Abstract
Similar to patients with orbitofrontal cortex lesions, substance dependent individuals (SDI) show signs of impairments in decision-making, characterised by a tendency to choose the immediate reward at the expense of severe negative future consequences. The somatic-marker hypothesis proposes that decision-making depends in many important ways on neural substrates that regulate homeostasis, emotion and feeling. According to this model, there should be a link between abnormalities in experiencing emotions in SDI, and their severe impairments in decision-making in real-life. Growing evidence from neuroscientific studies suggests that core aspects of substance addiction may be explained in terms of abnormal emotional guidance of decision-making. Behavioural studies have revealed emotional processing and decision-making deficits in SDI. Combined neuropsychological and physiological assessment has demonstrated that the poorer decision-making of SDI is associated with altered reactions to reward and punishing events. Imaging studies have shown that impaired decision-making in addiction is associated with abnormal functioning of a distributed neural network critical for the processing of emotional information, including the ventromedial cortex, the amygdala, the striatum, the anterior cingulate cortex, and the insular/somato-sensory cortices, as well as non-specific neurotransmitter systems that modulate activities of neural processes involved in decision-making. The aim of this paper is to review this growing evidence, and to examine the extent of which these studies support a somatic-marker model of addiction.
Key Words: Decision-making, addiction, somatic states, craving, ventromedial prefrontal cortex, amygdala, dopamine, serotonin
INTRODUCTION
One of the important characteristics of human drug addiction is the continuous consumption of abused substances, despite a rise in negative consequences, including medical, social and legal problems [6,15]. This is quite similar to patients with orbitofrontal cortex lesions in that they both show signs of impairments in judgement and decision-making, characterised by a tendency to choose the immediate reward, at the expense of severe negative future consequences. The question is: why are substance dependent individuals so insensitive to the future consequences of their drug seeking behaviour and have difficulties making the right choices? Several models of addiction have been proposed to explain the compulsive drug seeking of individuals with substance dependence [41,52,60]. This article will apply a “somatic marker” model of addiction to explain the “myopia” for the future manifested in the behavioural decisions of many individuals with substance dependence problems. The somatic-marker hypothesis [34] was originally proposed in order to account for the underlying neural mechanisms of this type of “myopia for the future” in a group of neurological patients with orbitofrontal cortex lesions. The central idea behind this hypothesis is that the process of decision-making depends in many important ways on neural substrates that regulate homeostasis, emotion, and feeling [34]. Later studies have suggested that this somatic marker model can also be applied to explain the “myopia for the future” characteristic of many substance dependent individuals (SDI) [6,15]. The somatic-marker model can also account for the hypersensitivity to immediate reward and insensitivity to delayed punishment observed in SDI [11,16].
The primary aim of this article is to review a growing line of evidence from behavioural, physiological, and imaging studies on substance addiction, and to examine the extent of which these studies support a somatic marker model of addiction.
A Somatic Marker Model of Addiction
The somatic marker framework provides a systems-level neuroanatomical and cognitive framework for decision-making, and for choosing according to long-term outcomes rather than short-term ones. The main point of the somatic-marker model is that decision-making is a process guided by emotions. The model attributes SDI difficulty to make advantageous decisions in real-life to a defect in an emotional mechanism that rapidly signals the prospective consequences of an action, and accordingly assists in the selection of the advantageous response option. This emotional mechanism is a somatic state, a special instance of feelings that arise in bioregulatory processes and can be enacted in the body, involving physiological modifications (“body loop”), or in brain areas involved in the representation of emotional states (“as if body loop”).
1. Induction of Somatic States
Somatic states can be induced from (1) primary inducers, and (2) secondary inducers. The main distinction between primary and secondary inducers hinges on the process by which they are experienced. Primary inducers are innate or learned stimuli that induce pleasurable or aversive states. Once present in the immediate environment, they automatically and obligatorily elicit a somatic response. The actual encounter of a drug by a SDI is an example of primary inducers. Secondary inducers, on the other hand, are entities generated by the recall of a personal or hypothetical emotional event, i.e., “thoughts” and “memories” of the primary inducer, which elicit a somatic response. The recall or imagination of a drug experience by a SDI is one example of secondary inducers [13].
It has been proposed that the amygdala is a critical substrate in the neural system necessary for triggering somatic states from primary inducers. This somatic state is evoked via effector structures such as the hypothalamus and autonomic brainstem nuclei that produce changes in internal milieu and visceral structures along with other effector structures such as the ventral striatum, periacqueductal gray (PAG), and other brainstem nuclei, which produce changes in facial expression and specific approach or withdrawal behaviours [13].
Signals from these somatic states are relayed to the brain. Signals from activated somatic states lead to the development of somatic state patterns in brainstem nuclei (e.g., the parabrachial nuclei (PBN)), and in somatosensing cortices (e.g., insular and somatosensory I and II cortices, and cingulate cortices). After a somatic state has been triggered by a primary inducer and experienced at least once, a pattern for this somatic state is formed. The subsequent presentation of a stimulus that evokes memories about a specific primary inducer will then operate as a secondary inducer. Secondary inducers are presumed to re-activate the pattern of somatic state belonging to a specific primary inducer. For example, recalling or imagining the experience of a drug re-activates the pattern of somatic state belonging to the actual previous encounter of that drug. However, the somatic state generated by the recall or imagination of using a drug (secondary inducer) is usually fainter than one triggered by an actual use of that drug (primary inducer).
Provided that somatic state representations in somatosensing cortices develop normally, triggering somatic states from secondary inducers becomes dependent on cortical circuitry in which the orbitofrontal and ventromedial prefrontal cortex plays a critical role. The orbitofrontal/ ventromedial prefrontal cortex is a trigger structure for somatic states from secondary inducers [13]. The ventromedial prefrontal cortex (VMPFC) includes the medial sector of the orbitofrontal cortex, the subgenual part of the anterior cingulate, and the ventral region of the medial prefrontal cortex, thus encompassing Brodmann’s areas 25, lower 24, 32, and medial aspect of 11, 12, and 10, and the white matter subjacent to all these areas [7].
2. Operation of Somatic States
During the pondering of a decision, somatic states are triggered by primary (drug cues) or secondary inducers (thoughts about taking drugs) (See Fig. 1, a and b). Once induced, they participate in two functions (see Fig. 1, c). (i) In one, they provide a substrate for feeling the emotional state. (ii) In the other, they provide a substrate for biasing decisions.
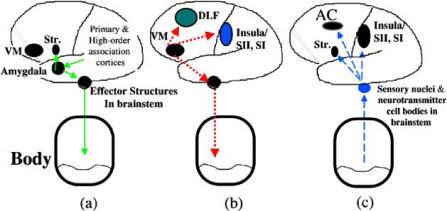
Fig. (1).
A schematic model of somatic state activation and decision-making. (a) The amygdala is a trigger structure for emotional (somatic) states from primary inducers. It couples the features of primary inducers, which can be processed subliminally (e.g., via the thalamus) or explicitly (e.g., via early sensory and high-order association cortices), with effector structures that trigger the emotional/somatic response. (b) The ventromedial prefrontal (VM) cortex is a trigger structure for emotional (somatic) states from secondary inducers. It couples knowledge of events held temporarily in working memory (which is dependent on dorsolateral prefrontal (DLF) cortices) to effector structures that induce the somatic responses, and to structures holding representations of previous feeling states (e.g., Insula and Somatosensory I (SI) and Somatosensory II (SII) cortices).
During the pondering of a decision, somatic states are triggered by primary (drug cues) or secondary inducers (thoughts about taking drugs). Once induced, their ascending feedback signals participate in two functions (c): in one they provide a substrate for feeling the emotional state, through the somatosensing cortices (Insula/SII, SI); in the other they provide a substrate for biasing decisions through motor effector structures such as the striatum (Str.) and anterior cingulate cortex (AC) and adjacent cortices.
(i). Feeling the Emotional State
The insular/somatosensory I and II cortices are often involved in emotional feelings [35,36]. Evidence suggests that there may be two variant forms of feelings dependent on partially separate neural sectors. This evidence is derived from studies on pain showing dissociation between two sensory aspects of pain. One is related to feeling the pain itself, so called “pain sensation”, and the other is related to discomfort and the desire to avoid the pain, so called “pain affect” [93]. In the case of drugs, Berridge and Robinson [17,18] have proposed a model that dissociates the “liking” from the “wanting” effects of drugs. The “liking” effects include feelings of pleasure and affective facial reactions during the pleasurable state. The “wanting” effects include the desire and urge to obtain the drug. It is suggested that the insular/somatosensory cortices are necessary substrates for the feeling of euphoria (not action related). On the other hand, the supracallosal sector of the anterior cingulate cortex is necessary for the feeling of craving (related to the action of seeking, obtaining, and consuming the drug). In support, studies have revealed changes in activity in the insular and somatosensory cortices in association with euphoric experience of acute doses of opiate and stimulant drugs [24,72,117]. Craving has also been linked to activity in the supracallosal sector of the anterior cingulate cortex in functional neuroimaging studies [28].
(ii). Biasing the Decision to Select a Response
In order for somatic signals to influence cognition and behaviour, they must act on appropriate neural systems:
One target for somatic state action is the striatum. This is consistent with several investigations that suggested that the amygdala-ventral striatum system is important for drug stimulus-reward (incentive) learning [67,129], and the control of drug-related cues over behaviour [26,67]. Other relevant target structure for somatic state action is the supracallosal sector of the anterior cingulate, and perhaps the adjacent supplementary motor area (SMA). This is consistent with a number of studies that indicated that these areas are often involved in the experience of craving, which is related to the action of seeking the drug [28].
There are other neural sites where ascending somatic signals exert influence on cognition. At the level of the lateral orbitofrontal and dorsolateral prefrontal region, the biasing mechanism of somatic states is at the level of “thought” or “memory”, and not behavioural action. In other words, as one deliberates on several options and scenarios held in their working memory, the biasing effect of somatic states is to endorse some options and reject other ones, before any of these options is translated into actions.
Once somatic states from primary and/or secondary inducers are induced in the body, a large number of channels convey body information to the central nervous system (e.g., spinal cord, vagus nerve, humoral signals). Evidence suggests that the vagal route is especially critical for relaying somatic signals [78]. Although research in this area is still in progress, early evidence suggests that the biasing action of somatic states on behaviour and cognition is mediated by the release of neurotransmitters. Indeed, the cell bodies of the neurotransmitters dopamine (DA), serotonin (5-HT), noradrenaline (NA), and acetylcholine (Ach) are located in the brainstem; the axon terminals of these neurotransmitter neurons synapse on cells and/or terminals all over the cortex [20]. When somatic state signals are transmitted to the cell bodies of serotonin neurons, for example, the signalling influences the pattern of serotonin release at the terminals. In turn, changes in serotonin release modulate synaptic activities of neurons subserving behaviour and cognition within the reflective system. This chain of neural mechanisms provides a way for somatic states to exert a biasing effect on decisions. Fig. 2 presents a diagram illustrating different levels at which somatic states can bias decisions via the release of neurotransmitters (Fig. 2).
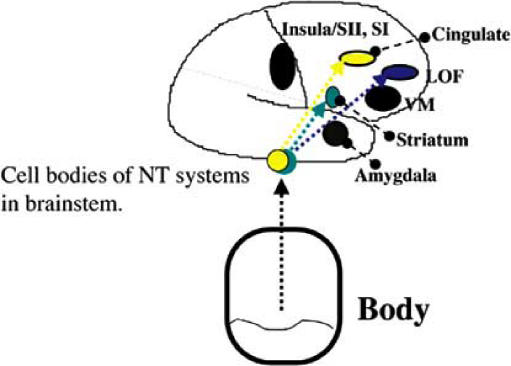
Fig. (2).
