Abstract
Background/Objective:
To evaluate which tests best predict the ability of patients with ventilator-dependent tetraplegia to wean from the ventilator.
Methods:
Retrospective review of patients.
Participants:
Twenty-six ventilator-dependent patients with tetraplegia admitted to a university inpatient spinal cord–injury rehabilitation unit with American Spinal Injury Association (ASIA) injury levels C2 to C6, A or B.
Results:
Failure to wean off the ventilator completely was predicted by absence of motor unit recruitment of one hemidiaphragm or at least moderate decreased recruitment with needle electromyography (EMG) in both hemidiaphragms. Phrenic nerve conduction studies would have predicted that all patients who weaned off the ventilator would have failed. Fluoroscopic examination of the diaphragm and bedside spirometry were not as good predictors of ability to wean, failing to predict accurately in 44% and 19% of cases, respectively. ASIA examination was also not entirely predictive, and any outliers that may have been expected to wean based on ASIA examination (ie, C4 or lower neurological levels) were predicted not to wean by needle electromyography.
Conclusions:
Negative inspiration force diaphragm needle EMG best predicted the ability to wean from the ventilator. Bedside spirometry (negative inspiratory force and forced vital capacity) is an accurate bedside measure of a patient's readiness to wean. Fluoroscopic examination of the diaphragm and phrenic nerve conduction studies were not helpful in determining weaning potential in ventilator-dependent patients with cervical spine injury.
Keywords: Spinal cord injuries, cervical; Tetraplegia; Mechanical ventilation; Ventilator dependence; Ventilator weaning; Electromyography
INTRODUCTION
Some patients with acute high cervical spinal cord injury (SCI) are ventilator dependent. The level of neurological injury as it affects diaphragm function certainly has an influence on this complication because the diaphragm receives primary innervation at the C4 level, with contribution commonly seen from C3 and C5 (1). Prior comorbidities such as asthma or chronic obstructive pulmonary disease might have an effect, as would new pulmonary complications such as adult respiratory distress syndrome, pulmonary contusion, or pneumothorax. The incidence of ventilator dependence in patients with injuries at the C1 to C4 levels has been reported to be 40% (2). The ability to wean is anticipated, in that patients will show an improvement of forced vital capacity (FVC) of as much as 80% over the first 5 months postinjury (3). Carter (4) demonstrated that 16 of 22 patients with injury levels of C4 and below were able to be weaned from the ventilator in an average of 16 days. In a retrospective review, Oo et al (5) demonstrated that 7 of 33 patients with C1 to C4 SCI and diaphragmatic paralysis weaned from the ventilator in 40 to 292 days. In that study, diaphragm paralysis was demonstrated by fluoroscopic examination of the diaphragm and by transcutaneous phrenic nerve stimulation with diaphragm fluoroscopy. This cohort consisted of 5 patients with C2 level injuries, 6 with C3, and 1 with C4. Patients were weaned if they had an FVC of at least 17 mL/kg. The other 74 patients in this series had intact diaphragms and were weaned in 36.8 ± 25 days. Oo and colleagues noted that 4 of the 12 patients who successfully weaned after demonstrating negative diaphragm motion also had no response on phrenic nerve motor conduction studies. A study of 134 ventilator-dependent patients with tetraplegia demonstrated that neurological level influenced the rate of ventilator weaning, with greater than 85% success in weaning at levels C4 and below, 60% success at C3, 28% at C2, and 15% at C1. Other factors that predicted failure from weaning included age greater than 50 years and medical comorbidities (6).
Others have discussed the expected differences in recovery pattern of patients with diaphragmatic paralysis with either neurapraxic or axonal injuries without demonstrating this difference via electrodiagnostic or radiologic studies in their patients (7,8). Studies of motor recovery after SCI have demonstrated that 27% of patients with an American Spinal Injury Association (ASIA) level A injury will achieve at least antigravity strength in the first zero-grade muscle below the neurological level of injury during the first year following injury (9,10). A study looking just at cervical-level recovery noted that 36% of the first zero-grade muscles below the level of injury and 82% of the grade 1 and 2/5 muscles achieved a grade of 3/5 within 6 months of injury. In patients with initial zero strength, rates of improvement increased to 41% at 6 months and 64% at 2 years (11). It might be reasonable to expect an analogous improvement in the functional recovery of the diaphragm in persons with high cervical SCI.
