function: Implications for methylation-associated cellular processes. Pharmacol Ther. 1995;65:19–46. doi: 10.1016/0163-7258(94)00053-6. [DOI] [PubMed] [Google Scholar]
- [82].Almeida A, Kokalj-Vokac N, Lefrancois D, Viegas-Pequignot E, Jeanpierre M, Dutrillaux B, Malfoy B. Hypomethylation of classical satellite DNA and chromosome instability in lymphoblastoid cell lines. Hum Genet. 1993;91:538–546. doi: 10.1007/BF00205077. [DOI] [PubMed] [Google Scholar]
- [83].Vilain A, Bernardino J, Gerbault-Seureau M, Vogt N, Niveleau A, Lefrancois D, Malfoy B, Dutrillaux B. DNA methylation and chromosome instability in lymphoblastoid cell lines. Cytogenet Cell Genet. 2000;90:93–101. doi: 10.1159/000015641. [DOI] [PubMed] [Google Scholar]
- [84].Tsien F, Fiala ES, Youn B, Long TI, Laird PW, Weissbecker K, Ehrlich M. Prolonged culture of normal chorionic villus cells yields ICF syndrome-like chromatin decondensation and rearrangements. Cytogenet Genome Res. 2002;98:13–21. doi: 10.1159/000068543. [DOI] [PubMed] [Google Scholar]
- [85].Brown DC, Grace E, Summer AT, Edmunds AT, Ellis PM. ICF syndrome (immunodeficiency, centromeric instability and facial anomalies): Investigation of heterochromatin abnormalities and review of clinical outcome. Hum Genet. 1995;96:411–416. doi: 10.1007/BF00191798. [DOI] [PubMed] [Google Scholar]
- [86].Sawyer JR, Swanson CM, Wheeler G, Cunniff C. Chromosome instability in ICF syndrome: Formation of micronuclei from multibranched chromosome 1 demonstrated by fluorescence in situ hybridization. Am J Med Genet. 1995;56:203–209. doi: 10.1002/ajmg.1320560218. [DOI] [PubMed] [Google Scholar]
- [87].Ehrlich M. DNA methylation and cancer-associated genetic instability. In: Nigg EA, editor. Genomic instability in cancer development., Advances in Experimental Medicine and Biology. Vol. 570. Amsterdam: Kluwer Academic Publishers; 2005. pp. 363–392. [DOI] [PubMed] [Google Scholar]
- [88].Sawyer J, Tricot G, Mattox S, Jagannath S, Barlogie B. Jumping translocations of chromosome 1q in multiple myeloma: Evidence for a mechanism involving decondensation of pericentromeric heterochromatin. Blood. 1998;91:1732–1741. [PubMed] [Google Scholar]
- [89].Wong N, Lam WC, Lai PB, Pang E, Lau WY, Johnson PJ. Hypomethylation of chromosome 1 heterochromatin DNA correlates with q-armcopy gain in human hepatocellular carcinoma. Am J Pathol. 2001;159:465–471. doi: 10.1016/S0002-9440(10)61718-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Nakagawa T, Kanai Y, Ushijima S, Kitamura T, Kakizoe T, Hirohashi S. DNA hypomethylation on pericentromeric satellite regions significantly correlates with loss of heterozygosity on chromosome 9 in urothelial carcinomas. J Urol. 2005;173:243–246. doi: 10.1097/01.ju.0000141577.98902.49. [DOI] [PubMed] [Google Scholar]
- [91].Cadieux B, Ching TT, Vandenberg SR, Costello JF. Genome-wide hypomethylation in human glioblastomas associated with specific copy number alteration, methylenetetrahydrofolate reductase allele status, and increased proliferation. Cancer Res. 2006;66:8469–8476. doi: 10.1158/0008-5472.CAN-06-1547. [DOI] [PubMed] [Google Scholar]
- [92].Mitelman F, Mertens F, Johansson B. A breakpoint map of recurrent chromosomal rearrangements in human neoplasia. Nat Genet. 1997;15:417–474. doi: 10.1038/ng0497supp-417. [DOI] [PubMed] [Google Scholar]
- [93].Eden A, Gaudet F, Waghmare A, Jaenisch R. Chromosomal instability and tumors promoted by DNA hypomethylation. Science. 2003;300:455. doi: 10.1126/science.1083557. [DOI] [PubMed] [Google Scholar]
