Abstract
Background:
Cigarette smoking and alcohol use disorders are closely linked, but it is not clear whether higher rates of alcohol use disorder (AUD) among smokers are solely attributable to heavier drinking, or alternatively, whether smokers are more vulnerable to alcohol abuse and dependence than non-smokers who drink comparable quantities. We sought to address this issue using data from a nationally representative U.S. sample of adolescents and young adults. Specifically, we analyzed the relationship between cigarette smoking, drinking, and alcohol use disorders.
Methods:
Data were from the aggregated 2002 through 2004 U.S. National Survey on Drug Use and Health. Participants were randomly selected, household-dwelling adolescents and young adults (ages 12-20) from the non-institutionalized, civilian population of the United States (N=74,836). Measurements included current DSM-IV alcohol abuse or dependence, number of drinks in the past 30-days, and past-year cigarette smoking, defined as having smoked more than 100 cigarettes across the lifetime and having smoked during the past year.
Results:
Past-year smokers, (prevalence=16.0%) drank in higher quantities than never-smokers, but were also at elevated risk for AUD when compared to never-smokers who drank equivalent quantities. The effect was observed across age groups, but was more prominent among younger adolescents. After adjusting for drinking quantity and sociodemographic variables, smokers had 4.5-fold higher odds of AUD than never-smokers (95% CI: 3.1-6.6). Youths who reported smoking but did not cross the 100-cigarette threshold were at intermediate risk (OR=2.3, 95% CI: 1.7-3.3). Differences in AUD between smokers and never-smokers were most pronounced at lower levels of drinking.
Conclusions:
The results are consistent with a higher vulnerability to alcohol use disorders among smokers, compared to non-smokers who drink equivalent quantities.
Keywords: Cigarettes, epidemiology, alcohol, abuse, dependence, tobacco, adolescence
Introduction
Tobacco smoking and excessive alcohol use comprise the first and third most lethal modifiable risk factors affecting health in the United States (Mokdad et al., 2004). Every year, approximately 1.5 million people in the U.S. become daily cigarette smokers and the overwhelming majority of those individuals are adolescents and young adults (Chen and Kandel, 1995; Substance Abuse and Mental Health Services Administration, 2004; U. S. Department of Health and Human Services, 1994). In addition to the chronic effects that smoking has on morbidity later in life, smoking in adolescence presents a unique set of health-risks, including reduced rates of lung growth and elevated respiratory problems (Arday et al., 1995). Moreover, individuals who smoke early in life are less likely to quit as adults (Breslau and Peterson, 1996). Likewise, alcohol use typically begins in adolescence, and early initiation of alcohol use is a strong predictor of subsequent problems and dependence (DeWit et al., 2000; Grant and Dawson, 1997; Prescott and Kendler, 1999).
In addition to the direct impact of smoking and excessive drinking on general health outcomes, there is a strong tendency for cigarette smoking and alcohol dependence to co-occur, and both are associated with other drug use disorders (Dani and Harris, 2005; Grant et al., 2004; John et al., 2004; Kessler et al., 2005). Tobacco smoking and alcohol use have long been recognized as early and important steps on the pathway to more serious drug use (Kandel, 1975; Kandel et al., 1992; Lai et al., 2000; Torabi et al., 1993). Because of their legality (for adults) and ready availability, both alcohol and tobacco are seen as gateways to more serious substance use. Cigarette smoking is of special interest because cigarettes were legally available to minors until recently, and are still readily available to minors from the Internet and non-commercial sources (Castrucci et al., 2002; Jensen et al., 2004; Ribisl et al., 2003). Moreover, evidence from a number of studies indicates that cigarette smoking is a strong predictor of subsequent alcohol use, abuse and dependence (Biederman et al., 2005; Chen et al., 2002; Grant, 1998; Lewinsohn et al., 1999). Prospective (Lewinsohn et al., 1999) and retrospective (Grant, 1998) studies have shown that the age at which smoking starts is a robust predictor of heavy alcohol consumption and alcohol use disorders. In an analysis of retrospective data from a large, nationally representative sample, this association held even when accounting for such factors as age at first drink, duration of alcohol use and family history of alcohol dependence (Grant, 1998).
While the link between smoking and alcoholism is well documented, it is not clear whether smoking is simply related to heavier drinking, resulting in alcohol problems, or whether drinkers who smoke are more vulnerable to alcohol use disorders than those who do not. A great deal of research on the connection between cigarette smoking and alcohol use or alcoholism has focused on psychosocial factors, which presumably lead to higher levels of drinking by resulting in more opportunities and greater inclinations to drink. Such factors include deviant peer group association, and risk-prone personality traits that are known to predict use of alcohol and other drugs (Dinn et al., 2004; Fergusson et al., 2002; Kopstein et al., 2001; Wills and Cleary, 1999). However, these psychosocial factors may not completely account for the association between early smoking and subsequent alcohol and drug problems (Siqueira and Brook, 2003). Some authors have speculated that the pathway from use of alcohol and tobacco to abuse of the same substances, and of illicit drugs, may be facilitated by effects of early-stage drug use on central reward circuitry. Such suggestions are based on observations in animal models that exposure to some drugs alters future behavioral responses to the same or other drugs (Schenk, 2002).
One potential indicator of whether groups of individuals exhibit differential vulnerability to addiction for a given substance is the relationship between use and abuse or dependence. This approach was used by Chen and Kandel to examine the relationship between substance use and dependence for the cases of nicotine and cocaine (Chen and Kandel, 2002; Kandel and Chen, 2000;). In the present study, we take an analogous approach to address whether smoking might predict differential susceptibility to alcohol abuse and/or dependence, also known as alcohol use disorder (AUD). We sought to examine the relationship between alcohol consumption and AUD in youths ages 12-20 as a function of cigarette smoking. Higher levels of AUD among smokers who drink at similar levels as their never-smoking counterparts could indicate that smoking among youths is associated specifically with vulnerability to AUD, rather than simply being a predictor of higher rates of drinking.
The National Survey on Drug Use and Health is an ideal source of data to address these questions further because it is the only major U.S. national survey that assesses diagnostic criteria for alcohol use disorder (AUD) among younger adolescents (ages 12-14), in addition to including commonly used measures of alcohol consumption. To our knowledge, none of the existing studies on the associations between smoking and AUD in adolescence utilize nationally representative samples, except those based on retrospective reports from adults. Accordingly, this report will also describe the epidemiology of cigarette smoking and AUD in a large, nationally representative sample of adolescents and young adults.
