Abstract
Background/Objective:
There are few reports of developmental or congenital cervical spinal deformities. Such cases may be mistaken for traumatically induced fractures, and additional treatment may ensue.
Methods:
A retrospective analysis was performed to identify patients with congenital cervical spine deformities. These patients were matched with a confirmed traumatic spinal fracture population with similar demographic features. Patients were analyzed for age, gender, imaging findings (plain roentgenograms including dynamic flexion and extension views, computed tomography scan, and MRI), neurologic status, and subjective complaints of pain.
Results:
Thirty-six individuals were included in the final analysis, 7 with congenital abnormalities and 29 with radiographically confirmed traumatic injuries. Patients with congenital abnormalities had significantly less soft-tissue swelling compared with the population with traumatic fractures (P < 0.001). Furthermore, those with congenital defects presented with lesser degrees of vertebral subluxation (0.29 mm vs 7.24 mm) (P < 0.0001) and without neurologic deficits (P < 0.0001).
Conclusions:
Congenital abnormalities, though rare, can be mistaken for traumatic fractures of the spine. Physicians should note any evidence of soft-tissue swelling, neurologic deficits, degree of subluxation, and radiographic evidence of pedicle absence because these characteristics often provide insight into the specific etiology of the observed spinal deformity (congenital vs traumatic).
Keywords: Cervical spine; Fracture; Spine, congenital defect; Deformity, developmental; Spinal cord injuries, traumatic; Pedicle, absence
INTRODUCTION
Patients frequently present after minor or low-mechanism blunt cervical trauma with complaints of musculoskeletal pain. Fortunately, very few patients will incur significant cervical instability or spinal cord injury. The incidence of instability increases with high-energy force impact injuries, which may result in osseous fractures, vertebral body dislocation, and ligamentous injury. These unstable cervical spine injuries may warrant surgical treatment and stabilization.
Following trauma, assessment of spinal injury via physical examination may be of limited value because of coexisting paraspinal muscle pain, tenderness, or other distracting injuries. Cervical spine radiographs are routinely performed following trauma to assess the structural integrity of the spinal column and to determine spinal stability. During this initial radiographic evaluation, a small subset of patients with developmental or congenital structural cervical spine deformities may be encountered. In some cases, congenital anomalies may resemble acute traumatic fractures and must be differentiated.
Failure to appreciate a congenital deformity may lead to overtreatment, including additional surgical intervention (1). We reviewed pertinent cervical anatomy related to congenital bony cervical facet anomalies and compared those findings to the imaging characteristics of acute cervical spinal injuries to help differentiate those entities.
METHODS
Traumatic spinal fractures evaluated through the Delaware Valley Regional Spinal Cord Injury Center at Thomas Jefferson University Hospital were reviewed. The study covered a time span of 4 years, consisting of 1,823 patients with cervical spinal injuries treated at our center. Eleven patients with cervical congenital abnormalities were identified, of which 4 patients were excluded from analysis due to either incomplete imaging (1 patient) or due to the congenital abnormality being consistent with an anterior spinal anomaly, Klippel-Fiel deformity, (3 patients), and thus not interpreted as a fracture. The final analysis therefore consisted of 7 congenital cervical spinal deformities.
Upon admission, patients were independently examined by a spinal cord injury service consisting of a neurosurgeon, an orthopedic surgeon, and a physiatrist, which graded neurologic function using the American Spinal Injury Association classification.
Anteroposterior and lateral plain radiographs were obtained on all patients, consisting of cervical, thoracic, and lumbar films as well as cervical oblique and open-mouth odontoid views. Computed tomography imaging was then performed to evaluate further any suspicious fracture or anomaly or to image the cervicothoracic junction if not adequately visualized.
A matched cohort of patients with radiographically confirmed cervical spinal injuries was generated during the same period using the same database. A detailed review of medical charts, office records, discharge summaries, and imaging studies was performed. The translation or subluxation of the vertebral bodies was measured by drawing lines along the posterior vertebral bodies of the two involved vertebrae on plain lateral cervical radiographs. Translation is measured as the transverse distance between the lines at the level of the inferior endplate of the upper (dislocated) vertebra (2). Data points obtained included patient demographics (eg, age, gender), admission neurologic evaluation, mechanism of injury, vertebral level of abnormality, presence of soft-tissue swelling, location of the abnormality on the vertebral body, and subluxation in millimeters. Statistical analyses were performed using the JMP statistical software package (Statistical Analysis System, Inc, Cary, NC), and because cell counts were small, contingency table analyses were performed using the Fisher exact test (two-tailed).
