Abstract
Objective:
To describe the occurrence of finger autophagia in 5 persons with traumatic spinal cord injury and to present a discussion of putative causes and potential treatments.
Background:
Minor self-mutilating actions, such as nail biting and hair pulling, are common in humans and usually benign. In some circumstances, these behaviors are associated with obsessive-compulsive personality traits. In humans, self-injurious biting behaviors are well described in the setting of mental retardation and psychosis and in persons with Lesch-Nyhan syndrome. Rare cases of human autophagia in persons with intact cognition have been reported, most commonly in the setting of acquired nervous system lesions. After spinal cord injury, it has been suggested that this behavior constitutes a human variant of animal autotomy and a response to neuropathic pain.
Design:
Case presentation narrative.
Main Outcome Measures:
Photographic and radiological study, administration of Yale-Brown Obsessive-Compulsive Scale (YBOCS).
Findings:
In 5 patients with complete tetraplegia, pain in the hands was present in only one instance. The severity of autoamputation varied from minor to extreme. In all cases, damage was confined to analgesic body parts. In 3 cases, autophagia behavior was discovered in progress. Treatments included pharmacotherapy, counseling, and behavioral therapy, with mixed results. All patients were intelligent, willing to discuss their issues, and able to identify conditions of stress and isolation in their lives. Mild preinjury obsessive-compulsive behaviors, such as nail biting, were universal. On the YBOCS, only 1 patient scored in a range indicative of mild obsessive-compulsive symptomatology.
Conclusions:
This group exhibited heterogeneous medical, social, and cultural characteristics. A link between pain and self-injurious behavior could not be demonstrated. This behavior may be viewed as an extreme variant of nail biting, with potential ominous complications. Treatment strategies have been employed with mixed results.
Keywords: Spinal cord injuries; Tetraplegia; Pain; Obsessive-compulsive disorder; Nail biting; Autoamputation; Autophagia; Self-injurious behavior, Traumatic brain injury
INTRODUCTION
In humans, self-injurious behavior (SIB) is seen in the context of a wide array of congenital, psychiatric, and medical conditions (1–3). In some instances, these behaviors (eg, nail biting, hair pulling) are noted as benign habits. In others, destructive behaviors (finger autophagia, self-inflicted facial ulcerations) may be exhibited. The study of these behaviors is difficult from a methodological standpoint; SIB constitutes a heterogeneous condition with widely variable severity. Over 18 years, we encountered 5 patients with tetraplegia who engaged in self-injurious finger and upper limb biting. These patients were chosen for study in hopes of determining the causes and best treatments for this phenomenon.
SIB has been described in persons with a spinal cord injury (SCI), and 2 causative models are most commonly cited, either that this SIB represented expression of anxiety or that this was a direct response to pain in the targeted body part (4–6). Neither explanation seemed appropriate in our patients. For this reason, we attempted to characterize their predisposing comorbid conditions and clinical histories to gain a clearer picture of this phenomenon.
METHODS
Through review of case histories, medical records, and patient interviews, autophagia behavior in these patients was detailed. Because people disabled from SCI may constitute a vulnerable research group from a medical, financial, and psychological standpoint, Institutional Review Board approval was sought to oversee protection of confidentiality and to ensure that sensitive psychological information was gathered in a scientific and professional manner. All patients had an established relationship with one of the authors (S.M., F.F.). A structured telephone interview was developed under the auspices of the Institutional Review Board, incorporating a Yale-Brown Obsessive-Compulsive Scale (YBOCS), pain rating, and detailed questioning regarding current and historical medical, social, and psychological issues. The YBOCS was administered to measure historical and current obsessive-compulsive symptomatology. The YBOCS is a widely utilized measurement tool used to measure obsessive-compulsive symptom severity (7). This tool is composed of questions about current or past behaviors that help identify obsessive-compulsive symptoms, such as ritualized handwashing, abnormal eating behaviors, and hoarding. A score of 16 or higher on the YBOCS is commonly used in pharmaceutical research to identify patients with significant obsessive-compulsive symptomatology. A verbal numerical pain scale (0–10) (8) was used to obtain pain ratings, and a history regarding pain patterns and symptomatology was documented. The YBOCS and pain history were undertaken through telephone interview in all 5 patients. During the telephone interview, subjects were asked to reflect upon psychological or social stressors (social isolation, financial difficulties, and relationship issues) that may have existed in concert with their autophagia behavior. In addition, inquiry into feelings of gratification or pleasure associated with this behavior was undertaken.
Patients were asked to rate their current pain and whether the same type of pain was present at the time of their autophagia. Due to the limitations of recall, superimposed upon the restricted face validity of a self-report, no attempt was made to rate pain at the time of their SIB. Telephone YBOCS administration was carried out according to the methods described by Taylor; questions are posed in the past tense to survey any recollected history of a targeted obsessive or compulsive behavior (9).