A diagram illustrating three different levels at which somatic states can bias decisions via the release of neurotransmitters (NT). (1) Dopamine biases decisions covertly (perhaps through action in the striatum and affective sector of anterior cingulate (Brodmann Area (BA) 25 and lower 24, 32). (2) Serotonin biases decisions overtly (perhaps through action in the cognitive sector of anterior cingulate and probably the adjacent SMA (Supplementary Motor Area)). (3) Somatic states also bias working memory in the LOF (lateral orbitofrontal and dorsolateral regions of the prefrontal cortex); They help endorse or reject “thoughts”, “options”, or “scenarios” brought to mind during the pondering of decisions, i.e., before their translation into action. The neurotransmitter system that mediates this biasing function remains to be determined.
Thus, once somatic states are enacted in the body (bodyloop) or in the brainstem (as-if-body-loop) via direct and indirect connections between the amygdala and the VMPFC, and the neurotransmitter nuclei within the brainstem [20,87], they can then influence activity in (1) regions involved in body mapping, i.e., holding patterns of somatic states that help generate feelings; (2) regions involved in the triggering of somatic states (e.g., amygdala and ventromedial prefrontal cortex), so that the threshold for triggering subsequent somatic states is increased or decreased; (3) regions involved in working memory (e.g., lateral orbitofrontal, dorsolateral prefrontal, and other high order association cortices), so that a particular representation is strengthened or weakened; and finally (4), somatic state signals influence activity in regions concerned with motor responses and behavioural actions (e.g., striatum and anterior cingulate/ supplementary motor area (SMA)).
The significance of this neural arrangement is that regardless of how somatic states are triggered, i.e., impulsively (primary induction) or reflectively (secondary induction), once they are triggered, they can gain access to cortical and subcortical neurons subserving cognition. Thus, depending on their strength, they have the capacity to modify and influence cognition.
BEHAVIOURAL AND PHYSIOLOGICAL STUDIES
According to the somatic-maker model, which proposes that decision-making is a process guided by emotions [7,9,34], there should be a link between abnormalities in expressing emotions and experiencing feelings in SDI on the one hand, and severe impairments in decision-making on the other hand [6,7]. This section will review evidence that supports this notion.
Decision-Making in Substance Dependent Individuals
The real life problems in judgement and decision-making often observed in substance dependent individuals (SDI) have led to initial studies aimed at testing the performance of SDI on behavioural paradigms of decision-making. Since then, a number of studies that used similar decision-making paradigms have shown impairments in decision-making performance among alcohol, cannabis, cocaine, opioids, and methamphetamines abusers [15,53,55,65,85,90,91,92,99]. Decision-making deficits have also been reported in populations who are at high risk for drug abuse, such as adolescents with externalising behaviour disorders [38]. Interestingly, impaired decision-making has been observed also in individuals with Antisocial Personality Disorder (APD) [82,83,113], a psychiatric disorder that is robustly associated with substance dependence, and which involves severe disturbances in emotion processing [19].
The evidence for impaired decision-making in SDI stems from studies using different decision-making paradigms, including tasks of delayed discounting [65,85], betting tasks [99], and probabilistic choice tasks [55,90,91]. Most of these tasks do not speak directly of the validity of the somatic-marker model. Nonetheless, the most frequently used paradigm to assess decision-making is the Iowa Gambling Task (IGT) [15,39,53,85,92,130], which was initially developed to investigate the decision-making defects of neurological patients in real-life, and to investigate the somatic-marker hypothesis further. This task factors a number of aspects: immediate rewards and delayed punishments, risk, and uncertainty of outcomes [6]. The task has been described in detail elsewhere [10,12]. Briefly, in the IGT, participants have to choose between decks of cards that yield high immediate gain but larger future loss, and decks that yield lower immediate gain but a smaller future loss. As such, the participants’ choices are largely influenced by different schedules of immediate reward and future punishment: decks A′ and B′ yield an average immediate reward-payoff that is greater than that of decks C′ and D′, but they also lead to harsher penalties, thus producing an overall negative expected value, i.e., they are disadvantageous in the long run. It is important to note that in this task, it is difficult for an individual to keep track of the rewards and punishments encountered in each deck, and therefore, performance in the task is not entirely based on computations of the net value of each deck. Studies have shown that a parsimonious explanation for how normal individuals perform this task advantageously is that their response selection becomes largely guided by signals from emotional representations of prior experiences with reward and punishment, i.e., somatic markers. These emotional signals or somatic markers are often unconscious to the individual in whom they are enacted, albeit that they can become conscious and experienced as a “hunch” or a “gut feel” that a given choice may be good or bad [14,31]. A number of critics of the somatic-marker hypothesis have argued that alternative explanations may equally account for normal/ altered performance in the IGT. For example, a recent study in healthy volunteers has shown that the reinforcement schedule of the IGT is more cognitively penetrable than previously believed [76]. Furthermore, alternative explanations have been proposed to explain the altered performance of different clinical populations in the IGT, including working memory [25,58] and reversal learning deficits [43,101], or increased risk-taking [30]. Although this remains as a limitation, psychophysiological [11,16] and cognitive modelling analyses [106,107] strongly support the notion that emotional factors associated with affective processing of reward and punishment play a significant role in the decision-making performance of SDI on the IGT.
In a series of studies using the IGT, Bechara et al. compared the performance of SDI to patients with damage to the orbitofrontal/ VMPFC [11,16]. These studies also included physiological measures of autonomic activity before and after making a choice in the IGT. The physiological responses triggered after making the choice and seeing the outcome (i.e., gain or loss of a certain amount of money) were called (i) reward/punishment responses; and those generated before making the choice were called (ii) anticipatory response, i.e., responses triggered during the time the participant was pondering from which deck to chose. Good performance in the IGT has been shown to be linked to the development of these anticipatory emotional responses, which in this case were changes in the skin conductance response (SCR), especially before selecting cards from the disadvantageous decks (A and B). It was suggested that these anticipatory emotional responses help guide decision-making away from disadvantageous choices (i.e., avoid decks A and B, and choose from decks C and D) [12,14,31]. In a study that used the IGT to measure behavioural decisions, and the SCR to measure anticipatory and reward/punishment responses in SDI, the behavioural and physiological results revealed that there were at least two different subgroups within this SDI population [11]. One subgroup of SDI (a minority of the sample) showed a behavioural profile similar to that of healthy participants, i.e., they selected more cards from the advantageous decks.
They also showed a physiological profile similar to healthy participants, in that they began to trigger anticipatory SCRs before selecting cards from the bad decks. By contrast, another subgroup of SDI (a majority of the sample) exhibited behavioural and physiological profiles that were different from healthy participants, and more similar to patients with orbitofrontal/VMPFC damage, i.e., they chose disadvantageously on the task, and they failed to acquire anticipatory SCRs.
In a subsequent study, the authors used a variant version of the IGT, in which they reversed the order of reward and punishment contingencies, so that the advantageous decks yielded high immediate punishment and even higher future reward, and the disadvantageous decks had lower immediate punishment, and even lower long-term reward. The combination of the behavioural results from the original and variant tasks, in conjunction with physiological responses recorded during the performance of both tasks, helped discriminate between two other sub-groups: those who were hypersensitive to immediate reward and those who were insensitive to long-term consequences [16]. In this way, they identified three sub-populations of SDI: one small subpopulation of SDI that was indistinguishable from healthy participants, a second small subpopulation that was indistinguishable from orbitofrontal/ VMPFC lesion patients, and a third larger sub-population of SDI that was different from the other two; these SDI exhibited signs of hypersensitivity to reward, as evidenced by impaired performance on the original IGT, normal performance on the variant version, and abnormally high reward skin conductance responses in both tasks. Interestingly, these subpopulations did not differ in terms of basic neuropsychological abilities or clinical characteristics such as severity of drug use. A recent study has replicated this pattern of behavioural and physiological response using the Cambridge Gamble Task paradigm [44] that was designed to isolate different components of the IGT [30]. In this study, polydrug users selected more risky choices in the high-risk conditions of the task, and failed to generate increased SCR responses when making riskier decisions with regard to healthy participants.
Another potential area of research, not yet fully explored is investigation of the development of substance dependence among neurological patients with damage to the VMPFC or other areas critical to somatic-marker processing. Certainly, people with head injuries (which often involve the VMPFC) have a higher incidence of substance abuse. The problem is that it is difficult to determine in this population whether the head injury facilitated the drug abuse problem, or whether the head injury followed substance abuse. Although there is some evidence to suggest that frontal lesion patients present with a higher vulnerability for developing substance use disorders [4,37], more research is needed to provide firm support for this hypothesis.
The evidence thus far points to the presence of decision-making impairments in SDI as measured by different behavioural paradigms. Different studies using the IGT have shown that poorer decision-making performance in SDI is associated with abnormal generation of anticipatory emotional responses (somatic markers), which precede the selection of cards from high-risk decks. Abnormal triggering and/or processing of these somatic markers have also been reported in healthy participants who perform poorly in the IGT [31,108]. The development of these anticipatory somatic markers seems to be detected only in complex paradigms of decision-making, such as the IGT, but not in other simpler cognitive tasks of executive functions [44]. It is important to note that abnormal processing of somatic-markers and defective decision-making in the IGT have not been consistently associated with clinical characteristics of substance dependence, including severity of drug abuse. Although strong conclusions cannot be drawn from the lack of correlations, the somatic-marker model assumes that at least some of the decision-making alterations observed in SDI may have actually preceded the drug abuse stage, and in fact, served as a predisposing factor that contributed to the switch from a casual drug use to a compulsive and uncontrolled substance dependence problem. This becomes quite pertinent in view of the fact that even among drug naïve individuals, there are individual differences in the capacity to make advantageous decisions, including sensitivity to reward/insensitivity to punishment, and in decision-making performance as measured by the IGT [31,108]. This raises the question of whether these “emotional” and decision-making measures serve as markers predictive of whether these drug naïve individuals are more susceptible to succumbing to drug abuse and dependence. Most importantly, although these pre-existing differences by themselves, may not induce decision-making impairments that are severe enough to trigger and maintain substance abuse, it is possible that their interaction with some neuroadaptive effects of abused drugs exacerbates the decision-making impairments that lead to substance dependence problems.
Overall, these results provide strong support for the hypothesis that impaired decision-making in SDI is associated with altered reactions to rewarding and punishing events, as well as altered elicitation of emotional signals that help forecast or anticipate the consequences of future events.
Emotion Processing in Substance Dependent Individuals
There are relatively few studies that examined emotional perception and experience, and their relationship to decision-making, in SDI. Most studies on emotional perception have focused on analysing possible alterations in the processing of emotional facial expressions in long-term substance abusers [59,61,68,69,111]. However, the results of such studies remain somewhat controversial [68,111]. Some studies have reported that chronic alcohol abusers show significant alterations in the processing of facial expressions. One study showed that alcohol dependent individuals showed specific impairments for recognising facial expressions portraying happiness and anger [68]. These alterations were characterised as overestimation of the intensity of the emotion depicted in these emotional facial expressions. Similar results have been revealed in abstinent subjects with both alcohol and opiate dependence, and in opiate addicts following methadone treatment [69]. By contrast, other studies showed that overestimation of the intensity of emotion in facial expressions reported by alcoholics related mainly to the facial expression of fear. The degree of this overestimation correlated with the number of previous formal detoxifications [111]. Alcoholics also presented with difficulties in distinguishing between the facial expressions of anger and disgust [111]. Other studies have analysed the effects of controlled acute doses of different drugs on the perception of emotions. These studies have shown that acute low doses of alcohol and MDMA can improve the recognition of emotional facial expressions in current users, although recognition accuracy significantly decreased during the following days [59,61]. Detrimental effects of acute drug doses on the recognition of emotions in facial expressions have also been reported using ketamine, an NMDA receptor antagonist [1]. These results indicate that SDI are impaired in the recognition of facial expressions portraying different emotions, including fear, anger, disgust, and happiness. The poorer recognition of facial emotional expressions can affect SDI’s interpretation of social cues, so that they can be less able to manage and regulate emotions, and to make decisions and solve problems of an interpersonal or social nature. In this sense, their poor ability to recognise facial emotional expressions has been attributed to several aspects of their addictive behaviours, such as diminished empathy, increased levels of aggression [59], and a higher frequency of relapse and ensuing alcohol detoxification [111]. In particular, poor recognition of fear expressions, which is thought to depend on the amygdala, can be associated with impaired conditioning of fear responses to drug related environments, increasing the probability of relapses.
