Abstract
This article discusses the use of image guided endovascular stenting to treat obstruction of the superior vena cava
The patient
A 59 year old woman with a history of recurrent left sided breast cancer presented in October 2004 with bilateral arm and neck swelling, increasing shortness of breath, and headaches. We made a working diagnosis of obstruction of the superior vena cava. She had undergone surgery and external beam radiotherapy 13 years before for primary breast cancer. She subsequently underwent left mastectomy and chemotherapy for reoccurrence in 2000.
What is the next investigation?
Superior vena cava obstruction is usually diagnosed clinically, with the patient presenting with signs and symptoms related to venous congestion (box 1). Chest radiography usually demonstrates the abnormality with a widened mediastinum, although this may be normal.1
Box 1 Signs and symptoms associated with obstruction of the superior vena cava2 3 4
Early signs and symptoms
Signs
Dilatation of the neck, arm, and chest wall veins
Oedema of the upper body, extremities, and face
Symptoms
Cough and haemoptysis
Dysphagia
Chest pain
Dyspnoea
Late signs and symptoms
Signs
Severe respiratory distress
Cyanosis
Engorged conjunctiva
Convulsions and coma
Symptoms
Severe headache and feelings of “tension in the head”—worse in the morning and on bending down
Visual disturbance
Contrast enhanced computed tomography is the most commonly performed diagnostic imaging test. With multiplanar reformatting, this test allows accurate diagnosis and can show the extent, level, and cause of superior vena cava obstruction. The presence of dilated collateral vessels is highly suggestive of superior vena cava obstruction, with a sensitivity of 96% and specificity of 92%.5 6 7 Before the widespread use of computed tomography, upper limb venography was used to determine the level and extent of superior vena cava obstruction. However, it does not identify the cause of the obstruction and can overestimate the extent of venous occlusion as a result of shunting of blood through collaterals. Magnetic resonance venography is an alternative investigation that is increasingly being used. It has 100% sensitivity, specificity, and accuracy to assess large central veins.8 9 Contraindications include claustrophobia and the presence of a permanent cardiac pacemaker.
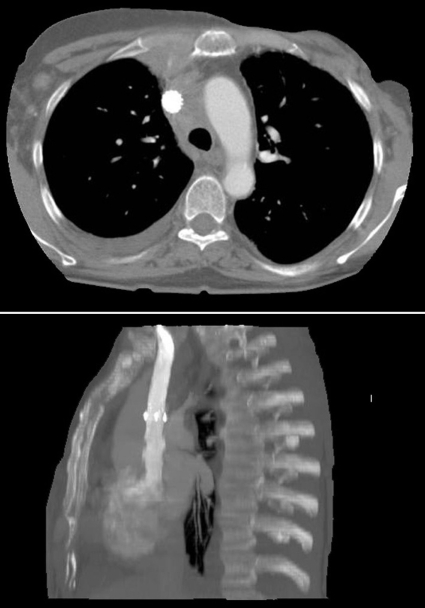
In our case, chest radiography confirmed the presence of a superior mediastinal mass. The patient underwent contrast enhanced computed tomography (fig 1), with the contrast medium injected into the right arm. Axial images showed large metastatic nodes encasing and narrowing the superior vena cava, resulting in a short tight stenosis of this vessel (fig 1).