RESULTS
When examined as a group, pain in the targeted limb(s) was reported in only 1 of 5 patients (Table 1). In addition, none reported nonpainful sensory perversions or paresthesias in the affected limb. In 2 other patients, chronic symptoms of central deafferentation pain in the abdomen and pelvis were reported, isolated from the targeted limbs. For this group, the mean age at initial SCI was 35.0 ± 14.4 years. Onset of SIB was delayed after injury in all patients (onset mean 4.6 ± 1.6 years post SCI). At the time of onset of SIB, this group of patients averaged 39.2 ± 13.5 years of age. All 5 patients possessed the muscle function to bring hands to the mouth, although all had complete tetraplegic lesions (3 ASIA Impairment Scale [AIS] C5 A, 2 AIS C6 A) (10). Sensation was absent in all of the body parts targeted by the SIB. In 3 cases, the autophagia was discovered in progress. None of the patients was employed. Descriptions of SIB for each patient are detailed as follows:
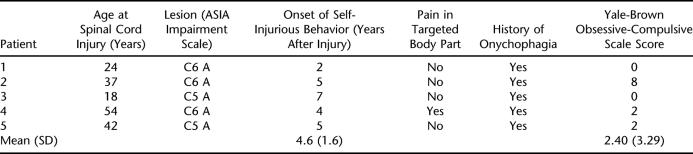
Table 1.
Descriptive Information on 5 Patients with Autophagia
Case 1
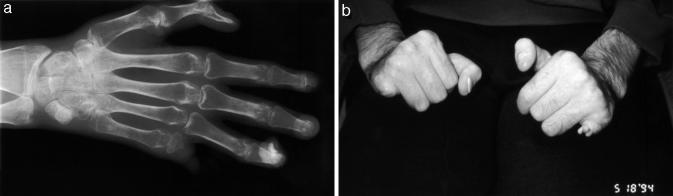
A 45-year-old, high school–educated, unmarried man with a C6 International Classification A neurological lesion was injured 21 years ago in a motorcycle collision. He has been unemployed since the date of injury. His SIB began 2 years after injury. His medical history, after injury, is otherwise notable only for a single ischial pressure ulcer developing 18 years after injury. The SIB continued over 2 years until multiple phalanges were autoamputated (Figures 1a and b). He did not seek medical care for his fingers during this time and received no antibiotic or other treatments for finger injury. He tried to use gloves to stop the behavior but found them uncomfortable. His SIB resolved spontaneously without treatment. He was unable to identify extraordinary stressors in his life that might have precipitated the SIB but acknowledged feelings of social isolation related to his leaving home rarely and his mother's serving as a full-time care giver. Likewise, he was unable to identify a reason for stopping the behavior, although he noted that he was embarrassed by the hand deformity and was likely to offer vague explanations when questioned about the appearance of his hands. The patient reported severe nail biting behavior before his SCI, but his YBOCS testing showed a score of 0.
Figure 1a and b. Autoamputation of bilateral small finger distal phalanges and terminal proximal phalanges, resulting in chronic healed, callus-covered bony spicules.
Case 2
This 55-year-old, unmarried, high school–educated, unemployed man with a C6 International Classification A lesion was injured 16 years ago in a diving accident. His SIB developed 5 years after injury. His medical history is notable for multiple pressure ulcers and multiple episodes of pneumonia requiring chronic tracheostomy placement for secretion management. His SIB resulted in permanent damage to the distal phalanges (Figure 2). The patient reported no pain history. He acknowledged feelings of social isolation, lifelong extraordinary family stress, and a chronic struggle with alcoholism and smoking. He had been successful in abstinence from alcohol since the day of his SCI. He acknowledged engaging in fingernail biting since childhood. The patient accepted psychological counseling for his SIB, along with medication management with fluoxetine and fluvoxamine. The patient stopped both medications due to side effects described as drowsiness. Gloves were tried but not tolerated due to discomfort from the heat on his hands. He was treated with multiple courses of antibiotics for cellulitis associated with finger injury. He no longer takes psychoactive medications, and the finger-biting behavior has improved over the last 2 years. Although he reports intermittent “relapses” of the behavior, he has not required medical treatment for his hands, and he has sustained no further permanent damage. He discussed his autophagia in a frank and open manner. His YBOCS score was 8.
Figure 2. Autoamputation of the right small finger distal phalanx and terminal proximal phalanx, along with damage to the nail beds of middle and ring fingers. The left hand was undamaged.