- [94].Yamada Y, Jackson-Grusby L, Linhart H, Meissner A, Eden A, Lin H, Jaenisch R. Opposing effects of DNA hypomethylation on intestinal and liver carcinogenesis. Proc Natl Acad Sci USA. 2005;102:13580–13585. doi: 10.1073/pnas.0506612102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Schuetz C, Barbi G, Barth TF, Hoenig M, Schulz A, Moeller P, Smeets D, de Greef JC, van der Maarel SM, Vogel W, et al. ICF syndrome: High variability of the chromosomal phenotype and association with classical Hodgkin lymphoma. Am J Med Genet A. 2007;143:2052–2057. doi: 10.1002/ajmg.a.31885. [DOI] [PubMed] [Google Scholar]
- [96].Narayan A, Tuck-Muller C, Weissbecker K, Smeets D, Ehrlich M. Hypersensitivity to radiation-induced nonapoptotic and apoptotic death in cell lines from patients with the ICF chromosome instability syndrome. Mutat Res. 2000;456:1–15. doi: 10.1016/s0027-5107(00)00103-2. [DOI] [PubMed] [Google Scholar]
- [97].Seidemann K, Henze G, Beck JD, Sauerbrey A, Kuhl J, Mann G, Reiter A. Non-Hodgkin's lymphoma in pediatric patients with chromosomal breakage syndromes (AT and NBS): Experience from the BFM trials. Ann Oncol. 2000;11(Suppl 1):141–145. [PubMed] [Google Scholar]
- [98].Blanco-Betancourt CE, Moncla A, Milili M, Jiang Y, Viegas-Pequignot E, Roquelaure B, Thuret I, Schiff C. Defective B-cell-negative selection and terminal differentiation in the ICF syndrome. Blood. 2004:2683–2690. doi: 10.1182/blood-2003-08-2632. [DOI] [PubMed] [Google Scholar]
- [99].Mack KD, Von Goetz M, Lin M, Venegas M, Barnhart J, Lu Y, Lamar B, Stull R, Silvin C, Owings P, et al. Functional identification of kinases essential for T-cell activation through a genetic suppression screen. Immunol Lett. 2005;96:129–145. doi: 10.1016/j.imlet.2004.08.004. [DOI] [PubMed] [Google Scholar]
- [100].Yao Z, Zhou G, Wang XS, Brown A, Diener K, Gan H, Tan TH. Anovel human STE20-related protein kinase, HGK, that specifically activates the c-Jun N-terminal kinase signaling pathway. J Biol Chem. 1999;274:2118–2125. doi: 10.1074/jbc.274.4.2118. [DOI] [PubMed] [Google Scholar]
- [101].Miled C, Pontoglio M, Garbay S, Yaniv M, Weitzman JB. A genomic map of p53 binding sites identifies novel p53 targets involved in an apoptotic network. Cancer Res. 2005;65:5096–5104. doi: 10.1158/0008-5472.CAN-04-4232. [DOI] [PubMed] [Google Scholar]
- [102].Tesz GJ, Guilherme A, Guntur KV, Hubbard AC, Tang X, Chawla A, Czech MP. Tumor necrosis factor alpha (TNFalpha) stimulates Map4k4 expression through TNFalpha receptor 1signaling to c-Jun and activating transcription factor 2. J Biol Chem. 2007;282:19302–19312. doi: 10.1074/jbc.M700665200. [DOI] [PubMed] [Google Scholar]
- [103].Collins CS, Hong J, Sapinoso L, Zhou Y, Liu Z, Micklash K, Schultz PG, Hampton GM. A small interfering RNA screen for modulators of tumor cell motility identifies MAP4K4 as a promigratory kinase. Proc Natl Acad Sci USA. 2006;103:3775–3780. doi: 10.1073/pnas.0600040103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Yamashita Y, Hooker SW, Jiang H, Laurent AB, Resta R, Khare K, Coe A, Kincade PW, Thompson LF. CD73 expression and fyn-dependent signaling on murine lymphocytes. Eur J Immunol. 1998;28:2981–2990. doi: 10.1002/(SICI)1521-4141(199810)28:10<2981::AID-IMMU2981>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- [105].Borst J, Hendriks J, Xiao Y. CD27 and CD70 in T cell and B cell activation. Curr Opin Immunol. 2005;17:275–281. doi: 10.1016/j.coi.2005.04.004. [DOI] [PubMed] [Google Scholar]