This study attempts to clarify this issue by redirecting the analysis to those factors that predict ventilator weaning. Data such as fluoroscopic examination of the diaphragm and spirometry results are used prospectively in the evaluation of ventilator-dependent patients. Understanding which data are most predictive of weaning would be helpful in determining which patients with SCI would be candidates for weaning from the ventilator. In addition, needle electromyography (EMG) of the diaphragm is included in the evaluation process. Such an evaluation would be expected to clarify whether lack of diaphragm motion as noted on fluoroscopic examination is due to an axonal process. EMG may also show actual diaphragmatic motor unit activity that may not be picked up on fluoroscopic studies. This knowledge would change the expected time frame of recovery and case planning during inpatient rehabilitation.
METHODS
Subjects
Upon Institutional Review Board approval, the charts of 29 consecutive patients with SCI who were ventilator dependent upon admission to acute rehabilitation were investigated. Success or failure to wean from the ventilator was determined. Successful weaning was defined as being ventilator free, including not requiring a nighttime ventilator or positive pressure support. Age, ASIA level as a single neurological level (12), date of injury, time to rehabilitation, and time to ventilator weaning were established. Premorbid cardiac and pulmonary morbidities were recorded, including smoking history. Postinjury cardiac complications were recorded. Postinjury pulmonary complications, including atelectasis and pneumonia, were recorded.
Measures
The result of bedside spirometry was recorded, as completed by a respiratory therapist using a handheld flow gauge and an LTV 1000 ventilator (Pulmonetic Corporation, Colton, CA) to measure pressure and volume. The results were obtained through an adapter to a #6 or 8 tracheostomy tube in all cases. FVC was measured over 3 trials, with the largest being recorded in milliliters. The patients were all semirecumbent at an angle of 30 to 60 degrees. Negative inspiratory force was measured over 3 trials, with the largest being recorded in centimeters of water. As the results changed over time, the value recorded was the one taken at the time that weaning was accomplished or at the time that it was determined that weaning would not be possible. The results were obtained in the morning to avoid the negative affect of prior nighttime sleeping medication and before administration of morning pain or antispasticity medication.
Fluoroscopic examination of the diaphragm was completed over 3 trials to ensure accuracy. The study was completed for 3 breaths taken with the patient off the ventilator. The study was conducted and interpreted by an attending radiologist. Responses were recorded as normal, attenuated, no response, or paradoxical response of the diaphragm. This test was conducted before weaning was attempted.
Phrenic nerve conduction studies were completed prior to attempted weaning, as demonstrated by Kimura (13). Stimulation was conducted posterior to the sternocleidomastoid above the clavicle and over the anterior scalene. The recording electrode was over the xiphoid process with the reference electrode over a rib on the side being tested. Amplitude and distal latency were recorded.
Diaphragm needle EMG was completed prior to attempted weaning, as demonstrated by Chiodo et al (14) and Bolton et al (15). The diaphragm was sampled by needle insertion perpendicular to the skin above the eighth rib in the anterior axillary line. When the intercostal muscles are traversed, the needle enters a short electrically silent space before entering the diaphragm. Spontaneous activity was recorded as 0 to 4. Recruitment was recorded as normal or decreased, as noted by Daube (16). Determination for decreased 1+ was made if second order recruitment was greater than 12 Hz or if mild decrease in full interference pattern was seen. Determination for decreased 4+ was made if only a single or two motor units were seen with attempts at full effort. Decreased 2+ and 3+ are gradations between this, with 2+ showing a small degree of further loss of recruitment compared with 1+ and 3+ as showing a small degree of additional recruitment beyond 4+.
Analysis
These data as well as the presence of cardiac and pulmonary comorbidities were obtained and entered into a database. Statistical analysis of the relationship between these factors was conducted using chi-square analysis. A t-test was used to evaluate the age of patients and the time to wean and to be admitted to rehabilitation.