Very few studies have examined the emotional experience of SDI. The most frequently used paradigm in the study of the experience of emotions in SDI is the presentation of affective images that induce emotional states, such as the International Affective Picture System (IAPS). The IAPS consists of a large set of images classified according to their normative values in three relevant dimensions: valence (indicating if the emotional response induced is pleasant or unpleasant), arousal (if the emotional response induced is arousing or relaxing), and control (if the emotional response induced can/cannot be controlled by the subject). Gerra et al. [50] used this paradigm to analyse the neuroendocrine response of SDI and healthy participants to experimentally induced pleasant and unpleasant emotions. Their results showed that in response to unpleasant images, SDI showed decreased activity in several neuroendocrine markers, including norepinephrine, cortisol, and adrenocorticotropic hormone levels. Similar results have been obtained in the laboratory using a different response modality, the subjective affective response to IAPS images [3]. SDI showed a more flattened response pattern to both pleasant and unpleasant images. SDI scored as less positive the images considered by normal participants to be very pleasant and arousing. SDI also scored as less negative the images considered by normal participants to be highly unpleasant and arousing. Additionally, SDI showed a consistently higher feeling of control over the emotions elicited by both pleasant and unpleasant emotions, as reflected by higher subjective scores in the control dimension in response to the emotions elicited by both pleasant and unpleasant images. The fact that SDI showed a flattened emotional response to affective images showing both pleasant and aversive scenes may suggest that they also have a diminished emotional response to natural reinforcers other than drugs, where the latter in fact begin to possess exaggerated rewarding effects. This notion is strongly supported by imaging studies on craving in drug addiction, which show that drug related stimuli are able to strongly activate brain regions involved in emotional evaluation and reward processing [48,49,54,63,64, 109,126,128]. In contrast, the same brain regions show blunted activation to other natural reinforcing stimuli such as food or sex [48]. Consistent with this evidence, the somatic-marker model proposes that somatic states associated with natural reinforcers may not be strong enough to bias decisions in SDI, while strong somatic states associated with the prospect of abusing drugs may override decisions towards drug use. This issue will be discussed more in depth in “The Neural Substrates of Substance Craving” and “Conclusion” sections.
Although these are relatively few studies, the evidence thus far underscores the notion that SDI present with a reduced ability to perceive and experience emotions. This reduced ability merits further investigation, since it might be importantly related to the weak processing of somatic signals during decision-making. In other words, this reduced perception and experience of emotions observed in SDI in response to pleasant and unpleasant images may be the underlying cause of their poor decision-making in real life, and their apparent “myopia” for the long-term consequences of their actions.
NEUROIMAGING AND NEUROPHARMACOLOGICAL STUDIES
As mentioned earlier, it has been suggested that the mechanism by which somatic states influence decision-making is via non-specific neurotransmitter systems [6,8,20]. The goal of this section is to review neuroimaging and neuropharmacological findings that provide support for this notion.
Structural and Functional Neural Abnormalities Associated with Substance Addiction
Franklin et al. [46] were the first to use a focal structural analysis of images from the brain scans of crack-cocaine dependent individuals. They used voxel-based-morphometry analyses (VBM) from magnetic resonance imaging (MRI) in a sample of cocaine dependent individuals. They found significant decrements in grey matter concentrations (ranging from 5% to 11%) in a number of neural regions considered critical for the operations of the somatic-marker circuit, including the VMPFC bilaterally, the anterior insular cortex, bilaterally, in addition to changes in some temporal cortices, and also in the right anterior cingulate cortex, which is also a target region in the somatic marker neural circuitry. Interestingly, these reductions in grey matter volume were not significantly correlated with measures of severity of drug dependence. Matochik et al. [81] used VBM analyses to examine grey and white matter composition of the brains of abstinent cocaine dependent individuals. However, these authors focused on the analysis of tissue composition in the frontal lobe, and its main structural subdivisions: dorsolateral, cingulate, and orbitofrontal regions. Their results showed significant grey matter decrements in the lateral prefrontal cortex, cingulate gyrus/ cortex, and medial and lateral aspects of the orbitofrontal cortex, predominantly in the right hemisphere. All these findings reflect changes in areas that are known as critical components of the somatic marker circuitry (Figure 1), and are consistent with the suggestion that the operation of the somatic marker circuitry may be more dependent on right-hemisphere, as opposed to left-hemisphere, processing [29,112]. This study also failed to report significant correlations between indices of severity of drug abuse and reductions in grey matter volume, although the years of cocaine use were associated with lower tissue density in the inferior white matter adjacent to the frontal cortex. In a later study, Makris et al. [77] specifically measured the volume of the amygdala on both sides using segmentation-based morphometric analysis in cocaine dependent individuals. They found decreased absolute volume, primarily in the right amygdala (23% volume reductions, although total volume was also decreased), covering nuclei of the centromedial and basolateral areas and absence of laterality asymmetry in the cocaine group. The reduced volumetric measures of the amygdala were not correlated with measures of drug use severity or co-morbid psychiatric conditions, and these volume reductions were present in all cocaine dependent individuals, including those who used the drug for a short time period (1-2 years of abuse). Although all these studies reveal structural abnormalities in neural structures known to be critical for somatic state activation (or processing emotions), the critical question that remains unanswered, is whether these abnormalities preceded the substance abuse condition, or whether these abnormalities were the consequences of the abuse of these drugs.
Other studies have focused on white matter microstructure [5,71]. White matter abnormalities were consistently found in pathways that connect regions thought to be critical components of the somatic-marker circuit. For instance, Bartzokis et al. [5], in an MRI study compared male cocaine dependent individuals to healthy participants. The results revealed age-related, higher incidence of white matter lesions within the insular cortex of the cocaine group. Using diffusion tensor MRI, Lim et al. [71] analysed the white matter composition of the different subregions of the prefrontal cortex in cocaine dependent individuals. Their results also showed altered white matter microstructure in the inferior frontal regions. These abnormalities seem to reflect disruption of functional connectivity between the orbitofrontal/ ventromedial prefrontal cortex and a number of paralimbic regions involved in the processing of emotional/ somatic states, such as the insular cortex. These results have been recently replicated by Lyoo et al. [74], who found white matter abnormalities in prefrontal and insular regions in cocaine dependent individuals. A recent study using diffusion tensor imaging has also demonstrated that cocaine dependent individuals present with white matter abnormalities in the anterior region of the corpus callosum, and that the severity of these abnormalities correlate with measures of impulsivity [84]. The authors suggested that these anterior corpus callosum abnormalities may be the underlying cause of some alterations in prefrontal cortex functions. It is important to note that deficits in impulse control are often observed in both SDI and neurological patients with lesions in target regions of the somatic-marker circuit, and that these problems in impulse control may contribute to their poor decision-making abilities. Therefore, future studies should investigate further the relationship between structural abnormalities and behavioural domains associated with decision-making in SDI. Once again, an important question to be addressed in future studies is to conduct longitudinal studies to determine whether underlying brain abnormalities in decision-making and impulse control are pre-existing characteristics, or perhaps they are a consequence of drug abuse.
Alterations in neural regions that represent critical components of the somatic-marker circuit have also been shown in functional imaging studies, such as functional abnormalities in the frontal, parietal, and subcortical (including paralimbic) regions of the brains of SDI [27,88, 115]. A number of studies using Positron Emission Tomography (PET) and Single Photon Emission Computerised Tomography (SPECT) have revealed VMPFC functional abnormalities in alcohol, cocaine, and methamphetamine abusers [reviewed in 52,117,118]. Other studies have observed functional abnormalities in other regions known to be critical for emotional/ somatic states processing, such as the insular/ somatosensory cortices, and the striatum. Furthermore, metabolic abnormalities in the anterior cingulate cortex have been associated with abnormal measures on tests of executive functions in SDI [51].
Chang et al. [27], using functional MRI, analysed the regional cerebral blood flow of long-term abstinent methamphetamine dependent individuals. Their results showed decreased regional CBF in the insular cortices and inferior frontal regions, bilaterally, and in the right lateral parietal region. Nonetheless, methamphetamine dependent individuals showed increased regional CBF in the occipital, and right dorsal/ posterior parietal regions. This pattern of alterations in functional activity was attenuated in the female methamphetamine abusers, relative to male drug abusers. The authors interpreted this finding as reflecting a neuroprotective effect of estrogens, in females, on the potential neurotoxic action of methamphetamine. Volkow et al. [115] also demonstrated higher cortical (mainly parietal), and lower subcortical (thalamus and striatum) metabolism in abstinent methamphetamine abusers, although no significant gender differences were reported in this sample of drug abusers. Thus, the issue of gender and vulnerability to drug abuse remains unsettled, and the question should be addressed in future research.
In a large sample of ecstasy abusers, functional abnormalities were found, bilaterally, in the cingulate cortices, amygdala, striatum, and hippocampus [88]. Although no significant relationships were observed between severity of ecstasy use and brain regional functional activity, earlier exposure to ecstasy was associated with decreased functional activity in the amygdala and striatum. However, one must take caution in interpreting the effects of ecstasy on cognition, since the drug is almost always co-abused with marijuana, thus rendering it difficult to determine whether the deficits are linked to ecstasy or marijuana use.
Overall, findings from both structural and functional imaging studies consistently indicate that several key neural substrates in the circuitry of somatic state activation and decision-making are affected in SDI. Decreased grey matter volumes have been detected in regions involved in the triggering of somatic markers, i.e., the amygdala and VMPFC, and in the covert and overt processing of emotional (somatic) signals in the brain, i.e., the striatum, and insular/anterior cingulate cortices [46,77,81]. Additionally, studies of brain white matter of individuals addicted to substances showed abnormalities in white matter pathways that connect the VMPFC to several other limbic structures involved in core aspects of somatic state activation and decision-making [5,71,73].
One interesting and consistent finding among all these studies was the asymmetry of these abnormalities in terms of their presence in the right, as opposed to the left hemisphere [46,77,81]. Such a finding is congruent with the suggested predominant role of the right hemisphere in somatic state activation and decision-making [29,112]. Finally, it is also striking that almost none of these studies found significant correlations between abnormalities in some morphological and structural indices of the brain, and various measures of the severity of drug abuse, including age of onset, frequency of drug use, peak use, or amount of money spent in illegal drugs [46,77,81]. This lack of correlations may suggest that these brain abnormalities, to some extent, precede the onset of drug use, thus predisposing the individual to drug addiction [118]. Nonetheless, this is a very controversial issue, since some studies have been able to correlate brain imaging and drug use measures [88]. More research is needed to settle the issue about the relationship between drug use patterns and alterations in certain brain structures and functions.
Neuropharmacological Changes Associated with Substance Addiction
Several studies have demonstrated that pharmacological manipulations of the dopamine, serotonin, and noradrenaline systems can significantly affect different aspects of emotional experience [86] and decision-making [9,98] in healthy participants, as measured in various experimental settings.
In humans, there is a compelling evidence for a major role of dopamine (DA) in the increased sensitisation of the incentive motivational properties of drugs of abuse [118]. This increased sensitisation to the reinforcing effects of drugs tends to facilitate the continuous administration of drugs of abuse, even when they lose their pleasurable hedonic effects (i.e., wanting vs. liking) [17,96,97], thus contributing to the reinstatement of drug consumption after protracted abstinence [47,57,73,126]. Recent theoretical accounts [41,42,60] have proposed that during the sensitised state, there is an enhanced DA mediated response to the incentive motivational value of drugs in the striatum and the amygdala. This enhanced response coincides with a weakened activity within the prefrontal cortex, which reflects a weakened inhibitory control of the prefrontal cortex to the hyperactive amygdala-striatum system [41,42]. This weakens the capacity of the individual to self-regulate the drug seeking behaviour, thus leading to a persistent and compulsive use of drugs, irrespective of the long-term negative consequences.