- [106].Jacquot S, Kobata T, Iwata S, Morimoto C, Schlossman SF. CD154/CD40 and CD70/CD27 interactions have different and sequential functions in T cell-dependent B cell responses: Enhancement of plasma cell differentiation by CD27 signaling. J Immunol. 1997;159:2652–2657. [PubMed] [Google Scholar]
- [107].Eris JM, Basten A, Brink R, Doherty K, Kehry MR, Hodgkin PD. Anergic self-reactive B cells present self antigen and respond normally to CD40-dependent T-cell signals but are defective in antigen-receptor-mediated functions. Proc Natl Acad Sci USA. 1994;91:4392–4396. doi: 10.1073/pnas.91.10.4392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Barry F, Boynton R, Murphy M, Haynesworth S, Zaia J. The SH-3 and SH-4 antibodies recognized istinct epitopes on CD73 from human mesenchymal stem cells. Biochem Biophys Res Commun. 2001;289:519–524. doi: 10.1006/bbrc.2001.6013. [DOI] [PubMed] [Google Scholar]
- [109].Hathcock KS, Hirano H, Murakami S, Hodes RJ. CD44 expression on activated B cells. Differential capacity for CD44-dependent binding to hyaluronic acid. J Immunol. 1993;151:6712–6722. [PubMed] [Google Scholar]
- [110].Bohnhorst JO, Bjorgan MB, Thoen JE, Natvig JB, Thompson KM. Bm1–Bm5 classification of peripheral blood B cells reveals circulating germinal center founder cells in healthy individuals and disturbance in the B cell subpopulations in patients with primary Sjogren's syndrome. J Immunol. 2001;167:3610–3618. doi: 10.4049/jimmunol.167.7.3610. [DOI] [PubMed] [Google Scholar]
- [111].Li T, Zhong J, Chen Y, Qiu X, Zhang T, Ma D, Han W. Expression of chemokine-like factor 1 is upregulated during T lymphocyte activation. Life Sci. 2006;79:519–524. doi: 10.1016/j.lfs.2006.01.042. [DOI] [PubMed] [Google Scholar]
- [112].Peters T, Bloch W, Wickenhauser C, Tawadros S, Oreshkova T, Kess D, Krieg T, Muller W, Scharffetter-Kochanek K. Terminal B cell differentiation is skewed by deregulated interleukin-6 secretion in beta 2 integr indeficient mice. J Leukoc Biol. 2006;80:599–607. doi: 10.1189/jlb.1205740. [DOI] [PubMed] [Google Scholar]
- [113].Lamkanfi M, Kanneganti TD, Franchi L, Nunez G. Caspase-1 inflammasomes in infection and inflammation. J Leukoc Biol. 2007;82:220–225. doi: 10.1189/jlb.1206756. [DOI] [PubMed] [Google Scholar]
- [114].Husain Z, Holodick N, Day C, Szymanski I, Alper CA. Increased apoptosis of CD20 + IgA + B cells is the basis for IgA deficiency: The molecular mechanismfor correction in vitro by IL-10 and CD40L. J Clin Immunol. 2006;26:113–125. doi: 10.1007/s10875-006-9001-y. [DOI] [PubMed] [Google Scholar]
- [115].Stacey M, Bennett MS, Hulten M. FISH analysis on spontaneously arising micronuclei in the ICF syndrome. J Med Genet. 1995;32:502–508. doi: 10.1136/jmg.32.7.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Pezzolo A, Prigione I, Facchetti P, Castellano E, Viale M, Gimelli G, Pistoia V. T-cell apoptosis in ICF syndrome. J Allergy Clin Immunol. 2001;108:310–312. doi: 10.1067/mai.2001.116863. [DOI] [PubMed] [Google Scholar]
- [117].Ke N, Godzik A, Reed JC. Bcl-B, a novel Bcl-2 family member that differentially binds and regulates Bax and Bak. J Biol Chem. 2001;276:12481–12484. doi: 10.1074/jbc.C000871200. [DOI] [PubMed] [Google Scholar]
- [118].Naumann U, Weit S, Wischhusen J, Weller M. Diva/Boo is a negative regulator of cell death in human glioma cells. FEBS Lett. 2001;505:23–26. doi: 10.1016/s0014-5793(01)02768-5. [DOI] [PubMed] [Google Scholar]
