Abstract
AIMS
To determine the prevalence and treatment of hypertension, dyslipidaemia and both together in the UK between 1998 and 2006.
METHODS
We used The Health Improvement Network (THIN) a general practice-based database from 1998 to 2006 and we compared the 1998 and 2003 data to that taken from the Health Survey for England (HSE) in 1998 and 2003.
RESULTS
The prevalence (treatment) of hypertension was 25.3% (11.4%) in 1998, 27.8% (15.1%) in 2003 and 26.9% (16.2%) in 2006 in THIN. In HSE it was 37.3% (9.6%) in 1998 and 32.9% (13.8%) in 2003. For dyslipidaemia the figures were 8.6% (1.9%), 18.5% (6.5%) and 24.4% (9.8%) for THIN and 67.8% (2.3%) and 74.9% (7.0%) for HSE. Concurrent hypertension and dyslipidaemia in THIN increased from 5.5% (1.1%) in 1998 to 13.5% (4.5%) in 2003 and 17.4% (7.1%) in 2006. The prevalence of both conditions was 30.6% (0.7%) in HSE in 1998 and 28.7% (3.1%) in 2003.
CONCLUSIONS
There has been a progressive improvement in the detection and treatment of hypertension, dyslipidaemia and both conditions together between 1998 and 2006. However, much still needs to be done to improve the diagnosis and treatment of hypertension, hypercholesterolaemia and concurrent hypertension and hypercholesterolaemia in the United Kingdom.
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
The 1998 and 2003 Health Survey for England revealed a high prevalence of hypertension and hypercholesterolaemia in the population of England.
Major changes in the reimbursement of primary care for the management of both hypertension and hypercholesterolaemia have occurred in the UK.
WHAT THIS STUDY ADDS
Using a GP database we have examined the proportion of subjects diagnosed and treated for hypertension and hypercholesterolaemia over time. To examine the true population rates and primary care data we compared the results of the Health survey for England in both 1998 and 2003 with the recorded data on GP computers.
Despite current guidelines, many patients with hypertension and/or hypercholesterolaemia are under-treated and, even amongst those who are treated, many do not achieve their blood pressure and/or lipid targets.
Although treatment rates in the UK have improved recently, particularly for lipid-lowering therapies, they remain suboptimal.
Keywords: cholesterol, cross-sectional studies, hypercholesterolaemia, hypertension, population-based prevalence, treatment patterns
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide. In Europe, it contributes to nearly 2 million deaths per year in people under the age of 75 years [1], and accounts for 49% of all deaths in Europe [2]. The high prevalence of CVD is attributed to the presence of high levels of modifiable cardiovascular risk factors including hypertension, hypercholesterolaemia, smoking, sedentary lifestyle, diabetes or glucose intolerance and obesity [3]. Hypertension is second only to smoking in its contribution to the burden of disease in developed countries [4]. Globally, hypertension and hypercholesterolaemia are estimated to contribute to 7.1 and 4.4 million deaths per year, respectively [4]. These two risk factors frequently coexist [5–8], and their impact on CVD events is thought to be more than additive [9, 10].
Lifestyle changes are recommended for patients at risk of CVD [11, 12]. However, lifestyle measures alone are often not sufficient and patients should be treated with appropriate antihypertensive and lipid-lowering therapy [11, 12]. Meta-analyses of clinical trials have demonstrated beyond doubt that antihypertensive [13–16] and lipid-lowering [17–19] therapies significantly reduce patients' CVD morbidity and mortality. Current guidelines also advocate the use of statins as lipid-lowering agents [11, 12, 20, 21].
Despite these guidelines, many patients with hypertension and/or hypercholesterolaemia are under-treated and, even amongst those who are treated, many do not achieve their blood pressure [22] and/or lipid targets [22–26]. However, treatment rates have improved somewhat recently, particularly for lipid-lowering therapies, but remain suboptimal [27].
The 1998 Health Survey for England (HSE) demonstrated the high prevalence of hypertension and hypercholesterolaemia in the population of the United Kingdom [28, 29]. In order to estimate the extent to which these conditions are clinically diagnosed and treated in primary practice in the United Kingdom, we conducted a study utilizing electronic records from The Health Improvement Network (THIN) [30] and compared these results against the population-based data from the 1998 HSE [31, 32] and the 2003 HSE [33, 34].
Methods
Primary analyses
The primary aim of this study was to compare the prevalence of hypertension and hypercholesterolaemia, occurring either alone or together, and drug treatment for these conditions, in the 1998 and 2003 population-based HSE and in a cross-sectional analysis of THIN primary care database for the same years. We also examined trends in the prevalence and drug treatment of these conditions from 1998 to 2006 in THIN.
THIN database contains clinical, prescribing and other records, including blood pressures and test results, of over 5.5 million patients. Data are derived directly from the practitioner's electronic patient records, dating from 1985 for some practices. THIN data are likely to reflect what actually happens in primary care in the United Kingdom [http://www.epic-uk.org/thin.htm].
At the time of this analysis THIN study population included patients from 326 THIN practices. We identified patients (aged ≥ 16 years) with a history of hypertension or drug treatment for hypertension among those registered with each practice at the beginning of 1998, 2003 or 2006. The presence of hypertension was determined by one or more of the following: a recorded clinical diagnosis, blood pressure recordings (systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg, averaged over three successive occasions), or a record of antihypertensive drug prescribing. Treatment for hypertension was defined as: thiazide diuretics, unless prescribed for oedema or congestive heart failure; β-adrenoceptor blockers, unless prescribed for angina or anxiety or with nitrates; calcium channel blockers, unless prescribed for angina or with nitrates; angiotensin-converting enzyme inhibitors, unless prescribed for congestive heart failure or with loop diuretics; angiotensin II receptor blockers; α-adrenoceptor blockers or centrally acting drugs. We also identified patients with hypercholesterolaemia in 2003 and 2006. The presence of hypercholesterolaemia was determined by one or more of the following: a recorded clinical diagnosis, a recorded cholesterol measurement (total cholesterol ≥ 5 mmol l−1 (193 mg dl−1) or low-density lipoprotein cholesterol ≥ 3 mmol l−1 (116 mg dl−1)) or a record of prescription of lipid-lowering drug treatment (drugs in BNF chapter 2.12: statins, ezetimbe, fibrates, anion exchange resins, nicotinic acid, fish oils).
The HSE comprised data on individuals from randomly selected addresses. We used the subset of people aged ≥ 16 years with valid blood pressure and total cholesterol data. These individuals were defined as hypertensive if, on the day they were surveyed, they had systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg (based on the average of the last two of three blood pressure measurements taken on the same day), or they were being treated for hypertension. They were defined as dyslipidaemic if they had a total cholesterol concentration ≥ 5 mmol l−1 or they were being treated with lipid-regulating drugs.
The prevalence of hypercholesterolaemia in patients with or without hypertension and the prevalence of hypertension in patients with or without hypercholesterolaemia were also determined in the HSE and THIN.
Secondary analysis
In a secondary analysis, we determined the time to diagnosis of hypercholesterolaemia in patients with or without hypertension and, conversely, the time to diagnosis of hypertension in patients with or without hypercholesterolaemia. We identified patients in THIN aged ≥ 16 years and with no prior history of hypertension or hypercholesterolaemia on 1 January 2003. An inception cohort of hypertensive patients was identified, comprising patients in whom hypertension was first identified between 1 January 2003 and 31 December 2005. Each patient in this cohort was matched with four patients of the same age and gender in the same practice who did not have hypertension. The date of diagnosis of hypertension was defined as the index date for each hypertension case and their controls. The time from the index date to the diagnosis of hypercholesterolaemia in patients with recognized hypertension was compared with that in patients not diagnosed as hypertensive.