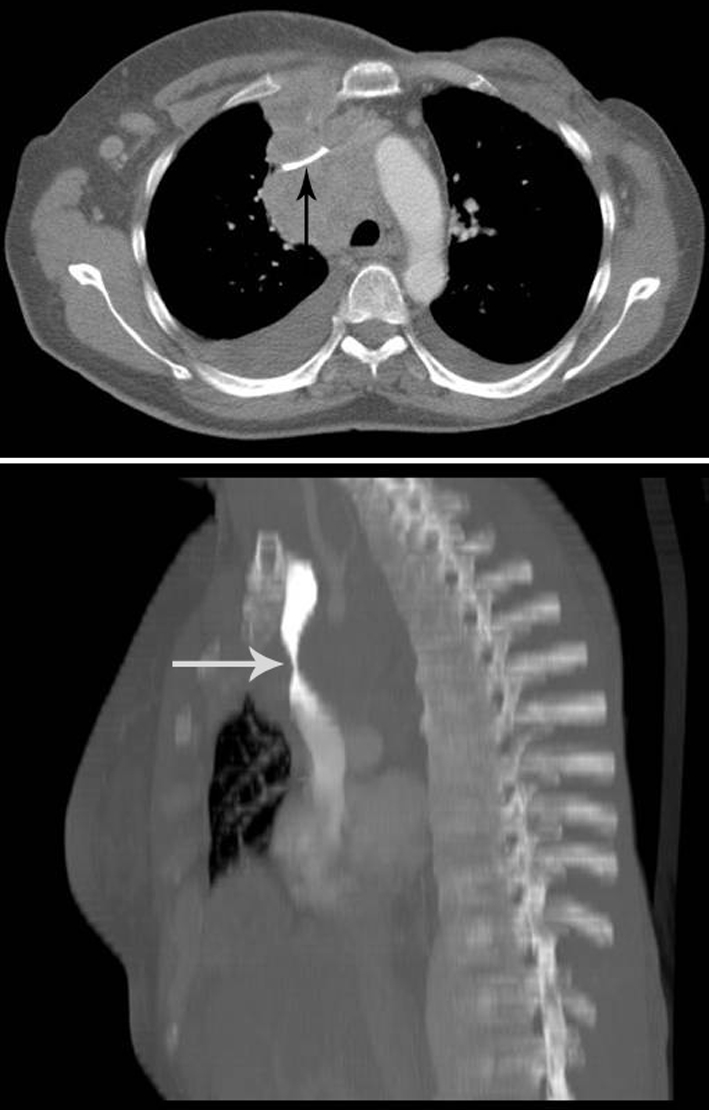
Fig 1 Contrast enhanced computed tomography in October 2004 shows enlarged mediastinal nodes with significant focal narrowing of the superior vena cava (top; arrow). Contrast enhanced computed tomography, with reconstruction using maximum intensity projection in the sagittal plane, shows focal narrowing of the superior vena cava (bottom; arrow)
The aim of treatment is to alleviate the patient’s symptoms and to treat the underlying cause (box 2). Placement of a percutaneous stent is the quickest way to relieve symptoms in most patients with superior vena cava obstruction secondary to malignancy. It does not affect the ability to deliver radiotherapy or chemotherapy. The exception is patients who have tumours, such as small cell lung cancer or lymphoma, that are highly responsive to other treatments. Surgical intervention involves thoracotomy but is rarely performed in patients with a malignant cause of obstruction because of the high morbidity and mortality. Medical management has almost no role in treating symptomatic superior vena cava obstruction of benign origin. Anti-inflammatory agents such as steroids do not usually help, so stenting or surgery are the only options.
Box 2 Treatment options
Chemotherapy
External beam radiotherapy
Endovascular stenting
Open surgical reconstruction
Medical management (for example, hormonal treatment)
The decision
Because our patient had already had two courses of chemotherapy for breast cancer with poor response and high toxicity, further chemotherapy was not thought appropriate. The recurrence was within her previous radiation field so further radiotherapy was not considered an option. Bypass surgical reconstruction was not considered appropriate. Surgical treatment is usually reserved for treatment of non-malignant causes of superior vena cava obstruction.10 11
The patient’s breast cancer was oestrogen receptor and progesterone receptor positive but human epidermal growth factor receptor 2 (HER2) negative and could therefore not be treated with herceptin. She was already on tamoxifen when she developed early signs and symptoms of superior vena cava obstruction with oedema of the upper extremities and face, superficial vein dilatation, and associated dyspnoea. She was started on a trial of hormonal treatment with Arimidex but responded poorly, and after two months she became increasingly symptomatic, with advanced signs of superior vena cava obstruction including headache, cyanosis, engorged conjunctiva, and severe respiratory distress.