- [119].Ivanov VN, Ronai Z, Hei TK. Opposite roles of FAP-1 and dynamin in the regulation of Fas(CD95) translocation to the cell surface and susceptibility to Fas ligand-mediated apoptosis. J Biol Chem. 2006;281:1840–1852. doi: 10.1074/jbc.M509866200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Irie S, Hachiya T, Rabizadeh S, Maruyama W, Mukai J, Li Y, Reed JC, Bredesen DE, Sato TA. Functional interaction of Fas-associated phosphatase-1 (FAP-1) with p75(NTR) and their effect on NF-kappa B activation. FEBS Lett. 1999;460:191–198. doi: 10.1016/s0014-5793(99)01324-1. [DOI] [PubMed] [Google Scholar]
- [121].Dromard M, Bompard G, Glondu-Lassis M, Puech C, Chalbos D, Freiss G. The putative tumor suppressor gene PTPN13/PTPL1 induces apoptosis through insulin receptor substrate-1 dephosphorylation. Cancer Res. 2007;67:6806–6813. doi: 10.1158/0008-5472.CAN-07-0513. [DOI] [PubMed] [Google Scholar]
- [122].Ehrlich M, Gama-Sosa M, Huang L-H, Midgett RM, Kuo KC, McCune RA, Gehrke C. Amount and distribution of 5-methylcytosine in human DNA from different types of tissues or cells. Nucleic Acids Res. 1982;10:2709–2721. doi: 10.1093/nar/10.8.2709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Saras J, Claesson-Welsh L, Heldin CH, Gonez LJ. Cloning and characterization of PTPL1, a protein tyrosine phosphatase with similarities to cytoskeletal-associated proteins. J Biol Chem. 1994;269:24082–24089. [PubMed] [Google Scholar]
- [124].Zhou YW, Komada Y, Inaba H, Azuma E, Sakurai M. Down-regulation of Fas-associated phosphatase-1(FAP-1) in interleukin-2-activated T cells. Cell Immunol. 1998;186:103–110. doi: 10.1006/cimm.1998.1297. [DOI] [PubMed] [Google Scholar]
- [125].Lamkanfi M, Kalai M, Saelens X, Declercq W, Vandenabeele P. Caspase-1 activates nuclear factor of the kappa-enhancer in B cells independently of its enzymatic activity. J Biol Chem. 2004;279:24785–24793. doi: 10.1074/jbc.M400985200. [DOI] [PubMed] [Google Scholar]
- [126].Nakai Y, Irie S, Sato TA. Identification of IkappaBalpha as a substrate of Fas-associated phosphatase-1. Eur J Biochem. 2000;267:7170–7175. doi: 10.1046/j.1432-1327.2000.01818.x. [DOI] [PubMed] [Google Scholar]
- [127].Rawlings DJ, Sommer K, Moreno-Garcia ME. The CARMA1 signalosome links the signalling machinery of adaptive and innate immunity in lymphocytes. Nat Rev Immunol. 2006;6:799–812. doi: 10.1038/nri1944. [DOI] [PubMed] [Google Scholar]
- [128].Lucas PC, McAllister-Lucas LM, Nunez G. NF-kappaB signaling in lymphocytes: A new cast of characters. J Cell Sci. 2004;117:31–39. doi: 10.1242/jcs.00904. [DOI] [PubMed] [Google Scholar]
- [129].Kim HP, Ryter SW, Choi AM. CO as acellular signaling molecule. Annu Rev Pharmacol Toxicol. 2006;46:411–449. doi: 10.1146/annurev.pharmtox.46.120604.141053. [DOI] [PubMed] [Google Scholar]
- [130].Brouard S, Berberat PO, Tobiasch E, Seldon MP, Bach FH, Soares MP. Heme oxygenase-1-derived carbon monoxide requires the activation of transcription factor NF-kappa B to protect endothelial cells from tumor necrosis factor-alpha-mediated apoptosis. J Biol Chem. 2002;277:17950–17961. doi: 10.1074/jbc.M108317200. [DOI] [PubMed] [Google Scholar]
- [131].Soares MP, Usheva A, Brouard S, Berberat PO, Gunther L, Tobiasch E, Bach FH. Modulation of endothelial cell apoptosis by heme oxygenase-1-derived carbon monoxide. Antioxid Redox Signal. 2002;4:321–329. doi: 10.1089/152308602753666370. [DOI] [PubMed] [Google Scholar]
- [132].Uht RM, Amos S, Martin PM, Riggan AE, Hussaini IM. The protein kinase C-eta isoform induces proliferation in glioblastoma cell lines through an ERK/Elk-1 pathway. Oncogene. 2007;26:2885–2893. doi: 10.1038/sj.onc.1210090. [DOI] [PubMed] [Google Scholar]