Methods
Survey Description
Data were aggregated from the 2002 through 2004 administrations of the National Survey on Drug Use and Health (NSDUH; Substance Abuse and Mental Health Services Administration, 2003; Wright et al., 2002). Samples for all three administrations were selected to be representative of the non-institutionalized civilian population of the United States, ages 12 and older, including those residing in group quarters (e.g., college dormitories). Independent, multistage area probability samples were collected each year for all 50 U.S. states and the District of Columbia. The total sample size was 135,910. Prior to public release of the data, sub-sampling was used to protect respondent identity, reducing the combined sample size to 109,309. The survey was conducted anonymously, that is, participants' names were not recorded or linked with their answers. General information was collected in face-to-face interviews administered by trained interviewers while audio computer-assisted self-interview (ACASI) methods were used to collect sensitive information; i.e. responses to substance use modules were not disclosed to the interviewer. Informed consent was obtained from all participants.
Oversampling of youths (ages 12-17) and young adults (ages 18-25) was incorporated into the NSDUH procedures. The present analyses include subjects ages 20 and younger. Age 20 was selected as the upper bound to avoid complications arising from combining legal aged drinkers with underage drinkers in the same analyses. Response rate for the 12-20 year-old age bracket was 80.7% for the 2002-2004 surveys. The subsample size for individuals under age 21 was 75,633; 78 participants were excluded from the analyses because of missing responses to questions needed for smoking categorization.
Cigarette Smoking
Individuals who indicated that they had ever smoked cigarettes were probed about the quantity they had smoked and whether they had ever smoked daily for a period of 30 days or longer. For the present analyses, individuals who had never initiated smoking were classified as never-smokers (n=44,009). Those who had ever smoked, but had smoked 100 or fewer cigarettes in their lifetime were classified as experimenters (n=19,442). Former smokers (individuals who had smoked more than 100 cigarettes in their lives, but reported not smoking at all in the past year) were excluded from the analyses (n=719), as were subjects with incomplete data on necessary variables (n=78). Those who had smoked more than 100 cigarettes in their lives and reported any past-year smoking were classified as smokers (n=11,385). Resulting sample size for the analyses was 74,836. The 100-cigarette threshold is a commonly used cutoff, employed by several major surveys including the National Health Interview Survey (e.g., Wortley et al., 2003). Individuals whose tobacco use was limited to pipes, cigars, or smokeless tobacco were counted as never-smokers (n=3,050, or 4.1% of the total sample). The vast majority (85.9%) of non-cigarette tobacco users also smoked cigarettes at some point in their lives. The decision to count the remainder as never-smokers was made as a more conservative alternative to excluding these subjects from the analyses. Analyses contrasted past-year smokers with never-smokers and experimenters.
Alcohol Use
Questions assessing quantity of alcohol use covered the past 30-day time frame. Past-30 day consumption was calculated from responses to questions regarding the number of drinking days during this time frame and the typical amount consumed per drinking day. For some descriptive analyses, categories of drinking quantity were defined based on the distribution among the subset of participants who reported one or more drink in the past month (n=18,290 or 25.3% of the weighted sample). The cutoffs were chosen such that the lowest drinking category (1-8 drinks in the past month) comprised approximately 40% of past-month drinkers, while the remaining three groups (9-20 drinks, 21-50 drinks, more than 50 drinks) each consisted of about 20% of these subjects.
Alcohol Use Disorder
The NSDUH interview included a section of 14 questions that probed symptoms of DSM-IV (American Psychiatric Association, 2000) alcohol abuse and dependence that was administered to past-year drinkers. Each question is asked on a 12-month basis; e.g., “During the past 12 months, did drinking alcohol cause you to do things that repeatedly got you in trouble with the law?” Alcohol-use disorder, defined as the presence of alcohol abuse or dependence in the last 12-months, was coded according to DSM-IV specifications. The level of agreement between alcohol-use disorder diagnoses obtained using the NSDUH interview and clinician-administered interviews is comparable to levels of agreement with clinician diagnoses obtained using state-of-the-art lay-administered structured interviews (BK Jordan, RS Karg, K Batts, CA Wiesen, and JF Epstein; Manuscript submitted for publication, 2005).
Other Variables
Age was categorized into three, 3-year intervals: 12-14 years old, 15-17 years and 18-20 years old. Race combined with ethnicity was grouped into four categories: White, Black, Hispanic, and other; the latter category includes non-Hispanic mixed race individuals. For models incorporating past 30-day quantity of alcohol consumption, the logarithms of the number of drinks was used. The log transformation was a substantially better predictor of AUD than the untransformed variable. Inclusion of polynomial terms did not result in substantive improvements in model fit. Family income was grouped into four categories: <$20,000 per year, $20,000-$50,000 per year, $50,000-$75,000 per year and over $75,000 per year. Population density was defined by whether or not the individual resided in a metropolitan statistical area, or “metropolitan area”, as defined by the U.S. Census Bureau.
Statistical Methods
All statistical analyses were conducted using the SUDAAN statistical software package (RTI International, 2004). Variance estimation utilized a Taylor linearization method appropriate for the multistage design of the survey; sampling weights were utilized for all analyses so that the sample was demographically representative of the 12-20 year old U.S. population according to U.S. census estimates. Two-by-two contingency tables with Chi-square tests were used to analyze associations between categorical variables. Logistic regression models were employed for bivariate and multivariate models of alcohol use disorder.
Results
Sociodemographic Correlates of Youth Smoking
Demographic description of the unweighted and weighted 2002-2004 NSDUH sample is presented in Table 1. The prevalences of past-year smoking by demographic group are presented in Table 2. For this sample of youths ages 12-20, the prevalence of past-year smoking was 16.0% (SE=0.2%) -- this includes only individuals who report having smoked more than 100 cigarettes in their life. The vast majority (84%) of past-year smokers reported being daily smokers, defined as ever having smoked daily for a period of 30 days or longer. Hence, the 100-cigarette cut-off appears to be effective at identifying committed smokers in this age range. An additional 26.3% of youths reported trying smoking at some point in their lives (labeled “experimenters”), but had not crossed the 100-cigarette threshold. Males and females reported smoking in approximately equal numbers in the 12-16 year old range, but there were more male smokers than female smokers in the 17-20 year-old range. Only 2.1% (SE=0.1) of 12-14 year-olds reported past-year smoking but prevalence rose rapidly with age: more than one-in-three 19-20 year-olds reported past-year smoking. Smoking was more prevalent in White youths than in racial / ethnic minorities, particularly Black youths. Youths from lower income households were more likely to report past-year smoking, as were those from non-metropolitan areas.
Table 1.