Similarly, we defined an inception cohort of dyslipidaemic patients and compared the time to diagnosis of hypertension in these patients with that in a control group of patients not diagnosed with hypercholesterolaemia.
Statistical methods
In the primary analysis, the prevalence of diagnosis and treatment for hypertension, hypercholesterolaemia and both conditions were calculated for patients in seven age categories, by gender and for all patients. Survival models with Weibull distributions were used to model time to diagnosis of disease, adjusting for year, age and gender.
Results
Primary analyses
We used data from 326 practices contributing to THIN. We identified a population of 2.04, 2.46 and 2.58 million patients aged ≥ 16 years and permanently registered in THIN in 1998, 2003 and 2006, respectively. The HSE included 15 908 individuals aged ≥ 16 years in 1998, and 14 836 in 2003. Of these, measurements for blood pressure and total cholesterol were available for 9410 and 6855 individuals. Table 1 shows the gender and age distribution in the five study groups. About 32% of THIN population was under the age of 35 years, compared with only 20% of the HSE sample in 2003 with both blood pressure and cholesterol data.
Table 1.
Prevalence of diagnosis and treatment rates by age for hypertension, hypercholesterolaemia and both conditions in the HSE and in THIN in 1998 and 2003 and in THIN alone in 2006
| Hypertension | Hypercholesterolaemia | Concurrent hypertension and hypercholesterolaemia | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diagnosed | Treated | Diagnosed | Treated | Diagnosed | Treated | ||||||||
| Total patients | n | % | n | % | n | % | n | % | n | % | n | % | |
| HSE 1998 | |||||||||||||
| Men | |||||||||||||
| Age (years) | |||||||||||||
| 16–24 | 364 | 69 | 19.0 | 81 | 22.2 | 20 | 5.5 | ||||||
| 25–34 | 791 | 153 | 19.3 | 3 | 0.4 | 390 | 49.3 | 2 | 0.2 | 88 | 11.1 | ||
| 35–44 | 849 | 221 | 26.0 | 22 | 2.6 | 604 | 71.1 | 7 | 0.8 | 179 | 21.1 | 4 | 0.5 |
| 45–54 | 830 | 343 | 41.3 | 52 | 6.3 | 653 | 78.7 | 24 | 2.9 | 283 | 34.1 | 8 | 1.0 |
| 55–64 | 647 | 389 | 60.1 | 112 | 17.3 | 543 | 83.9 | 49 | 7.6 | 330 | 51.0 | 11 | 1.7 |
| 65–74 | 570 | 400 | 70.2 | 119 | 20.9 | 454 | 79.6 | 36 | 6.3 | 329 | 57.7 | 10 | 1.8 |
| 75+ | 349 | 257 | 73.6 | 80 | 22.9 | 249 | 71.4 | 3 | 0.9 | 193 | 55.3 | ||
| All ages | 4 400 | 1 832 | 41.6 | 388 | 8.8 | 2 974 | 67.6 | 121 | 2.8 | 1 422 | 32.3 | 33 | 0.8 |
| Women | |||||||||||||
| Age (years) | |||||||||||||
| 16–24 | 397 | 17 | 4.3 | 1 | 0.2 | 103 | 25.9 | 8 | 2.0 | ||||
| 25–34 | 850 | 56 | 6.6 | 3 | 0.4 | 380 | 44.7 | 29 | 3.4 | ||||
| 35–44 | 959 | 126 | 13.1 | 23 | 2.4 | 564 | 58.8 | 3 | 0.3 | 96 | 10.0 | ||
| 45–54 | 989 | 306 | 30.9 | 61 | 6.2 | 729 | 73.7 | 11 | 1.1 | 251 | 25.4 | 2 | 0.2 |
| 55–64 | 728 | 359 | 49.3 | 101 | 13.9 | 646 | 88.7 | 35 | 4.8 | 330 | 45.3 | 12 | 1.6 |
| 65–74 | 591 | 427 | 72.2 | 167 | 28.3 | 544 | 92.0 | 37 | 6.3 | 396 | 67.0 | 18 | 3.1 |
| 75+ | 496 | 386 | 77.8 | 155 | 31.2 | 444 | 89.5 | 12 | 2.4 | 350 | 70.6 | 5 | 1.0 |
| All ages | 5 010 | 1 677 | 33.5 | 511 | 10.2 | 3 410 | 68.1 | 98 | 2.0 | 1 460 | 29.1 | 37 | 0.7 |
| Both sexes | 9 410 | 3 509 | 37.3 | 899 | 9.6 | 6 384 | 67.8 | 219 | 2.3 | 2 882 | 30.6 | 70 | 0.7 |
| THIN1998 | |||||||||||||
| Men | |||||||||||||
| Age (years) | |||||||||||||
| 16–24 | 126 073 | 2 024 | 1.6 | 304 | 0.2 | 411 | 0.3 | 36 | 0.0 | 62 | 0.0 | 6 | 0.0 |
| 25–34 | 202 080 | 9 292 | 4.6 | 1 173 | 0.6 | 3 930 | 1.9 | 223 | 0.1 | 896 | 0.4 | 45 | 0.0 |
| 35–44 | 184 959 | 20 267 | 11.0 | 3 804 | 2.1 | 12 374 | 6.7 | 1 261 | 0.7 | 4 147 | 2.2 | 404 | 0.2 |
| 45–54 | 165 152 | 40 637 | 24.6 | 12 158 | 7.4 | 22 582 | 13.7 | 4 474 | 2.7 | 11 505 | 7.0 | 2 151 | 1.3 |
| 55–64 | 124 905 | 51 283 | 41.1 | 21 841 | 17.5 | 25 277 | 20.2 | 7 521 | 6.0 | 16 770 | 13.4 | 4 433 | 3.5 |
| 65–74 | 98 450 | 53 725 | 54.6 | 27 599 | 28.0 | 20 669 | 21.0 | 6 797 | 6.9 | 16 348 | 16.6 | 4 408 | 4.5 |
| 75+ | 75 406 | 43 413 | 57.6 | 23 446 | 31.1 | 7 151 | 9.5 | 1 605 | 2.1 | 6 186 | 8.2 | 1 076 | 1.4 |
| All ages | 977 025 | 220 641 | 22.6 | 90 325 | 9.2 | 92 394 | 9.5 | 21 917 | 2.2 | 55 914 | 5.7 | 12 523 | 1.3 |
| Women | |||||||||||||
| Age (years) | |||||||||||||