- [133].Chen CC, Wang JK, Chen WC, Lin SB. Protein kinase C eta mediates lipopolysaccharide-induced nitric-oxide synthase expression in primary astrocytes. J Biol Chem. 1998;273:19424–19430. doi: 10.1074/jbc.273.31.19424. [DOI] [PubMed] [Google Scholar]
- [134].Pham TN, Brown BL, Dobson PR, Richardson VJ. Protein kinase C-eta (PKC-eta) is required for the development of inducible nitric oxide synthase (iNOS) positive phenotype in human monocytic cells. Nitric Oxide. 2003;9:123–134. doi: 10.1016/j.niox.2003.09.006. [DOI] [PubMed] [Google Scholar]
- [135].Kubo M, Hata J, Ninomiya T, Matsuda K, Yonemoto K, Nakano T, Matsushita T, Yamazaki K, Ohnishi Y, Saito S, et al. A nonsynonymous SNP in PRKCH (protein kinase C eta) increases the risk of cerebral infarction. Nat Genet. 2007;39:212–217. doi: 10.1038/ng1945. [DOI] [PubMed] [Google Scholar]
- [136].Quan T, Fisher GJ. Cloning and characterization of the human protein kinase C-eta promoter. J Biol Chem. 1999;274:28566–28574. doi: 10.1074/jbc.274.40.28566. [DOI] [PubMed] [Google Scholar]
- [137].Takata Y, Hamada D, Miyatake K, Nakano S, Shinomiya F, Scafe CR, Reeve VM, Osabe D, Moritani M, Kunika K, et al. Genetic association between the PRKCH gene encoding protein kinase Ceta isozyme and rheumatoid arthritis in the Japanese population. Arthritis Rheum. 2007;56:30–42. doi: 10.1002/art.22262. [DOI] [PubMed] [Google Scholar]
- [138].Morrow TA, Muljo SA, Zhang J, Hardwick JM, Schlissel MS. Pro-B-cell-specific transcription and proapoptotic function of protein kinase Ceta. Mol Cell Biol. 1999;19:5608–5618. doi: 10.1128/mcb.19.8.5608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [139].Niedbala W, Cai B, Liew FY. Role of nitric oxide in the regulation of T cell functions. Ann Rheum Dis. 2006;65(Suppl 3):iii37–iii40. doi: 10.1136/ard.2006.058446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [140].Zabel U, Weeger M, La M, Schmidt HH. Human soluble guanylate cyclase: Functional expression and revised iso-enzyme family. Biochem J. 1998;335:51–57. doi: 10.1042/bj3350051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Hartsfield CL. Cross talk between carbon monoxide and nitric oxide. Antioxid Redox Signal. 2002;4:301–307. doi: 10.1089/152308602753666352. [DOI] [PubMed] [Google Scholar]
- [142].Montoliu C, Piedrafita B, Serra MA, Del Olmo JA, Ferrandez A, Rodrigo JM, Felipo V. Activation of soluble guanylate cyclase by nitric oxide in lymphocytes correlates with minimal hepatic encephalopathy in cirrhotic patients. J Mol Med. 2007;85:233–241. doi: 10.1007/s00109-006-0149-y. [DOI] [PubMed] [Google Scholar]
- [143].Maekawa K, Imagawa N, Nagamatsu M, Harada S. Molecular cloning of a novel protein-tyrosine phosphatase containing a membrane-binding domain and GLGF repeats. FEBS Lett. 1994;337:200–206. doi: 10.1016/0014-5793(94)80273-4. [DOI] [PubMed] [Google Scholar]
- [144].Aoyama K, Suh SW, Hamby AM, Liu J, Chan WY, Chen Y, Swanson RA. Neuronal glutathione deficiency and age-dependent neurodegeneration in the EAAC1 deficient mouse. Nat Neurosci. 2006;9:119–126. doi: 10.1038/nn1609. [DOI] [PubMed] [Google Scholar]
- [145].Itoh T, Itoh A, Pleasure D. Bcl-2-related protein family gene expression during oligodendroglial differentiation. J Neurochem. 2003;85:1500–1512. doi: 10.1046/j.1471-4159.2003.01795.x. [DOI] [PubMed] [Google Scholar]