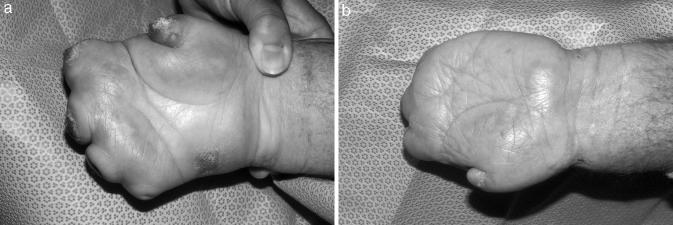
Case 3
This 68-year-old, married, high school–educated farmer sustained a C5 International Classification A lesion from a fall 50 years ago. He was initially seen in the hospital after being referred from a local doctor for tertiary level urological care. He started SIB 7 years after injury, and over the course of 10 years accomplished total auto amputation of all digits (Figures 3a and b). He remembered several courses of outpatient antibiotic treatment for “skin infection” during the period of his autophagia. His medical history is notable for geographical isolation from medical care, that is, in a rural setting. He has a long history of severe central deafferentation pain in the low back and legs but no hand pain. His SIB resolved after all his fingers were removed. He otherwise reported no unusual stresses in his life. He reported having a loving and supportive family and minimal other medical problems and described a very active postinjury lifestyle on his family farm. Although intermittent use of gloves had failed to prevent finger autoamputation, he wore gloves when in the presence of strangers to “prevent having to explain what happened.” Despite this, he discussed his autophagia in a forthright and open manner. His YBOCS score was 0.
Figure 3a and b. Complete autoamputation of all 10 digits to the level of the metacarpal-phalangeal joints.
Case 4
This 56-year-old, high school–educated, married homemaker with a C6 International Classification A injury noted onset of SIB 4 years after injury, associated with the initiation of pain in her hands, after tendon transfer surgery. Her postinjury medical history was unremarkable. The postoperative pain was localized to the hands and was described as aching and burning. She received treatment with narcotics and tricyclic antidepressant medication, without significant relief. She began biting her fingers 5 days postoperatively (Figure 4). Antibiotics were given in light of apparent damage to epidermis and the nail beds. Aversive training by painting the nails with vinegar was tried but did not suppress the behavior. The patient agreed to use gloves, which reduced the rate of damage to the fingers. Her autophagia behavior resolved over 3 months, coincident with spontaneous resolution of her postsurgical hand pain. No unusual psychological stresses were identified by the rehabilitation psychologist during her hospital stay for rehabilitation after her tendon transfers. She acknowledged a lifetime of nail biting, which persists to date, with no further damage to other soft tissues. Her YBOCS was 2.
Figure 4. Nail bed destruction of the index through small fingers on the right and the left middle, ring, and small fingers.
Case 5
This 59-year-old, high school–educated, married homemaker sustained a C5 International Classification A spinal cord injury as a complication of cervical disk surgery at age 42 years. SIB began 5 years after injury, consisting of biting forearms and digits. Medical history after injury was notable for treatment of depression and central deafferentation pain. Her pain was experienced as a burning sensation, limited to the lumbar region, buttocks, and hips. The patient had extensive treatment for her pain prior to the onset of SIB, ranging from multiple medications to bilateral cingulate gyrectomy. She had no upper limb pain. Her SIB came to light after damage to the upper limbs extended to the nail beds. She also gnawed her radial forearms (Figure 5). Autophagia reduced slightly with fluoxetine treatment, use of gloves, and bandaging the hands and arms. No unusual psychological stresses were reported by the patient, who after extensive counseling elected to have removal of all her teeth, which were in very poor repair. The dental extraction resulted in the resolution of her self-inflicted tissue damage. Six months later, dentures were fitted. The patient remained on fluoxetine at 60 mg once a day and has had mild, intermittent recurrence of SIB after 6 years of follow up, confined to superficial skin gnawing without significant soft-tissue injury. Her YBOCS score was 2.
Figure 5. Self-inflicted damage to the skin of the right ulnar forearm and to the nail bed of the left small finger (covered with bandage).
DISCUSSION
These examples of self-mutilation inevitably lead to questions regarding the etiology of such maladaptive behavior (11). Finger and fingernail biting is seen in humans with mental retardation and severe mental illness, as well as in persons with congenital insensitivity to pain and Lesch-Nyhan syndrome. The syndrome of onycho-pathomimia (12) has also been described; it is characterized by purposeful self-induced trauma for the purpose of initiating false legal claims. The study of this group of patients was undertaken in hopes of identifying patterns or unifying psychological, social, or medical characteristics that might, in turn, lead to a better treatment model. Biological, behavioral, and psychopathological models have been proposed to explain the wide range of human SIB: these models may help us understand the self-mutilation seen in our group of patients.