In support of this view, a number of studies using PET have shown persistent reductions of dopamine D2 receptors at the level of the striatum in SDI, including alcohol, heroin, cocaine and methamphetamine dependent individuals [116, 119,122,125]. Interestingly, related studies have demonstrated an association between striatal dopamine D2 postsynaptic receptor densities and the metabolic activity of the orbitofrontal cortex in cocaine and methamphetamine addicts [116,125]. This association is proposed to reflect a higher sensitivity of the orbitofrontal cortex to dopamine modulation stemming from limbic structures involved in emotional signalling and reward processing. Also, it may reflect the mechanism by which altered somatic signals may bias decision-making in SDI towards immediate reward. The reductions of dopamine D2 receptor densities tend to recover in certain brain regions, such as the thalamus, but the reductions seem to be long lasting at the level of the striatum [125]. This suggests a possible dissociation between the recoverable locomotor sensitisation effects of abused drugs, and their longer lasting and sensitised motivational/emotional effects.
Abnormal DA functions in several neural regions known to be components of the somatic-marker circuit have been reported in studies showing decreased DA transporter density in the striatum (including nucleus accumbens) and prefrontal cortex of cocaine and methamphetamine dependent individuals [104,122]. Other studies revealed reduced occupancy of striatal DA receptors in response to the addition of competitive radioligands (e.g., [11C]raclopride) and mimetic drugs like methylphenidate [102,120,121,124]. These findings suggest that there are significant reductions in DA release in several neural structures, considered as key components of the somatic-marker neural circuitry, in SDI [118]. This reduced DA activity may explain the blunted response of SDI to a variety of natural reinforcers, beside drugs, which has been reported in several neuroimaging [48,79] as well as subjective self-report studies [3]. This reduced DA activity may also explain the sensitised response of addicted individuals to the reinforcing effects of drugs of abuse, since they are probably the only powerful stimuli that are capable of inducing reward [57].
The serotonin (5HT) system has also been implicated in mediating the biasing effects of somatic-markers on cognition [86], including decision-making [9,99]. Nonetheless, studies of the role of 5HT in addiction have been far less extensive in comparison to DA. Some studies have proposed that low 5HT activity contributes significantly to the dysphoric, or anhedonic state associated with abstinence from drugs of abuse [66]. Other studies showed that low 5-HT activity is associated with decreased prefrontal activity, which is necessary for exerting inhibitory or impulse control over behaviour [95]. Thus, low 5-HT and prefrontal activity observed in SDI may explain not only their compulsive drug use, but also several other co-morbid conditions, such as their depressed mood, and antisocial behaviour [100,103].
The Neural Correlates of Substance Craving
People still disagree on how craving should be defined [45,97,110]. Here craving will be defined as the accompanied emotional state that is produced by emotionally competent stimuli that are associated with the reinforcing effects of drugs of abuse [6,45]. To study craving in the laboratory, a number of studies have used different strategies to induce craving. These strategies include the visual presentation of the drug, or drug related paraphernalia, through images (pictures), or videos; the auditory presentation of audio-taped scripts containing autobiographical experiences related to drug use; or the direct infusion of the drug itself. The aim of this section is to review the evidence showing an overlap between the neural structures that represent critical components of the somatic-marker neural circuitry, and neural structures activated during states of craving in substance abusers. The somatic-marker model proposes that there should be a robust response within these neural structures in response to drug cues, but a diminished response of the neural circuitry to non-drug, natural reinforcers.
Grant et al. [54] used PET to study craving in recently abstinent cocaine abusers. In the scanner, participants were shown videos of drug related paraphernalia, and cocaine self-administration. A pattern of significantly increased activation associated with craving was detected primarily in frontal (VMPFC and dorsolateral –DLPFC-), parietal, temporal, and striatal regions. The correlation analyses showed that the subjective response of craving was associated with changes in the activation of the amygdala in cocaine abusers. A follow up study by the same group [23] used auditory presentation of drug cues, i.e., a script describing sensations associated with being “high” on cocaine. The results revealed increased activation in the DLPFC, orbitofrontal cortex, amygdala and adjacent rhinal cortices. The correlation analyses showed that the subjective response of craving correlated with the degree of activity within these neural regions.
Numerous subsequent PET studies in cocaine abusers have also revealed a significant overlap between the neural regions activated during craving and those considered as components of the somatic marker neural circuitry. Wang et al. [126] detected higher metabolism in the orbitofrontal and insular cortices of abstinent cocaine abusers after an interview in which participants were allowed to manipulate drug paraphernalia. Furthermore, activation of the left insular cortex was significantly correlated with self-reported craving. Similarly, Childress et al. [28] found amygdalar and anterior cingulate activation in cocaine abusers exposed to a drug-related video.
In two subsequent PET studies [63,64], Kilts et al. examined the craving response of cocaine dependent men and women to auditory scripts describing events from their own previous drug experience. These studies reveal that there are important gender differences in regional patterns of brain activation in relation to drug cue induced craving. However, irrespective of these differences, the general neural circuitry engaged during craving, in both males and females, tends to reveal activation within neural regions that are considered critical components of the neural circuitry underlying somatic state activation and decision-making.
Using a different neuroimaging technique (functional magnetic resonance imaging, fMRI), Garavan et al. [48] contrasted the responses of crack-cocaine dependent individuals to films containing natural outdoors, sexual explicit, and drug use related scenes. The drug-associated film induced increased activation of an extensive neural circuitry that included the prefrontal and parietal regions, temporal, insular, anterior and posterior cingulate cortices, and the striatum. A similar pattern of activation was observed in healthy participants when exposed to the film containing explicit sexual scenes (an emotionally competent natural reinforcing stimulus), which contrasted with the fainter activation of these regions in the cocaine abusers. These findings suggest that cocaine dependent individuals present with a reduced sensitivity to the rewarding properties of natural reinforcers, while at the same time, they present with an increased sensitivity to drug related stimuli. Thus, they strongly support the proposal of the somatic-marker model that SDI have a robust response, within their somatic-marker circuitry, to drug related stimuli, but a diminished response to non-drug stimuli, i.e., natural reinforcers. This abnormal capacity to process the emotional value of a stimulus has a significant impact on decision-making, in that it can shift the decision-making process towards short-term horizons, i.e., the seeking of drugs. In support, several fMRI studies have shown an exaggerated brain response to drug cues [49,75,109,126,128,131].
The brain activation studies on craving were not restricted to individuals who abused stimulant drugs, but similar findings were obtained from individuals addicted to opioids [32,33]. A relevant finding from these studies was the correlation between length of abstinence and anterior cingulate activation, i.e., longer abstinence duration predicted larger cerebral blood flow changes in the anterior cingulate. This finding seems to suggest that the affective evaluation of drug related stimuli do not decrease. Rather it increases after prolonged abstinence, thus suggesting a persistent sensitisation effect.
To mimic the acute dopamine response induced by cocaine, Volkow et al. [120] injected two sequential doses of the drug methylphenidate to a sample of cocaine dependent individuals. The correlation analyses showed that changes in the subjective report of craving were significantly correlated with changes in the right striatum and orbitofrontal cortex. Activation of the right orbitofrontal cortex was specifically associated with intense feelings of craving. A recent study [2] obtained similar results using a procaine challenge in a sample of cocaine dependent patients. With regard to healthy participants, cocaine patients showed increased response to procaine injection in the right orbitofrontal, midfrontal, midtemporal, and parietal cortices, and in the brainstem. Saline administration was associated with deactivation of the orbitofrontal region in the cocaine patients. There was also a trend of a significant relationship between duration of cocaine abuse and right orbitofrontal cortex change rate in response to craving.
Another set of studies has directly employed the administration of the abuser’s drug of choice to evoke craving states. Breiter et al. [24] administered repeated cocaine infusions to examine the “rush” and “craving” patterns of brain activation using fMRI in cocaine dependent patients. Their results showed a wide array of regional activations on regions involved in the ongoing evaluation of the emotional significance of emotionally competent stimuli [62], and the modification of behaviour through somatic signals [47].
In another study [105], a combination of heroin injection and visual presentation of films containing drug related scenes was used to induce craving in a sample of heroin dependent individuals undergoing methadone treatment. The correlation analyses showed that the subjective response of “urge to use heroin” (equivalent to subjective craving measures) was significantly associated with increased activation in the inferior frontal, right orbitofrontal, and insular cortices of heroin dependent patients. The insula activation was significantly correlated with physiological measures of pulse rate, outlining its role in autonomic regulation. Significant activations were also observed in the brainstem in response to both the heroin injection and the drug-related film.
Together, these studies reveal a great overlap between the neural structures known to be critical components of the somatic-marker neural circuit, and the neural systems engaged in emotional states such as craving in substance abusers [2,23,24,28,32,33,49,54,63,64,75,105,109,126,128, 131]. Activities within the orbitofrontal cortex and amygdala, two key areas for triggering somatic states, were shown to correlate with subjective self-reports of craving across several different studies [2,23,24,32,33,54,109,120]. Areas involved in body mapping and emotional representation, such as the insula and anterior cingulate, were also engaged during the experience of craving [24,33,126].
Most of the regions activated during the experience of craving induced by drug cues in SDI were also engaged in healthy participants when they were exposed to natural reinforcers, such as sex cues [48]. This suggests that the neural substrates that mediate craving in drug addicts have actually evolved to subserve natural emotional functions, such as those related to food and sex. Nonetheless, it is important to note that drug addicts present with some degree of dissociation between the emotional responses to drug versus non-drug related stimuli. In other words, drug addicts tend to trigger strong emotional responses (or somatic states) in response to drug related cues, but they trigger relatively weak somatic states in response to non-drug related, natural reinforcers.
The Neural Correlates of Abnormal Decision-Making in Substance Dependent Individuals
The neural circuitry that is critical for processing emotions (or somatic state activation) overlaps considerably with that subserving decision-making, as measured by complex laboratory decision-making tasks, such as the IGT. In other words, performance on this task is impaired by damage to various key structures that make up somatic-marker circuitry. Alternatively, performance of this task activates neural components of the somatic marker circuitry in functional neuroimaging studies. In a PET activation study, which examined patterns of brain activation during IGT performance in healthy participants [38], the authors observed that decision-making was associated with increased activation in the VMPFC, anterior cingulate, parietal/insular cortices and the amygdala, predominantly on the right side. Other regions that were also activated during the performance of decision-making tasks included the dorsolateral prefrontal cortex, thalamus and cerebellum. Later imaging studies have confirmed and extended these findings, and implicated additional neural regions, e.g., the striatum [114], and the nucleus accumbens [80], in processes that are critical for decision-making. Recent studies have also reported important gender differences in brain activations induced by complex decision-making tasks, such as the IGT [22].
In SDI, Bolla et al. [21] used oxygen labelled PET to examine brain activation in 25-day abstinent cocaine dependent patients while performing the Iowa Gambling Task (IGT). Group analyses showed increased activation during gambling task performance in the right orbitofrontal cortex, and less activation in the left dorsolateral cortex of cocaine patients, with regard to healthy subjects. Activation of the orbitofrontal cortex was directly correlated with better performance of both groups, and negatively correlated with amount of cocaine used in the patient group. In another study, Ersche et al. [40] tested current opiate and amphetamine users and ex-users in the Cambridge Gamble task [30], which was designed to isolate the evaluation of risky decision-making from the planning and working memory components inherent in the IGT. SDI and matched healthy comparison participants were subjected to oxygen labelled PET while performing this decision-making task. Results revealed that drug abusers performing the risk task showed increased activation of the left orbitofrontal cortex and decreased activation of the right dorsolateral cortex (identical localisation but reversed lateralisation with respect to the results of the Bolla et al. study). With regard to ex-users, current drug users showed decreased activation in the striatum, although this effect did not survive multiple comparison correction analyses. No significant differences were found between the current users consuming pharmacologically different components (amphetamine vs. opiates).