- [146].Burette A, Zabel U, Weinberg RJ, Schmidt HH, Valtschanoff JG. Synaptic localization of nitric oxide synthase and soluble guanylyl cyclase in the hippocampus. J Neurosci. 2002;22:8961–8970. doi: 10.1523/JNEUROSCI.22-20-08961.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Gemma C, Bickford PC. Interleukin-1beta and caspase-1: Players in the regulation of age-related cognitive dysfunction. Rev Neurosci. 2007;18:137–148. doi: 10.1515/revneuro.2007.18.2.137. [DOI] [PubMed] [Google Scholar]
- [148].Masso-Welch PA, Winston JS, Edge S, Darcy KM, Asch H, Vaughan MM, Ip MM. Altered expression and localization of PKC eta in human breast tumors. Breast Cancer Res Treat. 2001;68:211–223. doi: 10.1023/a:1012265703669. [DOI] [PubMed] [Google Scholar]
- [149].Lusser A, Kadonaga JT. Chromatin remodeling by ATP-dependent molecular machines. Bioessays. 2003;25:1192–1200. doi: 10.1002/bies.10359. [DOI] [PubMed] [Google Scholar]
- [150].Xiong Z, Laird PW. COBRA: A sensitive and quantitative DNA methylation assay. Nucleic Acids Res. 1997;25:2532–2534. doi: 10.1093/nar/25.12.2532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [151].Ehrlich M. Expression of various genes is controlled by DNA methylation during mammalian development. J Cell Biochem. 2003;88:899–910. doi: 10.1002/jcb.10464. [DOI] [PubMed] [Google Scholar]
- [152].Zhao Y, Srivastava D. A developmental view of microRNA function. Trends Biochem Sci. 2007;32:189–197. doi: 10.1016/j.tibs.2007.02.006. [DOI] [PubMed] [Google Scholar]
- [153].Horn PJ, Peterson CL. Heterochromatin assembly: A new twist on an old model. Chromosome Res. 2006;14:83–94. doi: 10.1007/s10577-005-1018-1. [DOI] [PubMed] [Google Scholar]
- [154].Mathieu O, Bender J. RNA-directed DNA methylation. J Cell Sci. 2004;117:4881–4888. doi: 10.1242/jcs.01479. [DOI] [PubMed] [Google Scholar]
- [155].Partridge JF, DeBeauchamp JL, Kosinski AM, Ulrich DL, Hadler MJ, Noffsinger VJ. Functional separation of the requirements for establishment and maintenance of centromeric heterochromatin. Mol Cell. 2007;26:593–602. doi: 10.1016/j.molcel.2007.05.004. [DOI] [PubMed] [Google Scholar]
- [156].Alexiadis V, Ballestas ME, Sanchez C, Winokur S, Vedanarayanan V, Warren M, Ehrlich M. RNAPol-ChIP analysis of transcription from FSHD-linked tandem repeats and satellite DNA. Biochim Biophys Acta. 2007;1769:29–40. doi: 10.1016/j.bbaexp.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [157].Jolly C, Metz A, Govin J, Vigneron M, Turner BM, Khochbin S, Vourc'h C. Stress-induced transcription of satellite III repeats. J Cell Biol. 2004;164:25–33. doi: 10.1083/jcb.200306104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Gasser SM. Positions of potential: Nuclear organization and gene expression. Cell. 2001;104:639–642. doi: 10.1016/s0092-8674(01)00259-8. [DOI] [PubMed] [Google Scholar]
- [159].Goldmit M, Ji Y, Skok J, Roldan E, Jung S, Cedar H, Bergman Y. Epigenetic ontogeny of the Igk locus during B cell development. Nat Immunol. 2005;6:198–203. doi: 10.1038/ni1154. [DOI] [PubMed] [Google Scholar]
- [160].Alcobia I, Quina AS, Neves H, Clode N, Parreira L. The spatial organization of centromeric heterochromatin during normal human lymphopoiesis: Evidence for ontogenically determined spatial patterns. Exp Cell Res. 2003;290:358–369. doi: 10.1016/s0014-4827(03)00335-5. [DOI] [PubMed] [Google Scholar]
- [161].Bartlett J, Blagojevic J, Carter D, Eskiw C, Fromaget M, Job C, Shamsher M, Trindade IF, Xu M, Cook PR. Specialized transcription factories. Biochem Soc Symp. 2006:67–75. doi: 10.1042/bss0730067. [DOI] [PubMed] [Google Scholar]