Demographic Composition of 2002-04 NSDUH Samples of Youth 20 and Under.
| N | Weighted % | (SE) | |
|---|---|---|---|
| Sex | |||
| Male | 37,786 | 51.1 | (0.2) |
| Female | 37,050 | 48.9 | (0.2) |
| Age | |||
| 12-14 | 27,540 | 34.1 | (0.3) |
| 15-17 | 26,326 | 32.9 | (0.2) |
| 18-20 | 20,970 | 33.0 | (0.3) |
| Race/Ethnicity | |||
| White | 48,187 | 62.2 | (0.3) |
| Black | 10,236 | 14.7 | (0.3) |
| Hispanic | 10,766 | 16.5 | (0.3) |
| Other | 5,647 | 6.6 | (0.2) |
| Household Income | |||
| <$20K/yr | 17,766 | 23.4 | (0.3) |
| $20-50K/yr | 26,132 | 34.2 | (0.3) |
| $50-75K/yr | 13,748 | 17.7 | (0.2) |
| >$75K/yr | 17,190 | 24.7 | (0.3) |
| Population Density | |||
| Metropolitan | 53,790 | 77.9 | (0.3) |
| Non-metropolitan | 21,046 | 22.1 | (0.3) |
| Total | 74,836 | 100.0 |
Table 2.
Prevalence of Smoking1 by Demographic Group
|
Never-Smokers (N=44,009) |
Experimenters (N=19,442) |
Smokers (N=11,385) |
Chi-square Tests |
|||||
|---|---|---|---|---|---|---|---|---|
| % | (SE) | % | (SE) | % | (SE) | χ2 | p | |
| Total (N=74,836) | 57.7 | (0.3) | 26.3 | (0.2) | 16.0 | (0.2) | ||
| Sex | ||||||||
| Male | 57.1 | (0.4) | 25.8 | (0.3) | 17.1 | (0.3) | 46 | <0.001 |
| Female | 58.3 | (0.4) | 26.9 | (0.3) | 14.7 | (0.2) | ||
| Age | ||||||||
| 12-14 | 82.9 | (0.3) | 15.0 | (0.3) | 2.1 | (0.1) | 6329 | <0.001 |
| 15-17 | 54.7 | (0.4) | 31.8 | (0.3) | 13.5 | (0.3) | ||
| 18-20 | 34.5 | (0.5) | 32.7 | (0.4) | 32.7 | (0.5) | ||
| Race/Ethnicity | ||||||||
| White | 54.3 | (0.3) | 26.1 | (0.3) | 19.6 | (0.3) | 795 | <0.001 |
| Black | 67.2 | (0.6) | 25.1 | (0.6) | 7.7 | (0.4) | ||
| Hispanic | 59.5 | (0.7) | 29.2 | (0.7) | 11.3 | (0.5) | ||
| Other | 64.4 | (1.0) | 24.5 | (0.8) | 11.0 | (0.6) | ||
| Household Income | ||||||||
| <$20K/yr | 50.9 | (0.6) | 28.7 | (0.5) | 20.3 | (0.5) | 466 | <0.001 |
| $20-50K/yr | 55.7 | (0.4) | 27.3 | (0.4) | 17.0 | (0.3) | ||
| $50-75K/yr | 61.5 | (0.5) | 25.4 | (0.5) | 13.1 | (0.4) | ||
| >$75K/yr | 64.2 | (0.5) | 23.4 | (0.4) | 12.4 | (0.3) | ||
| Population Density | ||||||||
| Inside MSA2 | 58.8 | (0.3) | 25.8 | (0.3) | 14.9 | (0.2) | 57 | <0.001 |
| Not inside MSA | 54.4 | (0.5) | 28.3 | (0.4) | 19.6 | (0.4) | ||
Notes:
Experimenters are defined as those who have ever smoked cigarettes, but have smoked fewer than 100 in their lives. Smokers are those who have smoked 100 or more cigarettes and have also smoked in the past year.
Metropolitan statistical area.
Past-month Drinking by Smoking Status and Demographics
Past-month drinking quantity was grouped into five categories: No drinking at all, between 1 and 8 drinks, 9 to 20 drinks, 21-50 drinks and 50 or more drinks. Populations of these categories by demographic group are shown in Table 3. Overall, 25.3% of youths drank in the past month, roughly 10 percent had 8 or fewer drinks, and each of the three heavier drinking categories comprised about 5% of youths. Males and females were nearly equally represented among non-drinkers, though males exhibited a slight trend to drink more heavily. Drinking quantity rose sharply with age, with fewer than 1% of 12-14 year olds drinking more than 20 drinks in the past month, contrasted with 8.3% of 15-17 and more than 20% of 18-20 year olds. White youths were more likely than other racial and ethnic groups to report drinking, while Black youths were the least likely to report drinking. There was a slight trend toward more drinking for youths from the lowest income group, <$20,000 per year, and only trivial differences between youths within a metropolitan statistical area (MSA) and those outside of an MSA. As expected, smoking status was a very strong predictor of drinking behavior. For example, the prevalence of drinking more than 50 drinks in the past 30 days was 19% among smokers, contrasted with 5.7% among experimenters and only 0.6% among never-smokers.
Table 3.