Two other studies have examined patterns of brain regional activation in abstinent methamphetamine abusers using a two-choice prediction task [90,91]. This task also taps into decision-making function under conditions of uncertainty, by requiring the prediction of an uncertain outcome, which can be predicted correctly (success) or incorrectly (failure). However, unlike the IGT or Cambridge Gamble tasks, this task does not involve incentive evaluation of rewards and punishments. Overall, the behavioural results of these studies demonstrated a more rigid stimulus driven decision-making pattern in the methamphetamine group, as opposed to a more outcome driven pattern in the healthy participants. Imaging patterns in methamphetamine individuals while performing the two-choice prediction task showed decreased activation of the orbitofrontal, dorsolateral, insular and inferior parietal cortices; orbitofrontal activation was inversely correlated with duration of methamphetamine use [90]. This decreased activation was particularly observed in low error-rate phases of the task (i.e., when the subjects successfully predicted the correct outcomes).
CONCLUSION
The somatic-marker model of addiction proposes that the process of decision-making depends in many important ways on neural substrates that regulate homeostasis, emotion, and feeling. The evidence reviewed in this article shows that numerous studies in SDI point to abnormalities in key neural components of the neural circuitry necessary for somatic state activation and decision-making. According to this model, addiction is viewed as a condition in which the person becomes unable to choose according to long-term outcomes. Choosing according to long-term outcomes rather than short-term ones requires that the pain signals triggered by thoughts about the future negative consequences of seeking drugs dominate those triggered by the immediate rewarding consequences of consuming the drug. Based on the somatic marker model, it was suggested that two broad types of conditions could alter this relationship and lead to defective decision-making, and the poor ability to resist the temptation of drug use. (1) One condition may involve a dysfunction in the VMPFC system, which is critical for processing emotional (somatic) states from secondary inducers. This is a sort of a “reflective” system, which loses its ability to process and trigger somatic signals associated with future prospects, such as the negative consequences associated with drug use. (2) Another condition may involve hyperactivity in the amygdala system, which is critical for processing emotional (somatic) states from primary inducers. This is a sort of an “impulsive” system, whose activity becomes altered in such a way that it diminishes the emotional/ somatic impact of natural reinforcers, but it exaggerates the emotional/ somatic impact of the immediate prospects of obtaining drugs. Thus, drug cues acquire properties for triggering bottom-up, automatic, and involuntary somatic states through the amygdala. Once they do, this bottom-up somatic bias can modulate top-down cognitive mechanisms, in which the ventromedial prefrontal cortex is a critical substrate. If strong enough, this bottom-up influence can interfere or “hijack” the top-down cognitive mechanisms necessary for triggering somatic states about future outcomes. In other words, drugs acquire properties of triggering bottom-up, involuntary signals through the amygdala that modulate and bias top-down goal-driven attentional resources needed for the normal operation of the reflective system, which is critical for exerting control enabling an individual to resist the temptation to seek the drug.
There is evidence to suggest that somatic-markers may exert their biasing influence on decisions through the release of specific neurotransmitters [9,86,98,99]. Advances in the ability to prevent relapse and break the cycle of addiction may be made from pharmacological research aimed at understanding the modulatory influence of different neurotransmitter systems, such as DA, 5HT and NA, in the reflective/prefrontal system of SDI, which underlies their decision-making impairment and loss of control over their drug abuse behaviour. Although some evidence suggests that pharmacological interventions influence decision-making, it is argued that pharmacological treatments alone, i.e., without cognitive and behavioural rehabilitation, may not be the most effective strategy for treating addiction. The idea is that poor prefrontal mechanisms of decision-making in SDI are in part related to learning in the presence of a deficiency in the neurotransmitters that modulate, unconsciously or consciously, the cognitive and emotional resources involved in decision-making. In other words, poor decision-making and poor learning to control certain behaviours are due in part to this deficiency. Reversal of this chemical deficiency alone is not sufficient for improving decision-making. The individual must re-learn how to think and behave in a particular situation related to drugs while being treated with medications, which correct the deficiency in the neurotransmitter substrates of decision-making. Thus, only relearning (i.e., rehabilitation) in the presence of normal pharmacology (i.e., drug treatment) is perhaps the most effective way to restore advantageous decisions in an addicted individual. The somatic-marker model of addiction has some implications for the clinical treatment of addiction. Since the model focuses on the existence of abnormal emotional regulation, intervention strategies aimed at improving emotional processing may be especially useful in the potential management or treatment of addiction.
This review provides extensive evidence for the pertinence of applying the somatic-marker hypothesis to addiction, and generates a somatic-marker model of addiction that provides a number of testable predictions for future research. The main contribution of this model, with regard to previous models of addiction, is that it provides a systems-level neuroanatomical and cognitive framework for explaining the decision-making deficits of SDI, and their inability for choosing according to long-term outcomes rather than short-term ones. The model highlights the role of abnormal emotion processing in the decision-making deficits of SDI. Despite these contributions, several specifications and limitations of the model should be mentioned. First, the somatic-marker hypothesis is an evolving theoretical framework still being empirically evaluated. For example, there are a number of compatible and alternative explanations for the abnormal performance of SDI and patients with VMPFC lesions in the IGT, including working memory or reversal learning deficits [43,58,101]. Additionally, some studies have challenged the notion that body-state feedback causally influences decision-making [56]. Furthermore, more research is needed to investigate if the extent of emotional blunting correlates with the extent of decision-making impairments in SDI. Second, the somatic-marker model of addiction is not incompatible with previous theoretical models of addiction, including animal models of emotional response to drug cues [89], brain-based DA reinforcement models [94], and the incentive sensitisation theory [96,97] [see 70 for review of these models]. In particular, the somatic-marker model is compatible with the incentive sensitisation theory, in the sense that both models predict a strong salience attribution for drug related stimuli. However, the somatic-marker model proposes that this salience attribution is modulated by the development of strong somatic-markers of emotive nature, which are able to bias decision-making towards drug abuse. An additional difference is that the somatic-marker model predicts blunted emotional processing of other relevant natural reinforcers not related to drugs. Third, the somatic-marker model is not specific to addiction. The model provides an account of how emotional states help guide decision-making towards long-term adaptive goals. Impaired decision-making and emotional dysregulation are core characteristics of substance dependence, but they are also prominent characteristics of a variety of disorders, such as pathological gambling, OCD or APD. Interestingly, these disorders are often concurrent with substance dependence, suggesting possible common underlying mechanisms. Further research is necessary to address how pre-existing genetic factors, and/or environmental influences, lead to neural functional abnormalities that may account for the development of these different disorders.
ACKNOWLEDGMENT
Authors of this review have been supported by grants INT/2012/2002 from the Spanish “Ministerio del Interior”, and BSO2003-07169 from the Spanish “Ministerio de Ciencia y Tecnologìa” (Principal Investigator is Miguel Pérez Garcìa), and by grants from the National Institute on Drug Abuse (NIDA): DA11779, DA12487, and DA16708 (Principal Investigator is Antoine Bechara).
REFERENCES
- 1.Abel KM, Allin MPG, Kuchrska-Pietura K, David A, Andrew C, Williams S, Brammer MJ, Phillips ML. Ketamine alters neural processing of facial emotion recognition in healthy men: and fMRI study. Cogn Neurosci Neuropsychol. 2003;14:387–391. doi: 10.1097/00001756-200303030-00018. [DOI] [PubMed] [Google Scholar]
- 2.Adinoff B, Devous MD, Best SM, George MS, Alexander D, Payne K. Limbic responsiveness to procaine in cocaine-addicted subjects. Am J Psychiatry. 2001;158:390–398. doi: 10.1176/appi.ajp.158.3.390. [DOI] [PubMed] [Google Scholar]
- 3.Aguilar F, Verdejo A, Peralta MI, Sánchez-Barrera M, Pérez-García M. Experience of emotions in substance abusers exposed to images containing neutral, positive, and negative affective stimuli. Drug Alcohol Depend. 2004;78:159–167. doi: 10.1016/j.drugalcdep.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 4.Barnfield TV, Leathern JM. Incidence and outcomes of traumatic brain injury and substance abuse in a New Zealand prison population. Brain Inj. 1998;12:455–466. doi: 10.1080/026990598122421. [DOI] [PubMed] [Google Scholar]
- 5.Bartzokis G, Goldstein IB, Hance DB, Beckson M, Shapiro D, Lu PH, Edwards N, Mintz J, Bridge P. The incidence of T2-Weighted MR imaging signal abnormalities in the brain of cocaine-dependent patients is age-related and region-specific. Am J Neuroradiol. 1999;20:1628–1635. [PMC free article] [PubMed] [Google Scholar]