After discussion with the referring oncologist, the patient chose to undergo endovascular stenting for rapid relief of the obstruction. She gave fully informed consent and accepted the risk of complications, including stent occlusion and migration.
The procedure
We performed the procedure in the radiology vascular operating theatre using X ray guidance under local anaesthetic. The tight stenosis in the superior vena cava was transversed with a catheter and guide wire via a right retrograde venous approach from the common femoral vein, and venography was performed. This showed high grade focal stenosis of the superior vena cava (fig 2). A 14 mm × 10 cm self expanding nitinol stent was released across the stenosis and then dilated with a 12 mm balloon. The patient received 5000 IU of heparin intravenously during the procedure. Dilatation of the stricture can be transiently painful and analgesia is often needed. Venography performed after the procedure showed good flow through an expanded stent. The patient experienced dramatic and immediate relief of symptoms and was discharged home the same day. This improvement was maintained for the next three years.
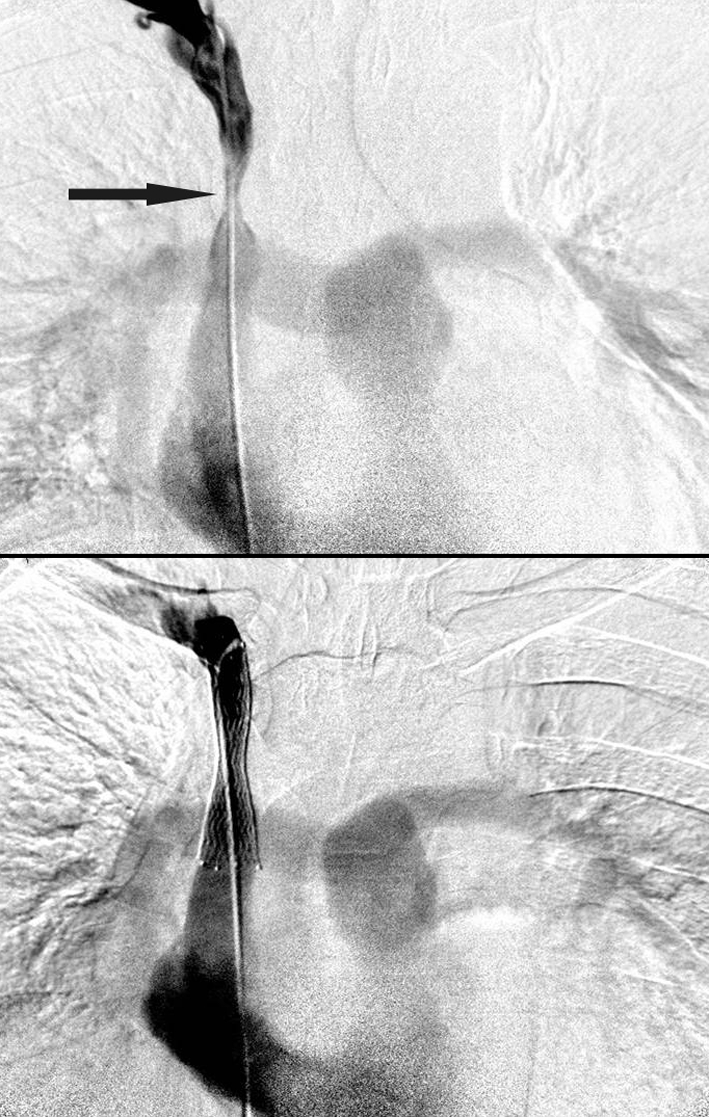
Fig 2 Digital subtraction venogram from a femoral vein approach shows tight focal stenosis of the mid superior vena cava (top; arrow). Digital subtraction venography after placement of a self expanding nitinol 14 mm stent, which was later dilated to 12 mm, shows good flow through the stent at the end of the procedure (bottom)
Contrast enhanced computed tomography performed three years later (fig 3) showed a patent stent with excellent flow. The patient died three years and two months after stent insertion from generalised metastatic disease (liver and bone metastases) but remained symptom free from the obstruction.
