Abstract
Osteoporosis affects more than 1.2 million women in England and Wales. Hip fractures are associated with increased mortality. The total cost of treating osteoporotic fractures in postmenopausal women is expected to rise to £2.1 billion by 2010. The National Institute for Health and Clinical Excellence (NICE) has issued guidelines for the secondary prevention of osteoporotic fractures in postmenopausal women. The objective of this study was to review the NICE guidelines and to assess the implementation of and compliance with these guidelines in a district general hospital.
Keywords: Compliance, Hip fractures, Guidelines, Implementation, Osteoporosis
Osteoporosis is defined as a progressive, systemic skeletal disorder characterised by low bone mass and micro-architectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture.1
Recent epidemiological data, based on a UK sample, show that 1.2 million women have osteoporosis in England and Wales.3 Osteoporosis results in about 60,000 hip fractures a year in the UK, 90% of which are in people over 50 years of age and 80% of which are in women. There are also some 50,000 wrist and 40,000 clinically diagnosed other fractures a year from osteoporosis.2
After sustaining hip fractures, many patients are unable to walk without aid or perform other activities of daily living and so are unable to live independently. Hip fractures are also associated with increased mortality. In the 12 months after a hip fracture, estimates of relative hip mortality risk vary from 2 to more than 10, depending on age.3
The total cost of treating osteoporotic fractures is huge – between £1.5–1.8 billion in 2000 and expected to increase to £2.1 billion by 2010.3
Hence, the National Institute for Health and Clinical Excellence (NICE) has issued guidelines on preservation of bone mass and fracture prevention. These guidelines were issued in January 2005 for the secondary prevention of osteoporotic fractures in postmenopausal women, and include:
For a woman aged 75 years or older, biphosphonates are considered as treatment option, without the need for Dexa scan. For a woman aged 65–74 years, biphosphonates are considered as treatment option with Dexa confirmed osteoporosis. For a woman younger than 65 years, biphosphonates are considered as treatment options if the woman has very low bone mineral density (BMD), with the T score of approximately −3.5 SD or below or confirmed osteoporosis plus one or more additional age-independent risk factors. This World Health Organization classification is based on the measurement of BMD with reference to the number of SD from the BMD in an average 25-year-old woman (T-score): (i) normal – T-score of −1 SD or more; (ii) osteopenia – T-score between −1 and −2.5 SD; (iii) osteoporosis – T-score below −2.5 SD; and (iv) established osteoporosis – T-score below −2.5 SD with one or more associated fragility fractures.
Raloxifene is considered as an alternative treatment option to biphosphonates, if the patient has any contra-indications or is physically unable to comply with special recommendations or shows unsatisfactory response or intolerance to biphosphonates.
Teriparatide is recommended for women over 65 years of age who cannot take a biphosphonate and have either an extremely low BMD or a very low BMD, suffered more than two fractures and have other non-age-related risk factors. Non-age-related risk factors are low body mass index (under 19 kg/m2), premature menopause, prolonged immobility, history of maternal hip fracture under the age of 75 years, and certain medical disorders independently associated with bone loss (such as chronic inflammatory bowel disease, rheumatoid arthritis, hyperthyroidism or celiac disease).
Dexa scan is recommended for all women aged below 75 years. However, treatment could commence with antiporotic measures even while she is waiting for the Dexa scan, based on clinical suspicion.
The objective of this study was to evaluate the awareness of and compliance with NICE guidelines in the secondary prevention of osteoporotic fractures in the postmenopausal women in a district general hospital in the UK.
Patients and Methods
The baseline audit was conducted at St Richard's Hospital, Chichester. This is a 2-star, 437-bedded district general hospital situated in West Sussex, with a catchment population of approximately 212,000. The average number of accident and emergencies seen are 49,000 per year. The average hospital in-patient admission rate is approximately 35,500 per year.
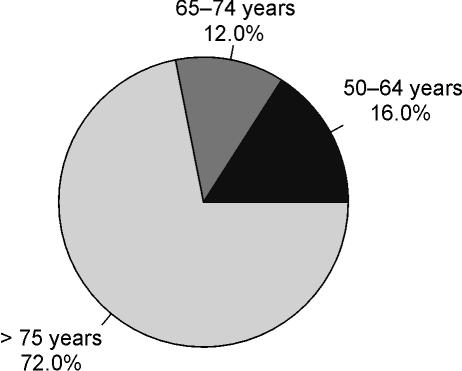
Data were collected on all consecutive postmenopausal women (above 50 years of age) with osteoporotic fractures treated as in-patients in this hospital, during the period 1 January 2005 to 31 March 2005 (Fig. 1).
Figure 1.
Study group age distribution.
The management of each patient was compared against the standard NICE guidelines by way of a retrospective study of case notes.
