Abstract
Background:
Primary spinal hydatid cysts are uncommon and account for 1% of all cases of hydatid disease. Echinococcus granulosus is most often responsible for the cyst hydatid. Intradural, extramedullary involvement is rare. When the cysts do not demonstrate typical magnetic resonance imaging findings, the differential diagnosis is more complex.
Method:
Case report.
Findings:
An isolated primary hydatid cyst of the spine in a 35-year-old man that appeared to be an arachnoid cyst on preoperative radiographic examination.
Conclusion:
Hydatid cysts that lack the typical radiographic appearance may be mistaken for arachnoid cysts. Misdiagnosis has serious implications for surgical intervention and long-term care.
Keywords: Myelopathy, Hydatidosis, Arachnoid cyst, Spinal extradural cyst, Echinococcus granulosus, Albendazole
INTRODUCTION
Hydatid cyst caused by the larval form of the parasitic organism Echinococcus granulosus is the most common cause of liver and lung hydatidosis. Primary spinal hydatid cyst is extremely rare (1–3). Spinal hydatid cysts are usually situated in the dorsal region and generate medullary or radicular symptoms according to their location (4). They give rise to fluctuating symptoms as an effect of internal change in pressure resulting from changes in the hydrostatic pressure of the cerebrospinal fluid caused by physical efforts, such as coughing and sneezing (5). Radiological diagnosis is usually demonstrated by magnetic resonance imaging (MRI) scans. Characteristic findings of hydatid disease are well known, but unusual imaging features and related complications are less frequently documented in the literature (6,7). When the cysts do not show characteristic MRI features, the differential diagnosis is quite difficult and the lesion can imitate different cystic pathology, as in our case. The management of hydatid cyst is always surgery, but incorrect preoperative diagnosis of these lesions can compromise management of the lesion or lead to complications related to cyst rupture intraoperatively.
CASE REPORT
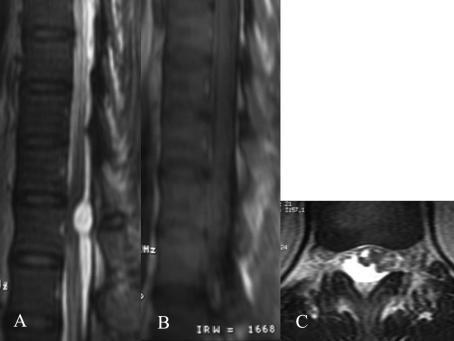
A 35-year-old man was admitted with complaints of progressive back pain and numbness and weakness of lower extremities bilaterally for 2 months and inability to walk for the last few days. There was no history of any other disease or trauma. Neurological examination revealed slight paraparesis and sensorial loss in both lower extremities. MRI revealed an intradural extramedullary well-demarcated cystic lesion that demonstrated low signal intensity on T1- and high signal intensity on T2-weighted images. The lesion appeared to be an arachnoid cyst on radiological examination (Figure 1A, B, C).
Figure 1. (A) Sagittal T2-weighted thoracic magnetic resonance image (MRI) demonstrates a well-demarcated intradural extramedullary hyperintense lesion with 1.5- × 1-cm dimensions at T12 vertebra corpus level. (B) The lesion is hypointense on T1-weighted sagittal MRI. (C) Axial T2-weighted MRI of T12 level reveals the hyperintense homogeneous cystic lesion displacing the left anterolateral spinal cord.
The patient underwent T11 and T12 total laminectomy and total excision of the cyst. Intraoperative microscopy indicated the presence of a hydatid cyst. The diagnosis of hydatid disease was subsequently confirmed histopathologically. The patient underwent comprehensive scanning postoperatively. On control MRI, total removal of the lesion was confirmed. Another systemic cystic lesion had not been found preoperatively on craniovertebral MRI, thorax computerized tomography (CT) and abdominal ultrasound.
Cystic hydatid disease is endemic to areas inhabited by carriers of E granulosus, that is, dogs and livestock (eg, cattle, goats, sheep). Humans contract the disease from direct contact with the infected animal or its feces or via contaminated food (2,3). This patient denied contact with any animals, including cats and dogs. Albendazole medication was prescribed. Postoperatively, the patient's symptoms improved within 8 months.
DISCUSSION
Spinal hydatid cysts account for 1% of all cases of hydatid disease and has rarely been reported in the literature. It was first described by Chaussier in 1807. E granulosus usually involves the liver and lungs in most cases. Disease usually spreads to the spine by direct extension from pulmonary, abdominal, or pelvic infestation and most commonly affects the dorsal region. Spinal involvement is reported in 50% of these cases with a mortality of 50% on an average of 5 years after the onset of symptoms (8). Spinal intradural and extramedullary involvement is rare. Primary vertebral hydatid disease without any other systemic involvement can occur with direct protovertebral venous shunts. Treatment is mainly total removal without cyst rupture followed by adjuvant pharmacological therapy. Careful dissection and irrigation around the cyst is essential to avoid intraoperative cyst rupture, which leads to recurrence.