| 16–24 | 132 707 | 3 427 | 2.6 | 691 | 0.5 | 500 | 0.4 | 44 | 0.0 | 65 | 0.0 | 10 | 0.0 |
| 25–34 | 209 048 | 13 069 | 6.3 | 3 553 | 1.7 | 3 226 | 1.5 | 156 | 0.1 | 658 | 0.3 | 28 | 0.0 |
| 35–44 | 178 875 | 22 538 | 12.6 | 8 518 | 4.8 | 7 932 | 4.4 | 461 | 0.3 | 2 535 | 1.4 | 170 | 0.1 |
| 45–54 | 160 895 | 46 776 | 29.1 | 20 040 | 12.5 | 16 834 | 10.5 | 1 988 | 1.2 | 8 897 | 5.5 | 1 041 | 0.6 |
| 55–64 | 125 631 | 60 351 | 48.0 | 27 818 | 22.1 | 22 358 | 17.8 | 5 415 | 4.3 | 16 105 | 12.8 | 3 178 | 2.5 |
| 65–74 | 113 030 | 66 502 | 58.8 | 33 920 | 30.0 | 21 096 | 18.7 | 7 094 | 6.3 | 17 585 | 15.6 | 4 622 | 4.1 |
| 75+ | 135 305 | 81 109 | 59.9 | 47 495 | 35.1 | 10 206 | 7.5 | 2 454 | 1.8 | 9 145 | 6.8 | 1 760 | 1.3 |
| All ages | 1 055 491 | 293 772 | 27.8 | 142 035 | 13.5 | 82 152 | 7.8 | 17 612 | 1.7 | 54 990 | 5.2 | 10 809 | 1.0 |
| Both sexes | 2 032 516 | 514 413 | 25.3 | 232 360 | 11.4 | 174 546 | 8.6 | 39 529 | 1.9 | 110 904 | 5.5 | 23 332 | 1.1 |
| HSE 2003 | |||||||||||||
| Men | |||||||||||||
| Age (years) | |||||||||||||
| 16–24 | 239 | 16 | 6.7 | 0 | 0.0 | 64 | 26.8 | 0 | 0.0 | 9 | 3.8 | 0 | 0.0 |
| 25–34 | 415 | 48 | 11.6 | 2 | 0.5 | 249 | 60.0 | 1 | 0.2 | 36 | 8.7 | 0 | 0.0 |
| 35–44 | 639 | 114 | 17.8 | 17 | 2.7 | 496 | 77.6 | 11 | 1.7 | 96 | 15.0 | 1 | 0.2 |
| 45–54 | 576 | 204 | 35.4 | 56 | 9.7 | 488 | 84.7 | 28 | 4.9 | 179 | 31.1 | 13 | 2.3 |
| 55–64 | 575 | 274 | 47.7 | 114 | 19.8 | 513 | 89.2 | 81 | 14.1 | 246 | 42.8 | 36 | 6.3 |
| 65–74 | 432 | 270 | 62.5 | 138 | 31.9 | 374 | 86.6 | 98 | 22.7 | 237 | 54.9 | 50 | 11.6 |
| 75+ | 263 | 179 | 68.1 | 83 | 31.6 | 205 | 77.9 | 46 | 17.5 | 143 | 54.4 | 17 | 6.5 |
| All ages | 3 139 | 1 105 | 35.2 | 410 | 13.1 | 2 389 | 76.1 | 265 | 8.4 | 946 | 30.1 | 117 | 3.7 |
| Women | |||||||||||||
| Age (years) | |||||||||||||
| 16–24 | 276 | 4 | 1.4 | 0 | 0.0 | 99 | 35.9 | 0 | 0.0 | 1 | 0.4 | 0 | 0.0 |
| 25–34 | 487 | 26 | 5.3 | 4 | 0.8 | 246 | 50.5 | 0 | 0.0 | 20 | 4.1 | 0 | 0.0 |
| 35–44 | 726 | 74 | 10.2 | 13 | 1.8 | 443 | 61.0 | 1 | 0.1 | 52 | 7.2 | 0 | 0.0 |
| 45–54 | 659 | 150 | 22.8 | 50 | 7.6 | 523 | 79.4 | 22 | 3.3 | 129 | 19.6 | 9 | 1.4 |
| 55–64 | 701 | 303 | 43.2 | 139 | 19.8 | 635 | 90.6 | 51 | 7.3 | 273 | 38.9 | 22 | 3.1 |
| 65–74 | 471 | 299 | 63.5 | 164 | 34.8 | 439 | 93.2 | 82 | 17.4 | 279 | 59.2 | 41 | 8.7 |
| 75+ | 396 | 297 | 75.0 | 164 | 41.4 | 357 | 90.2 | 62 | 15.7 | 269 | 67.9 | 25 | 6.3 |
| All ages | 3 716 | 1 153 | 31.0 | 534 | 14.4 | 2 742 | 73.8 | 218 | 5.9 | 1 023 | 27.5 | 97 | 2.6 |
| Both sexes | 6 855 | 2 258 | 32.9 | 944 | 13.8 | 5 131 | 74.9 | 483 | 7.0 | 1 969 | 28.7 | 214 | 3.1 |
| THIN 2003 | |||||||||||||
| Men | |||||||||||||
| Age (years) | |||||||||||||
| 16–24 | 161 238 | 2 807 | 1.7 | 528 | 0.3 | 926 | 0.6 | 92 | 0.1 | 182 | 0.1 | 24 | 0.0 |
| 25–34 | 216 423 | 11 164 | 5.2 | 1 898 | 0.9 | 7 093 | 3.3 | 602 | 0.3 | 2 205 | 1.0 | 215 | 0.1 |
| 35–44 | 236 869 | 28 315 | 12.0 | 7 351 | 3.1 | 26 357 | 11.1 | 3 743 | 1.6 | 10 748 | 4.5 | 1 642 | 0.7 |
| 45–54 | 184 817 | 49 163 | 26.6 | 19 723 | 10.7 | 45 557 | 24.6 | 11 872 | 6.4 | 26 068 | 14.1 | 6 562 | 3.6 |
| 55–64 | 163 941 | 73 183 | 44.6 | 38 266 | 23.3 | 62 043 | 37.8 | 24 850 | 15.2 | 44 910 | 27.4 | 16 192 | 9.9 |
| 65–74 | 116 819 | 70 962 | 60.7 | 44 825 | 38.4 | 54 385 | 46.6 | 29 277 | 25.1 | 46 099 | 39.5 | 21 301 | 18.2 |
| 75+ | 99 335 | 62 376 | 62.8 | 41 570 | 41.8 | 32 684 | 32.9 | 16 728 | 16.8 | 29 955 | 30.2 | 12 840 | 12.9 |
| All ages | 1 179 442 | 297 970 | 25.3 | 154 161 | 13.1 | 229 045 | 19.4 | 87 164 | 7.4 | 160 167 | 13.6 | 58 776 | 5.0 |
| Women | |||||||||||||
| Age (years) | |||||||||||||
| 16–24 | 173 435 | 5 776 | 3.3 | 904 | 0.5 | 1 278 | 0.7 | 81 | 0.0 | 238 | 0.1 | 30 | 0.0 |
| 25–34 | 232 093 | 17 404 | 7.5 | 3 832 | 1.7 | 5 895 | 2.5 | 397 | 0.2 | 1 726 | 0.7 | 122 | 0.1 |
| 35–44 | 230 243 | 32 994 | 14.3 | 11 912 | 5.2 | 18 572 | 8.1 | 1 715 | 0.7 | 7 511 | 3.3 | 761 | 0.3 |
| 45–54 | 180 037 | 55 911 | 31.1 | 27 322 | 15.2 | 36 778 | 20.4 | 6 088 | 3.4 | 22 162 | 12.3 | 3 716 | 2.1 |
| 55–64 | 166 202 | 83 929 | 50.5 | 46 753 | 28.1 | 57 925 | 34.9 | 16 884 | 10.2 | 44 344 | 26.7 | 11 650 | 7.0 |
| 65–74 | 131 126 | 82 515 | 62.9 | 51 944 | 39.6 | 57 430 | 43.8 | 25 631 | 19.5 | 50 500 | 38.5 | 19 269 | 14.7 |