Past-month Drinking Quantity, by Smoking and Demographic Group
|
None (N=41,368) |
1-8 Drinks (N=22,370) |
9-20 Drinks (N=3,974) |
21-50 Drinks (N=3,681) |
51+ Drinks (N=3,443) |
Chi-square Test |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | (SE) | % | (SE) | % | (SE) | % | (SE) | % | (SE) | χ2 | p | |
| Total (N=74,836) | 74.7 | (0.3) | 9.7 | (0.1) | 5.5 | (0.1) | 5.2 | (0.1) | 4.9 | (0.1) | ||
| Sex | ||||||||||||
| Male | 74.1 | (0.4) | 8.2 | (0.2) | 5.3 | (0.2) | 5.9 | (0.2) | 6.6 | (0.2) | 393 | <0.0001 |
| Female | 75.3 | (0.3) | 11.3 | (0.2) | 5.7 | (0.2) | 4.5 | (0.2) | 3.1 | (0.1) | ||
| Age | ||||||||||||
| 12-14 | 94.3 | (0.2) | 3.9 | (0.1) | 0.8 | (0.1) | 0.5 | (0.1) | 0.4 | (0.1) | 4245 | <0.0001 |
| 15-17 | 75.9 | (0.3) | 10.5 | (0.2) | 5.3 | (0.2) | 4.6 | (0.2) | 3.7 | (0.1) | ||
| 18-20 | 53.2 | (0.5) | 15.0 | (0.3) | 10.6 | (0.3) | 10.7 | (0.3) | 10.6 | (0.3) | ||
| Race/Ethnicity | ||||||||||||
| White | 70.4 | (0.3) | 10.4 | (0.2) | 6.4 | (0.1) | 6.5 | (0.2) | 6.3 | (0.2) | 1062 | <0.0001 |
| Black | 84.5 | (0.5) | 9.2 | (0.4) | 3.0 | (0.2) | 1.9 | (0.2) | 1.4 | (0.2) | ||
| Hispanic | 79.1 | (0.6) | 8.4 | (0.4) | 4.7 | (0.3) | 4.3 | (0.3) | 3.6 | (0.3) | ||
| Other | 82.4 | (0.8) | 7.8 | (0.5) | 4.1 | (0.5) | 3.1 | (0.3) | 2.6 | (0.3) | ||
| Household Income | ||||||||||||
| <$20K/yr | 70.9 | (0.7) | 9.7 | (0.3) | 6.3 | (0.3) | 6.6 | (0.3) | 6.5 | (0.3) | 111 | <0.0001 |
| $20-50K/yr | 77.0 | (0.4) | 9.6 | (0.3) | 4.9 | (0.2) | 4.4 | (0.2) | 4.2 | (0.2) | ||
| $50-75K/yr | 76.1 | (0.5) | 9.8 | (0.3) | 5.1 | (0.2) | 4.8 | (0.2) | 4.2 | (0.2) | ||
| >$75K/yr | 74.0 | (0.4) | 10.0 | (0.3) | 5.9 | (0.2) | 5.4 | (0.2) | 4.8 | (0.2) | ||
| Population Density | ||||||||||||
| Inside MSA | 74.8 | (0.3) | 9.8 | (0.2) | 5.6 | (0.1) | 5.2 | (0.1) | 4.6 | (0.1) | 18 | 0.0013 |
| Not inside MSA | 74.2 | (0.5) | 9.5 | (0.3) | 5.2 | (0.2) | 5.4 | (0.3) | 5.7 | (0.2) | ||
| Smoking Status | ||||||||||||
| Never-Smoker | 91.0 | (0.2) | 5.7 | (0.1) | 1.7 | (0.1) | 1.1 | (0.1) | 0.6 | (0.0) | 5345 | <0.0001 |
| Experimenter | 61.1 | (0.5) | 16.3 | (0.4) | 9.1 | (0.3) | 7.8 | (0.3) | 5.7 | (0.2) | ||
| Smoker | 38.2 | (0.6) | 13.7 | (0.4) | 13.3 | (0.4) | 15.9 | (0.5) | 19.0 | (0.5) | ||
Notes:
Metropolitan statistical area.
Prevalence and Univariate Predictors of Alcohol Use Disorder
Of the full sample, 9.5% (SE=0.2) of youths met criteria for past year alcohol use disorder, which is defined as alcohol abuse or dependence; this includes a 3.6% prevalence of alcohol dependence combined with a 5.9% prevalence of alcohol abuse only. Among the subset of youth who report any past-30 day drinking, 29.0% (SE=0.5) met diagnostic criteria for alcohol use disorder. The left-hand side Table 4 describes the univariate predictors of AUD among past-month drinkers, including smoking status, past-month drinking quantity, and demographic factors. In the univariate logistic models, smoking status is highly predictive of AUD. Compared with never-smokers, smokers had more than 4-fold higher odds of AUD and experimenters had over 2-fold higher odds. Age was inversely associated with AUD; the odds ratio for 12-14 year olds was 0.6, relative to 18-20 year-olds; 15-17 year olds were equivalent to their older counterparts in terms of AUD risk. Black youth were at substantially lower risk than Whites. Males were at 1.4-fold higher risk than females. Youths from households earning less than $20,000 per year were at slightly elevated odds for AUD; there were was no significant difference in AUD risk associated with living in a metropolitan area compared with living in a non-metropolitan area.
Table 4.
Univariate and Multivariate Logistic Regression Models for the Prediction of Alcohol use Disorder among Past-Month Drinkers (N=18,290).
| Univariate Models |
Multivariate Model |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male |
Female |
Combined |
Male |
Female |
Combined |
|||||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Smoking (vs. Never) | ||||||||||||
| Smoker | 4.0 | (3.3 - 4.8)! | 4.1 | (3.6 - 4.7)! | 4.1 | (3.6-4.7)! | 4.7 | (2.7-8.3)! | 4.3 | (2.6-7.0)! | 4.5 | (3.1-6.6)! |
| Experimenter | 2.2 | (1.8 - 2.7)! | 2.2 | (1.9 - 2.5)! | 2.2 | (1.9-2.5)! | 2.5 | (1.5-4.3)! | 2.3 | (1.5-3.7)! | 2.3 | (1.7-3.3)! |
| Log (Drinks) | 4.8 | (4.3 - 5.4)! | 6.0 | (5.2 - 6.8)! | 5.2 | (4.8-5.7)! | 8.4 | (5.8-12.3)!1 | 10.3 | (7.0-15.2)!2 | 9.1 | (6.9-11.8)!1 |
| Male (vs. Female) | ---- | ---------- | ---- | ---------- | 1.4 | (1.3-1.5)! | ---- | ---------- | ---- | ---------- | 1.0 | (0.9-1.1) |
| Age (vs. 18-20) | ||||||||||||
| 12-14 | 0.5 | (0.4 - 0.7)! | 0.9 | (0.7 - 1.1) | 0.6 | (0.5-0.8)! | 3.2 | (1.8-5.4)! | 2.8 | (1.6-4.9)! | 3.0 | (2.1-4.4)! |
| 15-17 | 0.8 | (0.7 - 0.9)‡ | 1.2 | (1.0 - 1.3)* | 1.0 | (0.9-1.1) | 2.3 | (1.5-3.4)! | 2.0 | (1.4-3.0)! | 2.2 | (1.7-2.9)! |
| Race (vs. White) | ||||||||||||
| Black | 0.6 | (0.5 - 0.8)! | 0.5 | (0.4 - 0.6)! | 0.6 | (0.5 - 0.7)! | 1.0 | (0.8-1.3) | 0.9 | (0.6-1.1) | 1.0 | (0.8-1.2) |
| Hispanic | 1.1 | (0.9 - 1.3) | 0.8 | (0.6 - 1.0) | 1.0 | (0.9 - 1.1) | 1.3 | (1.1-1.6)‡ | 0.9 | (0.7-1.2) | 1.2 | (1.0.-1.4) |
| Other | 1.1 | (0.8-1.5) | 1.1 | (0.8-1.4) | 1.1 | (0.9-1.3) | 1.4 | (1.0-1.9)* | 1.4 | (1.0-1.9)* | 1.4 | (1.1-1.8)‡ |
| Income (vs. >$75,00/Yr) | ||||||||||||
| <$20,000/yr | 1.3 | (1.1 - 1.6)! | 1.1 | (0.9 - 1.3) | 1.2 | (1.1-1.3)‡ | 1.2 | (1.0-1.5)‡ | 1.0 | (0.8-1.2) | 1.1 | (1.0-1.3) |
| $20,000-50,000/yr | 1.1 | (0.9 - 1.3) | 0.9 | (0.8 - 1.1) | 1.0 | (0.9-1.1) | 1.1 | (0.9-1.3) | 0.9 | (0.7-1.1) | 1.0 | (0.9-1.1) |
| $50,000-75,000/yr | 1.0 | (0.8 - 1.2) | 0.9 | (0.8 - 1.2) | 1.0 | (0.8-1.1) | 1.0 | (0.8-1.2) | 0.9 | (0.8-1.2) | 1.0 | (0.9-1.1) |
| MSA (vs. Non-MSA) | 1.0 | (0.9 - 1.1) | 0.9 | (0.8 - 1.0) | 0.9 | (0.8-1.0) | 1.1 | (1.0-1.3) | 0.9 | (0.8-1.1) | 1.0 | (0.9-1.2) |
Note:
p<0.001
p<0.01
p<0.05
Significant, negative interactions with smoking status and age (p<0.01).
