SYNOPSIS
Objective.
The purpose of this study was to assess the relationship between pre-pregnancy maternal obesity and risk of infant death.
Methods.
In March 2004, maternal height and pre-pregnancy weight were added to the data collected on the Florida birth certificate. Using birth records linked to infant deaths, these data were used to assess the relationship between pre-pregnancy maternal obesity, as measured by body mass index, and infant death.
Results.
Pre-pregnancy maternal obesity was associated with increased odds of infant death. The increased risk was found with and without adjustments for maternal race, marital status, age, education, trimester prenatal care began, first birth, and tobacco use.
Conclusion.
There is a substantial and significant association between pre-pregnancy maternal obesity and infant death.
The large and growing prevalence of obesity among the U.S. population1 has led to increased concern in the medical and public health fields due to the strong relationships found among obesity, illness, and mortality.2 A 2003–2004 National Health and Nutrition Examination Survey showed that 17.1% of U.S. adults aged 20 and older were overweight and 16.5% were obese, which equates to 33.6% of the U.S. adult population being classified as either overweight or obese.3 Consistent with the increasing focus on weight and health outcomes of the general population, maternal pre-pregnancy weight is also being assessed for impact on perinatal health outcomes. Published studies have shown significant associations between pre-pregnancy maternal overweight/obese status and increased risks of pregnancy complications, such as cesarean delivery, gestational diabetes, preeclampsia/eclampsia, macrosomia, and congenital anomalies.4–9 In studies conducted in Sweden and Denmark, the relationship between maternal pre-pregnancy weight and pregnancy outcome was examined. These studies found that women with higher pre-pregnancy body mass index (BMI) values had increased odds of fetal death and early neonatal death compared with women who had lower pre-pregnancy BMI values.10–13
In 2005, the American College of Obstetricians and Gynecologists released guidance to obstetricians and gynecologists on obesity in pregnancy that recommended the collection of maternal height and weight during the first prenatal visit for BMI index calculations.14 The intent was to facilitate monitoring of weight gain during pregnancy, to advise pregnant women on the risk of obesity in pregnancy, and to assist in recommendations for postpartum weight loss and management.
In 2001, the National Center for Health Statistics Panel to Evaluate the U.S. Standard Certificates recommended that maternal height and pre-pregnancy weight be added to U.S. birth certificates to allow BMI calculation due to the association of maternal BMI to perinatal outcomes.15 In March 2004, the Florida Department of Health, Office of Vital Statistics implemented a revised Florida birth record that includes maternal height and pre-pregnancy weight. The addition of these two measures in 2004 made it possible to conduct Florida population-based analyses using BMI.
The purpose of this analysis was to assess and quantify the relationship between pre-pregnancy BMI and risk of infant death for the 2004 Florida birth cohort. To our knowledge, this analysis is the first to use a statewide birth cohort to examine the relationship between obesity and infant death.
METHODS
The data used for this analysis were the Florida resident birth records from March 2004 to December 2004. The birth records of infants born in January and February 2004 were excluded, because birth records in Florida prior to March 2004 did not include maternal height and pre-pregnancy weight information. For this analysis, 183,618 total resident birth records were linked to 1,288 resident infant death records. There were 17,317 (9.4%) linked records excluded due to missing data for the required variables. These excluded birth records were linked to 273 infant death records, which were also excluded. Remaining were 166,301 (90.6%) birth records linked to 1,015 (78.8%) infant death records for the analysis.
BMI is a measure of weight relative to height. The formula for BMI is: [(weight in pounds) / (height in inches)2] 3 703.16 BMI calculations were used to classify the maternal pre-pregnancy weight into five categories as defined by clinical guidelines from the the National Heart, Lung and Blood Institute's Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults:16 (1) underweight (BMI <18.5), (2) normal (BMI 18.5–24.9), (3) overweight (BMI 25.0–29.9), (4) obese (BMI 30.0–39.9), and (5) morbidly obese (BMI 40+).
