Abstract
Objectives. Rheumatological conditions are common, thus nurses (Ns) occupational therapists (OTs) and physiotherapists (PTs) require at least basic rheumatology knowledge upon qualifying. The aim of this study was to develop a core set of teaching topics and potential ways of delivering them.
Methods. A modified Delphi technique was used for clinicians to develop preliminary core sets of teaching topics for each profession. Telephone interviews with educationalists explored their views on these, and challenges and solutions for delivering them. Inter-professional workshops enabled clinicians and educationalists to finalize the core set together, and generate methods for delivery.
Results. Thirty-nine rheumatology clinicians (12N, 14OT, 13PT) completed the Delphi consensus, proposing three preliminary core sets (N71 items, OT29, PT26). Nineteen educationalists (6N, 7OT, 6PT) participated in telephone interviews, raising concerns about disease-specific vs generic teaching and proposing many methods for delivery. Three inter-professional workshops involved 34 participants (clinicians: N12, OT9, PT5; educationalists: N2, OT3, PT2; Patient 1) who reached consensus on a single core set comprising six teaching units: Anatomy and Physiology; Assessment; Management and Intervention; Psychosocial Issues; Patient Education; and the Multi-disciplinary Team, recommending some topics within the units receive greater depth for some professions. An innovative range of delivery options was generated plus two brief interventions: a Rheumatology Chat Show and a Rheumatology Road Show.
Conclusions. Working together, clinicians and educationalists proposed a realistic core set of rheumatology topics for undergraduate health professionals. They proposed innovative delivery methods, with collaboration between educationalists, clinicians and patients strongly recommended. These potential interventions need testing.
Keywords: Rheumatology, Undergraduate, Nursing, Physiotherapy, Occupational therapy, Health professionals, Curriculum
Introduction
In an average year, ∼9 million people attend GP surgeries for arthritis-related conditions, which are also found in about two-fifths of hospital inpatients [1, 2]. Most nurses (Ns), physiotherapists (PTs) and occupational therapists (OTs) therefore need the skills and knowledge to manage rheumatological conditions or understand their impact (e.g. the consequences for a patient with RA who is temporarily immobilized through a myocardial infarction). Rheumatology should therefore be a core component of undergraduate health professional (HP) education.
Nurses, OTs and PTs in the UK are trained over 3 yrs. There are guidelines from the governing bodies but no agreed national core curricula [3–5] and validation is provided by individual Universities. Two major problems in providing a rheumatological component to HP undergraduate education are limited curriculum time available for theoretical input and decreasing opportunities for clinical placements as hospitals concentrate on acute illness [6], with fewer rheumatology inpatient beds. Paradoxically, these challenges come at a time when the role of the rheumatology HP is expanding, with almost every rheumatology department employing specialist rheumatology nurses, OTs and PTs [7].
In a recent survey of undergraduate nursing, OT and physiotherapy courses in the UK, educationalists reported only limited coverage of rheumatology theory for disease mechanisms, disability, psycho-social issues and multi-disciplinary team working [8]. They found it difficult to identify rheumatology-specific content, as many curricula concentrate on generic skills [8]. Concerns about disease-related vs generic education for undergraduate HPs have been raised and Government recommendations are that although nurse education should be principle-based, it should be built around patient pathways [9–13]. It is thus possible that rheumatology-specific teaching is being delivered on clinical placements, but again the data showed little rheumatology exposure during clinical placements for nurses and OTs, and many educationalists felt that the rheumatology content of their course was inadequate (50% of nursing courses, OT 30%, PT 42%) [8]. Similar problems occur in medicine where undergraduate rheumatology exposure is only offered to some students, and the time spent teaching rheumatology continues to decrease [14, 15].
Limited rheumatology exposure for undergraduate HPs may mean that rheumatology patients on general wards, in the community or being treated for other problems but with underlying rheumatological conditions, may receive less than optimal care. In addition, fewer HPs may consider rheumatology as a career option if they have not been exposed to it during training. The removal of theatre placements from the undergraduate nursing curriculum reduced recruitment rates for theatre nurses, while increased clinical exposure in psychiatry improved recruitment [9, 10].