Significant, negative interaction with smoking status. See text for more details on interaction parameters.
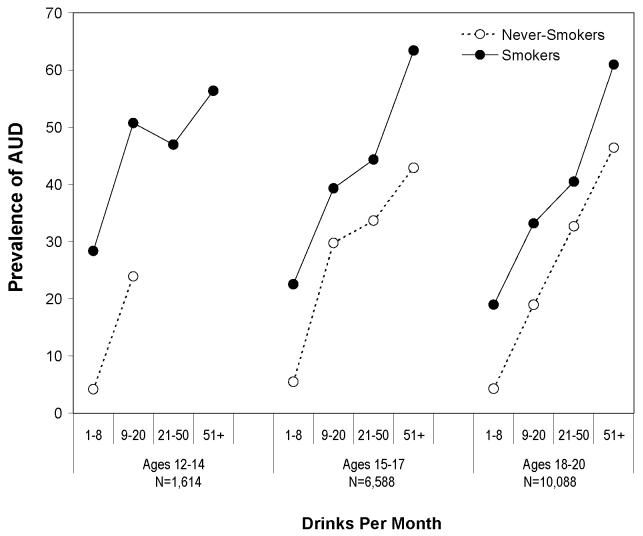
Smoking Status as a Predictor of AUD at Fixed Levels of Drinking
The relationship between drinking quantity and alcohol use disorder in is listed Table 4 as the odds ratio between AUD and the logarithm of the number of drinks consumed in the past-30 days. This relationship is explored in more detail in Figure 1, which contrasts the prevalence of AUD in smokers with the prevalence in never-smokers in each category of drinking quantity. Separate plots were generated for each of the three age groups -- two cells with fewer than 40 individuals were omitted from the analysis. For all groups, smokers had higher rates of AUD than never-smokers at any given quantity of drinking. Hence, even at low levels of alcohol use, youths who smoke have high rates of alcohol use disorder. For example, among youths who report 1-8 drinks in the past month, 28.4% of 12-14 year-old smokers met criteria for AUD, as well as 22.5% of 15-17 year-old smokers and 19.0% of 18-20 year-old smokers. In contrast, the prevalences of AUD for never-smokers in the same category of drinking quantity were 4.2%, 5.5%, and 4.3% respectively. Experimenters were omitted from the plots for clarity, but generally constituted an intermediate category between never-smokers and smokers.
Figure 1.
Prevalence of past-year alcohol use disorder among past-30 day drinkers. Prevalences for never smokers (Open Circles) and smokers (Filled Circles) are plotted as a function of past-month drinking quantity, stratified by age. Cells with fewer than 40 subjects were omitted from the analysis.
Multivariate Regression Model of AUD
The right-hand side of Table 4 summarizes the multivariate logistic regression model of AUD, predicted from demographic variables, smoking status, and past-month drinking quantity. Models were computed for males and females separately, and for the combined sample. In addition to the variables listed above, two-way interactions were tested between drinking quantity (logarithm of number of past-month drinks), smoking status, and age category, as these were the largest predictors in the univariate models. The smoking status by age category interaction did not reach significance, and so was not included in the final model, but the other two interactions were included. Results for all models are shown, though the male and female models exhibited few differences. To facilitate presentation of the results, we will focus on the combined sex model and only refer to single-sex models where important differences were observed.
Smoking status remained a substantial predictor of AUD, even after adjusting for drinking quantity and other variables, consistent with the results shown in Figure 1. Smokers were at 4.5-fold higher odds for AUD than non-smokers, with experimenters falling between the two groups. Younger age groups, though at lower overall risk for AUD in the univariate models, were at elevated risk after adjusting for drinking quantity, smoking status, and demographic characteristics. Family income was no longer a significant predictor in the multivariate model, and the protective effect observed for Black youth relative to Whites in the bivariate model was not present in the multivariate model. Likewise, males and females were at equal odds for AUD in the multivariate model. The differences associated with race, gender, and family income in the bivariate analyses are likely to be partially or fully attributable to differences in drinking behavior, which are accounted for in the multivariate model.
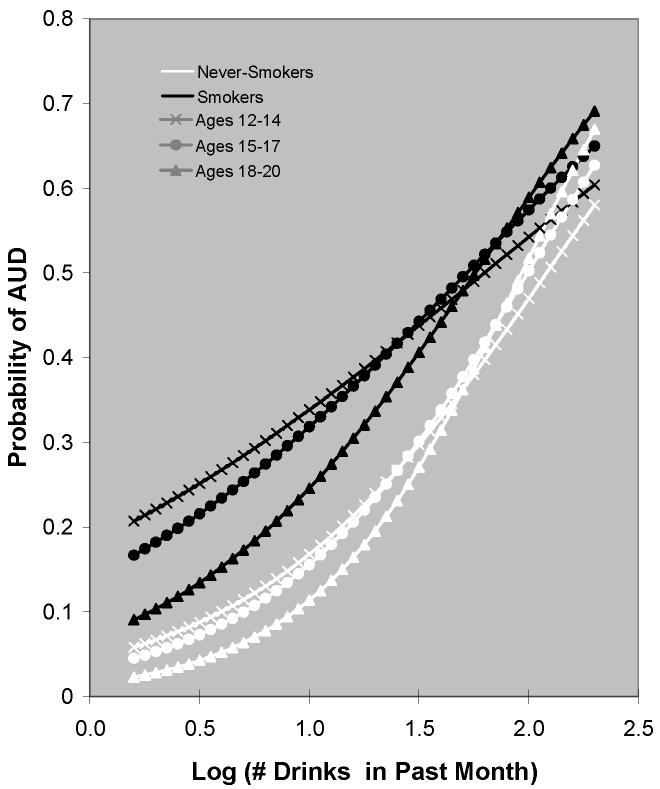
Age and smoking status both interacted with drinking quantity in the prediction of AUD for the combined gender (overall Wald-χ2= 10.5 and 11.2, respectively, both p<0.001) and male-only (Wald-χ2=5.7, 7.4, p=0.004 and p<0.001, respectively) models; only the interaction of smoking status with drinking quantity was significant in the female-only model. The interactions were all negative, indicating a lower slope between drinking quantity and AUD for smokers and for younger adolescents. As discussed in more detail below, this is a reflection of the elevated risk for smokers and for younger adolescents at low quantities of drinking (intercepts). In the combined gender model, the interaction odds ratio between drinking quantity and smoking category was 0.5 (95% CI 0.4-0.7) for smokers and 0.7 (95% CI: 0.5-0.9) for experimenters, relative to never-smokers. The interaction odds ratio between drinking quantity and age category was 0.6 (95% CI 0.4-0.8) for 12-14 year olds and 0.7 (95% CI: 0.6-0.8) for 15-17 year olds, relative to 18-20 year olds.