Multivariate logistic regression was used to compute adjusted odds ratios (AORs) and associated confidence intervals for infant death. Infant death was used as the dependent variable and the BMI categories were used as dummy variables in Model 1 of the multivariate logistic regression analysis. Using Chi-square statistics, maternal race, marital status, age, education, tobacco use, first birth, and trimester of entry into prenatal care were found to be statistically significantly associated with obesity and infant death, and were therefore included in subsequent regression models to adjust for potential confounding. These variables were also assessed as potential effect modifiers for the BMI variables. This was done by using all first-level interaction terms between the BMI variables and the adjusting variables, in the logistic regression analysis.
In reviews of research literature, obesity has been found to be causally associated with diabetes mellitus, hypertension, and preeclampsia.17,18 These conditions have also been found to be associated with adverse perinatal outcomes.19–24 Assessments of risk for women with these conditions might affect the relationship between infant death and maternal pre-pregnancy weight. To determine the extent of the potential influence associated with these conditions, a subset analysis was performed that computed adjusted odds ratios for cases that did not have any of these aforementioned conditions indicated on the birth record. There were 150,369 of the 166,301 analysis records that met the criteria of “birth records without the previously listed maternal complications,” leaving 15,932 records excluded in this subset analysis. The AORs for women without the specified complications were compared to the AORs for all women to assess any differences in association.
RESULTS
Table 1 displays the frequency distributions for the independent variables and the infant death rates among the subgroups defined by the independent variables. The rates in Table 1 were unadjusted and show that higher infant death rates were associated with maternal obesity, black race, unmarried marital status, young age, older age, smoking, and late entry into prenatal care. In the obesity categories, the rate was lowest for the normal BMI category and the rates were higher for the underweight and the higher BMI categories.
Table 1.
Maternal demographic statistics and infant death rates for Florida infants born from March through December 2004
Includes diabetes, gestational diabetes, chronic hypertension, preeclampsia, and eclampsia
BMI = body mass index
Table 2 compares records excluded from the analysis because of missing values to records that were included in the analysis. As shown in Table 2, births that were linked to infant deaths were more likely to be excluded, as 21.2% of the 1,288 linked birth records were excluded and overall only 9.4% of the 183,618 total records were excluded. A similar pattern was evident for records of infants born weighing less than 500 grams. There were a small number of these births (n=325), but a relatively high proportion (29.5%) were excluded due to missing values. The distribution of maternal characteristics was similar between the records included and excluded in this analysis. For example, 12.1% of the births to black mothers were excluded, and 10.0% of the births to unmarried mothers were excluded, which was closer to the overall exclusion percentage of 9.4%.
Table 2.
Comparison of maternal characteristics for infants included in the analysis and infants excluded due to missing data for Florida infants born from March through December 2004
BMI = body mass index
Table 3 shows the results from a series of logistic regression models. Model 1 displays the unadjusted odds ratios for infant death associated with the four BMI categories: underweight (BMI <18.5), overweight (BMI 25.0–29.9), obese (BMI 30.0–39.9), and morbidly obese (BMI 40+). The reference group for the four BMI groups included infants whose mothers had a pre-pregnancy BMI in the normal range (18.5–24.9).
Table 3.
Infant death odds ratios for Florida infants born from March through December 2004 linked to infant deaths by maternal BMI
Adjusted for maternal race, age, marital status, education, tobacco use, first birth, and trimester of entry into prenatal care
Model 3 includes only births where the mother did not have chronic diabetes, gestational diabetes, chronic high blood pressure, pregnancy-related high blood pressure, preeclampsia, or eclampsia indicated on the birth record.
Statistically significant at the alpha=0.05 level
BMI = body mass index
OR = odds ratio
CI = confidence interval
Model 2 gives the odds ratios for the BMI variables adjusted for associations between the BMI variables and the demographic variables. As a result, all of the BMI odds ratios in Model 2 are lower than the odds ratios in Model 1. This suggests that a portion of the association between infant death and the BMI variables in Model 1 was due to the association between the BMI variables and the demographic variables.
Model 2 shows that infants born to women who were obese had odds of infant death that were 23% higher than the odds for the reference group of infants born to women with a normal BMI (AOR = 1.23, 95% confidence interval [CI] 1.03, 1.46). The association between maternal pre-pregnancy weight and infant death was more pronounced for infants born to women classified as morbidly obese with odds of infant death that were 70% higher than the reference group (AOR=1.70, 95% CI 1.28, 2.28).