Results
We audited a total number of 100 in-patients admitted during the study period. None of these patients received a Dexa scan, which meant that the compliance rate calculated from Equation 1 was zero.
i.e. 0/(16 + 12) × 100 = 0%
Of the 72 patients above 75 years of age, only 15 received treatment with biphosphonates. There were 17 patients who met the criteria of exception. The compliance rate with regards to treatment (44.44%) was calculated with Equation 2 (Tables 1–3):
i.e. (15 + 17)/72 × 100 = 44.44%
Table 1.
Patients who could not and cannot be treated with biphosphonates or raloxifene or teriparatide as they had associated medical conditions
| 50–64 years | 65–74 years | 75 years | Total | |
|---|---|---|---|---|
| Total | 16 | 12 | 72 | 100 |
| Renal failure | – | – | 1 | 1 |
| Upper GI | – | 1 | 16 | 17 |
| Venous thrombosis | 1 | 2 | 3 | 6 |
| Liver failure | – | – | 1 | 1 |
| Bladder carcinoma | – | – | 2 | 2 |
| Breast carcinoma | – | – | 1 | 1 |
| None | 15 | 9 | 46 | 70 |
| Percentage | 93.8 | 75.0 | 63.9 | 70.0 |
Table 3.
Patients who were actually treated with antiporotic measures after admission and discharged with antiporotic medicines
| 50–64 years | 65–74 years | 75 years | Total | |
|---|---|---|---|---|
| Total | 16 | 12 | 72 | 100 |
| HRT | 2 | – | – | 2 |
| Calcium | – | 2 | 2 | 4 |
| Vitamin D | 1 | 2 | 8 | 11 |
| Raloxifene | – | – | 1 | 1 |
| Biphosphonates | – | – | 7 | 7 |
| None | 13 | 10 | 59 | 82 |
| Percentage | 81.3 | 83.3 | 81.9 | 82.0 |
Table 2.
Number patients who were already being treated with antiporotic measures at time of admission
| 50–64 years | 65–74 years | 75 years | Total | |
|---|---|---|---|---|
| Total | 16 | 12 | 72 | 100 |
| HRT | 2 | – | – | 2 |
| Calcium | – | 1 | 2 | 3 |
| Vitamin D | – | 1 | 5 | 6 |
| Raloxifene | – | – | 1 | 1 |
| Biphosphonates | – | – | 6 | 6 |
| None | 14 | 11 | 63 | 88 |
| Percentage | 87.5 | 91.7 | 87.5 | 88.0 |
There were 12 patients aged 65–74 years in the study group. None of these patients were treated with biphosphonates. There was one patient who met the criteria of exception. The compliance rate (8.33%) was calculated from Equation 3 (Tables 1–3):
i.e. (0 + 1)/12 × 100 = 8.33%
There were 16 patients aged 50–64 years in the study group. None received biphosphonates and none met the criteria of exception. Thus, the compliance rate calculated from Equation 4 was zero (Tables 1–3):
i.e. (0 + 0)/16 × 100 = 0%
Discussion
NICE issued its guidelines based on the recommendations of an Appraisal Committee.
For a woman aged 75 years or older, biphosphonates are considered as treatment option, without the need for Dexa scan. For a woman aged 65–74 years, biphosphonates are considered as treatment option with Dexa confirmed osteoporosis. For a woman younger than 65 years, biphosphonates are considered as treatment options only if the woman has very low BMD (i.e. T score of approximately −3.5 SD or below) or confirmed osteoporosis plus one or more additional age-independent risk factors. Dexa scan is recommended for this group of patients.
In our study, we found the implementation and compliance to be low. This could be due to the fact that the NICE guidelines were released only in January 2005 and the study was done during this period. However, the study will act as a baseline for future implementation of the guidelines so as to reach the desired target of 100% compliance.
All clinicians in NHS hospitals and primary care trusts who care for postmenopausal women who have had an osteoporotic fracture should review their current practice and policies to take account of the guidance set out above.
Conclusions
We recommend that all clinicians should be aware of the seriousness and magnitude of the problems associated with osteoporosis. We should be aware of the NICE guidelines and include Dexa scanning in the protocol for management either during hospitalisation or following discharge from the hospital. We should also educate the junior doctors and pharmacists regarding the appropriate use of antiporotic medications and general practitioners should be informed accordingly.
Acknowledgments
We should like to thank Ms Lynda Searle, Clinical Audit Manager for her support in this audit.
References
- 1.British National Formulary. 2005. Sep, pp. 385–9.
- 2.Department of Health. Health service circular, series no: HSC 1998/124. Issue date 21 July 1998.
- 3.NICE guidelines. Technology Appraisal 87. London: NICE; 2005. pp. 4–6. [Google Scholar]
- 4.Royal College of Physicians of London. Osteoporosis, new perspectives on causes, prevention and treatment. London: RCP; 1996. [Google Scholar]