RESULTS
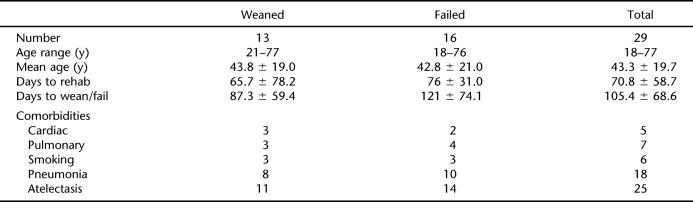
Twenty-nine patients were identified who met the inclusion criteria of this study in that they were admitted to the rehabilitation unit with ventilator dependence and an acute cervical SCI. All patients were ASIA level A or B on admission to rehabilitation, with a neurological level of C2 to C6. Table 1 notes pertinent demographic and medical history information about these patients. Mean age was 43.3 years, with a range of 18 to 77 years. The mean age of the weaned patients and the failed-weaning patients did not differ. The mean time before inpatient rehabilitation was 70.8 days, with a range of 14 to 191 days. The mean time before inpatient rehabilitation did not differ between the weaned patients and those who failed to wean. The mean time elapsed before a patient weaned was 87.3 days, whereas the mean time elapsed before it was decided a patient would not wean was 121 days. This difference was significant. The number of patients with cardiac or pulmonary comorbidity, smoking history, pneumonia, and atelectasis did not differ between the successfully weaned and the failed-weaning groups.
Table 1.
Patient Demographics
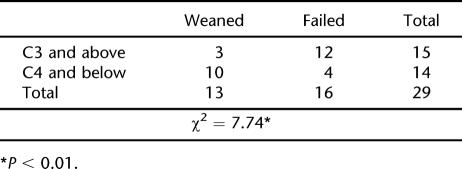
Neurological Level
Thirteen of 29 patients successfully weaned. Three patients had C3-level injuries, 7 had C4, 2 had C5, and 1 had C6. Of the 16 patients who remained ventilator dependent, 3 had C2-level injuries, 9 had C3, 2 had C4, and 2 had C5. In this series, the wean rate was 0% of patients with C2-level injuries, 25% with C3, 77% with C4, and 50% with C5. Table 2 shows that ASIA classification significantly differentiated people who were unable to wean, although false-positive and false-negative rates were 4 of 16 (25%) and 3 of 13 (23%), respectively. There was no significant difference in age, time to rehabilitation, time to wean or fail, or incidence of pulmonary or cardiac comorbidities in these two groups. Of the three C3 patients who were able to wean, successful weaning was predicted by their diaphragm needle EMG results, and in 2 of 3, success was predicted by their spirometry results. Of the four C4/C5 patients who failed to wean, neither age nor comorbidity explained this inability. Spirometry predicted failure to wean in 2 of 4, and needle EMG predicted failure in 3 of 4. The 1 patient in whom needle EMG failed to predict weaning had a negative inspiratory force of 32 mL/kg and an FVC of 540 mL/kg.
Table 2.
Weaning as Predicted by ASIA Classification
Laboratory Testing
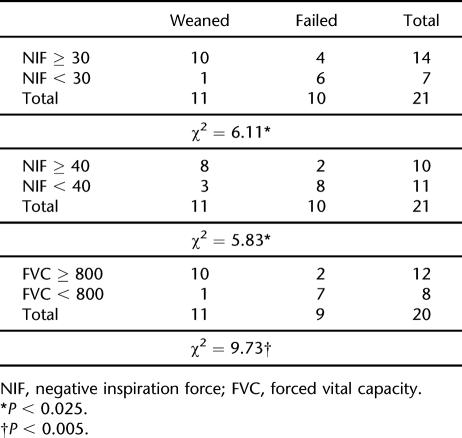
Spirometry.
Bedside spirometry was successfully completed and documented in 21 patients, which represented 72% of the patient population. The patients who did have spirometry results documented are included in Table 3. The spirometry data show that both FVC and negative inspiratory force significantly differentiated people who were able to wean from those who were not. Using negative inspiratory force of ≥ 30, false positive and negative rates were 1 of 11 (9%) and 4 of 10 (40%). The one patient able to wean was predicted by needle EMG recruitment. Needle EMG also predicted 2 of the 4 who failed to wean who had documented EMG data. Using force ≥40 as the cutoff gave rates of 3 of 11 (27%) and 2 of 10 (20%); all 5 outliers were accurately predicted by the EMG recruitment data. Forced vital capacity ≥800 mL/kg gave false positive and negative rates of 1 of 11 (9%) and 2 of 9 (22%). The two who failed to wean both had one hemidiaphragm with no motor unit recruitment.
Table 3. Weaning as Predicted by Bedside Spirometry in 21 Patients.