Fig 3 Contrast enhanced computed tomography in November 2007 (top). Three years after stent insertion, the patency of the stent is still good. Three dimensional reconstruction (maximum intensity projection) in the sagittal plane three years after stent insertion shows a widely patent stent (bottom)
Superior vena caval stenting
Superior vena caval stenting is an image guided technique that restores the venous return in patients with superior vena cava obstruction. The stent is placed via the internal jugular, subclavian vein, or common femoral vein, under local anaesthetic. A guide wire is manipulated through the stenosis or obstruction to guide and stabilise the insertion and to deploy the metallic stent across the lesion. It is usually sufficient to achieve in line flow on one side only to relieve symptoms. The National Institute for Health and Clinical Excellence (NICE) has issued guidance in support of this procedure. The guidance states that stenting is an accepted treatment for immediate restoration of venous flow, which has low complication rates and high patency rates.12
Benefit
Most cases of superior vena cava obstruction (>85%) are secondary to underlying malignancy—lung cancer then lymphoma are the most common causes.2 However, an increasing number of patients have benign disease secondary to long term indwelling central venous catheters or cardiac procedures.13 Systematic review of different treatment options for superior vena cava obstruction in patients with lung cancer found that endovascular stenting improved symptoms in 95% of cases; 11% of patients relapsed, usually because of thrombosis or tumour in-growth in the stent. This is superior to chemotherapy and radiotherapy, which have response rates of 84% and 78% and relapse rates of 17% and 19% for small cell lung cancer and non-small cell lung cancer, respectively.3 A comparison of percutaneous self expanding stent insertion with external beam radiotherapy suggests that stent insertion fulfils the requirements of a palliative procedure significantly better than radiotherapy and should be the first choice.14 Box 3 summarises the indications and contraindications for superior vena caval stenting
Indications and contraindications for superior vena cava stenting3 10 11
Indications
Patients with symptomatic superior vena cava obstruction who have malignant disease and a short to medium life expectancy, either at the initial presentation or after failed chemotherapy or radiotherapy
Patients with symptomatic superior vena cava obstruction secondary to benign disease
Contraindications (relative)
Patient is asymptomatic
Patient cannot lie flat or semi-supine on the table
Patients with malignant disease that has a good chance of cure or remission (such as lymphoma or germ cell tumour) should be treated with chemotherapy or radiotherapy first. Stenting should be reserved for treatment failure with these modalities
Endovascular stenting usually relieves symptoms within 0-72 hours, whereas chemotherapy or radiotherapy can take up to two weeks. This greatly improves the quality of life of patients, who usually have a short life expectancy. Stents do not interfere with subsequent radiotherapy or chemotherapy.10 In view of this, early stenting is advised for rapid relief of symptoms.2 14 15
The cost of stents varies but is around £550 (€700; $1000). This may be prohibitive in healthcare communities with severe financial constraints, but we think that the improved quality of life is worth the cost. Scoring systems that correlate clinical grading and radiological grading of severity of obstruction may help identify patients most likely to benefit from stent placement.16
Complications
The main complication reported is stent occlusion caused by tumour in-growth or thrombosis. However, most patients with superior vena cava obstruction secondary to malignancy have a short life expectancy and the stent remains patent until death. If stent thrombosis does occur, occlusion rates are lower than with alternative treatments.17 18 In addition, stent occlusion can be treated with thromboaspiration, thrombolysis, or further stent insertion, and secondary patency rates are good.10 3 Other complications reported include transient chest pain, infection, misplaced stent, stent migration, and pulmonary emboli, although fortunately these are rare. Stent migration may occur as a result of inappropriate placement or an imperfect fixing site within the superior vena cava.19 Perforation or rupture of the vein, requiring emergency surgery, is a potential but extremely rare risk.