| 75+ | 167 585 | 106 825 | 63.7 | 75 026 | 44.8 | 49 102 | 29.3 | 21 350 | 12.7 | 46 006 | 27.5 | 17 109 | 10.2 |
| All ages | 1 280 721 | 385 354 | 30.1 | 217 693 | 17.0 | 226 980 | 17.7 | 72 146 | 5.6 | 172 487 | 13.5 | 52 657 | 4.1 |
| Both sexes | 2 460 163 | 683 324 | 27.8 | 371 854 | 15.1 | 456 025 | 18.5 | 159 310 | 6.5 | 332 654 | 13.5 | 111 433 | 4.5 |
| THIN 2006 | |||||||||||||
| Men | |||||||||||||
| Age (years) | |||||||||||||
| 16–24 | 172 886 | 2 440 | 1.4 | 637 | 0.4 | 1 309 | 0.8 | 144 | 0.1 | 271 | 0.2 | 47 | 0.0 |
| 25–34 | 210 967 | 9 684 | 4.6 | 1 916 | 0.9 | 8 416 | 4.0 | 917 | 0.4 | 2 460 | 1.2 | 321 | 0.2 |
| 35–44 | 245 272 | 26 806 | 10.9 | 8 545 | 3.5 | 34 006 | 13.9 | 5 498 | 2.2 | 13 298 | 5.4 | 2 483 | 1.0 |
| 45–54 | 197 554 | 48 832 | 24.7 | 22 999 | 11.6 | 60 560 | 30.7 | 17 014 | 8.6 | 33 003 | 16.7 | 9 686 | 4.9 |
| 55–64 | 175 750 | 76 280 | 43.4 | 45 542 | 25.9 | 82 390 | 46.9 | 36 342 | 20.7 | 58 154 | 33.1 | 24 524 | 14.0 |
| 65–74 | 121 542 | 72 659 | 59.8 | 50 426 | 41.5 | 69 549 | 57.2 | 42 708 | 35.1 | 58 008 | 47.7 | 31 603 | 26.0 |
| 75+ | 109 641 | 67 649 | 61.7 | 49 362 | 45.0 | 51 149 | 46.7 | 32 175 | 29.3 | 46 823 | 42.7 | 25 212 | 23.0 |
| All ages | 1 233 612 | 304 350 | 24.7 | 179 427 | 14.5 | 307 379 | 24.9 | 134 798 | 10.9 | 212 017 | 17.2 | 93 876 | 7.6 |
| Women | |||||||||||||
| Age (years) | |||||||||||||
| 16–24 | 183 289 | 4 994 | 2.7 | 841 | 0.5 | 1 893 | 1.0 | 141 | 0.1 | 343 | 0.2 | 42 | 0.0 |
| 25–34 | 231 248 | 16 343 | 7.1 | 3 500 | 1.5 | 7 835 | 3.4 | 626 | 0.3 | 2 258 | 1.0 | 238 | 0.1 |
| 35–44 | 242 420 | 33 322 | 13.7 | 12 223 | 5.0 | 25 767 | 10.6 | 2 955 | 1.2 | 10 074 | 4.2 | 1 348 | 0.6 |
| 45–54 | 191 499 | 53 652 | 28.0 | 28 248 | 14.8 | 50 643 | 26.4 | 9 413 | 4.9 | 28 080 | 14.7 | 5 646 | 2.9 |
| 55–64 | 179 344 | 86 253 | 48.1 | 52 904 | 29.5 | 80 078 | 44.7 | 25 557 | 14.3 | 58 542 | 32.6 | 17 826 | 9.9 |
| 65–74 | 135 424 | 82 262 | 60.7 | 56 279 | 41.6 | 74 061 | 54.7 | 36 685 | 27.1 | 63 406 | 46.8 | 28 106 | 20.8 |
| 75+ | 179 179 | 111 377 | 62.2 | 84 351 | 47.1 | 79 926 | 44.6 | 42 607 | 23.8 | 74 684 | 41.7 | 34 855 | 19.5 |
| All ages | 1 342 403 | 388 203 | 28.9 | 238 346 | 17.8 | 320 203 | 23.9 | 117 984 | 8.8 | 237 387 | 17.7 | 88 061 | 6.6 |
| Both sexes | 2 576 015 | 692 553 | 26.9 | 417 773 | 16.2 | 627 582 | 24.4 | 252 782 | 9.8 | 449 404 | 17.4 | 181 937 | 7.1 |
HSE, Health Survey for England; THIN, The Health Improvement Network.
Prevalence and drug treatment of hypertension
The prevalence of hypertension increased with advancing age in both men and women across all three study groups (Table 2, Figure 1A). Similar rates were found in THIN and in the HSE, except in 1998 when the rates in the HSE were higher across all age groups.
Table 2.
Prevalence of hypertension with and without hypercholesterolaemia and hypercholesterolaemia with and without hypertension in the HSE and in THIN in 2003 (row and column totals are not shown for clarity) and in THIN alone for 2006
| Hypercholesterolaemia | ||||
|---|---|---|---|---|
| No | Yes | % Yes | ||
| HSE 2003 (n = 6 855) | ||||
| Hypertension | No | 1 435 | 3 162 | 68.8% |
| Yes | 289 | 1 969 | 87.2% | |
| % Yes | 16.8% | 38.4% | ||
| THIN 2003 (n = 2 460 163) | ||||
| Hypertension | No | 1 653 468 | 123 371 | 8.9% |
| Yes | 350 670 | 332 654 | 48.7% | |
| % Yes | 21.7% | 72.9% | ||
| THIN 2006 (n = 2 576 015) | ||||
| Hypertension | No | 1 705 284 | 178 178 | 12.4% |
| Yes | 243 149 | 449 404 | 64.9% | |
| % Yes | 16.2% | 71.6% | ||
HSE, Health Survey for England; THIN, The Health Improvement Network.
Figure 1.
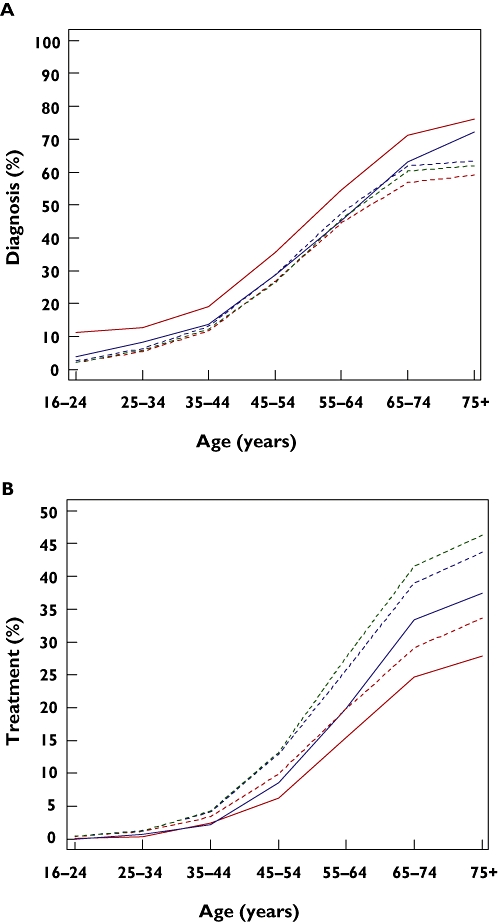
Prevalence of diagnosis (A) and treatment (B) for hypertension in the HSE (solid lines) and THIN (dashed lines) in 1998 (red), 2003 (blue) and 2006 (green)
The overall prevalence of hypertension was lower in the 2003 HSE (32.9%) than in 1998 HSE (37.3%). The treatment rates among those with hypertension increased from 25.6% to 41.8%. In THIN population the prevalence of recorded hypertension was 25.3% in 1998, 27.8% in 2003 and 26.9% in 2006. Treatment rates with antihypertensive medication among these patients were 45.2% in 1998, 54.4% in 2003 and 60.3% in 2006 (Table 2).