In Model 3, regression analysis was performed on the subset of births with no indication of maternal chronic/gestational diabetes, chronic/gestational hypertension, preeclampsia, or eclampsia on the birth record. These subset criteria resulted in the exclusion of 15,932 records from the primary dataset, which left 150,369 records for subset analysis. As explained previously, these exclusions were performed to control directly for potential influence from possible associations between these conditions and the analysis variables. As shown in Table 2, the AORs in Model 3 are very close to those in Model 2, which indicates the results were not substantially affected by presence or absence of these conditions as recorded on the birth record.
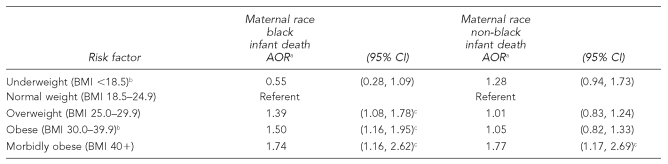
In assessing potential effect modification between the adjusting variables and the BMI variables, it was found that only the maternal race variable was associated with statistically significant effect modification. The implication of the effect modification is that the AORs were significantly different for the two racial subgroups. To illustrate the difference, the AORs were computed separately for the two racial subgroups of black and non-black (Table 4). As suggested by the effect modification analysis, the pattern of the BMI-infant mortality association, as indicated by the AORs, was different for these two groups.
Table 4.
Infant death odds ratios for Florida infants born from March through December 2004 linked to infant deaths by maternal BMI and race
Adjusted for maternal age, marital status, education, tobacco use, first birth, and trimester of entry into prenatal care
Statistically significant difference between black and non-black AORs at the alpha=0.05 level
Statistically significant at the alpha=0.05 level
BMI = body mass index
AOR = adusted odds ratio
CI = confidence interval
For infants born to black women, the AORs in the overweight and obese categories were statistically significant, while for infants born to non-black women, the corresponding AORs were not associated with increased risk. For example, in the obese category, the AORs for infants born to black mothers was 1.50 (95% CI 1.16, 1.95), and the corresponding AOR for infants born to non-black mothers was 1.05 (95% CI 0.82, 1.33). The AOR for infants born to black mothers was statistically significant, indicating that the odds of infant death were 50% higher for infants born to black mothers in the overweight BMI category compared with infants born to black mothers in the normal BMI category. The corresponding AOR for infants born to non-black mothers did not indicate increased odds of infant death. These two AORs were significantly different and indicate that obesity was associated with increased odds of infant death for black women, but not for non-black women. In contrast, the AORs in the morbidly obese category were significantly associated with increased risk for infants born to both maternal race groups with similar AORs, 1.74 (95% CI 1.16, 2.62) for infants born to black mothers, and 1.77 (95% CI 1.17, 2.69) for infants born to non-black mothers.
Additionally, in Table 4, the AORs for infant death in the underweight category were significantly different for infants born to black vs. non-black mothers. In the black underweight category, the AOR was 0.55 (95% CI 0.28, 1.09); in the non-black underweight category, the AOR was 1.28 (95% CI 0.94, 1.73). The 0.55 AOR was significantly different from the 1.28 AOR.
DISCUSSION
This analysis indicates that maternal obesity is associated with increased odds of infant death. This association was found before and after adjusting for maternal race, marital status, age, education, first birth, tobacco use, and trimester of entry into prenatal care. The results also suggest a different pattern of increased infant mortality odds for infants born to black and non-black women who are underweight or obese. High maternal BMI was associated with increased risk of infant death for infants born to overweight or obese black women, but not for infants born to overweight or obese non-black women. The difference between the odds ratios for infants born to black and non-black women was statistically significant in the underweight and in the obese categories. However, the difference was in opposite directions for these two categories, with the underweight category being associated with lower risk of infant death for infants born to black mothers and higher risk of death for infants born to non-black mothers. In the obese category, this pattern was different in that infants born to black women in this category were associated with higher risk of infant death, while infants born to non-black women were not. In the morbidly obese category, infants born to both black and non-black women experienced approximately the same increase in odds of infant death.