Biological Model of SIB
The occurrence of autophagia in SCI has been documented previously in medical case reports (4–6). Previous authors familiar with the study of pain in the rodent model have suggested a biological etiology of human SIB, drawing a connection between SIB in persons with neurological lesions and the autophagia response that is seen in lower animals after induction of a painful stimulus. Studies of biological induction of SIB are legion in the rodent experimental model; SIB can be induced by drugs and by induction of (presumably painful) experimental lesions both inside and outside the nervous system. The lack of a consistent pattern of limb pain in our series of patients speaks to a more complex underlying mechanism for this behavior. Although pain complaints were present in 3 of 5 patients, only 1 patient reported pain in the targeted limb. Pain is a common comorbid condition after SCI, with prevalence in the chronic phase of injury estimated between 48 and 94% (13,14). Limb autotomy, or autoamputation, may be seen as a response to pain in the targeted limb. It is possible, however, that SIB is exacerbated by psychological and medical distress and that pain in remote body regions can predispose the patient to SIB (15).
Emphasis on the rodent model of SIB ignores the vast psychiatric literature describing the many forms of SIB in humans. These studies identify a complex mixture of behavioral, social, and biological risk factors for SIB and describe a spectrum of SIB that ranges from benign habit to the type of anatomically mutilating behavior seen in our patients.
Social and biological correlates of SIB are seen in nonhuman mammals; self-mutilation behavior is well recognized in circuses, zoos, and laboratories (1). Self-biting, head slapping, and pathological scratching have been studied in the monkey model and have been correlated with partial social isolation (ie, deprivation of physical contact but not visual and auditory contact) (16). The classic studies of Kluver and Bucy (17) noted SIB in macaques with temporal lobe dysfunction and regarded SIB as a byproduct of sexual self-stimulation. In higher animals, self-mutilation is also noted to occur as a complex and pathological variant of grooming behavior, seen with excessive attention to hair (trichotillomania) or fur, nails, or hand washing.
Behavioral and Psychological Models of SIB
Our patients shared common characteristics of high, complete neurological injuries and the experience of markedly diminished central sensory input. “Deafferentation theory” (18) assumes that organisms with reduced sensory input may seek stimuli to reach the optimal level of arousal. Numerous negative physiological, cognitive, perceptual, and behavioral effects are associated with sensory deprivation. Sensory deprivation has been studied in tetraplegia and may be apparent in the clinical setting, manifested by preferences for high ventilator volumes or by excessive needs for oral gratification or fluid intake. For persons with acute SCI, who are limited in mobility and dexterity, few opportunities to compensate for sensory deprivation are available.
None of our patients recalled experiences of any sensation, pleasant or unpleasant, through their SIB. None reported production of an autonomic rush (piloerection, flushing, headache, change in body temperature) through finger biting. Oral gratification needs may propagate this behavior in patients who may be restricted in accessing such items as food, drink, cigarettes, and chewing gum. All 5 patients described here, by virtue to their disability and impaired hand function, required substantial caregiver assistance for feeding and access to these items. It is conceivable that the SIB noted in these patients represents a behavior designed to provide psychological or physiological stimulation, in compensation for their neurological or functional deficits (19).
Decreased stimulation to the central nervous system has been demonstrated to change cortical arousal and cognition (20). Research on sensory deprivation in people with SCI has shown that people with longstanding SCI perform better on vigilance tasks than those recently injured and able-bodied controls (21). Sleep patterns are distorted in persons with sensory and social isolation after SCI (22), and aberrant behavior is noted more frequently in SCI patients who have few family members visiting them in the hospital (23).
An in-depth study of this issue by Richards (21) detailed the effects of afferent loss attributable to SCI and its impact on cortical processing and task efficiency. He found that improved auditory processing after SCI probably reflected a higher level of motivation in the test setting, rather than an intrinsic change in cognitive processing. Absence of tactile sensation and physical immobilization may be less important than the social isolation experienced by these persons over the course of their lifetimes. Environmental stimuli and self-stimulation may act to compensate for somatosensory losses (24). Due to the limitations of our retrospective study, we did not screen or evaluate our patients for the possibility of traumatic brain injury. Many people with traumatic SCI demonstrate signs of concomitant brain injury, and the incidence is highest in persons with tetraplegia (25). Four of 5 patients reviewed in this report had sustained high-velocity traumatic injury to the cervical spinal cord, raising the possibility that the poor impulse control often seen with brain injury played a role in their SIB.