Many specialties face challenges in agreeing core theoretical teaching for undergraduate HPs but several have been able to identify these, along with delivery methods [11, 12]. The aims of this study were for rheumatology clinicians to propose a draft core set of rheumatology topics for undergraduates; for educationalists to explore potential ways of delivering it; and for clinicians and educationalists together to finalize the rheumatology core topics and proposals for their delivery.
Subjects and Methods
Phase I (clinicians’ preliminary core set)
The Delphi technique uses ‘expert’ opinions to establish consensus through a series of questionnaire rounds, with the results of each round informing the contents of the next [16]. Data from the literature are commonly used to construct the initial questionnaire [16]; therefore, Round 1 was based on a previous consensus on the standards for qualified HPs in rheumatology [17]. Several topics clearly applied only to qualified HPs (e.g. joint injections) and were therefore removed, leaving 17 broad topics such as pathology, assessment, treatment, education and psychology.
Round 1
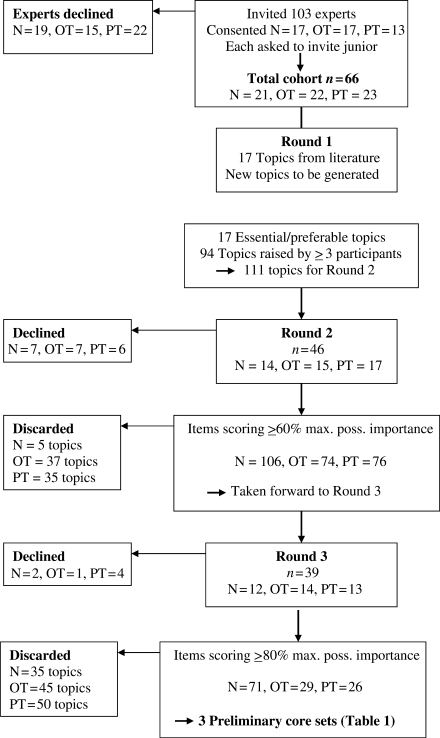
Expert clinicians from the previous consensus [17] or professional society handbooks were approached (Fig. 1). Consenting clinicians were also asked to pass a study invitation to a local HP with ≤1 year's rheumatology experience, as they might bring a more recent perspective on preparation for entering rheumatology. A postal Delphi was used, with no reminders. Participants rated each topic as not required, optional, preferable or essential (0–3) for undergraduate HPs. The Delphi technique was modified [18] by also asking participants to generate specific issues for each topic (e.g. psychology might generate issues such as depression). Topics rated as essential/preferable and any new issues generated by ≥3 participants were taken forward to Round 2 (Fig. 1).
Fig. 1.
Flow chart of Phase I (Delphi study).
Round 2
Participants rated Round 2 items using the same 0–3 scale. Data were converted to a percentage of the maximum possible importance score for each topic, e.g. if all nurses scored a topic as essential (3), this would score 100%. There is no universally agreed cut-off point for consensus and Delphi studies have adopted levels of 51–100% [16, 18]. There was no clear level at which consensus markedly dropped; therefore, an inclusive approach was taken and items scoring ≥60% for each profession were taken into Round 3.
Round 3
Using the same scoring system and a more stringent consensus of ≥80%, a preliminary core set of rheumatology topics was created for undergraduates in each profession.
In Round 3, recent entrants to rheumatology were also asked what motivated them to take up rheumatology (Did anything or anyone inspire you? Which aspects of training did you find inspiring, helpful or interesting? What would have enthused you about rheumatology as a student?). Free text was examined using thematic analysis [19] by two researchers working independently and then agreeing emerging themes together (A.O.B., S.H.).
Phase II (educationalists’ challenges)
For each profession, 6–7 curriculum organizers/clinical placement officers from the UK survey [8] were invited to participate in a 30–40-min telephone discussion. Participants were selected to reflect a range of Universities and Trusts across the UK. The interviews followed a structured format, asking how rheumatology was currently taught, views on the preliminary core sets from Phase I and how they might be delivered. Responses were documented on a record sheet and the typed summary returned to participants for validation. The data were examined by two researchers (C.A., S.H.) using a thematic approach [19] to produce a summary of common issues.