MRI is the preferred imaging modality in the diagnosis of hydatid cysts. Hydatid cysts have a fairly consistent appearance on MRI. They are sausage like in shape with 2 dome-shaped ends and no debris in the lumen. Infrequently, they appear spherical. Cysts have thin walls and are regular with no septation. On T1-weighted images, the cyst wall may be isointense or reveal slightly lower signal than its contents, and T2-weighted images show a low-intensity rim surrounding the homogeneous hyperintense cyst content. The presence of the markedly hypointense cyst wall on T1- and T2-weighted MRI images is characteristic of hydatid disease (9).
Arachnoid cysts occur as single or multiple cysts and are frequently extradural. Because they have long T1 and T2 relaxation times, they demonstrate a homogeneous signal pattern like that of cerebrospinal fluid: hypointense on T1-weighted and hyperintense on T2-weighted images. One of the differential diagnoses of spinal arachnoid cyst is unilocular type-1 hydatid cyst. Unilocular type-1 hydatid cysts usually have thinner walls than their counterparts. However, arachnoid cysts are an exception because of the existence of decreased inflammatory response (10). Management of spinal arachnoid cysts can be conservative when cysts are small, asymptomatic, and without any evidence of cord compression. Management of spinal cyst hydatid should always be surgical removal and medical therapy. Misdiagnosis of spinal cyst hydatid as an arachnoid cyst will result in 2 potential sequelae. One is inadequate follow up of the patient because of lack of evidence of cord compression and clinical signs indicative of arachnoid cyst. The second is seeding of the organism during surgery and a high risk spreading the hydatid disease.
In this patient, the lesion was diagnosed as an arachnoid cyst initially; there was no radiological evidence for hydatid cyst. We planned our surgical approach based on clinical and radiological signs of cord compression. Intraoperative appearance of the cyst, however, was typical for hydatid cyst, enabling us to avoid the serious complications of a ruptured cyst.
CONCLUSION
Although primary spinal hydatid cysts are uncommon, the incidence of these lesions may be higher if we consider the lesions that could not be verified as hydatid cysts but simulated other cystic lesions radiologically and thus were managed conservatively. When hydatid cysts do not demonstrate typical MRI features, the lesion may mimic other cystic pathology. This can lead to inappropriate management or complications related to intraoperative cyst rupture.
Hydatid disease should be kept in mind when planning a surgical approach for cystic spinal lesions diagnosed as arachnoid cysts based on preoperative findings.
REFERENCES
- Karadereler S, Orakdogen M, Kilic K, Ozdogan C. Primary spinal extradural hydatid cyst in a child: case report and review of the literature. Eur Spine J. 2002;11:500–503. doi: 10.1007/s00586-002-0411-0. Epub 2002 May 9. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkan E, Cengiz SL, Cicek O, Erdi F, Baysefer A. Primary spinal intradural extramedullary hydatid cyst in a child: case report. J Spinal Cord Med. 2007;30:297–300. [PMC free article] [PubMed] [Google Scholar]
- Prabhakar MM, Acharya AJ, Modi DR, Jadav B. Spinal hydatid disease: a case series. Review. J Spinal Cord Med. 2005;28:426–431. doi: 10.1080/10790268.2005.11753843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prevo RL, Hageman G, Bruyn RP, Broeve G, van de Stadt J. Extended extradural spinal arachnoid cyst: an unusual cause of progressive spastic paraparesis. Clin Neurol Neurosurg. 1999;101:260–263. doi: 10.1016/s0303-8467(99)00050-5. [DOI] [PubMed] [Google Scholar]
- Bhojraj SY, Shetty NR. Primary hydatid disease of the spine: an unusual cause of progressive paraplegia. Case report and review of the literature. J Neurosurg. 1999;91:216–218. doi: 10.3171/spi.1999.91.2.0216. [DOI] [PubMed] [Google Scholar]
- Tsitouridis I, Dimitriadis AS. CT and MRI in vertebral hydatid disease. Eur Radiol. 1997;7:1207–1210. doi: 10.1007/s003300050275. [DOI] [PubMed] [Google Scholar]
- Tekkök IH, Benli K. Primary spinal extradural hydatid disease: report of a case with magnetic resonance characteristics and pathological correlation. Neurosurgery. 1993;33:320–323. [PubMed] [Google Scholar]
- Ozdemir MH, Ogun TC, Tasbas B. A lasting solution is hard to achieve in primary hydatid disease of the spine. Spine. 2004;29:932–9397. doi: 10.1097/00007632-200404150-00022. [DOI] [PubMed] [Google Scholar]
- Berk C, Ciftci E, Erdogan A. MRI in primary intraspinal extradural hydatid disease: case report. Neuroradiology. 1998;40:390–392. doi: 10.1007/s002340050608. [DOI] [PubMed] [Google Scholar]
- Turgut AT, Altin L, Topcu S, et al. Unusual imaging characteristics of complicated hydatid disease. Eur J Radiol. 2007;63:84–93. doi: 10.1016/j.ejrad.2007.01.001. Epub 2007 Feb 1. [DOI] [PubMed] [Google Scholar]