- 6.Bechara A. Risky business: emotion, decision-making and addiction. J Gambl Stud. 2003;19:23–51. doi: 10.1023/a:1021223113233. [DOI] [PubMed] [Google Scholar]
- 7.Bechara A. The role of emotion in decision-making: Evidence from neurological patients with orbitofrontal damage. Brain Cogn. 2004;55:30–40. doi: 10.1016/j.bandc.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Bechara A, Damasio AR. The somatic marker hypothesis: a neural theory of economic decision. Games Econ Behav. 2004;52:336–372. [Google Scholar]
- 9.Bechara A, Damasio AR, Damasio H. Manipulation of dopamine and serotonin cause different effects on covert and overt decision-making. Abstr Soc Neurosci. 2001;27 [Google Scholar]
- 10.Bechara A, Damasio AR, Damasio H, Anderson SW. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition. 1994;50:7–15. doi: 10.1016/0010-0277(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 11.Bechara A, Damasio H. Decision-making and addiction (part I): impaired activation of somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychologia. 2002;40:1675–1689. doi: 10.1016/s0028-3932(02)00015-5. [DOI] [PubMed] [Google Scholar]
- 12.Bechara A, Damasio H, Damasio AR. Emotion, decision-making and the orbitofrontal cortex. Cereb Cortex. 2000;10:295–307. doi: 10.1093/cercor/10.3.295. [DOI] [PubMed] [Google Scholar]
- 13.Bechara A, Damasio H, Damasio AR. Shinnick-Gallagher P, Pitkanen A, Shekhar A, Cahill L, editors. The role of the amygdala in decision-making. The Amygdala in Brain Function: Basic and Clinical Approaches. 2003:356–369. Ann. N.Y. Acad. Sci. [Google Scholar]
- 14.Bechara A, Damasio H, Tranel D, Damasio AR. Deciding advantageously before knowing the advantageous strategy. Science. 1997;275:1293–1295. doi: 10.1126/science.275.5304.1293. [DOI] [PubMed] [Google Scholar]
- 15.Bechara A, Dolan S, Denburg N, Hindes A, Anderson SW, Nathan PE. Decision-making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in alcohol and stimulant abusers. Neuropsychologia. 2001;39:376–389. doi: 10.1016/s0028-3932(00)00136-6. [DOI] [PubMed] [Google Scholar]
- 16.Bechara A, Dolan S, Hindes A. Decision-making and addiction (part II): myopia for the future or hypersensitivity to reward? Neuropsychologia. 2002;40:1690–1705. doi: 10.1016/s0028-3932(02)00016-7. [DOI] [PubMed] [Google Scholar]
- 17.Berridge KC, Robinson TE. The mind of an addicted brain: neural sensitization of wanting versus liking. Curr Dir Psychol Sci. 1995;4:71–76. [Google Scholar]
- 18.Berridge KC, Robinson TE. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Rev. 1998;24:309–369. doi: 10.1016/s0165-0173(98)00019-8. [DOI] [PubMed] [Google Scholar]
- 19.Blair J, Utah F. Neurocognitive explanations of the antisocial personality disorders. Crim Behav Ment Health. 2000;10:66–81. [Google Scholar]
- 20.Blessing WW. The Lower Brainstem and Bodily Homeostasis. New York: Oxford University Press; 1997. Anatomy of the lower brainstem. In; pp. 29–99. [Google Scholar]
- 21.Bolla KI, Eldreth DA, London ED, Kiehl KA, Mouratidis M, Contoreggi C, Matochik JA, Kurian JL, Cadet JL, Kimes AS, Funderburk FR, Ernst M. Orbitofrontal cortex dysfunction in abstinent cocaine abusers performing a decision-making task. Neuroimage. 2003;19:1085–1094. doi: 10.1016/s1053-8119(03)00113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bolla KI, Eldreth DA, Matochik JA, Cadet JL. Sex-related differences in a gambling task and its neurological correlates. Cereb Cortex. 2004;14:1226–1232. doi: 10.1093/cercor/bhh083. [DOI] [PubMed] [Google Scholar]
- 23.Bonson KR, Grant SJ, Contoreggi CS, Links JM, Metcalfe J, Weyl J, Kurian V, Ernst M, London E. Neural systems and cue-induced cocaine craving. Neuropsychopharmacology. 2002;26:376–386. doi: 10.1016/S0893-133X(01)00371-2. [DOI] [PubMed] [Google Scholar]
- 24.Breiter HC, Gollub RL, Weisskoff RM, Kennedy DN, Makris N, Berke JD, Goodman JM, Kantor HL, Gastfriend DR, Riorden JP, Mathew RT, Rosen BR, Hyman SE. Acute effects of cocaine on human brain activity and emotion. Neuron. 1997;19:591–611. doi: 10.1016/s0896-6273(00)80374-8. [DOI] [PubMed] [Google Scholar]
- 25.Busemeyer JR, Stout JC. A contribution of cognitive decision models to clinical assessment: Decomposing performance on the Bechara gambling task. Psychol Assess. 2002;14:253–262. doi: 10.1037//1040-3590.14.3.253. [DOI] [PubMed] [Google Scholar]
- 26.Cador M, Robbins TW, Everitt BJ. Involvement of the amygdala in stimulus-reward associations: interaction with the ventral striatum. Neuroscience. 1989;30:77–86. doi: 10.1016/0306-4522(89)90354-0. [DOI] [PubMed] [Google Scholar]
- 27.Chang L, Ernst T, Speck O, Patel H, DeSilva M, Leonido-Yee M, Miller EN. Perfusion MRI and computerized cognitive test abnormalities in abstinent methamphetamine users. Psychiatry Res. 2002;114:65–79. doi: 10.1016/s0925-4927(02)00004-5. [DOI] [PubMed] [Google Scholar]
- 28.Childress AR, Mozley PD, McElgin W, Fitzgerald J, Reivich M, O´Brien CP. Limbic activation during cue-induced cocaine craving. Am J Psychiatry. 1999;156:11–18. doi: 10.1176/ajp.156.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clark L, Manes F, Antoun N, Sahakian BJ, Robbins TW. The contributions of lesion laterality and lesion volume to decision-making impairment following frontal lobe damage. Neuropsychologia. 2003;41:1474–1483. doi: 10.1016/s0028-3932(03)00081-2. [DOI] [PubMed] [Google Scholar]
- 30.Clark L, Robbins TW. Decision-making deficits in drug addiction. Trends Cogn Sci. 2002;6:361–363. doi: 10.1016/s1364-6613(02)01960-5. [DOI] [PubMed] [Google Scholar]
- 31.Crone EA, Somsen RJM, Van Beek B, Van der Molen MW. Heart rate and skin conductance analysis of antecedents and consequences of decision making. Psychophysiology. 2004;41:531–540. doi: 10.1111/j.1469-8986.2004.00197.x. [DOI] [PubMed] [Google Scholar]
- 32.Daglish MRC, Weinstein A, Malizia AL, Wilson S, Melichar JK, Britten S, Brewer C. Changes in cerebral blood flow elicited by craving memories in abstinent opiate-dependent subjects. Am J Psychiatry. 2001;158:1680–1686. doi: 10.1176/appi.ajp.158.10.1680. [DOI] [PubMed] [Google Scholar]
- 33.Daglish MRC, Weinstein A, Malizia AL, Wilson S, Melichar JK, Lingford-Hughes A, Myles JS, Grasby P, Nutt D. Functional connectivity analysis of the neural circuits of opiate craving: “more” rather than “different”? Neuroimage. 2003;20:1964–1970. doi: 10.1016/j.neuroimage.2003.07.025. [DOI] [PubMed] [Google Scholar]
- 34.Damasio AR. Descartes´ error: Emotion, Reason, and the Human Brain. New York: Grosset/Putnam; 1994. [Google Scholar]
- 35.Damasio AR. Toward a neurobiology of emotion and feeling: operational concepts and hypotheses. Neuroscience. 1995;1:19–25. [Google Scholar]
- 36.Damasio AR. The Feeling of What Happens: Body and Emotion in the Making of Consciousness. New York: Harcourt Brace & Co.; 1999. [Google Scholar]
- 37.Delmonico RL, Hanley-Peterson P, Englander J. Group psycho-therapy for persons with traumatic brain injury: management of frustration and substance abuse. J Head Trauma Rehabil. 1998;13:10–22. doi: 10.1097/00001199-199812000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Ernst M, Bolla K, Mouratidis M, Contoreggi C, Matochik JA, Kurian V, Cadet J, Kimes AS, London ED. Decision-making in a risk-taking task: A PET study. Neuropsychopharmacology. 2002;26:682–691. doi: 10.1016/S0893-133X(01)00414-6. [DOI] [PubMed] [Google Scholar]
- 39.Ernst M, Grant SJ, London ED, Contoreggi CS, Kimes AS, Spurgeon L. Decision-making in adolescents with behavior disorders and adults with substance abuse. Am J Psychiatry. 2003;160:33–40. doi: 10.1176/appi.ajp.160.1.33. [DOI] [PubMed] [Google Scholar]
- 40.Ersche KD, Fletcher PC, Lewis SJG, Clark L, Stocks-Gee G, London M, Deakin JB, Robbins TW, Sahakian BJ. Abnormal frontal activations related to decision-making in current and former amphetamine- and opiate-dependent individuals. Psychopharmacology. 2005;180:612–623. doi: 10.1007/s00213-005-2205-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Everitt BJ, Parkinson JA, Olmstead MC, Arroyo M, Robledo P, Robbins TW. Associative processes in addiction and reward: the role of amygdala and ventral striatal subsystems. Ann NY Acad Sci. 1999;877:412–438. doi: 10.1111/j.1749-6632.1999.tb09280.x. Advancing from the Ventral Striatum to the Extended Amygdala. [DOI] [PubMed] [Google Scholar]
- 42.Everitt BJ, Wolf ME. Psychomotor stimulant addiction: a neural systems perspective. J Neurosci. 2002;22:3312–3320. doi: 10.1523/JNEUROSCI.22-09-03312.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fellows LK, Farah MJ. Different underlying impairments in decision-making following ventromedial and dorsolateral frontal lobe damage in humans. Cereb Cortex. 2005;15:58–63. doi: 10.1093/cercor/bhh108. [DOI] [PubMed] [Google Scholar]
- 44.Fishbein D, Hyde C, Eldreth D, London ED, Matochik J, Ernst M, Isenberg N, Steckley S, Schech B, Kimes A. Cognitive performance and autonomic reactivity in abstinent drug abusers and nonusers. Exp Clin Psychopharmacol. 2005;13:25–40. doi: 10.1037/1064-1297.13.1.25. [DOI] [PubMed] [Google Scholar]
- 45.Franken IHA. Drug craving and addiction: integrating psychological and neuropharmacological approaches. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27:563–579. doi: 10.1016/S0278-5846(03)00081-2. [DOI] [PubMed] [Google Scholar]
- 46.Franklin TR, Acton PD, Maldjian JA, Gray JD, Croft JR, Dackis CA, O´Brien CP, Childress AR. Decreased gray matter concentration in the insular, orbitofrontal, cingulate, and temporal cortices of cocaine patients. Biol Psychiatry. 2002;51:134–142. doi: 10.1016/s0006-3223(01)01269-0. [DOI] [PubMed] [Google Scholar]
- 47.Fresnois F, Stinus L, DiBlasi F, Cador M, LeMoine C. A specific limbic circuit underlies opiate withdrawal memories. J Neurosci. 2005;25:1366–1374. doi: 10.1523/JNEUROSCI.3090-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Garavan H, Pankiewicz J, Bloom A, Cho JK, Sperry L, Ross TJ. Cue-induced cocaine craving: Neuroanatomical specificity for drug users and drug stimuli. Am J Psychiatry. 2000;157:1789–1798. doi: 10.1176/appi.ajp.157.11.1789. [DOI] [PubMed] [Google Scholar]
- 49.George MS, Anton RF, Bloomer C, Teneback C, Drobes DJ, Lorberbaum JP, Nahas Z, Vincent DJ. Activation of prefrontal cortex and anterior thalamus in alcoholic subjects on exposure to alcohol-specific cues. Arch Gen Psychiatry. 2001;58:345–352. doi: 10.1001/archpsyc.58.4.345. [DOI] [PubMed] [Google Scholar]
- 50.Gerra G, Baldaro B, Zaimovic A, Moi G, Bussandri M, Raggi MA, Bambrilla F. Neuroendocrine responses to experimentally-induced emotions among abstinent opioid-dependent subjects. Drug Alcohol Depend. 2003;71:25–35. doi: 10.1016/s0376-8716(03)00065-6. [DOI] [PubMed] [Google Scholar]