Phase III (core set consensus, delivery solutions)
Three inter-professional workshops were held to finalize the core set and generate potential solutions for delivering it. Workshops comprised 8–14 participants, including Phase I clinical experts and Phase II educationalists, and were facilitated by members of the research team, including a patient (P.R.). Discussions were interactive, drawing on suggestions from Phases I and II, workshop participants and facilitators. Working in their professional groups, participants divided their Phase I core set into topics that could be delivered to all professions and topics that were only applicable to their own profession. The results were debated by the whole workshop, allowing the core set to be finalized, after which participants organized it into cohesive teaching units. Finally, participants worked in inter-professional groups to generate potential ways of delivering the core set, which were then discussed by the whole workshop. Data from all three workshops were collated, reviewed and summarized by the research team.
Ethics approval was given by the South West Multi-Centre Research Ethics Committee and individual participant consent obtained.
Results
Phase I: clinicians’ preliminary core set of topics
A total of 103 expert clinicians were invited to participate, of whom 47 consented and then enrolled 19 juniors (total n = 66, of whom 39 completed all three Delphi rounds) (Fig. 1). In Round 1, participants considered all 17 topics essential/preferable and 94 new issues were generated by ≥3 participants, giving 111 items to be taken forward into Round 2. After Round 2, using a conservative consensus of ≥60%, nurses retained 106 items, OTs 74 and PTs 76. After Round 3, using the more stringent ≥80% consensus, nurses retained 71 items, OTs 29 and PTs 26, some of which were common across professions (Table 1). Nurses had generated very detailed items compared with other HPs, and the wording of several overlapped; therefore, these three core sets were considered preliminary, to be fed into the Phase III workshops for inter-professional debate.
Table 1.
Clinicians’ preliminary consensus on core topics for their undergraduate students (Phase I Delphi)
Common (N, OT, PT)
|
Shared by two professions
|
Nurse-specific issues
|
Physiotherapy-specific issues
|
QoL: quality of life; A and P: Anatomy and Physiology; MDT: Multi-disciplinary Team; ADL: Activities of Daily Living; Pt Ed: Patient Education; MSK: Musculo-skeletal; DAS: Disease Activity Score; EMS: Early Morning Stiffness.
Phase II: educationalists’ challenges
Nineteen curriculum or clinical placement organizers were interviewed (N6, OT7, PT6). They reported that rheumatology issues are delivered within not only system-based modules (musculoskeletal), but also generic conditions modules (chronic illness, care of the elderly, enduring care) and generic skills modules (foundation skills, clinical thinking, skills for practice, occupational performance, anatomy and physiology). Clinical placements where rheumatology patients might be encountered include outpatients, general and orthopaedic wards, community and rheumatology units.
In response to the clinicians’ preliminary core sets of topics (Table 1), educationalists reflected that the growing emphasis on teaching transferable skills implies that condition-specific sessions such as rheumatology will become even less common, or will be taught through small, elective or student-driven seminars, inevitably leading to variability in coverage of any core set. For clinical exposure, there were concerns about access to and funding of clinicians to teach, and insurance concerns about patients on university premises, a perceived lack of rheumatology facilities and again the need for students to gain generic skills.
However, educationalists enthusiastically commented that many existing teaching methods could be utilized for delivering a rheumatology core set, including problem-based sessions, practical sessions, video-conferencing and e-learning. They suggested a range of resources such as Arthritis Research Campaign (ARC) literature, CDs and online discussion groups. Participants suggested that patient perspectives could be utilized, with visits from or videos of patients or vicariously through carers or speakers from charities.
Phase III: core set consensus, delivery solutions
The three workshops comprised 33 clinicians (N12, OT9, PT5), educationalists (N2, OT3, PT2) and a patient (P.R.), including several members of the research team who facilitated, and also contributed to the discussions around potential delivery methods. Several participants had combined clinical and educational roles.
Core set of rheumatology topics
All three workshops concluded that the items on each profession's preliminary core set could be delivered to all HP undergraduates, although some items should be covered in more depth for certain professions (e.g. medication for nurses, joint protection for OTs, exercise for PTs). When participants organized the items into cohesive teaching units, there was some variation in unit labels, but the contents were very similar across workshops. The three workshops’ proposals were collated and reviewed by the research team who refined any vaguely defined items, amalgamated several overlapping items and merged a few very detailed items into larger topics. This process clarified the six core teaching units: Anatomy and Physiology; Assessment; Management and Intervention; Psychosocial Issues; Patient Education; and the Multi-disciplinary Team, and their component topics (Table 2).