Prevalence and drug treatment of hypercholesterolaemia
The point prevalence of hypercholesterolaemia in the HSE increased with advancing age, peaking at 93.2% amongst women aged 65–74 years and at 89.2% amongst men aged 55–64 years in 2003 (Table 2). The rates were slightly higher in all age groups than those observed in 1998. The prevalence of hypercholesterolaemia was much higher in the population-based HSE than in THIN for all age groups (Figure 2A). In the 2003 HSE, 74.9% were diagnosed with hypercholesterolaemia whilst this condition was only diagnosed and recorded in 18.5% of the 2003 THIN population (Table 2). In THIN, the prevalence of diagnosed and recorded hypercholesterolaemia did not exceed 50% in any age group (Table 2). Between 1998 and 2006 the prevalence of diagnosed and recorded hypercholesterolaemia in THIN increased three-fold, but remained far below the rates observed in the HSE.
Figure 2.
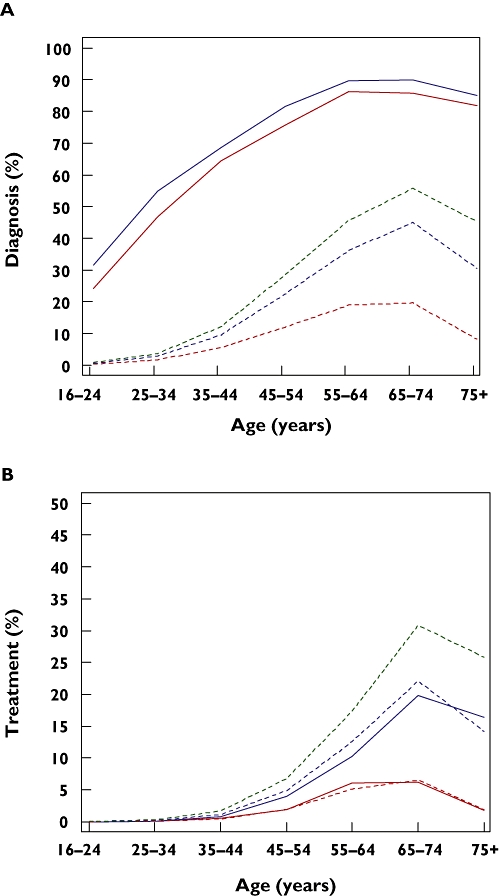
Prevalence of diagnosis (A) and treatment (B) for hypercholesterolaemia in the HSE (solid lines) and THIN (dashed lines) in 1998 (red), 2003 (blue) and 2006 (green)
In the 2003 HSE only 9.4% of those with hypercholesterolaemia were treated with lipid-lowering medication (Table 2), an increase from 3.4% in 1998. However, in THIN treatment rates among patient with recorded hypercholesterolaemia were 22.6% in 1998, 34.9% in 2003 and 40.3% in 2006 (Table 2, Figure 2B).
Prevalence and drug treatment of concurrent hypertension and hypercholesterolaemia
In 2003 28.7% of the HSE population had concurrent hypertension and hypercholesterolaemia, a small increase since 1998. The prevalence of concurrent hypertension and hypercholesterolaemia was higher in the HSE than THIN for all age groups (Table 2, Figure 3A). The prevalence of diagnosed and recorded concurrent disease in THIN increased from 5.5% in 1998 to 13.5% in 2003 and 17.4% in 2006 (Table 2, Figure 3A).
Figure 3.
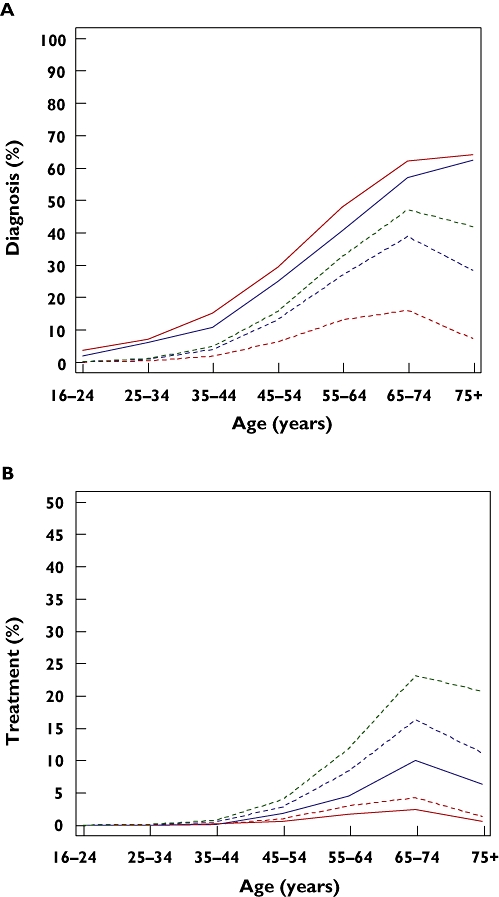
Prevalence of diagnosis (A) and treatment (B) for concurrent hypertension and hypercholesterolaemia in the HSE (solid lines) and THIN (dashed lines) in 1998 (red), 2003 (blue) and 2006 (green)
Treatment rates of concurrent disease were low in the HSE, 2.4% of those diagnosed with both conditions in 1998 and 10.9% in 2003. Treatment rates in THIN were higher: 21.0% in 1998, 33.4% in 2003 and 40.5% in 2006.
Table 2 shows the prevalence of hypertension in patients with and without hypercholesterolaemia and the prevalence of hypercholesterolaemia in patients with and without hypertension in the three study groups. In the 2003 HSE hypertension was more prevalent in individuals with hypercholesterolaemia (38.4%) than in those without hypercholesterolaemia (16.8%). Similarly, in THIN, hypertension was more prevalent in individuals with hypercholesterolaemia (1998 THIN: 72.9%) than in those without this condition (1998 THIN: 21.7%). The converse was also true, with hypercholesterolaemia being more prevalent in individuals with hypertension compared with patients without hypertension in both the 2003 HSE (87.2% vs. 68.8%) and THIN (2003 THIN: 48.7% vs. 8.9%) study populations.
Secondary analysis
In the secondary analysis using THIN patient population, we found that the likelihood of hypertension being diagnosed and recorded in patients with hypercholesterolaemia (n = 36 012) was 2.0 (95% CI 1.9, 2.1) times greater than in patients from the same practice and matched for age and gender, but without hypercholesterolaemia. The likelihood of hypercholesterolaemia being diagnosed in patients with hypertension (n = 19 107) was 5.4 (95% CI 5.2, 5.6) times greater than in patients without hypertension.