- 51.Goldstein RZ, Leskovjan AC, Hoff AL, Hitzemann R, Bashan F, Khalsa S, Wang GJ, Fowler J, Volkow ND. Severity of neuropsychological impairment in cocaine and alcohol addiction: association with metabolism in the prefrontal cortex. Neuropsychologia. 2004;42:1447–1458. doi: 10.1016/j.neuropsychologia.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 52.Goldstein RZ, Volkow ND. Drug addiction and its underlying neurobiological basis: Neuroimaging evidence for the involvement of the frontal cortex. Am J Psychiatry. 2002;159:1642–1652. doi: 10.1176/appi.ajp.159.10.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grant S, Contoreggi C, London ED. Drug abusers show impaired performance in a laboratory test of decision-making. Neuropsychologia. 2000;38:1180–1187. doi: 10.1016/s0028-3932(99)00158-x. [DOI] [PubMed] [Google Scholar]
- 54.Grant S, London E, Newlin DB, Villemagne VL, Liu X, Contoreggi C, Phillips RI, Kimes AS, Margolin A. Activation of memory circuits during cue-elicited cocaine craving. Proc Natl Acad Sci USA. 1996;93:12040–12045. doi: 10.1073/pnas.93.21.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Heiman GM, Dunn B. Decision biases and persistent illicit drug use: an experimental study of distributed choice and addiction. Drug Alcohol Depend. 2002;67:193–203. doi: 10.1016/s0376-8716(02)00071-6. [DOI] [PubMed] [Google Scholar]
- 56.Heims HC, Critchley HD, Dolan R, Mathias CJ, Cipolotti L. Social and motivational functioning is not critically dependent on feedback of autonomic responses: neuropsychological evidence from patients with pure autonomic failure. Neuropsychologia. 2004;42:1979–1988. doi: 10.1016/j.neuropsychologia.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 57.Heinz A, Siessmeier T, Wrase J, Hermann D, Klein S, Grüsser-Sinopoli SM, Flor H, Braus DT, Buchholtz HG, Gründer G, Schreckenberger M, Smolka MN, Rösch F, Mann K, Bartenstein P. Correlation between dopamine D2 receptors in the ventral striatum and central processing of alcohol cues and craving. Am J Psychiatry. 2004;161:1783–1789. doi: 10.1176/appi.ajp.161.10.1783. [DOI] [PubMed] [Google Scholar]
- 58.Hinson JM, Jameson TL, Whitney P. Somatic markers, working memory, and decision making. Cogn Affect Behav Neurosci. 2002;2:341–353. doi: 10.3758/cabn.2.4.341. [DOI] [PubMed] [Google Scholar]
- 59.Hoshi R, Bisla J, Curran HV. The acute and sub-acute effects of ‘ecstasy’ (MDMA) on processing of facial expressions: preliminary findings. Drug Alcohol Depend. 2004;76:297–304. doi: 10.1016/j.drugalcdep.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 60.Jentsch JD, Taylor JR. Impulsivity resulting from frontostriatal dysfunction in drug abuse: implications for the control of behavior by reward related stimuli. Psychopharmacology. 1999;146:373–390. doi: 10.1007/pl00005483. [DOI] [PubMed] [Google Scholar]
- 61.Kano M, Gyoba J, Kamachi M, Mochizuki H, Hongo M, Yanai K. Low doses of alcohol have a selective effect on therecognition ofhappy facialexpressions. Hum Psychopharmacol. 2002;18:131–139. doi: 10.1002/hup.440. [DOI] [PubMed] [Google Scholar]
- 62.Kilts C. Imaging the roles of the amygdala in drug addiction. Psychopharmacol Bull. 2001;35:84–94. [PubMed] [Google Scholar]
- 63.Kilts CD, Gross RE, Ely TD, Drexler KPG. The neural correlates of cue-induced craving in cocaine-dependent women. Am J Psychiatry. 2004;161:233–241. doi: 10.1176/appi.ajp.161.2.233. [DOI] [PubMed] [Google Scholar]
- 64.Kilts CD, Schweitzer JB, Quinn CK, Gross RE, Faber TL, Muhammad F, Ely TD, Hoffman JM, Drexler KPG. Neural activity related to drug craving in cocaine addiction. Arch Gen Psychiatry. 2001;58:334–341. doi: 10.1001/archpsyc.58.4.334. [DOI] [PubMed] [Google Scholar]
- 65.Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- 66.Kish SJ, Kalasinsky KS, Derkach P, Schmunk GA, Guttman M, Ang L, Adams V, Furukawa Y, Haycock JW. Striatal dopaminergic and serotonergic markers in human heroin users. Neuropsychopharmacology. 2001;24:561–567. doi: 10.1016/S0893-133X(00)00209-8. [DOI] [PubMed] [Google Scholar]
- 67.Knowlton BJ, Mangels JA, Squire LR. A neostriatal habit learning system in humans. Science. 1996;273:1399–1402. doi: 10.1126/science.273.5280.1399. [DOI] [PubMed] [Google Scholar]
- 68.Kornreich C, Blairy S, Philippot P, Dan B, Foisy M, Hess U, Le Bon O, Pelc I, Verbank P. Impaired emotional facial expression recognition in alcoholism compared with obsessive-compulsive disorders and normal controls. Psychiatry Res. 2001;102:235–248. doi: 10.1016/s0165-1781(01)00261-x. [DOI] [PubMed] [Google Scholar]
- 69.Kornreich C, Foisy M, Philippot P, Dan P, Tecco J, Noël X, Hees U, Pelec I, Verbank P. Impaired emotional facial expression recognition in alcoholic, opiate dependent subjects, methadone maintenance subjects, and mixed alcohol-opiate antecedent subjects compared with normal controls. Psychiatry Res. 2003;119:251–260. doi: 10.1016/s0165-1781(03)00130-6. [DOI] [PubMed] [Google Scholar]
- 70.Lawrence AD, Evans AH, Lees AJ. Compulsive use of dopamine replacement therapy in Parkinson´s disease: reward systems gone awry? Lancet Neurol. 2003;2:595–204. doi: 10.1016/s1474-4422(03)00529-5. [DOI] [PubMed] [Google Scholar]
- 71.Lim KO, Choi SJ, Pomara N, Wolkin A, Rotrosen JP. Reduced frontal white matter integrity in cocaine dependence: A controlled diffusion tensor imaging study. Biol Psychiatry. 2002;51:890–895. doi: 10.1016/s0006-3223(01)01355-5. [DOI] [PubMed] [Google Scholar]
- 72.London ED, Ernst M, Grant S, Bonson K, Weinstein A. Orbitofrontal cortex and human drug abuse: Functional imaging. Cereb Cortex. 2000;10:334–342. doi: 10.1093/cercor/10.3.334. [DOI] [PubMed] [Google Scholar]
- 73.Lu L, Grimm JW, Hope BT, Shaham Y. Incubation of cocaine craving after withdrawal: a review of preclinical data. Neuropsychopharmacology. 2004;47:214–226. doi: 10.1016/j.neuropharm.2004.06.027. [DOI] [PubMed] [Google Scholar]
- 74.Lyoo IK, Streeter CC, Ahn KH, Lee HK, Pollack MH, Silveri MM, Nassar L, Levin JM, Sarid-Segal O, Ciraulo DA, Renshaw PF, Kaufman MJ. White matter hyperintensities in subjects with cocaine and opiate dependence and healthy comparison subjects. Psychiatry Res. 2004;131:135–145. doi: 10.1016/j.pscychresns.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 75.Maas LC, Lukas SE, Kaufman MJ, Weiss RD, Daniels SL, Rogers VW, Kukes TJ, Renshaw PF. Functional magnetic resonance of human brain activation during cue-induced cocaine craving. Am J Psychiatry. 1998;155:124–126. doi: 10.1176/ajp.155.1.124. [DOI] [PubMed] [Google Scholar]
- 76.Maia TV, McLelland JV. A re-examination of the evidence for the somatic marker hypothesis: What participants really know about the Iowa gambling task. Proc Natl Acad Sci USA. 2004;9:16075–16080. doi: 10.1073/pnas.0406666101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Makris N, Gasic GP, Seidman LJ, Goldstein JM, Gastfriend DR, Elman I, Albaugh MD, Hodge SM, Ziegler DA, Sheahan FS, Caviness VS, Tsuang MT, Kennedy DN, Hyman SE, Rosen BR, Breiter HC. Decreased absolute amygdala volume in cocaine addicts. Neuron. 2004;44:729–740. doi: 10.1016/j.neuron.2004.10.027. [DOI] [PubMed] [Google Scholar]
- 78.Martin CO, Denburg NL, Tranel D, Granner MA, Bechara A. The effects of vagus nerve stimulation on decision-making. Cortex. 2004;40:605–612. doi: 10.1016/s0010-9452(08)70156-4. [DOI] [PubMed] [Google Scholar]
- 79.Martin-Soelch C, Chevalley AF, Kunig G, Missimer J, Magyar S, Mino A, Schultz W, Leenders KL. Changes in reward-induced brain activation in opiate addicts. Eur J Neurosci. 2001;18:2605–2610. doi: 10.1046/j.0953-816x.2001.01753.x. [DOI] [PubMed] [Google Scholar]
- 80.Mathews SC, Simmons AN, Lane SD, Paulus MP. Selective activation of the nucleus accumbens during risk-taking and decision-making. Neuroreport. 2004;15:2123–2127. doi: 10.1097/00001756-200409150-00025. [DOI] [PubMed] [Google Scholar]
- 81.Matochik JA, London ED, Eldreth DA, Cadet JL, Bolla KI. Frontal cortical tissue composition in abstinent cocaine abusers: a magnetic resonance imaging study. Neuroimage. 2003;19:1095–1102. doi: 10.1016/s1053-8119(03)00244-1. [DOI] [PubMed] [Google Scholar]
- 82.Mazas CA, Finn PR, Steinmetz JE. Decision-making biases, antisocial personality, and early onset alcoholism. Alcohol Clin Exp Res. 2000;24:1036–1040. [PubMed] [Google Scholar]
- 83.Mitchell DGV, Colledge E, Leonard A, Blair RJR. Risky decisions and response reversal: is there evidence of orbitofrontal cortex dysfunction in psychopathic individuals. Neuropsychologia. 2002;40:2013–2022. doi: 10.1016/s0028-3932(02)00056-8. [DOI] [PubMed] [Google Scholar]
- 84.Moeller FG, Hasan KM, Steinberg JL, Kramer LA, Dougherty DM, Valdes I, Swann AC, Barrat ES, Narayana PA. Reduced anterior corpus callosum white matter integrity is related to increased impulsivity and reduced discriminability in cocaine-dependent subjects: diffusion tensor imaging. Neuropsychopharmacology. 2005;30:610–617. doi: 10.1038/sj.npp.1300617. [DOI] [PubMed] [Google Scholar]
- 85.Monterosso J, Ehrman R, Napier K, O´Brien CP, Childress AR. Three decision-making tasks in cocaine-dependent patients: do they measure the same construct. Addiction. 2001;96:1825–1837. doi: 10.1046/j.1360-0443.2001.9612182512.x. [DOI] [PubMed] [Google Scholar]
- 86.Murphy FC, Smith KA, Cowen PJ, Robbins TW, Sahakian BJ. The effects of tryptophan depletion on cognitive and affective processing in healthy volunteers. Psychopharmacology. 2002;163:42–53. doi: 10.1007/s00213-002-1128-9. [DOI] [PubMed] [Google Scholar]
- 87.Nauta WJH. The problem of the frontal lobes: a reinterpretation. J Psychiatry Res. 1971;8:167–187. doi: 10.1016/0022-3956(71)90017-3. [DOI] [PubMed] [Google Scholar]
- 88.Obrocki J, Schmoldt A, Buchert R, Andresen B, Petersen K, Thomasius R. Specific neurotoxicity of chronic use of ecstasy. Toxicol Lett. 2002;127:285–297. doi: 10.1016/s0378-4274(01)00511-2. [DOI] [PubMed] [Google Scholar]
- 89.Panksepp J, Knutson B, Burgdorf J. The role of brain emotional systems in addictions: a neuro-evolutionary perspective and new self report animal model. Addiction. 2002;97:459–469. doi: 10.1046/j.1360-0443.2002.00025.x. [DOI] [PubMed] [Google Scholar]
- 90.Paulus MP, Hozack N, Frank L, Brown GB, Schuckit MA. Decision-making by methamphetamine-dependent subjects is associated with error-rate independent decrease in prefrontal and parietal activation. Biol Psychiatry. 2003;53:65–74. doi: 10.1016/s0006-3223(02)01442-7. [DOI] [PubMed] [Google Scholar]