Table 2.
Consensus on core rheumatology teaching units for all undergraduate HPs
Anatomy and Physiology
|
Assessment
|
Management and Intervention
|
Psychosocial issues
|
Patient education/self-management
|
Multi-disciplinary Team
|
In greater depth for Nnurses, OToccupational therapists, PTphysiotherapists. ADL: Activities of Daily Living; DAS: Disease Activity Score.
Delivery of rheumatology core topics
Participants discussed the methods raised by educationalists (Phase II) for teaching rheumatology and also generated their own ideas, resulting in a broad list of options (Table 3). For example, case studies were thought potentially useful for translating generic skills training into rheumatological situations. Resources that could be developed to support teaching included developing a standard rheumatology teaching resource pack for universities and a peripatetic rheumatology tutor. Participants recommended teaching rheumatology to inter-professional groups to reinforce the concept of multi-disciplinary team working.
Table 3.
Suggestions for delivering rheumatology core teaching set
| Classroom teaching | Resources | Clinical placements | Clinicians | Patients |
|---|---|---|---|---|
|
|
|
|
|
IP: Inter-professional; DIPEX: Directory of Individual Patient Experiences.
Exciting opportunities for providing clinical exposure were proposed (e.g. short placements nested within longer generalist placements), which could accommodate more students, but these should have learning outcomes and be structured to include shadowing different team members, interviewing patients and self-directed learning. Tips for clinicians on how to teach in the workplace were raised (e.g. team review of a patient) as well as important suggestions for involving patients (e.g. as teachers supported by a facilitator) (Table 3).
Participants identified patient and clinician involvement as key to effective classroom and clinical teaching of the core set. Recognizing the limitations on curriculum time for disease-specific issues, they proposed two brief but intensive interventions, provided by educationalists, clinicians and patients working together. In the classroom, an inter-professional seminar (Rheumatology Chat Show) could involve groups of students interviewing patients to find out about life with arthritis and the journey to self-management. The students’ findings would be drawn together by clinical and educationalist facilitators using the core teaching topics as a basis (particularly management and intervention, psychosocial issues and patient self-management). For students on clinical placements, a ‘Rheumatology Road Show’, run by clinical rheumatology teams in collaboration with educationalists and patients could be staged. This hands-on exhibition could run throughout the day and students from all professions, on any placement throughout the host Trust, could ‘drop-in’ for an hour. This would allow them to interact with the Multi-disciplinary Team and patients, and introduce them to many of the core topics through clinical and research posters, aids and appliances displays, physiotherapy demonstrations and patient discussions. It was considered that these short but intensive interventions might capture the essence of rheumatology and be a memorable learning experience for students.
Motivators for careers in rheumatology
Eighteen recently-appointed participants completed the questions on motivation (N4, OT4, PT10). Eight could not recall any rheumatology exposure during undergraduate training (‘Cannot remember there being any specific rheumatology training’—Physiotherapist I). Ten participants said that clinical exposure to patients had motivated them (‘Clinical placements were the most inspiring aspect’—Physiotherapist J), while others identified professional role models, including clinicians (‘Inspired by excellent nursing staff who were excellent role models’—Nurse A), educationalists (‘Rheumatology lecturer at university’—Physiotherapist C) and the multidisciplinary team (‘Nursed some rheumatology patients on a medical ward when their unit was closed, and enjoyed the MDT work’—Nurse B). A third theme was the influence of formal study (‘Quite in-depth module, lectures covering RA and OA’—Occupational Therapist E). Seven participants suggested that combining the three themes of patient exposure, professional role models and formal study into a classroom experience would be a powerful teaching tool (‘A practical session with patient and their therapist would be extremely interesting and likely to promote enthusiasm. This approach was applied in neuro and everyone seemed to gain from it—even the patient.’—Physiotherapist J).