Using thrombolytic agents as adjuvants to stent placement is associated with increased morbidity.3 These agents increase the risk of haematoma, gastrointestinal haemorrhage, haemoptysis, and epistaxis.17 18 However, superior vena cava thrombosis is not a contraindication to stent placement, and mechanical thrombectomy—with or without thrombolysis—and subsequent stent placement should be considered in these circumstances.
Questions for further research
Most of the evidence for superior vena cava stenting comes from non-randomised trials in individual centres and case series with small numbers of patients, so no level 1 or level 2 evidence exists. But because it provides such rapid and dramatic relief of symptoms it has become standard of care, and most clinicians think that a randomised trial of stent versus no stent is not justified. Questions remain, however, about the optimal time to insert the stent—whether at time of diagnosis, as a replacement or supplement to radiotherapy or chemotherapy, or after failure of these modalities.
No evidence based protocols on the use of anticoagulation after stent placement are available. There is some limited evidence for the use of anticoagulants—such as aspirin, warfarin, or low molecular weight heparin—from one month to longer term.20 Our policy is not to anticoagulate patients without evidence of central vein thrombosis. However, in patients with central venous thrombosis we advise long term anticoagulation with warfarin, even after successful thrombolysis.
Learning points
Superior vena cava obstruction can be asymptomatic but often the symptoms are distressing
Most (>85%) superior vena cava obstruction is secondary to malignancy, most often lung cancer
Endovascular stenting is a safe and effective minimally invasive technique for treating symptomatic superior vena cava obstruction
Stenting usually provides instant symptom relief, which is usually more complete than that seen with radiotherapy or chemotherapy
Endovascular stenting should be considered as first line treatment for obstruction with a malignant cause in patients with a short to medium life expectancy. It does not treat the underlying cause or interfere with its treatment
Symptoms may recur, usually as a result of thrombotic occlusion of the stent. This can be treated with thrombolysis or further coaxial stent placement
Contributors: AFW performed the procedure on the patient and is a coauthor and guarantor; TNY is also a coauthor; CF did the literature review.
Competing interests: AFW is a clinical adviser to Biocompatibles UK.
Provenance and peer review: Commissioned; externally peer reviewed.
Patient consent not required (patient anonymised, dead, or hypothetical).
This series provides an update on the best use of different imaging methods for common or important clinical presentations. The series advisers are Fergus Gleeson, consultant radiologist, Churchill Hospital, Oxford, and Kamini Patel, consultant radiologist, Homerton University Hospital, London.
References
- 1.Parish JM, Marschke RF Jr, Dines DE, Lee RE. Etiologic considerations in superior vena cava syndrome. Mayo Clin Proc 1981;56:407-13. [PubMed] [Google Scholar]
- 2.Ostler PJ, Clarke DP, Watkinson AF, Gaze MN. Superior vena cava obstruction: a modern management strategy. Clin Oncol (R Coll Radiol) 1997;9:83-9. [DOI] [PubMed] [Google Scholar]
- 3.Rowell NP, Gleeson FV. Steroids, radiotherapy, chemotherapy and stents for superior vena caval obstruction in carcinoma of the bronchus: a systematic review. Clin Oncol 2002;14:338-51. [DOI] [PubMed] [Google Scholar]