All of our patients, who targeted their hands during their autophagic episodes, noted a history of nail biting before their SCI. Does autophagia represent a “crime of opportunity,” an extreme variant of nail biting in persons who lack protective sensation in their fingertips? In the literature on human autophagia, the mutilation is confined to insensate body parts. The 100% incidence of pre-SCI nail biting behavior in our group is not unexpected (26). Nail biting is a common phenomenon and is seen in persons of all ages, degrees of intelligence, and economic status (27). Most authors state that it occurs in approximately half of all children (28) and in 4.5 to 23% of adults (29). In children, this behavior is not linked to psychological disturbances. Nail biting has long been viewed as a systematic behavior reflecting emotional distress or anxiety (30). Although nail biting is a fringe item on the psychiatric review of systems and is a common finding in patients with pathologies ranging from sociopathy to obsessive-compulsive disorders (31), it is usually viewed as a vague, psychiatric microsymptom (32) of little diagnostic significance.
Persons who self-inflict significant tissue damage to their fingernails fall under the clinical syndrome of onychophagia, a disorder that has been studied in some depth from both a behavioral and a psychodynamic perspective. Onychophagia is among the best studied of the self-harming behaviors, which include both indirect (eg, chronic alcoholism) and direct (single-episode suicide) types (33). In the psychopathology literature, this behavior is most often linked with obsessive-compulsive spectrum disorders. The study of our patients with the YBOCS attempted to screen for compulsive symptom severity as a possible precipitant of SIB. The YBOCS is an instrument utilized in determining the extent of historical and existing obsessive-compulsive traits (7). When used in isolation, however, symptom measurement through the YBOCS is not sufficient to make the diagnosis of obsessive-compulsive personality disorder. This diagnosis is a clinical one, based upon the patients' exhibition of a range of behaviors. It should be noted that the YBOCS tool asks about present as well as past behavior and includes some questions regarding obsessive-compulsive symptomatology that may have limited relevance to patients with tetraplegia, in light of their physical impairments. For example, individuals with tetraplegia would have limited opportunity to “line(s) up clothes, canned goods, or shoes in a fixed order.” Scores on the YBOCS scale were quite low overall, indicating a low incidence of obsessive-compulsive symptoms in this group. The fact that our patients with SCI scored uniformly low on the YBOCS measure of obsessive-compulsive symptomatology leads us to look for an alternative explanation from a psychological perspective.
In its mild form, nail biting is compared with nervous habits, such as thumb sucking, giggling, twitching, and hair twirling. Persistent, severe adult nail biting is often viewed in western society as an “outburst phenomenon” through which anxiety, stress, or fears are released. None of the patients reported that their SIB reduced their distress level. There is little empirical research that supports this “tension reduction” theory. Children who bite their nails have not been reported to be any more anxious than children who do not (34), although higher levels of anxiety in adults with nail biting have been reported (35). In its early stages, nail biting may serve as a coping mechanism, but it progresses into a simple habit (36). In severe cases, however, the underpinnings of this behavior may not be unlike those in eating disorders, in which nail biting is commonly seen. In these groups, the behavior may be linked to a quest to control psychological issues by physically altering the body, the somatization of psychological conflict (37–39). It is difficult to imagine that the type of severe mutilation behavior seen in the worst cases in our series of persons with complete tetraplegia did not arise in concert with significant psychological distress. All of our patients were quick to acknowledge feelings of social isolation that began after the onset of their paralysis. All identified this isolation as intrinsic to their paralysis, although none could identify a temporal link between the onset of social isolation and the onset of SIB. The psychological study of SIB is very complex; ritualistic or repetitive thoughts or behaviors may be considered the observed manifestations of a wide range of disorders ranging from mania to the ruminations associated with major depressive illness. Four of the 5 patients in our group had received medical treatment for depression at some time after their injury, and 3 of them were taking antidepressant medications at the outset of their SIB. Our literature review failed to find any evidence that depression increased the likelihood of SIB.
Our patients readily acknowledged stress and anxiety in their lives, but none went so far as to ascribe their SIB to this cause.
Treatment
Medical treatment of SIB was attempted in 3 of these patients, who were seen by medical personnel while the SIB was in progress. Two of these patients had pain. In one instance the pain was self-limited; in the other patient, extreme measures were undertaken to control central deafferentation pain in a body region remote to the targeted upper limb. In all 3, treatment fell back upon the use of psychoactive medications and behavioral and environmental modifications. These treatments were consistent with a psychiatric model of SIB treatment, inasmuch as anxiety or associated depressive symptomatology may have precipitated such extreme behavior (40,41). Again, experience with treating other maladaptive habitual oral behaviors (overeating, smoking, drinking alcohol) may be relevant (42). Fluoxetine has been used to treat SIB, in the setting of low obsessive-compulsive symptomatology (43), but was ineffective in one of our patients and marginally effective in symptom suppression in another.