Discussion
This study combined the expertise of both clinicians and educationalists to reach a consensus on a minimum core set of topics for undergraduate rheumatology education for HPs and potential ways of delivering these. Core topics comprise Anatomy and Physiology; Assessment; Management and Intervention; Psychosocial Issues; Patient Education; and Multi-disciplinary Team collaboration, with each profession covering some aspects in greater depth as appropriate. In addition, participants have suggested how current best practice in education and clinical placements might be combined to enhance delivery of core components, highlighting the need for underpinning collaboration between clinicians, educationalists and patients.
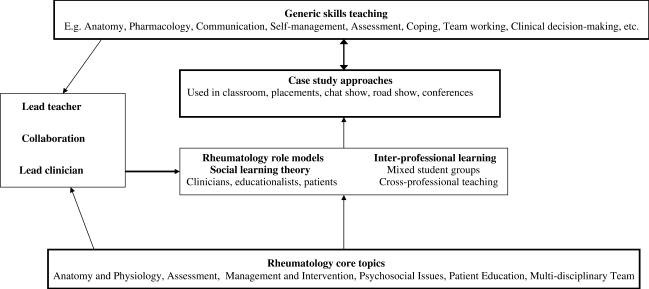
Most university courses focus on teaching transferable or generic knowledge and skills, as the basis for learning how to provide effective healthcare. It is likely that if asked, expert clinicians in most specialties would suggest that undergraduates would benefit from receiving disease-specific education in their area (e.g. diabetes, dermatology). As this would potentially overwhelm available curriculum time, teaching the generic skills that underpin healthcare practice, such as communication or coping theories, is likely to remain the only way of managing a time-limited curriculum. Clearly, five of the six rheumatology core topics agreed in this study could be generic skills (the exception being Anatomy and Physiology). However, there is little point in providing generic skills training unless students learn how to apply these to specific diseases in clinical care. Rheumatology case studies would be one way of incorporating rheumatology into the curriculum, by facilitating students in applying their generic skills training to particular patient scenarios, utilizing the rheumatology core set. For example, a case study around the journey into self-management of RA, could cover the six rheumatology core topics through diagnosis (Anatomy and Physiology; Assessment), management of common symptoms such as pain and fatigue (Management and Intervention; Multi-disciplinary Team working), through to coping and adaptation (Psychosocial Issues; Patient Education). Clear links could be made back to generic teaching on clinical reasoning, problem-solving, psychological reactions to illness, communication skills and behaviour change theories, fulfilling the government recommendation for principle-based teaching linked to patient pathways [3]. If classroom curriculum time is too limited even for this, then such a structured approach could be delivered as part of a clinical placement [20].
Inter-professional learning brings many benefits to health care students [21], but has a particular relevance to rheumatology where all team members are usually involved in care. Combined sessions involving not only nursing, OT and physiotherapy students but also medical, podiatry, psychology and pharmacy undergraduates should be considered. In addition, inter-professional teachers could be utilized: for example, OTs teaching nurses or nurses teaching medical students [22, 23].
Rheumatology clinical placements may be considered too narrow to provide the broad range of experience and exposure students require, particularly where nursing placements might last up to 24 weeks. Participants suggested brief, structured clinical placements, perhaps nested within longer placements. In other specialities, a week-long clinical attachment to theatres prompted 65% of the student nurse participants to consider theatres as a career option, while a 2-day rheumatology placement improved knowledge and enthusiasm (detailed data not reported) [9, 24]. Both interventions were carefully designed with pre-placement classroom preparation, structured clinical timetables and individualized learning outcomes. Thus, even a 2-h well-structured Rheumatology Chat Show or Rheumatology Road Show, linking the core topics to generic skills, might be effective and although unlikely to cover the core set sufficiently, is a practical solution likely to provide more rheumatology input than most current courses contain.
Recent entrants to rheumatology in this study, suggested that exposure to an enthusiastic role model (educationalist, clinician or patient) has a major impact on patient care and career choice. Workshop participants also identified that collaboration between educationalists, clinicians and patients is key to delivering the core set. These role model findings reflect the relevance of social learning theory to HP education [25] and suggest the importance of combining the expertise and enthusiasm of educationalists and rheumatology clinicians. Rheumatology teams and University departments need to work collaboratively to identify lead educationalists and clinicians who would work together to drive local initiatives forward. One model for successful collaboration between 10 Rheumatology Units and one University has been established to deliver the national, ARC-funded post-qualification Graduate Certificate in Rheumatology Practice, developed jointly by rheumatology clinicians and academics. Links between universities and hospital departments might be further facilitated by joint clinician/educationalist appointments.