- [162].Shestakova EA, Mansuroglu Z, Mokrani H, Ghinea N, Bonnefoy E. Transcription factor YY1 associates with pericentromeric gamma-satellite DNA in cycling but not in quiescent(G0)cells. Nucleic Acids Res. 2004;32:4390–4399. doi: 10.1093/nar/gkh737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [163].Jolly C, Konecny L, Grady DL, Kutskova YA, Cotto JJ, Morimoto RI, Vourc'h C. In vivo binding of active heat shock transcription factor 1 to human chromosome 9 heterochromatin during stress. J Cell Biol. 2002;156:775–781. doi: 10.1083/jcb.200109018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [164].Day RN, Voss TC, Enwright JF, 3rd, Booker CF, Periasamy A, Schaufele F. Imaging the localized protein interactions between Pit-1 and the CCAAT/enhancer binding protein alpha in the living pituitary cell nucleus. Mol Endocrinol. 2003;17:333–345. doi: 10.1210/me.2002-0136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [165].Enwright JF, 3rd, Kawecki-Crook MA, Voss TC, Schaufele F, Day RN. A PIT-1 homeodomain mutant blocks the intranuclear recruitment of the CCAAT/enhancer binding protein alpha required for prolactin gene transcription. Mol Endocrinol. 2003;17:209–222. doi: 10.1210/me.2001-0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [166].Piwien Pilipuk G, Galigniana MD, Schwartz J. Subnuclear localization of C/EBP beta is regulated by growth hormone and dependenton MAPK. J Biol Chem. 2003;278:35668–35677. doi: 10.1074/jbc.M305182200. [DOI] [PubMed] [Google Scholar]
- [167].Wen J, Huang S, Pack SD, Yu X, Brandt SJ, Noguchi CT. Tal1/SCL binding to pericentromeric DNA represses transcription. J Biol Chem. 2005;280:12956–12966. doi: 10.1074/jbc.M412721200. [DOI] [PubMed] [Google Scholar]
- [168].Yamashita K, Sato A, Asashima M, Wang PC, Nishinakamura R. Mouse homolog of SALL1, a causative gene for Townes–Brocks syndrome, binds to A/T-rich sequences in pericentric heterochromatin via its C-terminal zinc finger domains. Genes Cells. 2007;12:171–182. doi: 10.1111/j.1365-2443.2007.01042.x. [DOI] [PubMed] [Google Scholar]
- [169].Sabbattini P, Lundgren M, Georgiou A, Chow C, Warnes G, Dillon N. Binding of Ikaros to the lambda5 promoter silences transcription through a mechanism that does not require heterochromatin formation. EMBO J. 2001;20:2812–2822. doi: 10.1093/emboj/20.11.2812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [170].Ugarkovic D. Functional elements residing within satellite DNAs. EMBO Rep. 2005;6:1035–1039. doi: 10.1038/sj.embor.7400558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [171].Netzer C, Rieger L, Brero A, Zhang CD, Hinzke M, Kohlhase J, Bohlander SK. SALL1, the gene mutated in Townes–Brocks syndrome, encodes a transcriptional repressor which interacts with TRF1/PIN2 and localizes to pericentromeric heterochromatin. Hum Mol Genet. 2001;10:3017–3024. doi: 10.1093/hmg/10.26.3017. [DOI] [PubMed] [Google Scholar]
- [172].Liu X, Wu B, Szary J, Kofoed EM, Schaufele F. Functional sequestration of transcription factor activity by repetitive DNA. J Biol Chem. 2007;282:20868–20876. doi: 10.1074/jbc.M702547200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [173].Ehrlich M, Ehrlich KC. Effect of DNA methylation on the binding of vertebrate and plant proteins to DNA. In: Jost JP, Saluz HP, editors. DNA methylation: Biological significance. Boston: Birkhauser Verlag; 1993. pp. 145–168. [DOI] [PubMed] [Google Scholar]
- [174].Nan X, Tate P, Li E, Bird A. DNA methylation specifies chromosomal localization of MeCP2. Mol Cell Biol. 1996;16:414–421. doi: 10.1128/mcb.16.1.414. [DOI] [PMC free article] [PubMed] [Google Scholar]