To dissect the contributions of the two significant statistical interactions to overall risk profiles, the probability of AUD was calculated as a function of past-month drinking quantity for smokers and never-smokers, stratified by age. These calculations were based on the odds ratios derived from the regression analyses described above; results are plotted in Figure 2. For clarity, the experimenter groups were omitted from this plot. At low levels of drinking, smokers are at higher risk than non-smokers and younger adolescents are at higher risk than older individuals. Differences in prevalence between smokers and never-smokers are especially prominent for younger age groups, resulting in very high risk for young smokers, even at low quantities of drinking. Differences between smokers and never-smokers and between younger and older subjects are diminished at higher levels of drinking. Hence, the lower slopes for smokers and younger adolescents in the AUD versus drinking quantity plot are offset by higher levels of AUD at low levels of drinking for these groups.
Figure 2.
Probability of Alcohol Use Disorder among past-30 day drinkers, predicted from regression analysis for smokers (black lines) and never-smokers (white lines). Probabilities are also stratified by age group: 12-14 (hashes), 15-17 (circles), and 18-20 (triangles).
Ancillary Analyses
In order to assess the robustness of the results to analytical decisions, we conducted two additional analyses. In the first, the decision made in the original analysis to count non-cigarette smoking tobacco users (i.e., those who only used cigars, pipes, or smokeless tobacco) as never-smokers was evaluated. The final multivariate regression model for the prediction of AUD was recomputed with these users excluded from the analyses (n=3,050 or 4.1% of the original sample). Odds ratio estimates were little changed from those listed Table 4, and in all cases were within the 95% CI of the original OR; for example, OR estimates were 5.0 for smokers (95% CI: 3.3-7.6) and 2.6 for experimenters (95% CI: 2.6-5.0). In the second analysis, the measure of past-30 day drinking quantity was replaced with past-year drinking frequency; i.e., the number of drinking days in the past year. Though this is a less precise measure because it assesses number of drinking days, but not number of drinks per drinking day, it reflects the time frame over which AUD was assessed. In this analysis, smokers and experimenters were still at elevated risk compared to never-smokers (OR=3.9; 95% CI: 2.4-6.4 and OR=2.6; 95% CI: 1.6-4.3, respectively). Likewise, younger adolescents were at elevated risk (12-14 year old vs. 18-20 year old: OR=2.2; 95% CI: 1.2-4.1; 15-17 year old vs. 18-20 year old: OR=3.1; 95% CI: 2.1-4.6) and drinking frequency exhibited significant, negative interactions with smoking status and age. Hence, the major findings of the analysis were robust to differences in exclusion criteria and choice of quantitative indicator of alcohol use.
Discussion
Among youth ages 12 to 20, 16% reported past-year smoking. Smokers reported substantially higher quantities of past-month drinking than either experimenters or never-smokers. Among those who reported drinking in the past month, smokers had 4-fold higher odds of past-year AUD, and experimenters had more than two-fold higher odds of past-year AUD. Hence, smokers have higher rates of heavy drinking and AUD than never-smokers. However, these differences were observed at all levels of drinking quantity and across all age categories. After adjusting for demographic variables and drinking quantity, the odds of past-year AUD among smokers remained more than 4-fold higher than those for never-smokers; likewise experimenters remained at more than 2-fold higher odds for AUD than never-smokers. Therefore, the connection between smoking and AUD cannot be attributed solely to heavier drinking among smokers.
Though AUD was a strong function of drinking quantity, this relationship was moderated by age and smoking status. Large differences in AUD prevalence between smokers and never-smokers, and between older and younger subjects, are observed at low levels of drinking. These differences diminish at higher levels of drinking. This results in negative interactions between drinking quantity and age, and between drinking quantity and smoking status. The combination of young age and smoking puts adolescent smokers at especially high risk for AUD, and this additional risk is most pronounced at comparatively low levels of drinking. In other words, among adolescents, young smokers are at substantially higher risk for AUD than their non-smoking counterparts who drink comparable quantities.
The finding of high levels of AUD at low levels of drinking for adolescent smokers is reminiscent of the work of Kandel and Chen, relating smoking quantity to symptoms of nicotine dependence. In particular, they reported that adolescents had higher rates of nicotine dependence than adults at equivalent levels of smoking. Likewise, females exhibited higher rates of nicotine dependence than males at equivalent smoking quantities. These authors hypothesized that different rates of dependence at equivalent levels of use reflected differential sensitivity to nicotine, though they emphasized that this hypothesis requires further testing (Kandel and Chen, 2000). We have taken a complementary approach by examining use of one substance as a risk factor for addiction to another substance at equivalent levels of use of the second substance. Moreover, we have focused on adolescents only, so that a finer-grained examination of age trends within this important period of risk for AUD could be carried out. We reiterate the hypothetical nature of the interpretation of higher levels of dependence at equivalent levels of use as a reflection of heightened sensitivity to the substance (alcohol, in our case).
Assuming that elevated susceptibility to AUD at equivalent quantities of drinking is truly indicative of pharmacological sensitivity to alcohol, it remains to be determined whether adolescent smoking has a causal effect on that sensitivity, or whether it is an indicator of preexisting vulnerability. There may be other unmeasured or unanalyzed variables that mediate this association, including genetic factors. Adolescent smoking may be an indicator of genetic predisposition to AUD, and other unknown factors may contribute to both outcomes. That is, genetic or other factors involved in the initiation of adolescent smoking may also play a role in the development of alcohol abuse and dependence. However, these mechanisms are not mutually exclusive. That is, smoking may be both an indicator of pre-existing vulnerability to AUD and may also have a pharmacological influence on response to alcohol that modulates susceptibility to AUD.