A study of human onychophagia treatment by Leonard and others (29) noted that clomipramine was significantly better than desipramine in reducing SIB. The authors felt that its relative greater efficacy could be traced back to a greater anxiolytic effect and to the recognized usefulness of clomipramine in the treatment of obsessive-compulsive disorder. For the single patient with a history of mild obsessive-compulsive symptoms, we chose to initiate treatment with fluvoxamine in light of its recognized clinical efficacy in obsessive-compulsive disorder. This patient discontinued taking the drug after 3 weeks due to feelings of drowsiness, with no relief from SIB.
Effective behavioral treatments, including covert sensitization, relaxation training, and habit reversal treatments, have been described in adult onychophagia (44). These treatments commonly include 3 steps: (a) awareness training to sensitize the patient to the occurrence of the behavior, (b) teaching the patient a competing response or an alternative behavior to nail biting (eg, making a tight fist), and (c) follow-up social support. This type of treatment was not applied in our patients due to limited contact and resources. Passive treatments of SIB were attempted in 3 of our patients. Contingent glove wearing is an effective treatment of SIB in adolescents (45). All patients tried wearing gloves, but the gloves were modestly effective in only 1 instance (Case 4). All of these patients were initially in favor of this intrusive method of aversive conditioning, but 2 patients removed the gloves after less than 7 days of wear. Limited hand function in these patients made glove wear excessively restrictive, and all complained of heat and discomfort. One patient underwent elective removal of all of her teeth. This resolved her SIB for 2 years; her finger biting recurred on an intermittent basis after she raised the money needed to buy dentures. On the basis of 3 studies (46–48), aversive training (painting the nails with a bitter substance) was tried in 1 patient (Case 4) but was ineffective.
CONCLUSION
This case review, combined with a brief cross-sectional survey, failed to find substantial evidence of autophagia related to pain in the targeted body part or a consistent pattern of compulsive symptomatology in 5 patients with tetraplegia and SIB. This group exhibited heterogeneous medical, socioeconomic, and cultural characteristics. The retrospective nature of our study of conditions associated with SIB has many limitations. Although the experience of psychological distress was common in our patients, they were asked to synthesize and recall events, feelings, and behaviors that may have occurred several years ago. In addition, the face validity of a historical self-report survey may always be under question when the traits examined might be embarrassing or uncomfortable for the patient to discuss.
The presence of a complete neurological injury that rendered the afflicted body parts insensate made up the only universal finding in this group. All of our patients reported nail biting behavior that predated their SCI. The high incidence of nail biting in the general population prevents us from drawing definite conclusions about the ubiquitous presence of this behavior in our patients. Inasmuch as nail biters target insensate body parts, this SIB might be viewed as an extreme variant of nail biting with potentially ominous complications. Very mild compulsive habits (eg, finger biting) may become destructive when fingers are insensate.
Clinicians must be aware of the consequences of this behavior after SCI. To date, treatments have focused on behavioral management, psychotherapy, and pharmacotherapy with mixed results. The precipitants of autophagia in persons with SCI are unclear. When this phenomenon is encountered in the future, a more rigorous approach to psychological evaluation and treatment might shed more light into the causes of this behavior and, thereby, guide a more sensible treatment approach.
REFERENCES
- Jones IH, Barraclough BM. Auto-mutilation in animals and its relevance to self-injury in man. Acta Psychiatr Scand. 1978;58:40–47. doi: 10.1111/j.1600-0447.1978.tb06918.x. [DOI] [PubMed] [Google Scholar]