One potential source of bias in this analysis was the exclusion of records due to missing values for the required variables. As previously noted, births that were linked to infant deaths were more likely to be excluded from the analysis due to missing values. However, because more than 90% of the birth records and more than 78% of the infant death records were included in this analysis, it seems unlikely that the conclusions of this analysis have been substantively affected.
Another potential source of bias was the underreporting of maternal medical factors on the birth record, which were used to directly control for association with the analysis variables. If these conditions were present, but not recorded on the birth record, the incompleteness would have caused those cases to be misclassified as not having these factors. However, the results were virtually the same when cases with these maternal medical factors were excluded; therefore, any underreporting of these factors was unlikely to have affected the results.
CONCLUSIONS
This study's findings result in adding increased risk of infant death to the list of poor health outcomes associated with obesity. In April 2006, the Centers for Disease Control and Prevention (CDC) published “Recommendations to Improve Preconception Health and Health Care—United States,” which emphasized the need to improve a woman's health prior to conception.25 In this publication, obesity was one of 14 risk factors emphasized to be addressed prior to pregnancy, and was associated with the perinatal adverse outcomes of neural tube defects, preterm delivery, diabetes, cesarean section, and hypertensive and thromboembolic disease.
A recent article reviewing the history of preconception care noted a current trend among some medical groups to integrate preconception care into primary health care,26 but not all women have access to primary health care. Considering that approximately 18% of adults 18 to 64 years of age did not have a usual source of health care in 2004–2005, and about 13% were women (age adjusted),1 it is important that interventions are offered outside traditional health-care settings. One recommendation by the CDC workgroup was the integration of aspects of preconception health into existing local public health and related programs, including community-based approaches.25 The integration of an important component of preconception health and obesity prevention into effective community-based interventions may lead to beneficial outcomes for the overall population, including women of childbearing age.
Further investigation is needed to determine if a direct association exists between maternal weight (both obesity and underweight) and infant death. Researchers should be encouraged to conduct analyses for U.S. states that have included maternal height and pre-pregnancy weight on the birth certificate to assess the consistency and strength of associations between infant mortality and maternal pre-pregnancy weight. Given the relationships of social, economic, and environmental factors on health, future analyses should also consider the role of other important variables, such as income, health-care access, and quality, when assessing risks of poor perinatal outcomes.
REFERENCES
- 1.National Center for Health Statistics (US) Health, United States, 2007, with chartbook on trends in the health of Americans. Hyattsville (MD): NCHS; 2007. [PubMed] [Google Scholar]
- 2.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 4.Baeten JM, Bukuski EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health. 2001;91:436–40. doi: 10.2105/ajph.91.3.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu GC, Rouse DJ, DuBard M, Cliver S, Kimberlin D, Hauth JC. The effect of the increasing prevalence of maternal obesity on perinatal morbidity. Am J Obstet Gynecol. 2001;185:845–9. doi: 10.1067/mob.2001.117351. [DOI] [PubMed] [Google Scholar]
- 6.Cedergren MI, Källen BAJ. Maternal obesity and infant heart defects. Obes Res. 2003;11:1065–71. doi: 10.1038/oby.2003.146. [DOI] [PubMed] [Google Scholar]
- 7.Ehrenberg HM, Mercer BM, Catalano PM. The influence of obesity and diabetes on the prevalence of macrosomia. Am J Obstet Gynecol. 2004;191:964–8. doi: 10.1016/j.ajog.2004.05.052. [DOI] [PubMed] [Google Scholar]