Discussion
The HSE is a population-based sample and provides an assessment of the point prevalence of patients with blood pressures and/or total cholesterol concentrations above the thresholds used to define hypertension and hypercholesterolaemia. Guidelines stress the need for more than one blood pressure measurement to diagnose hypertension. In the HSE, blood pressure measurements were made during one visit and therefore the prevalence of hypertension may have been overestimated [29]. In contrast, THIN indicates the extent of clinically diagnosed and recorded hypertension and hypercholesterolaemia among patients who visit their general practitioner, and is likely to underestimate the prevalence in the general population. The prevalence of hypercholesterolaemia was indeed higher in the HSE (74.9% overall) than in THIN (18.5% overall) in 2003. The age specific prevalence rates of hypertension averaged over both sexes were similar in THIN and the HSE sample; there was a higher prevalence of hypertension in women aged 16–54 years in THIN than in the HSE and a lower prevalence in men. Many women in this age group are of child-bearing potential. Those prescribed the contraceptive pill or who are pregnant are likely to have their blood pressure more regularly monitored. Those aged 45–54 years may have begun their menopause, which may also increase their likelihood of visiting their general practitioner and having their blood pressure measured. Both oestrogen therapy and resulting repeated blood pressure measurements could contribute to the higher prevalence of diagnosed hypertension observed in young and middle-aged women.
Our study demonstrated a very low prevalence of recognized hypercholesterolaemia in THIN (18.5% in 2003 vs. 74.9% in the HSE). One explanation for this could be the lack of screening for this condition. Cholesterol screening in the United Kingdom was recommended only in those patients who were at high risk (10-year risk >20%) of CVD [20, 35, 36] at the time of this study. This may have contributed to the under-recognition of hypercholesterolaemia, particularly among younger patients. Whilst it would have been better to have had high density lipoprotein (HDL) concentrations measured in all subjects, these data were not available widely and so we used only total and LDL cholesterol measurements in this study.
Previously published analyses of the 1998 HSE confirm the prevalence of hypertension and hypercholesterolaemia reported in the present study (n = 11 529, hypertension 37%, defined as systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg [29]; n = 10 569, hypercholesterolaemia 68%, defined as total cholesterol ≥ 5 mmol l−1[28]). The prevalence of hypertension and hypercholesterolaemia observed in the HSE is comparable with figures reported in other national surveys [37–39].
The differences we have observed in the present study between clinic- and population-based data are consistent with reports of clinic-based studies conducted in Europe [25] and in the United States [40, 41].
Few surveys have looked into the prevalence of concurrent hypertension and hypercholesterolaemia. A study in the United States estimated that the prevalence of concurrent hypertension and hypercholesterolaemia is approximately 20% (LDL cholesterol ≥ 130 mg dl−1[or ≥100 mg dl−1 in patients with cardiovascular risk factors] and blood pressure ≥ 140/90 (or 130/80 mmHg depending on risk factors), or taking medications for these conditions) (42). We found that the overall prevalence of concurrent hypertension and hypercholesterolaemia was 30.6% in the HSE. A survey in France found that 36.2% of hypertensive men (SBP ≥ 140 mmHg or DBP ≥ 90 mmHg or antihypertensive treatment) aged ≥ 55 years had concurrent hypercholesterolaemia (defined as total cholesterol ≥ 6.5 mmol l−1 (250 mg dl−1)) [43]. A study in the United States comparing the prevalence of hypercholesterolaemia in two ethnically different, community-dwelling samples of hypertensive adults found levels of hypercholesterolaemia among hypertensive individuals similar to those we report, ranging from 49.5% in black women to 78.4% in white men [44]. In the HSE 82.1% of individuals with hypertension had concurrent hypercholesterolaemia.
The prevalence of concurrent hypertension and hypercholesterolaemia observed in the clinic mirrors the trend earlier discussed for isolated hypertension and hypercholesterolaemia. Concomitant hypertension and hypercholesterolaemia were reported in <10% of patients in both the Dutch [25] and United States managed care populations [40]. In the VA population [41], the recorded prevalence of concurrent hypertension and hypercholesterolaemia was considerably higher (30.7%), presumably due to the demographics of this study population. A key strength of the present study is that the GP clinic data and the HSE data were derived in the same National Health Service system.
The prevalence of diagnosed hypertension in THIN changed little between 1998 (25.3%) and 2006 (26.9%), while the prevalence of diagnosed hypercholesterolaemia increased from 8.6% to 24.4% over this 8 year period. Comparison of the prevalence rates in THIN and the HSE in 2003 suggests that about 84% of expected hypertension but only 25% of expected hypercholesterolaemia was detected and recorded in the United Kingdom in that year.
In the 2006 THIN, only 60.3%, 40.3% and 40.5% of patients with diagnosed and recorded hypertension, hypercholesterolaemia and both conditions together, respectively, were treated with antihypertensive and/or lipid-lowering medications. Such low treatment rates are particularly worrying considering that THIN is biased towards well-performing practices in the United Kingdom. Because of this, our results are likely to be optimistic estimates of the national primary care treatment rates in the United Kingdom. The VA clinic-based study by Johnson et al. reported treatment rates of 46.6%, 31.5% and 27.6% with antihypertensives, lipid-lowering agents and both types of medications for asymptomatic patients without diabetes but with hypertension, hypercholesterolaemia or both conditions, respectively. This increased to 66.8%, 42.5 and 50.5%, respectively, in patients with diabetes [26]. In patients with symptomatic CVD treatment rates were higher across all patient groups. In contrast, the treatment rates reported for the Dutch clinic-based study by van Wyk et al. were considerably higher. Among treatment-eligible patients with newly diagnosed hypertension, hypercholesterolaemia and both conditions, treatment rates of 71%, 57% and 72%, respectively, were observed within 1 year of diagnosis [25]. These higher treatment rates may be due to differences in the way in which treatment rates were calculated rather than just differences in the management of these patients. In studies in the United States based on the National Health and Nutrition Examination Survey (NHANES), 37.3% of participants with hypertension and hypercholesterolaemia in 2001–02 received treatment for both conditions [42]. A recent review has shown that hypertension treatment rates are much better in the USA compared with England [45].
The present findings have important clinical implications. The low rates of diagnosis of hypertension and hypercholesterolaemia in THIN compared with the prevalences in the HSE suggest the need to improve screening for hypertension and, particularly, hypercholesterolaemia in clinical practice. The increase in the prevalence of hypertension with advancing age is well documented. Clinicians are therefore more likely to screen older patients for this condition. Our observations from both the HSE and THIN clearly demonstrate an age-related increase in the prevalence of hypercholesterolaemia, suggesting the need to screen routinely for hypercholesterolaemia in the elderly, particularly because the elderly are susceptible to CVD. Others have argued that, in order to maximize the number of event-free life years gained, lipid-lowering treatment may often need to be started in younger individuals [46].
The high prevalence of concurrent hypertension and hypercholesterolaemia in the HSE suggests that when one of these conditions is diagnosed the patient should be screened for the other. Indeed, our results demonstrate considerable clustering of these two cardiovascular risk factors in the United Kingdom population. The observation that less than 25% of those diagnosed with both risk factors in THIN were treated for both conditions indicates a lost opportunity for further risk reduction, particularly in view of the substantial benefits offered by lipid-lowering treatment in hypertensive patients [47]. Future efforts must be directed towards educating clinicians and patients on the importance and benefits of treating all modifiable risk factors. However, educational approaches may only have short-term effects in changing practitioner behaviour, and therefore need to be augmented with wider-reaching approaches [48, 49].