Of the 8 patients for whom spirometry data were not available, 2 patients weaned from the ventilator. Both had C5-neurological-level injuries, weaned in 13 and 39 days, respectively, and had no more than moderate diaphragm denervation. Of the 6 patients who failed to wean, the mean time before failing to wean was 145.2 days. One was a C2-level patient with no recruited motor units in 1 hemidiaphragm and a single recruited motor unit in the other. A second patient had a C4-level injury and at least moderate denervation in both hemidiaphragms. Four patients had C3-level injuries. One patient had no motor unit recruitment in either hemidiaphragm, 1 had no motor unit recruitment in 1 hemidiaphragm, 1 had a least moderate decreased recruitment in both hemidiaphragms and severe coronary artery disease and chronic obstructive pulmonary disease from a lifetime of smoking, and 1 did not have EMG testing.
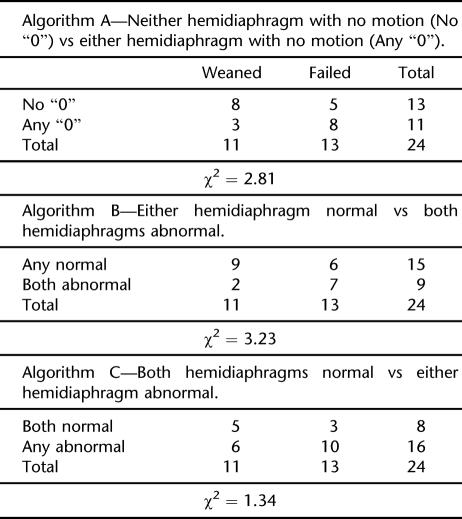
Diaphragm Fluoroscopy.
Fluoroscopic examination of the diaphragm was successfully completed in 24 patients. For the purpose of determining whether fluoroscopic examination of the diaphragm has the potential to classify subjects accurately in terms of their ability to wean, 3 schema were used for their classification: (a) whether any diaphragm motion was observed, (b) whether either hemidiaphragm was normal, and (c) whether both hemidiaphragms were normal. Table 4 shows that regardless of the stratification of the results, fluoroscopic examination of the diaphragm did not differentiate patients who were able to wean from the ventilator from those who were not.
Table 4. Weaning as Predicted by Diaphragm Fluoroscopy.
Phrenic Nerve Conduction Studies.
Phrenic nerve conduction studies were completed in 25 patients. The criterion used for distinguishing likely ventilator weaning was whether there was any evoked amplitude. As with the fluoroscopic examination of the diaphragm, results from these studies did not provide significant differentiation between patients who did and did not wean. Table 5 shows that motor nerve conduction studies did not differentiate patients who were able to wean from the ventilator from those who were not.
Table 5.
Weaning as Predicted by Phrenic Motor-Evoked Amplitude on Nerve Conduction Study
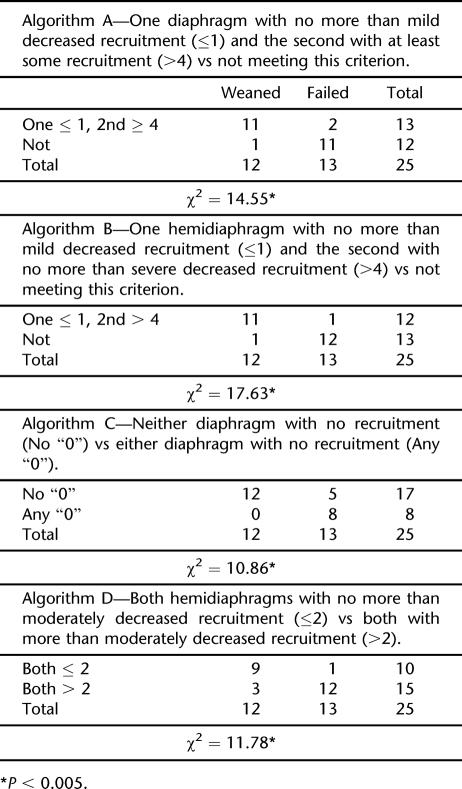
Diaphragm Needle EMG.
Needle EMG of the diaphragm was completed in 25 patients. Four different algorithms were evaluated for appraising needle EMG's ability to differentiate ability to wean. All 4 demonstrated significant ability to do so. False-positive and false-negative rates varied with the algorithms' stringency. As seen in Table 6, the false-positive rate was 0 using algorithm C, in which subjects were separated depending upon whether either diaphragm had any recruitment. Conversely, the false-negative rate was 38%. Of the 8 patients who failed to wean with no motor recruitment on diaphragm needle EMG, 4 had normal recruitment on the opposite side with a unilateral denervated diaphragm, which would have identified them as possible candidates for ventilator weaning after diaphragm plication. Using the parameter of 1 diaphragm with no more than mild decreased recruitment and the second with no more than severe decreased recruitment best differentiated patients with a false-positive and false-negative rate of 1 of 12 and 1 of 13, respectively. The difference observed in specificity and sensitivity using this algorithm and the second algorithm presented in Table 6 are not significant. The side of decreased recruitment did not predict the side of pneumonia or atelectasis in the ventilator-weaned or failed-weaning subgroups.