Many of the teaching methods proposed by the participants are current best practice in education (e.g. small clinical project placements, national teaching package for universities [26–28]) while some are relatively novel (e.g. peripatetic tutor, chat show, road show). Debating these methods together and sharing best practice, enthused educationalists about teaching rheumatology, and also enthused clinicians to try different teaching approaches. A model for delivering the rheumatology core set could be to utilize role models (social learning theory) and inter-professional settings to explore rheumatology case studies (in the classroom, placements, chat shows and road shows), as a vehicle for translating generic skills into rheumatology situations, with local opportunities facilitated by collaboration between a lead clinician and a lead educationalist (Fig. 2).
Fig. 2.
Potential model for linking rheumatology core topics and generic skills through case studies.
Limitations of this study include difficulty in identifying a clear cut-off point for core topic consensus, always a contentious issue [18]; therefore, an inclusive approach was taken first (60%) followed by a more stringent approach (80%). The interviews with educationalists in Phase II were documented by hand on a standard sheet, which may have resulted in some missing data. However, interview summaries were immediately returned to participants for verification, clarification and addition. The inclusion of other professions would have been beneficial and the core set could now be explored for relevance to podiatry and psychology undergraduates. The strengths of the study are the combination of clinicians and educationalists in generating, debating and agreeing the core set and delivery methods. In addition, the research team had backgrounds in clinical care, education, nursing, OT, physiotherapy and medicine, and included a patient.
This study has identified a minimum, standardized set of six core rheumatology topics for undergraduate nurses, OTs and PTs, and a variety of potential delivery methods. Further research is now needed to refine the content of the six teaching units, evaluate the feasibility and costs of delivering these core teaching sets using some of the interventions proposed, and assess the effects on student knowledge, skills and attitudes. Where curriculum time and clinical placements are limited, brief interventions that last only a few hours might be helpful (Rheumatology Chat Show, Rheumatology Road Show, case study, standard teaching package). The outputs from the workshops in particular, demonstrated the benefits of collaboration between enthusiastic educationalists, clinicians and patients. The next step is for clinical nurses, OTs and PTs to link with their local university and establish collaborations for enhancing rheumatology teaching in ways that best suit local needs and resources.
Acknowledgements
The authors would like to thank the participants for giving up their time, and the ARC for funding this study.
Funding: The Arthritis Research Campaign has funded the study. Funding to pay the Open Access publication charges for this article was provided by the Arthritis Research Campaign.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1.Symmons D, Bankhead C. UK: Arthritis and Rheumatism Council for Research. 1994. Health care needs assessment for musculo-skeletal diseases: the first step–estimating the number of incident and prevalent cases. [Google Scholar]
- 2.Arthritis Research Campaign. Derbyshire: arc; 2002. Arthritis: the big picture. [Google Scholar]
- 3.Nursing and Midwifery Council. London: Nursing and Midwifery Council; 2004. Standards of proficiency for pre-registration nursing education. [Google Scholar]
- 4.The College of Occupational Therapists. London: The College of Occupational Therapists; 2003. Standards for education: pre-registration education standards. [Google Scholar]
- 5.Chartered Society of Physiotherapy. London: Chartered Society of Physiotherapy; 2002. The Curriculum Framework. [Google Scholar]
- 6.Nolan M, Nolan J. Rehabilitation, chronic illness and disability: the missing elements in nurse education. J Adv Nurs. 1999;29:958–66. doi: 10.1046/j.1365-2648.1999.00972.x. [DOI] [PubMed] [Google Scholar]