Guidelines for the treatment of hypertension and hypercholesterolaemia call for the assessment and treatment of multiple rather than isolated cardiovascular risk factors [12, 20, 21]. Pharmacological treatment of hypertension [16, 50, 51] and hypercholesterolaemia [18, 19, 47, 50] has been demonstrated to result in significant reductions in the risk of major cardiovascular events.
Limitations
THIN data are limited in that they are observational and taken from electronic records created by general practitioners in primary care. The presence of a disease condition can therefore only be determined for patients who have sought medical care, and where the condition has been investigated, measured and/or diagnosed, and the measurements and/or diagnosis have been recorded electronically by the practitioner. Records may therefore be incomplete and subject to practitioner variation. For example, normal blood pressure recordings or cholesterol assessments may not have been recorded. They may also have been subjected to diagnostic bias for patients who sought medical care for other conditions. Treatment rates do not included nondrug therapy and are based on prescription records, rather than dispensing records. However, the latter would tend to overestimate actual drug treatment rates as patients may not have collected these prescriptions or taken their medications [52]. Finally, THIN practices are likely to represent the most motivated and better practices in the United Kingdom. Despite this, the treatment rates observed in this study are still low.
In contrast to THIN, which is based on longitudinal data accumulated over the course of a year, the HSE measured blood pressure and serum cholesterol during a single patient visit.
We acknowledge that the methodology we employed to ensure that drugs were prescribed for hypertension will have removed from the cohort those treated for both hypertension and ischaemic heart disease or heart failure. This is a limitation that will tend to underestimate the prevalence of these conditions.
In conclusion, our study demonstrates that much still needs to be done to improve the diagnosis and treatment of hypertension, hypercholesterolaemia and concurrent hypertension and hypercholesterolaemia in the United Kingdom. Clinicians need to be aware of the high prevalence of these conditions and should increase their efforts to screen for these conditions, particularly in patients who already have one of these cardiovascular risk factors identified or who are at a high risk of CVD. Furthermore, physicians should insure that all patients with hypertension and/or hypercholesterolaemia should be treated adequately in order to reduce the likelihood of CVD.
Acknowledgments
The Health Survey for England is commissioned by the Department of Health. The 1998 Health Survey for England was carried out by the National Centre for Social Research and the Department of Epidemiology and Public Health at University College London. Access to the dataset was provided by the UK Data Archive. None of the above organizations bear any responsibility for the analysis and interpretation of the data in the present study. Access to the THIN and Health Service for England databases were paid for by Pfizer Inc.
REFERENCES
- 1.Rayner M, Peterson S for the British Heart Foundation Health Promotion Research Group. European Cardiovascular Disease Statistics. 2000. Oxford: British Heart Foundation Health Promotion Research Group, Department of Public Health, University of Oxford, Institute of Health Sciences; 2000. [Google Scholar]
- 2.De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J, Ebrahim S, Faergeman O, Graham I, Mancia G, Manger Cats V, Orth-Gomér K, Perk J, Pyörälä K, Rodicio JL, Sans S, Sansoy V, Sechtem U, Silber S, Thomsen T, Wood D. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2003;24:1601–10. doi: 10.1016/s0195-668x(03)00347-6. [DOI] [PubMed] [Google Scholar]
- 3.Poulter N. Global risk of cardiovascular disease. Heart. 2003;89(Suppl. 2):ii2–5. doi: 10.1136/heart.89.suppl_2.ii2. discussion ii35–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 5.Kannel WB. Risk stratification in hypertension: new insights from the Framingham Study. Am J Hypertens. 2000;13(1 Pt 2):3S–10S. doi: 10.1016/s0895-7061(99)00252-6. [DOI] [PubMed] [Google Scholar]
- 6.Wilson PW, Kannel WB, Silbershatz H, D'Agostino RB. Clustering of metabolic factors and coronary heart disease. Arch Intern Med. 1999;159:1104–9. doi: 10.1001/archinte.159.10.1104. [DOI] [PubMed] [Google Scholar]
- 7.Onat A, Hergenc G, Sari I, Turkmen S, Can G, Sansoy V. Dyslipidemic hypertension: distinctive features and cardiovascular risk in a prospective population-based study. Am J Hypertens. 2005;18:409–16. doi: 10.1016/j.amjhyper.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 8.Tunstall-Pedoe H, Chen R, Kramarz P. Prevalence of individuals with both raised blood pressure and raised cholesterol in WHO MONICA project population surveys 1989–97. Eur Heart J. 2004;25:234. [Google Scholar]
- 9.Neaton JD, Wentworth D. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316 0 99 white men Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med. 1992;152:56–64. [PubMed] [Google Scholar]
- 10.Tunstall-Pedoe H. What was preventing coronary heart disease (CHD) prevention and why its time has now come. In: Wood D, McLeod A, Davis M, Miles A, editors. Effective Secondary Prevention and Cardiac Rehabilitation. London: Aesculapius Press; 2002. pp. 3–13. [Google Scholar]
- 11.Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF, Sever PS, Thom SMcG. Guidelines for management of hypertension: report of the fourth Working Party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens. 2004;18:139–85. doi: 10.1038/sj.jhh.1001683. [DOI] [PubMed] [Google Scholar]
- 12.British Cardiac Society, British Hypertension Society, Diabetes UK, HEART UK, Primary Care Cardiovascular Society, Stroke Association. JBS 2: Joint British Societies' guidelines on prevention of cardiovascular disease in clinical practice. Heart. 2005;91(Suppl. 5):v1–52. doi: 10.1136/hrt.2005.079988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, Weiss NS. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA. 2003;289:2534–44. doi: 10.1001/jama.289.19.2534. [DOI] [PubMed] [Google Scholar]
- 14.Turnbull F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362:1527–35. doi: 10.1016/s0140-6736(03)14739-3. [DOI] [PubMed] [Google Scholar]
- 15.Turnbull F, Neal B, Algert C, Chalmers J, Chapman N, Cutler J, Woodward M, MacMahon S. Effects of different blood pressure-lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trials. Arch Intern Med. 2005;165:1410–9. doi: 10.1001/archinte.165.12.1410. [DOI] [PubMed] [Google Scholar]
- 16.Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427. doi: 10.1136/bmj.326.7404.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.LaRosa JC, He J, Vupputuri S. Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA. 1999;282:2340–6. doi: 10.1001/jama.282.24.2340. [DOI] [PubMed] [Google Scholar]
- 18.Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 19.Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. BMJ. 2003;326:1423. doi: 10.1136/bmj.326.7404.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joint British recommendations on prevention of coronary heart disease in clinical practice. British Cardiac Society, British Hyperlipidaemia Association, British Hypertension Society, endorsed by the British Diabetic Association. Heart. 1998;80(Suppl. 2):S1–29. [PMC free article] [PubMed] [Google Scholar]