- 91.Paulus MP, Hozack N, Zauscher BE, Frank L, Brown GB, Braff DL, Schuckit MA. Behavioral and functional neuroimaging evidence for prefrontal dysfunction in methamphetamine-dependent subjects. Neuropsychopharmacology. 2002;26:53–63. doi: 10.1016/S0893-133X(01)00334-7. [DOI] [PubMed] [Google Scholar]
- 92.Petry NM, Bickel WK, Arnett M. Shortened time horizons and insensitivity to future consequences in heroin addicts. Addiction. 1998;93:729–738. doi: 10.1046/j.1360-0443.1998.9357298.x. [DOI] [PubMed] [Google Scholar]
- 93.Rainville P, Duncan GH, Price DD, Carrier B, Bushnell MC. Pain affect encoded in human anterior cingulated but not somatosensory cortex. Science. 1997;277:968–971. doi: 10.1126/science.277.5328.968. [DOI] [PubMed] [Google Scholar]
- 94.Redish AD. Addiction as a computational process gone awry. Science. 2004;306:1944–1947. doi: 10.1126/science.1102384. [DOI] [PubMed] [Google Scholar]
- 95.Robbins TW. Chemical neuromodulation of frontal-executive functions in humans and other animals. Exp Brain Res. 2000;133:130–138. doi: 10.1007/s002210000407. [DOI] [PubMed] [Google Scholar]
- 96.Robinson TE, Berridge KC. Addiction Annu Rev Psychol. 2003;54:25–53. doi: 10.1146/annurev.psych.54.101601.145237. [DOI] [PubMed] [Google Scholar]
- 97.Robinson TE, Berridge KE. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–291. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- 98.Rogers R, Lancaster M, Wakeley J, Bhagwagar Z. Effects of beta-adrenoceptor blockade on components of human decision-making. Psychopharmacology. 2004;172:157–174. doi: 10.1007/s00213-003-1641-5. [DOI] [PubMed] [Google Scholar]
- 99.Rogers RD, Everitt BJ, Baldacchino A, Blackshaw AJ, Swainson R, Wynne K, Baker NB, Hunter J, Carthy T, Booker E, London M, Deakin JFW, Sahakian BJ, Robbins TW. Dissociable deficits in the decision-making cognition of chronic amphetamine abusers, opiate abusers, patients with focal damage to prefrontal cortex, and tryptophan-depleted normal volunteers: evidence for monoaminergic mechanisms. Neuropsychopharmacology. 1999;20:322–339. doi: 10.1016/S0893-133X(98)00091-8. [DOI] [PubMed] [Google Scholar]
- 100.Roiser JP, Sahakian BJ. Relationship between ecstasy use and depression: a study controlling for poly-drug use. Psychopharmacology. 2004;173:411–417. doi: 10.1007/s00213-003-1705-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rolls ET. The orbitofrontal cortex. Philos Trans R Soc Lond. 1996;351:1433–1444. doi: 10.1098/rstb.1996.0128. [DOI] [PubMed] [Google Scholar]
- 102.Schlaepfer TE, Pearlson GD, Wong DF, Marenco S, Dannals RF. PET study of competition between intravenous cocaine and [11C]Raclopride at dopamine receptors in human subjects. Am J Psychiatry. 1997;154:1209–1213. doi: 10.1176/ajp.154.9.1209. [DOI] [PubMed] [Google Scholar]
- 103.Schreckenberger M, Gouzolis-Mayfrank E, Sabri O, Arning C, Zimny M, Zeggel T, Wagenknetch G, Kaiser HJ, Sass H, Buell U. “Ecstasy”-induced changes of cerebral glucose metabolism and their correlation to acute psychopathology. Eur J Nucl Med. 1999;26:1573–1579. doi: 10.1007/s002590050497. [DOI] [PubMed] [Google Scholar]
- 104.Sekine Y, Iyo M, Ouchi Y, Matsunaga T, Tsukada H, Okada H, Yoshikawa E, Futatsubashi M, Takey N, Mori N. Methamphetamine-related psychiatric symptoms and reduced brain dopamine transporters studied with PET. Am J Psychiatry. 2001;158:1206–1214. doi: 10.1176/appi.ajp.158.8.1206. [DOI] [PubMed] [Google Scholar]
- 105.Sell LA, Morris JS, Bearn J, Frackowiak RSJ, Friston KJ, Dolan RJ. Neural responses associated with cue evoked emotional states and heroin in opiate addicts. Drug Alcohol Depend. 2000;60:207–216. doi: 10.1016/s0376-8716(99)00158-1. [DOI] [PubMed] [Google Scholar]
- 106.Stout JC, Busemeyer JR, Lin A, Grant SJ, Bonson KR. Cognitive modeling analysis of decision-making processes in cocaine abusers. Psychon Bull Rev. 2004;4:742–747. doi: 10.3758/bf03196629. [DOI] [PubMed] [Google Scholar]
- 107.Stout JC, Rock SL, Campbell MC, Busemeyer JR, Finn PR. Psychological Processes Underlying Risky Decisions in Drug Abusers. Psychol Addict Behav. 2005;19:148–157. doi: 10.1037/0893-164X.19.2.148. [DOI] [PubMed] [Google Scholar]
- 108.Suzuki A, Hirota A, Takasawa N, Shigemasu K. Application of the somatic marker hypothesis to individual differences in decision-making. Biol Psychol. 2003;65:81–88. doi: 10.1016/s0301-0511(03)00093-0. [DOI] [PubMed] [Google Scholar]
- 109.Tapert SF, Brown GG, Baratta MV, Brown SA. fMRI BOLD response to alcohol stimuli in alcohol dependent young women. Addict Behav. 2004;29:33–50. doi: 10.1016/j.addbeh.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 110.Tiffany ST. Cognitive concepts of craving. Alcohol Res Health. 1999;23:215–224. [PMC free article] [PubMed] [Google Scholar]
- 111.Townshend JM, Duka T. Mixed emotions: alcoholics´ impairment in the recognition of specific facial expressions. Neuropsychologia. 2003;41:773–782. doi: 10.1016/s0028-3932(02)00284-1. [DOI] [PubMed] [Google Scholar]
- 112.Tranel D, Bechara A, Denburg NL. Asymmetric functional roles of right and left ventromedial prefrontal cortices in social conduct, decision-making, and emotional processing. Cortex. 2002;38:589–612. doi: 10.1016/s0010-9452(08)70024-8. [DOI] [PubMed] [Google Scholar]
- 113.van Honk J, Hermans EJ, Putman P, Montagne B, Schutter DJ. Defective somatic-markers in subclinical psychopathy. Neuroreport. 2002;13:1025–1027. doi: 10.1097/00001756-200206120-00009. [DOI] [PubMed] [Google Scholar]
- 114.Verney SP, Brown GG, Frank L, Paulus MP. Error-rate related caudate and parietal cortex activation during decision-making. Neuroreport. 2003;14:923–928. doi: 10.1097/01.wnr.0000072842.93264.b6. [DOI] [PubMed] [Google Scholar]
- 115.Volkow ND, Chang L, Wang G, Fowler JS, Franceschi D, Sedler MJ, Gatley SJ, Hitzemann R, Ding Y, Wong C, Logan J. Higher cortical and lower subcortical metabolism in detoxified methamphetamine abusers. Am J Psychiatry. 2001;158:383–389. doi: 10.1176/appi.ajp.158.3.383. [DOI] [PubMed] [Google Scholar]
- 116.Volkow ND, Chang L, Wang GJ, Fowler JS, Ding YS, Sedler M, Logan J, Franceschi D, Gatley J, Hitzemann RJ, Gifford A, Wong C, Pappas N. Low level of brain dopamine D2 receptors in methamphetamine abusers: association with metabolism in the orbitofrontal cortex. Am J Psychiatry. 2001;158:2015–2021. doi: 10.1176/appi.ajp.158.12.2015. [DOI] [PubMed] [Google Scholar]
- 117.Volkow ND, Fowler JS. Addiction: A disease of compulsion and drive: Involvement of the orbitofrontal cortex. Cereb Cortex. 2000;10:318–325. doi: 10.1093/cercor/10.3.318. [DOI] [PubMed] [Google Scholar]
- 118.Volkow ND, Fowler JS, Wang GJ. The addicted human brain viewed in the light of imaging studies: brain circuits and treatment strategies. Neuropharmacology. 2004;47:3–13. doi: 10.1016/j.neuropharm.2004.07.019. [DOI] [PubMed] [Google Scholar]
- 119.Volkow ND, Wang GJ, Fowler JS, Logan J, Hitzemann RJ, Ding YS, Pappas N, Shea C, Piscani K. Decreases in dopamine receptors but not in dopamine transporters in alcoholics. Alcohol Clin Exp Res. 1996;20:1594–1598. doi: 10.1111/j.1530-0277.1996.tb05936.x. [DOI] [PubMed] [Google Scholar]
- 120.Volkow ND, Wang GJ, Fowler JS, Hitzemann R, Angrist B, Gatley J, Logan SJ, Ding YS, Pappas N. Association of methylphenidate-induced craving with changes in right striato-orbitofrontal metabolism in cocaine abusers: implications in addiction. Am J Psychiatry. 1999;156:19–26. doi: 10.1176/ajp.156.1.19. [DOI] [PubMed] [Google Scholar]
- 121.Volkow ND, Wang GJ, Fowler JS, Logan SJ, Franceschi D, Maynard L, Ding YS, Gatley SJ, Gifford A, Zhu W, Swanson JM. Relationship between blockade of dopamine transporters by oral methylphenidate and the increases in extracellular dopamine: therapeutic implications. Synapse. 2002;43:181–187. doi: 10.1002/syn.10038. [DOI] [PubMed] [Google Scholar]
- 122.Volkow ND, Wang GJ, Fowler JS, Logan SJ, Gatley J, Hitzemann RJ, Chen AD, Pappas N. Decreased striatal dopaminergic responsiveness in detoxified cocaine-dependent subjects. Nature. 1997;386:830–833. doi: 10.1038/386830a0. [DOI] [PubMed] [Google Scholar]
- 123.Volkow ND, Wang GJ, Fowler JS, Logan SJ, Gatley J, Wong C, Hitzemann R, Pappas N. Reinforcing effects of psychostimulants in humans are associated with increases in brain dopamine and occupancy of D2 receptors. J Pharmacol Exp Ther. 1999;291:409–415. [PubMed] [Google Scholar]
- 124.Volkow ND, Wang GJ, Fowler JS, Thanos P, Logan SJ, Gatley J, Gifford A, Ding YS, Wong C, Pappas N. Brain DA D2 receptors predict reinforcing effects of stimulants in humans: replication study. Synapse. 2002;46:79–82. doi: 10.1002/syn.10137. [DOI] [PubMed] [Google Scholar]
- 125.Wang GJ, Volkow ND, Chang L, Miller E, Sedler M, Hitzemann RJ, Zhu W, Logan J, Fowler JS. Partial recovery of brain metabolism in methamphetamine abusers after protracted abstinence. Am J Psychiatry. 2004;161:242–248. doi: 10.1176/appi.ajp.161.2.242. [DOI] [PubMed] [Google Scholar]
- 126.Wang GJ, Volkow ND, Fowler JS, Cervany P, Hitzemann RJ, Pappas NR, Wong CT, Felder C. Regional brain metabolic activation during craving elicited by recall of previous drug experiences. Life Sci. 1999;64:775–784. doi: 10.1016/s0024-3205(98)00619-5. [DOI] [PubMed] [Google Scholar]
- 127.Wang GJ, Volkow ND, Fowler JS, Logan J, Hitzemann RJ, Pappas NS, Piscani K. Dopamine D2 receptor availability in opiate-dependent subjects before and after naloxone precipitated withdrawal. Neuropsychopharmacology. 1997;16:174–182. doi: 10.1016/S0893-133X(96)00184-4. [DOI] [PubMed] [Google Scholar]
- 128.Wexler BE, Gottschalk CH, Fulbright RK, Prohovnik I, Lacadie CM, Rounsaville BJ, Gore JC. Functional magnetic resonance imaging of cocaine craving. Am J Psychiatry. 2001;158:86–95. doi: 10.1176/appi.ajp.158.1.86. [DOI] [PubMed] [Google Scholar]
- 129.White Addictive drugs as reinforcers: Multiple partial actions on memory systems. Addiction. 1996;91:921–949. [PubMed] [Google Scholar]
- 130.Whitlow CT, Liguori A, Livengood LB, Hart SL, Mussat-Whitlow BJ, Lamborn CM, Laurienti PJ, Porrino LJ. Long-term heavy marijuana users make costly decisions on a gambling task. Drug Alcohol Depend. 2004;76:107–111. doi: 10.1016/j.drugalcdep.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 131.Wrase J, Grüsser SM, Klein S, Diener C, Hermann D, Flor H, Mann K, Braus DF, Heinz A. Development of alcohol-associated cues and cue-induced brain activation in alcoholics. Eur Psychiatry. 2002;17:287–291. doi: 10.1016/s0924-9338(02)00676-4. [DOI] [PubMed] [Google Scholar]