RESULTS
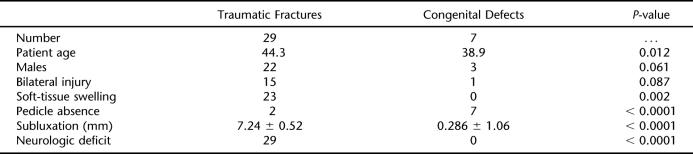
Thirty-six patients were included in the final analysis: 29 patients with traumatic fracture dislocations and 7 patients with congenital facet defects/developmental disorders (Table 1). Mean patient age for those with traumatic fractures was 44.3 years and for those with congenital defects was 38.9 years, a significant statistical difference. (P = 0.012) The 7 patients with congenital defects consisted of 4 females and 3 males, whereas the trauma patients consisted of 7 females and 22 males. Variations in gender distribution were not statistically significant (P = 0.061).
Table 1.
Summary of Data
The location of the pedicle fracture or congenital defect was categorized as either right-side, left-side, or bilateral. Again, none of these classifications showed a systematic variation. The congenital group had 1 bilateral, 3 left-sided, and 3 right-sided anomalies, whereas the patients with traumatic fractures had 15 bilateral, 7 left-sided, and 7 right-sided facet injuries (P = 0.264). Fifteen of the 29 patients with acute traumatic injury had a traumatically induced bilateral facet dislocation, as opposed to 1 of the 7 patients with congenital facet dislocations (P = 0.087).
None of the 7 patients with congenital facet defects had evidence of soft-tissue swelling, whereas 23 of the 29 patients with traumatic fractures had soft-tissue swelling (P = 0.002). On initial radiographs, the absence of a pedicle in only 1 segment was associated with the presence of congenital facet disorder; 7 out of 7 of the patients with congenital facet disorders had this anomaly vs only 2 of the 29 patients with traumatic injuries (P < 0.0001).
The degree of vertebral subluxation in the congenital facet disorders group was a mean of 0.286 mm ± 1.06 mm, compared with a mean of 7.24 mm ± 0.52 mm (P < 0.0001) in the traumatic population. None of the 7 patients with congenital facet disorders had evidence of neurologic deficit on initial evaluation, whereas all 29 of the patients with traumatic facet injuries had neurologic injury, which varied from nerve root injuries to spinal cord deficits. (P < 0.0001).
These analyses were repeated on the bilateral and unilateral cohorts, taken separately. For unilateral damage or defect, (5/19 congenital, 14/19 trauma), all statistical results remained significant: 12 of the 14 trauma cases showed soft-tissue swelling vs none of the 5 congenital cases (P = 0.0018); 2 of the 14 trauma cases had a pedicle abnormality, whereas all 5 of the congenital cases did (P = 0.0018); none of the 5 congenital cases had a neurologic deficit, whereas all of the trauma cases did (P < 0.0001); and the subluxation was 0.2 mm ± 0.45 mm for congenital vs 6.71 mm ± 3.50 mm for trauma (P = 0.0008). The situation was less clear for bilateral defect, because only 1 of the 16 cases was congenital vs 15 of the 16 for trauma. Subluxation was significantly different, with trauma cases having 7.73 mm ± 0.69 mm vs 1 mm for the sole congenital case (P = 0.0279), but none of the other relationships remained statistically significant.
DISCUSSION
Infrequently, the posterior cervical elements will have a developmental failure of migration resulting in the absence of the pedicle and malunion of the facet complex (1,3–7). These congenital facet disorders are typically asymptomatic. However, these anomalies may be incidentally noted during a routine radiographic examination or after radiographs are obtained following trauma (Figures 1–3). It would be helpful to differentiate these congenital facet defects from acute cervical fractures consistently in order to avoid additional treatment.