- 21.European Society of Hypertension-European Society of Cardiology Guidelines Committee 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–53. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 22.EUROASPIRE II Study Group. Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries; principal results from EUROASPIRE II Euro Heart Survey Programme. Eur Heart J. 2001;22:554–72. doi: 10.1053/euhj.2001.2610. [DOI] [PubMed] [Google Scholar]
- 23.Pearson TA, Laurora I, Chu H, Kafonek S. The lipid treatment assessment project (L-TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med. 2000;160:459–67. doi: 10.1001/archinte.160.4.459. [DOI] [PubMed] [Google Scholar]
- 24.Primatesta P, Poulter NR. Lipid levels and the use of lipid-lowering agents in England and Scotland. Eur J Cardiovasc Prev Rehabil. 2004;11:484–8. doi: 10.1097/01.hjr.0000152241.13209.38. [DOI] [PubMed] [Google Scholar]
- 25.van Wyk JT, Picelli G, Dieleman JP, Mozaffari E, Kramarz P, van Wijk MA, van der Lei J, Sturkenboom MC. Management of hypertension and hypercholesterolaemia in primary care in The Netherlands. Curr Med Res Opin. 2005;21:839–48. doi: 10.1185/030079905X46368. [DOI] [PubMed] [Google Scholar]
- 26.Johnson ML, Pietz K, Battleman DS, Beyth RJ. Therapeutic goal attainment in patients with hypertension and hypercholesterolaemia. Med Care. 2006;44:39–46. doi: 10.1097/01.mlr.0000188982.25397.37. [DOI] [PubMed] [Google Scholar]
- 27.Primatesta P, Poulter NR. Levels of hypercholesterolaemia and improvement in its management in England: results from the Health Survey for England 2003. Clin Endocrinol (Oxf) 2006;64:292–8. doi: 10.1111/j.1365-2265.2006.02459.x. [DOI] [PubMed] [Google Scholar]
- 28.Primatesta P, Poulter NR. Lipid concentrations and the use of lipid lowering drugs: evidence from a national cross sectional survey. BMJ. 2000;321:1322–5. doi: 10.1136/bmj.321.7272.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Primatesta P, Brookes M, Poulter NR. Improved hypertension management and control: results from the health survey for England 1998. Hypertension. 2001;38:827–32. [PubMed] [Google Scholar]
- 30.Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality evaluated database of primary care data. Inform Prim Care. 2004;12:171–177. doi: 10.14236/jhi.v12i3.124. [DOI] [PubMed] [Google Scholar]
- 31.Bajekal M, Boreham R, Brookes M, Falaschetti E, Hirani V, Laiho V, Prior G, Tait C. Health Survey for England: Cardiovascular Disease. [17 July 2007]. The Stationary Office, 1999. Available at http://www.archive.official-documents.co.uk/document/doh/survey98/hse98.htm.
- 32.National Centre for Social Research and University College London, Department of Epidemiology and Public Health. Health Survey for England, 1998. 4. Colchester: UK Data Archive; 2002. [Computer File] SN: 4150. [Google Scholar]
- 33.Sproston K, Primatesta P. Health Survey for England: Cardiovascular Disease. [17 December 2007]. The Stationary Office, 2003. Available at http://www.archive2.official-documents.co.uk/document/deps/doh/survey03/cardd/cardd05.htm.
- 34.National Centre for Social Research and University College London, Department of Epidemiology and Public Health. Health Survey for England, 2003. Colchester: UK Data Archive; 2005. [computer file]. SN: 5098. [Google Scholar]
- 35.Ramsay LE, Williams B, Johnston GD, MacGregor GA, Poston L, Potter JF, Poulter NR, Russell G. British Hypertension Society guidelines for hypertension management 1999: summary. BMJ. 1999;319:630–5. doi: 10.1136/bmj.319.7210.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prevention of coronary heart disease in clinical practice. Recommendations of the Second Joint Task Force of European and other Societies on coronary prevention. Eur Heart J. 1998;19:1434–503. doi: 10.1053/euhj.1998.1243. [DOI] [PubMed] [Google Scholar]
- 37.Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22:11–9. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 38.Ford ES, Mokdad AH, Giles WH, Mensah GA. Serum total cholesterol concentrations and awareness, treatment, and control of hypercholesterolemia among US adults: findings from the National Health and Nutrition Examination Survey, 1999–2000. Circulation. 2003;107:2185–9. doi: 10.1161/01.CIR.0000066320.27195.B4. [DOI] [PubMed] [Google Scholar]
- 39.Mantel-Teeuwisse AK, Verschuren WM, Klungel OH, Kromhout D, Lindemans AD, Avorn J, Porsius AJ, de Boer A. Undertreatment of hypercholesterolaemia: a population-based study. Br J Clin Pharmacol. 2003;55:389–97. doi: 10.1046/j.1365-2125.2003.01769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Selby JV, Peng T, Karter AJ, Alexander M, Sidney S, Lian J, Arnold A, Pettitt D. High rates of co-occurrence of hypertension, elevated low-density lipoprotein cholesterol, and diabetes mellitus in a large managed care population. Am J Manag Care. 2004;10(2 Pt 2):163–70. [PubMed] [Google Scholar]
- 41.Johnson ML, Pietz K, Battleman DS, Beyth RJ. Prevalence of comorbid hypertension and hypercholesterolaemia and associated cardiovascular disease. Am J Manag Care. 2004;10:926–32. [PubMed] [Google Scholar]
- 42.Wong ND, Lopez V, Franklin SS, Tang S, Williams GR. Prevalence, treatment status, and control of concomitant hypertension and hypercholesterolaemia in US adults in 2001–2002. Circulation. 2005;112:831. (abstract, 3840). [Google Scholar]
- 43.Thomas F, Rudnichi A, Bacri AM, Bean K, Guize L, Benetos A. Cardiovascular mortality in hypertensive men according to presence of associated risk factors. Hypertension. 2001;37:1256–61. doi: 10.1161/01.hyp.37.5.1256. [DOI] [PubMed] [Google Scholar]
- 44.O'Meara JG, Kardia SL, Armon JJ, Brown CA, Boerwinkle E, Turner ST. Ethnic and sex differences in the prevalence, treatment, and control of hypercholesterolaemia among hypertensive adults in the GENOA study. Arch Intern Med. 2004;164:1313–8. doi: 10.1001/archinte.164.12.1313. [DOI] [PubMed] [Google Scholar]
- 45.Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, Poulter N, Primatesta P, Stegamayr B, Thamm M. Hypertension treatment and control in five European Countries, Canada, and the United States. Hypertension. 2004;43:10–7. doi: 10.1161/01.HYP.0000103630.72812.10. [DOI] [PubMed] [Google Scholar]
- 46.Ulrich S, Hingorani AD, Martin J, Vallance P. What is the optimal age for starting lipid lowering treatment? A mathematical model. BMJ. 2000;320:1134–40. doi: 10.1136/bmj.320.7242.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sever PS, Dahlof B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J ASCOT investigators. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial – Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361:1149–58. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 48.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003;362:1225–30. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- 49.Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80% BMJ. 2003;326:1419. doi: 10.1136/bmj.326.7404.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Neal B, MacMahon S, Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists' Collaboration. Lancet. 2000;356:1955–64. doi: 10.1016/s0140-6736(00)03307-9. [DOI] [PubMed] [Google Scholar]
- 51.Joint National Committee on Prevention D, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: USDepartment of Health and Human Services. National Institutes of Health; 2003 May. Report no. 03-5233.
- 52.Beardon PH, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM. Primary non-compliance with prescribed medication in primary care. BMJ. 1993;307:846–8. doi: 10.1136/bmj.307.6908.846. [DOI] [PMC free article] [PubMed] [Google Scholar]