- 7.Hill J, Bird H, Lawton C, Harmer R, Wright V. An evaluation of the effectiveness, safety and acceptability of a nurse practitioner in a rheumatology outpatient clinic. Br J Rheumatol. 1994;33:283–8. doi: 10.1093/rheumatology/33.3.283. [DOI] [PubMed] [Google Scholar]
- 8.Almeida C, Clarke B, O’Brien A, et al. Current provision of rheumatology education for undergraduate nursing, occupational therapy and physiotherapy students in the UK. Rheumatology. 2006;45:868–73. doi: 10.1093/rheumatology/kel008. [DOI] [PubMed] [Google Scholar]
- 9.McCausland LL. A precepted perioperative elective for Baccalaureate nursing students. AORN J. 2002;76:1032–40. doi: 10.1016/s0001-2092(06)61005-3. [DOI] [PubMed] [Google Scholar]
- 10.Happel B, Rushworth L. Can educational methods influence the popularity of psychiatric nursing? Nurs Educ Today. 2002;20:318–26. doi: 10.1054/nedt.1999.0432. [DOI] [PubMed] [Google Scholar]
- 11.Jansen P, Nicholl H. Challenges in teaching undergraduate psychology courses to nursing students. Nurs Educ Today. 2007;27:267–70. doi: 10.1016/j.nedt.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 12.McCluskey A. Collaborative curriculum development: clinicians’ views on the neurology content of a new occupational therapy course. Australian OT J. 2000;47:1–10. [Google Scholar]
- 13.Department of Health. London: Department of Health; 2006. Modernising nursing careers. [Google Scholar]
- 14.Jones A, Maddison P, Doherty M. Teaching rheumatology to medical students: current practice and future aims. J Roy Coll Physicians. 1992;26:41–3. [PMC free article] [PubMed] [Google Scholar]
- 15.Kay L, Deighton C, Walker D, Hay E. Undergraduate rheumatology teaching in the UK: a survey of current practice and changes since 1990. Rheumatology. 2000;39:800–3. doi: 10.1093/rheumatology/39.7.800. [DOI] [PubMed] [Google Scholar]
- 16.Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32:1008–15. [PubMed] [Google Scholar]
- 17.Carr A, Gordon T. Defining the extended clinical role for allied health professionals in rheumatology. Chesterfield: ARC Conference Proceedings. 2001;12 [Google Scholar]
- 18.Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53:205–12. doi: 10.1111/j.1365-2648.2006.03716.x. [DOI] [PubMed] [Google Scholar]
- 19.Hayes N. Thematic qualitative analysis. In: Hayes N, editor. Doing psychological research. London: Open University Press; 2000. pp. 171–82. [Google Scholar]
- 20.Pollard C, Hibbert C. Expanding student learning using patient pathways. Nurs Standard. 2004;19:40–3. doi: 10.7748/ns2004.09.19.2.40.c3698. [DOI] [PubMed] [Google Scholar]
- 21.Department of Health. A health service of all the talents: developing the NHS workforce. London: HMSO; 2000. [Google Scholar]
- 22.Goh L, Samanta A, Cavendish S, Heney D. Rheumatology curriculum: passport to the future successful handling of the musculoskeletal burden? Rheumatology. 2004;43:1468–72. doi: 10.1093/rheumatology/keh335. [DOI] [PubMed] [Google Scholar]
- 23.Gadsby K, Deighton CM. The perceptions of final year medical students in rheumatology workshops when delivered by a consultant and a nurse clinical educator. Rheumatology. 2005;44:1047–50. doi: 10.1093/rheumatology/keh684. [DOI] [PubMed] [Google Scholar]
- 24.Cassady JR, McKay J, Nambayan A, Wade A. Rheumatology training enhances students long-term care skills. Nurs Health Care. 1987;8:39–41. [PubMed] [Google Scholar]
- 25.Mann KV. The role of educational theory in continuing medical education: has it helped us? J Contin Educ Health Prof. 2004;24:S22–30. doi: 10.1002/chp.1340240505. [DOI] [PubMed] [Google Scholar]
- 26.Prigg A, Mackenzie L. Project placements for undergraduate occupational therapy students: design, implementation and evaluation. Occ Ther Int. 2002;9:210–36. doi: 10.1002/oti.166. [DOI] [PubMed] [Google Scholar]
- 27.Arthritis Research Campaign. Chesterfield: Arthritis Research Campaign; 2005. Clinical assessment of the musculoskeletal system: a handbook for medical students. [Google Scholar]
- 28.JointZone: A study of rheumatology. [(23 March 2007, date last accessed)]; www.jointzone.org.uk.