- 8.Watkins ML, Rassmussen SA, Honein MA, Botto LD, Moore CA. Maternal obesity and risk for birth defects. Pediatrics. 2003;111(5 Part 2):1152–8. [PubMed] [Google Scholar]
- 9.Scialli AR, Public Affairs Committee of the Teratology Society. Teratology public affairs committee position paper: maternal obesity and pregnancy. Birth Defects Res A Clin Mol Teratol. 2006;76:73–7. doi: 10.1002/bdra.20236. [DOI] [PubMed] [Google Scholar]
- 10.Nohr EA, Bech BH, Davies MJ, Frydenberg M, Henriksen TB, Olsen J. Prepregnancy obesity and fetal death: a study within the Danish national birth cohort. Obstet Gynecol. 2005;106:250–9. doi: 10.1097/01.AOG.0000172422.81496.57. [DOI] [PubMed] [Google Scholar]
- 11.Cnattingius S, Bergström R, Lipworth L, Kramer MS. Prepregnancy weight and the risk of adverse pregnancy outcomes. N Engl J Med. 1998;338:147–52. doi: 10.1056/NEJM199801153380302. [DOI] [PubMed] [Google Scholar]
- 12.Kristensen J, Vestergaard M, Wisborg K, Kesmodel U, Secher NJ. Pre-pregnancy weight and the risk of stillbirth and neonatal death. BJOG. 2005;112:403–8. doi: 10.1111/j.1471-0528.2005.00437.x. [DOI] [PubMed] [Google Scholar]
- 13.Cedergren MI. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol. 2004;103:219–24. doi: 10.1097/01.AOG.0000107291.46159.00. [DOI] [PubMed] [Google Scholar]
- 14.American College of Obstetricians and Gynecologists. ACOG Committee opinion number 315, September 2005. Obesity in pregnancy Obstet Gynecol. 2005;106:671–5. doi: 10.1097/00006250-200509000-00054. [DOI] [PubMed] [Google Scholar]
- 15.National Center for Health Statistics (US) Washington: NCHS; 2000. Report of the Panel to Evaluate U.S. Standard Certificates. [Google Scholar]
- 16.National Heart, Lung, and Blood Institute, National Institute of Diabetes and Digestive and Kidney Diseases. Washington: National Institutes of Health (US); 1998. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. NIH Publication 98-4083. [Google Scholar]
- 17.National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health risk. Arch Intern Med. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 18.O'Brien TE, Ray JG, Chan W. Maternal body mass index and the risk of preeclampsia: a systemic overview. Epidemiology. 2003;14:368–74. doi: 10.1097/00001648-200305000-00020. [DOI] [PubMed] [Google Scholar]
- 19.Fretts RC. Etiology and prevention of stillbirth. Am J Obstet Gynecol. 2005;193:1923–35. doi: 10.1016/j.ajog.2005.03.074. [DOI] [PubMed] [Google Scholar]
- 20.Hedderson MM, Ferrara A, Sacks DA. Gestational diabetes mellitus and lesser degrees of pregnancy hyperglycemia: association with increased risk of preterm birth. Obstet Gynecol. 2003;102:850–6. doi: 10.1016/s0029-7844(03)00661-6. [DOI] [PubMed] [Google Scholar]
- 21.Gaugler-Senden IP, Huijssoon AG, Visser W, Steegers EA, de Groot CJ. Maternal and perinatal outcome of preeclampsia with an onset before 24 weeks' gestation: audit in a tertiary referral center. Eur J Obstet Gynecol Reprod Biol. 2006;128:216–21. doi: 10.1016/j.ejogrb.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 22.Jenkins SM, Head BB, Hauth JC. Severe preeclampsia at <25 weeks of gestation: maternal and neonatal outcomes. Am J Obstet Gynecol. 2002;186:790–5. doi: 10.1067/mob.2002.122290. [DOI] [PubMed] [Google Scholar]
- 23.Sibai BM, Lindheimer M, Hauth J, Caritis S, VanDorsten P, Klebanoff M, et al. Risk factors for preeclampsia, abruptio placentae, and adverse neonatal outcomes among women with chronic hypertension. N Engl J Med. 1998;339:667–71. doi: 10.1056/NEJM199809033391004. [DOI] [PubMed] [Google Scholar]
- 24.Solomon CG, Seely EW. Hypertension in pregnancy. Endocrinol Metab Clin N Am. 2006;457:157–71. doi: 10.1016/j.ecl.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Johnson K, Posner SF, Biermann J, Cordero JF, Atrash HK, Parker CS, et al. Recommendations to improve preconception health and health care—United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep. 2006;55(RR-6):1–23. [PubMed] [Google Scholar]
- 26.Freda MC, Moos MK, Curtis M. The history of preconception care: evolving guidelines and standards. Matern Child Health J. 2006;10(5) Suppl:S43–52. doi: 10.1007/s10995-006-0087-x. [DOI] [PMC free article] [PubMed] [Google Scholar]