Figure 1. Lateral cervical spine radiograph. Patient was transferred for evaluation from an outside hospital after a minor motor vehicle crash, and the question of a C3 fracture. Note: the smooth borders, the absence of the C3 pedicle, and abnormal C3–C4 facet complex (arrow).
Figure 3. Axial computed tomography scan through C4 vertebral body illustrating the absence of the pedicle. Note the well-corticated margins (arrows).
Radiographic Examination
After a traumatic injury, physicians must exclude ligamentous injury or fracture through a detailed physical examination and advanced imaging (8,9). If the history or physical examination is suggestive of a spinal injury, radiographs of the cervical spine are routinely obtained to assess for spinal instability (8,9). Infrequently, as part of this evaluation, an individual may present after a low-energy injury with an abnormality on plain radiographs thought to be of a congenital origin (Figure 1). A few clinical series have discussed the confusion surrounding these congenital abnormalities and how at times overtreatment may ensue through the application of unwarranted traction, halo vest application, or surgical intervention (4,7). Similar to other clinical series, congenital cervical facet abnormalities in this series were found throughout the cervical spine (C2–C7) (3).
In a patient with a suspected cervical spine traumatic injury, the physician must assess spinal soft tissues and ligamentous complex to determine spinal stability. The presence of soft-tissue swelling over the prevertebral region may serve as indirect evidence of a traumatic injury (10,11). In this series, no patient with a congenital defect (0 of 7) had evidence of soft-tissue swelling on initial plain radiographs, whereas the majority of the traumatic patients had significant soft-tissue swelling (23 of 29) (P < 0.001).
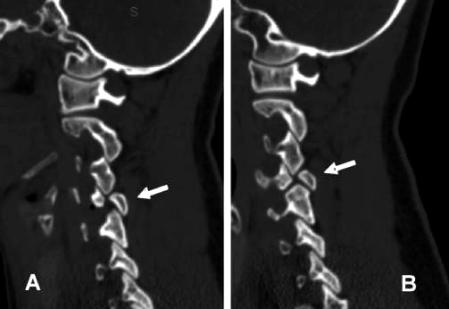
Additionally, a thorough evaluation of the osseous structures is required. In congenital facet disorders, the anterior vertebral column is intact and there is often no subluxation because the posterior facet anomaly is due to failure of bone formation. This differs from facet dislocations, in which there is disruption of the facet joints, with consistent radiographic evidence of vertebral body subluxation. This subluxation results in a decrease in spinal canal diameter and potentially a neurologic injury. In patients with traumatic injuries, the degree of vertebral subluxation was consistently greater than that measured for those with congenital abnormalities (mean 7.24 mm vs 1.06 mm) (P < 0.0001). The lack of significant vertebral subluxation in the congenital facet group is secondary to the disconnection of the facet and the vertebral body due to the absence of a pedicle. The exact etiology and pathophysiology of the malformation is not completely understood and may be due to a defect in the chondrification center of the neural arch during the early cartilaginous stage of development (6). The absence of a pedicle was not a significant finding between congenital and traumatically induced abnormalities (P = 0.264) (Figures 2 and 3). Although the pedicle was absent in all patients with a congenital anomaly, its absence or defect was also illustrated in some of the traumatic population.
Figure 2. Reformatted computed tomography scan of the cervical spine of the facet joints: (A) right side, (B) left side.
This perceived absence of the pedicle in the traumatic injuries actually represented a fracture through the pedicle with subsequent distraction of the osseous elements creating a void. This discontinuity, or absence, was considered a significant radiographic finding and was therefore recorded in the analysis. These absent pedicles can further be differentiated in that the congenital disorders had sclerotic margins, whereas the acute fractures had irregularities in the cortical margins consistent with an acute fracture.
Embryogenesis suggests that the absence of the congenital pedicle may be required to create a congenital facet defect due to failure in migration. This in isolation is not a pathognomonic feature because this finding was present in the traumatic fractures.
There was not a predilection for the lesions to be isolated or lateralized to one side of the spine (P > 0.264). Congenital facet disorders were less likely to occur bilaterally.