Table 6.
Weaning as Predicted by Diaphragm Motor Unit Recruitment on Needle Examination
Using the EMG data, the two outliers from algorithm B would not have been predicted by spirometry data. Using the no recruitment data from algorithm C, 3 of 5 patients who had recruitment in both hemidiaphragms but were unable to wean would have been predicted by their spirometry data to fail to wean. The other two did not have documented spirometry data (Table 6).
DISCUSSION
The results demonstrate that needle EMG is a predictive tool in the evaluation of the weaning potential of ventilator-dependent patients with acute SCI. The demonstration that recruitment abnormalities that are obvious and gross resulted in a dramatic ability to distinguish patients who were able to wean from those who could not makes this a viable test to apply in this fashion. Its high sensitivity and specificity makes it an invaluable tool in program planning in this patient population. This is especially true given that recent studies have reaffirmed the safety of this technique (14). In this case series, no complications of bleeding or pulmonary injury were seen.
Bedside spirometry is effective in noting most patients with the ability to wean. Those cases in which spirometry fails were the result of unilateral diaphragm paralysis. In those cases, the increased burden on the one intact hemidiaphragm must cause fatigue, as demonstrated by adequate spirometry data but inability to wean. That would seem to be the weakness of bedside spirometry, that is, the inability of a single trial test to adequately evaluate fatigue over time. Perhaps more extensive spirometric evaluation would have identified this patient vulnerability. Needle EMG in those cases is able to objectively identify and define the magnitude of diaphragmatic dysfunction in patients with this clinical problem.
The ASIA level does affect one's ability to wean. However, there is a high degree of variability of the ability to wean in the C3 and C4 population. Innervation pattern of the diaphragm may play a role in this variability. The presence of anterior horn cell damage with maintained sensory function may be an issue as well because ASIA classification in the C3 and C4 levels relies on sensory evaluation only. The presence of neurapraxic nerve root injury could also play a role in this variability. In all cases, needle EMG of the diaphragm was able to distinguish those patients capable of weaning from the ventilator, regardless of ASIA level.
Fluoroscopic examination of the diaphragm was found to be nonpredictive in the ability to wean from the ventilator. Many factors may contribute to this. First, fluoroscopy is unable to identify hemidiaphragms affected by neurapraxia and likely to recover rapidly. Second, fluoroscopy is unable to distinguish a diaphragm with no motion from one that is partly denervated and still showing evidence of electrical integrity. If nerve continuity is present, the potential exists for cross-innervation and for subacute diaphragm recovery. On our rehabilitation unit, transporting a ventilator-dependent patient to radiology is a cumbersome activity requiring a nurse and respiratory therapist to assist in transport. This would be even more difficult in a freestanding rehabilitation facility that does not have in-house fluoroscopy capability. Knowing the limited value of the fluoroscopic examination of the diaphragm would avoid this inconvenience, the associated costs, and the patient exposure to fluoroscopic radiation.
Phrenic nerve conduction study was not predictive in the ability to wean. This is similar to the findings of Oo et al (5). An absent or attenuated study may be due to neurapraxia, atrophy, or axonotmesis. The inability of the nerve conduction study to distinguish these possibilities means that it is not very useful in predicting ventilator outcome. In addition, a normal motor nerve conduction study would be expected in a patient with a neurological injury above C4 and an upper motor neuron injury affecting diaphragm function. In such a patient, there would be little possibility of ventilator weaning. In addition, in the unusual situation in which an implantable defibrillator was placed, thus preventing nerve conduction study, it is important to note that phrenic nerve conduction studies are not helpful and, therefore, can be eliminated in the evaluation.