There is abundant evidence from animal studies that nicotine impacts the adolescent central nervous system in such a manner as to increase vulnerability to addiction and that such effects are unique to adolescence (Adriani and Laviola, 2004). For example, in adolescent rat models, nicotine effects on gene expression and brain development are more deleterious than those observed in adults (Trauth et al., 1999). Additionally, adolescent rats exposed to nicotine become sensitized to the behavioral effects of subsequent cocaine exposure, suggesting that nicotine may alter future behavioral response to other drugs, thereby increasing vulnerability to alcohol and other drug use disorders (Collins and Izenwasser, 2004; McMillen et al., 2005). Thus, adolescent nicotine exposure in animals results in persistent neurobiological changes that may influence the reinforcing effects of multiple drugs of abuse (McMillen et al., 2005; Trauth et al., 2001; Trauth et al., 2000). Such observations have led to the proposal that nicotine may act as a “neurochemical gateway” to more serious substance abuse (Kelley and Rowan, 2004). However, it remains to be determined whether the well-documented effects of nicotine exposure on adolescent brain development in animals extend to humans.
Despite our inability to determine a precise mechanism by which the association between adolescent smoking and AUD takes place, these findings add to the large number of documented deleterious health effects associated with smoking, particularly among young people. Additionally, these results suggest that understanding the role of cigarette smoking in the development of alcohol dependence and other addictions could yield substantial public health benefits. If it is found that nicotine influences risk for AUD via direct pharmacological effects on brain development akin to those seen in animal models, a powerful message could be added to adolescent health education programs; namely, that smoking in adolescence poses tangible risks for the brain in addition to other well-known risks for physical health.
Among the limitations of this study is the use of self-reported data for substance use and abuse, which could introduce reporting bias as a confounding variable. The absence of longitudinal data represents an additional limitation; closely spaced longitudinal data on drinking quantity, smoking, and AUD on a representative sample of adolescents would allow for testing of a variety of causal models. However, very large samples would be required conduct analyses similar to those presented here. Accordingly, a major strength of this study is the large sample size, which provided the necessary statistical power to analyze the complex relationship between smoking, drinking quantity, and AUD in adolescence. Additional strengths are the representativeness of the sample and the availably of past-year diagnostic data directly from adolescent participants, rather than reliance on longer-term retrospective data from adults.
Summary
Adolescent smokers are more likely to drink and are at substantially elevated risk for alcohol use disorders than their never-smoking counterparts. This association remains even after adjusting for quantity of alcohol use, using either stratification or regression approaches. Moreover, the vulnerability to AUD is especially pronounced among younger smokers. Hence, smoking is not only an indicator of heavier drinking, but is associated with vulnerability to AUD even when accounting for drinking behaviors.
Acknowledgements
The Author's are grateful to Mr. Joe Gfroerer (SAMHSA-OAS), Dr. Tom Przybeck (Washington University), and Dr. Lewis R. Goldberg (Oregon Research Institute) for valuable comments on the manuscript).
Funding: Analysis and manuscript preparation were supported by NIH-K01DA16618 (RAG), NIH-U10AA08401 (LJB), and NIH-P01CA089392 (LJB). The NSDUH was sponsored by the Substance Abuse and Mental Health Services Administration, Office of Applied Studies (SAMHSA-OAS); field work was conducted by RTI, International. NSDUH data was obtained from the Substance Abuse and Mental Health Data Archive through the Inter-university Consortium for Political and Social Research (http://www.icpsr.umich.edu/SAMHDA).
5. References
- Adriani W, Laviola G. Windows of vulnerability to psychopathology and therapeutic strategy in the adolescent rodent model. Behav Pharmacol. 2004;15(56):341–352. doi: 10.1097/00008877-200409000-00005. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. American Psychiatric Association; Washington, D.C.: 2000. Text Revision. [Google Scholar]
- Arday DR, Giovino GA, Schulman J, Nelson DE, Mowery P, Samet JM. Cigarette smoking and self-reported health problems among U.S. high school seniors, 1982-1989. Am J Health Promot. 1995;10(2):111–116. doi: 10.4278/0890-1171-10.2.111. [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux MC, Mick E, Wilens TE, Fontanella JA, Poetzl KM, Kirk T, Masse J, Faraone SV. Is Cigarette Smoking a Gateway to Alcohol and Illicit Drug Use Disorders? A Study of Youths with and without Attention Deficit Hyperactivity Disorder. Biol Psychiatry. 2005;59(3):258–264. doi: 10.1016/j.biopsych.2005.07.009. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL. Smoking cessation in young adults: Age at initiation of cigarette smoking and other suspected influences. Am J Public Health. 1996;86(2):214–220. doi: 10.2105/ajph.86.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castrucci BC, Gerlach KK, Kaufman NJ, Orleans CT. Adolescents' acquisition of cigarettes through noncommercial sources. J Adolesc Health. 2002;31(4):322–326. doi: 10.1016/s1054-139x(02)00393-2. [DOI] [PubMed] [Google Scholar]
- Chen K, Kandel DB. The natural history of drug use from adolescence to the mid-thirties in a general population sample. Am J Public Health. 1995;85(1):41–47. doi: 10.2105/ajph.85.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K, Kandel D. Relationship between extent of cocaine use and dependence among adolescents and adults in the United States. Drug Alcohol Depend. 2002;68(1):65–85. doi: 10.1016/s0376-8716(02)00086-8. [DOI] [PubMed] [Google Scholar]
- Chen X, Unger JB, Palmer P, Weiner MD, Johnson CA, Wong MM, Austin G. Prior cigarette smoking initiation predicting current alcohol use: Evidence for a gateway drug effect among California adolescents from eleven ethnic groups. Addict Behav. 2002;27(5):799–817. doi: 10.1016/s0306-4603(01)00211-8. [DOI] [PubMed] [Google Scholar]
- Collins SL, Izenwasser S. Chronic nicotine differentially alters cocaine-induced locomotor activity in adolescent vs. adult male and female rats. Neuropharmacology. 2004;46(3):349–362. doi: 10.1016/j.neuropharm.2003.09.024. [DOI] [PubMed] [Google Scholar]