- Waisman M. Picker, plucker and impostors: a panorama of cutaneous self mutilation. Postgrad Med. 1965;38:620–630. doi: 10.1080/00325481.1965.11696846. [DOI] [PubMed] [Google Scholar]
- Rincover A. Behavioral research in self injury and self stimulation. Psych Clin N Am. 1986;9:755–766. [PubMed] [Google Scholar]
- Marmolya G, Yagan R, Freehafer A. Acro-osteolysis of the fingers in a spinal cord injury patient: a case report. Spine. 1989;14:137–139. doi: 10.1097/00007632-198901000-00033. [DOI] [PubMed] [Google Scholar]
- Vogel LC, Anderson CJ. Self-injurious behavior in children and adolescents with spinal cord injuries. Spinal Cord. 2002;40:666–668. doi: 10.1038/sj.sc.3101377. [DOI] [PubMed] [Google Scholar]
- Dahlin PA, Van Buskirk NE, Novotny RW, et al. Self-biting with multiple finger amputations following spinal cord injury. Paraplegia. 1985;23((5)):306–318. doi: 10.1038/sc.1985.48. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychol. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- McCaffery M, Pasero C. Assessment: Underlying complexities, misconceptions, and practical tools (Chapter 3) In: McCaffery M, Pasero C, editors. Pain: Clinical Manual for Nursing Practice. 2nd ed. New York, NY: Mosby; 1999. pp. 63–64. [Google Scholar]
- Taylor S, Thordarson DS, Spring T, et al. Telephone-administered cognitive behaviour therapy for obsessive-compulsive disorder. Cogn Behav Ther. 2003;32:13–25. doi: 10.1080/16506070310003639. [DOI] [PubMed] [Google Scholar]
- American Spinal Injury Association. International Standards for Neurological Classification of Spinal Cord Injury, Revised 2002. J Spinal Cord Med. 2003;26((suppl 1)):S50–S56. doi: 10.1080/10790268.2003.11754575. [DOI] [PubMed] [Google Scholar]
- Parrott HJ, Murray BJ. Self-mutilation: review and case study. Int J Clin Pract. 2001;55:317–319. [PubMed] [Google Scholar]
- Ronchese F. Peculiar nail anomalies. Arch Dermatol. 1951;63:565–580. doi: 10.1001/archderm.1951.01570050023003. [DOI] [PubMed] [Google Scholar]
- Frost FS. Spinal cord medicine: In: Braddom R, ed. Physical Medicine and Rehabilitation. Philadephia, PA: WB Saunders; 2000:1230–1282
- Bryce TN, Ragnarsson KT. Pain after spinal cord injury. Phys Med Rehab Clin N Am. 2000;11:157–168. [PubMed] [Google Scholar]
- Mailis A. Compulsive targeted self-injurious behaviour in humans with neuropathic pain: a counterpart of animal autotomy? Four case reports and literature review. Pain. 1996;64:569–578. doi: 10.1016/0304-3959(95)00173-5. [DOI] [PubMed] [Google Scholar]
- Cross HA, Harlow HF. Prolonged and progressive effects of partial isolation on the behaviour of macaque monkeys. J Exp Res Pers. 1965;1:39–49. [Google Scholar]
- Kluver H, Bucy PC. Preliminary analysis of functions of the temporal lobe in monkeys. Arch Neurol Psychiat. 1939;42:979–1000. [Google Scholar]
- Hodes R. Electrocortical synchronization resulting from reduced proprioceptive drive caused by neuromuscular blocking agents. Electroencephalogr Clin Neurophysiol. 1962;14:220–232. doi: 10.1016/0013-4694(62)90032-9. [DOI] [PubMed] [Google Scholar]
- Crossman MV. Sensory deprivation in spinal cord injury—an essay. Spinal Cord. 1996;34:573–577. doi: 10.1038/sc.1996.102. [DOI] [PubMed] [Google Scholar]
- Richards JS, Seitz MR, Eisele WA. Auditory processing in spinal cord injury: a priliminary investigation from a sensory deprivation perspective. Arch Phys Med Rehabil. 1986;67:115–117. doi: 10.1016/0003-9993(86)90119-x. [DOI] [PubMed] [Google Scholar]
- Richards JS, Hirt M, Melamed L. Spinal cord injury: a sensory restriction perspective. Arch Phys Med Rehabil. 1982;63:195–199. [PubMed] [Google Scholar]
- Adey WR, Bors E, Porter RW. EEG sleep patterns after high cervical lesions in man. Arch Neurol. 1968;19:277–383. doi: 10.1001/archneur.1968.00480040043003. [DOI] [PubMed] [Google Scholar]
- Krishnan KR, Glass CA, Turner SM, et al. Perceptual deprivation in the acute phase of spinal injury rehabilitation. J Am Paraplegia Soc. 1992;15:60–65. doi: 10.1080/01952307.1992.11735863. [DOI] [PubMed] [Google Scholar]
- Richards JS, Meredith RL, Nepomuceno C, et al. Psycho-social aspects of chronic pain in spinal cord injury. Pain. 1980;8:355–366. doi: 10.1016/0304-3959(80)90079-2. [DOI] [PubMed] [Google Scholar]
- Richards JS, Brown L, Hagglund K, et al. Spinal cord injury and concomitant traumatic brain injury: results of a longitudinal investigation. Am J Phys Med Rehabil. 1988;67:211–216. doi: 10.1097/00002060-198810000-00005. [DOI] [PubMed] [Google Scholar]