Physical Examination
Although spinal imaging may illustrate the presence of a congenital anomaly, detailed physical examination can further help differentiate these anomalies from a traumatically induced lesion (4). In general, the traumatic spinal injury population has a significant male predilection. In this series, there was also a trend for males to be associated with traumatic facet fractures, although our sample size may have been too small for statistical significance (P = 0.089). The patients with congenital defects presented without a neurologic deficit, as opposed to patients with traumatic fracture subluxation or dislocation, of whom all in our study had a spinal cord injury, radicular symptoms, or other deficit (P < 0.0001).
CONCLUSION
Physicians commonly encounter patients with traumatic cervical spinal fractures and injuries. Assessing physicians must be aware of the infrequent incidence of congenital deformities when making a diagnosis and preparing a treatment algorithm. It is possible to differentiate these disorders through physical examination and adequate imaging analysis for the presence of soft-tissue swelling and/or subluxation (>3 mm). If these anomalies are present, further testing and inquiry must be initiated to rule out a fracture injury, vertebral subluxation, or dislocation. Congenital anomalies do not require treatment but may require counseling and follow up to avoid dangerous activities that may predispose the patient to cervical instability and injury.
REFERENCES
- Mantilla-Martin MT, Miller JD. Congenital absence of a pedicle in a cervical vertebra: report of two cases. Can Assoc Radiol J. 1993;44:280–284. [PubMed] [Google Scholar]
- Bono CM, Vaccaro AR, Fehlings M, et al. Measurement techniques for lower cervical spine injuries. Spine. 2006;31((5)):603–609. doi: 10.1097/01.brs.0000201273.39058.dd. [DOI] [PubMed] [Google Scholar]
- Edwards MG, Wesolowski D, Matasar K. Imaging of the absent cervical pedicle. Skeletal Radiol. 1991;20:325–328. doi: 10.1007/BF01267656. [DOI] [PubMed] [Google Scholar]
- Gomez MA, Damie F, Besson M, Roger R, Alison D. Congenital anomaly of the cervical spine: misdiagnosis in the context of trauma (Fr) Rev Chir Orthop Reparatrice Appar Mot. 2003;89:738–741. Available at: http://srvsofcot.sofcot.com.fr/Apcort/rco/rco03/89_8/art11/art11_fs.htm. Accessed August 24, 2007. [PubMed] [Google Scholar]
- Jones DN, Price J. Imaging of the absent cervical pedicle syndrome. Australas Radiol. 1994;38:278–281. doi: 10.1111/j.1440-1673.1994.tb00198.x. [DOI] [PubMed] [Google Scholar]
- McLoughlin DP, Wortzman G. Congenital absence of a cervical vertebral pedicle. Can Assoc Radiol J. 1972;23:195–200. [PubMed] [Google Scholar]
- Wiener MD, Martinez S, Forsberg DA. Congenital absence of a cervical spine pedicle: clinical and radiological findings. AJR Am J Roentgenol. 1990;155:1037–1041. doi: 10.2214/ajr.155.5.2120932. [DOI] [PubMed] [Google Scholar]
- American Association of Neurological Surgeons and the Congress of Neurological Surgeons. Radiographic assessment of the cervical spine in asymptomatic trauma patients. Neurosurgery. 2002;50((suppl 3)):S30–S35. doi: 10.1097/00006123-200203001-00008. [DOI] [PubMed] [Google Scholar]
- American Association of Neurological Surgeons and the Congress of Neurological Surgeons. Radiographic assessment of the cervical spine in symptomatic trauma patients. Neurosurgery. 2002;50((suppl 3)):S36–S43. doi: 10.1097/00006123-200203001-00009. [DOI] [PubMed] [Google Scholar]
- DeBenhe K, Havel C. Utility of prevertebral soft tissue measurements in identifying patients with cervical spine injury. Ann Emerg Med. 1994;24:1119–1124. doi: 10.1016/s0196-0644(94)70242-x. [DOI] [PubMed] [Google Scholar]
- Miles KA, Finlay D. Is prevertebral soft tissue swelling a useful sign in injury of the cervical spine? Injury. 1988;19177–19179. [DOI] [PubMed]