- 4.Rice TW, Rodriguez RM, Light RW. The superior vena cava syndrome: clinical characteristics and evolving etiology. Medicine (Baltimore) 2006;85:37-42. [DOI] [PubMed] [Google Scholar]
- 5.Bechtold RE, Wolfman NT, Karstaedt N, Choplin RH. Superior vena caval obstruction: detection using CT. Radiology 1985;157:485-7. [DOI] [PubMed] [Google Scholar]
- 6.Kim HJ, Kim HS, Chung SH. CT diagnosis of superior vena cava syndrome: importance of collateral vessels. AJR Am J Roentgenol 1993;161:539-42. [DOI] [PubMed] [Google Scholar]
- 7.Eren S, Karaman A, Okur A. The superior vena cava syndrome caused by malignant disease. Imaging with multi-detector row CT. Eur J Radiol 2006;59:93-103. [DOI] [PubMed] [Google Scholar]
- 8.Lin J, Zhou KR, Chen ZW, Wang JH, Yan ZP, Wang YX. Vena cava 3D contrast-enhanced MR venography: a pictorial review. Cardiovasc Intervent Radiol 2005;28:795-805. [DOI] [PubMed] [Google Scholar]
- 9.Thornton MJ, Ryan R, Varghese JC, Farrell MA, Lecey B, Lee MJ. A three-dimensional gadolinium-enhanced MR venography technique for imaging central veins. AJR Am J Roentgenol 1999;173:999-1003. [DOI] [PubMed] [Google Scholar]
- 10.Lanciego C, Chacón JL, Julián A, Andrade J, López L, Martinez B, et al. Stenting as first option for endovascular treatment of malignant superior vena cava syndrome. AJR Am J Roentgenol 2001;177:585-93. [DOI] [PubMed] [Google Scholar]
- 11.Kalra M, Gloviczki P, Andrews JC, Cherry KJ Jr, Bower TC, Panneton JM, et al. Open surgical and endovascular treatment of superior vena cava syndrome caused by nonmalignant disease. J Vasc Surg 2003;38:215-23. [DOI] [PubMed] [Google Scholar]
- 12.National Institute for Health and Clinical Excellence. Stent placement for vena caval obstruction. IPG79. 2004www.nice.org.uk/page.redirect?o=IP_152
- 13.Chee CE, Bjarnason H, Prasad A. Superior vena cava syndrome: an increasingly frequent complication of cardiac procedures. Nat Clin Pract Cardiovasc Med 2007;4:226-30. [DOI] [PubMed] [Google Scholar]
- 14.Smayra T, Otal P, Chabbert V, Chemla P, Romero M, Joffre F, et al. Long-term results of endovascular stent placement in the superior caval venous system. Cardiovasc Intervent Radiol 2001;24:388-94. [DOI] [PubMed] [Google Scholar]
- 15.Nicholson AA, Ettles DF, Arnold A, Greenstone M, Dyet JF. Treatment of malignant superior vena cava obstruction: metal stents or radiation therapy. J Vasc Intervent Radiol 1997;8:781-8. [DOI] [PubMed] [Google Scholar]
- 16.Plekker D, Ellis T, Irusen EM, Bolliger CT, Diacon AH. Clinical and radiological grading of superior vena cava obstruction. Respiration 2007. Sep 25 [Epub ahead of print]. [DOI] [PubMed]
- 17.Crowe MT, Davies CH, Gaines PA. Percutaneous management of superior vena cava occlusions. Cardiovasc Intervent Radiol 1995;18:367-72. [DOI] [PubMed] [Google Scholar]
- 18.Kee S, Kinoshita L, Razavi MK, Nyman UR, Semba CP, Dake MD. Superior vena cava syndrome: treatment with catheter directed thrombolysis and endovascular stent placement. Radiology 1998;206:187-93. [DOI] [PubMed] [Google Scholar]
- 19.Entwisle KG, Watkinson AF, Reidy J. Case report: migration and shortening of a self-expanding metallic stent complicating the treatment of malignant superior vena cava stenosis. Clin Radiol 1996;51:593-5. [DOI] [PubMed] [Google Scholar]
- 20.Stock KW, Jacob AL, Proske M, Bolliger CT, Rochlitz C, Steinbrich W. Treatment of malignant obstruction of the superior vena cava with the self-expanding Wallstent. Thorax 1995;50:1151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]