Study Limitations
Although the number of patients was fairly small, the spirometry and needle EMG data are compelling. A prospective study, conducted with a large sample is necessary before definitive conclusions can be drawn. In future research, it would be important to evaluate spirometry in all patients differentiated with no recruitment on needle EMG to see how well this combined analysis predicted subjects' ability to wean. This would make more detailed motor unit configuration and recruitment analysis on EMG unnecessary. Another component of any future study's design would be to add a spirometry measure of fatigue to see whether spirometry alone would be as effective as needle EMG in predicting weaning in patients with cervical SCI. A third utility would be to follow patients who fail to wean over time, especially those with some bilateral motor unit capability, to see whether they become able to wean at a later time. It would also be helpful to follow over time those who fail to wean due to unilateral diaphragm denervation to see whether later reinnervation or diaphragm plication leads to weaning.
REFERENCES
- Bannister LH, Berry MM, Williams PL, editors. Gray's Anatomy. New York: Churchill Livingstone; 1995. [Google Scholar]
- Jackson AB, Groomes TE. Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil. 1994;75:270–275. doi: 10.1016/0003-9993(94)90027-2. [DOI] [PubMed] [Google Scholar]
- Ledsome JR, Sharp JM. Pulmonary function in acute cervical cord injury. Am Rev Respir Dis. 1981;124:41–44. doi: 10.1164/arrd.1981.124.1.41. [DOI] [PubMed] [Google Scholar]
- Carter RE. Unilateral diaphragmatic paralysis in spinal cord injury patients. Paraplegia. 1980;18:267–273. doi: 10.1038/sc.1980.46. [DOI] [PubMed] [Google Scholar]
- Oo T, Watt JMW, Soni BM, Sett PK. Delayed diaphragm recovery in 12 patients after high cervical spinal cord injury. A retrospective review of the diaphragm status of 107 patients ventilated after acute spinal cord injury. Spinal Cord. 1999;37:117–122. doi: 10.1038/sj.sc.3100775. [DOI] [PubMed] [Google Scholar]
- Wicks AB, Menter RR. Long-term outlook in quadriplegic patients with initial ventilator dependency. Chest. 1986;90((3)):406–410. doi: 10.1378/chest.90.3.406. [DOI] [PubMed] [Google Scholar]
- McKinley WO. Late return of diaphragm function in a ventilator-dependent patient with a high cervical tetraplegia; a case report and interactive review. Spinal Cord. 1997;34:622–629. doi: 10.1038/sc.1996.112. [DOI] [PubMed] [Google Scholar]
- Lieberman JS, Cookill G, Nayak NN, French BN, Taylor RF. Serial phrenic nerve conduction studies in candidates for diaphragm pacing. Arch Phys Med Rehabil. 1980;61:528–531. [PubMed] [Google Scholar]
- Waters RL, Adkins RH, Yakura JS, Sie I. Motor and sensory recovery following complete tetraplegia. Arch Phys Med Rehabil. 1993;74:242–247. [PubMed] [Google Scholar]
- Waters RL, Adkins RH, Yakura JS, Sie I. Effect of surgery on motor recovery following traumatic spinal cord injury. Spinal Cord. 1996;34:188–192. doi: 10.1038/sc.1996.37. [DOI] [PubMed] [Google Scholar]
- Ditunno JF, Stover SL, Freed MM, Ahn JH. Motor recovery of the upper extremities in traumatic quadriplegia: a multicenter study. Arch Phys Med Rehabil. 1992;73:431–436. [PubMed] [Google Scholar]
- American Spinal Injury Association/International Medical Society of Paraplegia. International Standards for Neurological and Functional Classification of Spinal Cord Injury Patients, Revised 2000. J Spinal Cord Med. 2003;26((suppl 1)):S50–S56. doi: 10.1080/10790268.2003.11754575. [DOI] [PubMed] [Google Scholar]
- Kimura J. Electrodiagnosis in Diseases of Nerve and Muscle. 2nd Edition. Philadelphia, PA: FA Davis; 1983. [Google Scholar]
- Chiodo A, Goodmurphy C, Haig A. Diaphragm needle examination techniques evaluated in cadaveric specimens. Arch Phys Med Rehabil. 2006;87((8)):1150–1152. doi: 10.1016/j.apmr.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Bolton CF, Grand'Maison F, Parkes A, Shkrum M. Needle electromyography of the diaphragm. Muscle Nerve. 1992;15((6)):678–681. doi: 10.1002/mus.880150608. [DOI] [PubMed] [Google Scholar]
- Daube JR. AAEM mini-monograph #11: needle examination in clinical electromyography. Muscle Nerve. 1991;14((8)):685–700. doi: 10.1002/mus.880140802. [DOI] [PubMed] [Google Scholar]