- Ellerbroek WC. Personal disarmament: nail-biting as a behavior. J Am Soc Psychosom Dent Med. 1978;25:7–11. [PubMed] [Google Scholar]
- Pennington LA. The incidence of nail biting among adults. Am J Psychiatry. 1945;102:241–244. [Google Scholar]
- Singer P, Gibson GH. Unilateral onychodystrophy secondary to nail biting. Cutis. 1988;42:191–192. [PubMed] [Google Scholar]
- Leonard HL, Lenane MC, Swedo SE, et al. A double-blind comparison of clomipramine and desipramine treatment of severe onychophagia (nail biting) Arch Gen Psychiatry. 1991;48:821–827. doi: 10.1001/archpsyc.1991.01810330045007. [DOI] [PubMed] [Google Scholar]
- Morley DS. Psychophysiological reactivity to stress in nail biters. Int J Neurosci. 2000;103:139–154. doi: 10.3109/00207450009003260. [DOI] [PubMed] [Google Scholar]
- Walker BA, Zinkind E. Relationship of nailbiting to sociopathy: brief communication. J Nervous Mental Dis. 1977;164:64–65. doi: 10.1097/00005053-197701000-00011. [DOI] [PubMed] [Google Scholar]
- Cavaggioni G, Romano F. Psychodynamics of onychophagists. Eat Weight Disord. 2003;8:62–67. doi: 10.1007/BF03324990. [DOI] [PubMed] [Google Scholar]
- Kahan J, Pattison EM. Proposal for a distinctive diagnosis: the deliberate self-harm syndrome. Suicide Life Threatening Behav. 1984;14:17–35. doi: 10.1111/j.1943-278x.1984.tb00334.x. [DOI] [PubMed] [Google Scholar]
- Deardorff PA, Finch AJ, Royall LR. Manifest anxiety and nail-biting. J Clin Psychol. 1974;30:378–379. doi: 10.1002/1097-4679(197407)30:3<378::aid-jclp2270300348>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Klatte KM, Deardorff PA. Nailbiting and manifest anxiety of adults. Psychol Reports. 1981;1:48–82. doi: 10.2466/pr0.1981.48.1.82. [DOI] [PubMed] [Google Scholar]
- Westling L. Fingernail biting: literature reviews and case reports. Cranio. 1988;6:182–187. doi: 10.1080/08869634.1988.11678237. [DOI] [PubMed] [Google Scholar]
- Wells JH, Haines J, Williams CL. Severe morbid onychophagia: the classification as self-mutilation and a proposed model of maintenance. Aust N Z J Psychiatry. 1998;32:534–545. doi: 10.3109/00048679809068328. [DOI] [PubMed] [Google Scholar]
- Tosti A, Peluso AM, Bardazzi F, et al. Phalangeal osteomyelitis due to nail biting. Acta Derma Venereol (Stockh). 1994;74:206–207. doi: 10.2340/0001555574206207. [DOI] [PubMed] [Google Scholar]
- Waldman BA, Frieden IJ. Osteomyelitis caused by nail biting. Pediatr Dermatol. 1990;7:189–190. doi: 10.1111/j.1525-1470.1990.tb00279.x. [DOI] [PubMed] [Google Scholar]
- Coppola RJ, Rolek DF. A neuropharmacologic approach to self-mutilating behavior. J Am Osteopath Assoc. 1975;74:555–557. [PubMed] [Google Scholar]
- Wadden P, Pawliuk G. Cessation of nail-biting and bupropion. Can J Psychiatry. 1999;44:709–710. [PubMed] [Google Scholar]
- Davidson AM, Denney DR, Elliott CH. Suppression and substitution in the treatment of nailbiting. Behav Res Ther. 1980;18:1–9. doi: 10.1016/0005-7967(80)90063-7. [DOI] [PubMed] [Google Scholar]
- Velazquez L, Ward-Chene L, Loosigian SR. Fluoxetine in the treatment of self-mutilating behavior. J Am Acad Child Adolesc Psychiatry. 2000;39:812–814. doi: 10.1097/00004583-200007000-00009. [DOI] [PubMed] [Google Scholar]
- Twohig MP, Woods DW. Evaluating the efficacy of habit reversal: comparison with a placebo control. J Clin Psychiatry. 2003;64:40–48. doi: 10.4088/jcp.v64n0109. [DOI] [PubMed] [Google Scholar]
- Luiselli JK. Contingent glove wearing for the treatment of self-excoriating behavior in a sensory-impaired adolescent. Behav Modif. 1989;13:65–73. doi: 10.1177/01454455890131004. [DOI] [PubMed] [Google Scholar]
- Manavbasi I, Kayikcioglu A. Protective effect of chili against autocannibalism. Plast Reconstr Surg. 2000;106:519–521. doi: 10.1097/00006534-200008000-00068. [DOI] [PubMed] [Google Scholar]
- Bucher BD. A pocket-portable shock device with application to nailbiting. Behav Res Ther. 1968;6:389–392. doi: 10.1016/0005-7967(68)90072-7. [DOI] [PubMed] [Google Scholar]
- Rosenthal TL, Linehan KS, Kelley JE, et al. Group aversion by imaginal, vicarious and shared recipient-observer shocks. Behav Res Ther. 1978;116:421–427. doi: 10.1016/0005-7967(78)90013-x. [DOI] [PubMed] [Google Scholar]