- Dani JA, Harris RA. Nicotine addiction and comorbidity with alcohol abuse and mental illness. Nat Neurosci. 2005;8(11):1465–1470. doi: 10.1038/nn1580. [DOI] [PubMed] [Google Scholar]
- DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: A risk factor for the development of alcohol disorders. Am J Psychiatry. 2000;157(5):745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- Dinn WM, Aycicegi A, Harris CL. Cigarette smoking in a student sample: Neurocognitive and clinical correlates. Addict Behav. 2004;29(1):107–126. doi: 10.1016/j.addbeh.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Swain-Campbell NR, Horwood LJ. Deviant peer affiliations, crime and substance use: A fixed effects regression analysis. J Abnorm Child Psychol. 2002;30(4):419–430. doi: 10.1023/a:1015774125952. [DOI] [PubMed] [Google Scholar]
- Grant BF. Age at smoking onset and its association with alcohol consumption and DSMIV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse. 1998;10(1):59–73. doi: 10.1016/s0899-3289(99)80141-2. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61(11):1107–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Jensen JA, Hickman NJ, 3rd, Landrine H, Klonoff EA. Availability of tobacco to youth via the Internet. JAMA. 2004;291(15):1837. doi: 10.1001/jama.291.15.1837. [DOI] [PubMed] [Google Scholar]
- John U, Meyer C, Rumpf HJ, Hapke U. Smoking, nicotine dependence and psychiatric comorbidity--a population-based study including smoking cessation after three years. Drug Alcohol Depend. 2004;76(3):287–295. doi: 10.1016/j.drugalcdep.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Kandel D. Stages in adolescent involvement in drug use. Science. 1975;190(4217):912–914. doi: 10.1126/science.1188374. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Chen K. Extent of smoking and nicotine dependence in the United States: 1991-1993. Nicotine Tob Res. 2000;2(3):263–274. doi: 10.1080/14622200050147538. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Yamaguchi K, Chen K. Stages of progression in drug involvement from adolescence to adulthood: Further evidence for the gateway theory. J Stud Alcohol. 1992;53(5):447–457. doi: 10.15288/jsa.1992.53.447. [DOI] [PubMed] [Google Scholar]
- Kelley BM, Rowan JD. Long-term, low-level adolescent nicotine exposure produces dose-dependent changes in cocaine sensitivity and reward in adult mice. Int J Dev Neurosci. 2004;22(56):339–348. doi: 10.1016/j.ijdevneu.2004.04.002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopstein AN, Crum RM, Celentano DD, Martin SS. Sensation seeking needs among 8th and 11th graders: Characteristics associated with cigarette and marijuana use. Drug Alcohol Depend. 2001;62(3):195–203. doi: 10.1016/s0376-8716(00)00170-8. [DOI] [PubMed] [Google Scholar]
- Lai S, Lai H, Page JB, McCoy CB. The association between cigarette smoking and drug abuse in the United States. J Addict Dis. 2000;19(4):11–24. doi: 10.1300/J069v19n04_02. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Brown RA. Level of current and past adolescent cigarette smoking as predictors of future substance use disorders in young adulthood. Addiction. 1999;94(6):913–921. doi: 10.1046/j.1360-0443.1999.94691313.x. [DOI] [PubMed] [Google Scholar]
- McMillen BA, Davis BJ, Williams HL, Soderstrom K. Periadolescent nicotine exposure causes heterologous sensitization to cocaine reinforcement. Eur J Pharmacol. 2005;509(23):161–164. doi: 10.1016/j.ejphar.2005.01.002. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Prescott CA, Kendler KS. Age at first drink and risk for alcoholism: A noncausal association. Alcohol Clin Exp Res. 1999;23(1):101–107. [PubMed] [Google Scholar]
- Ribisl KM, Williams RS, Kim AE. Internet sales of cigarettes to minors. JAMA. 2003;290(10):1356–1359. doi: 10.1001/jama.290.10.1356. [DOI] [PubMed] [Google Scholar]
- RTI International . SUDAAN Language Manual, Release 9.0. Research Triangle Institute; Research Triangle Park, NC: 2004. [Google Scholar]
- Schenk S. Sensitization as a process underlying the progression of drug use via gateway drugs. In: Kandel D, editor. Stages and Pathways of Drug Involvement. Cambridge University Press; Cambridge, UK: 2002. pp. 318–336. [Google Scholar]
- Siqueira LM, Brook JS. Tobacco use as a predictor of illicit drug use and drug-related problems in Colombian youth. J Adolesc Health. 2003;32(1):50–57. doi: 10.1016/s1054-139x(02)00534-7. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2002 National Survey on Drug Use and Health: National Findings. Office of Applied Studies; Rockville, MD: 2003. (NHSDA Series H-22, DHHS Publication No. SMA 03-3836). [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Overview of Findings from the 2003 National Survey on Drug Use and Health. Office of Applied Studies; Rockville, MD: 2004. (NSDUH Series H–24, DHHS Publication No. SMA 04–3963). [Google Scholar]
- Torabi MR, Bailey WJ, Majd-Jabbari M. Cigarette smoking as a predictor of alcohol and other drug use by children and adolescents: Evidence of the “gateway drug effect”. J Sch Health. 1993;63(7):302–306. doi: 10.1111/j.1746-1561.1993.tb06150.x. [DOI] [PubMed] [Google Scholar]
- Trauth JA, Seidler FJ, Ali SF, Slotkin TA. Adolescent nicotine exposure produces immediate and long-term changes in CNS noradrenergic and dopaminergic function. Brain Res. 2001;892(2):269–280. doi: 10.1016/s0006-8993(00)03227-3. [DOI] [PubMed] [Google Scholar]
- Trauth JA, Seidler FJ, McCook EC, Slotkin TA. Adolescent nicotine exposure causes persistent upregulation of nicotinic cholinergic receptors in rat brain regions. Brain Res. 1999;851(12):9–19. doi: 10.1016/s0006-8993(99)01994-0. [DOI] [PubMed] [Google Scholar]
- Trauth JA, Seidler FJ, Slotkin TA. An animal model of adolescent nicotine exposure: Effects on gene expression and macromolecular constituents in rat brain regions. Brain Res. 2000;867(12):29–39. doi: 10.1016/s0006-8993(00)02208-3. [DOI] [PubMed] [Google Scholar]
- U. S. Department of Health and Human Services Preventing tobacco use among youg people: A report of the Surgeon General. 1994 [Google Scholar]
- Wills TA, Cleary SD. Peer and adolescent substance use among 6th-9th graders: Latent growth analyses of influence versus selection mechanisms. Health Psychol. 1999;18(5):453–463. doi: 10.1037//0278-6133.18.5.453. [DOI] [PubMed] [Google Scholar]
- Wortley PM, Husten CG, Trosclair A, Chrismon J, Pederson LL. Nondaily smokers: A descriptive analysis. Nicotine Tob Res. 2003;5(5):755–759. doi: 10.1080/1462220031000158753. [DOI] [PubMed] [Google Scholar]
- Wright D, Barker P, Gfroerer J, Piper L. Summary of NHSDA Design Changes in 1999. In: Gfroerer J, Eyerman J, Chromy J, editors. Redesigning and Ongoing National Household Survey: Methodological Issues. Substance Abuse and Mental Health Services Administration, Office of Applied Studies; Rockville, MD: 2002. (DHHS Publication No. SMA 03-3768). [Google Scholar]