Abstract
Objectives
To develop and test the feasibility and acceptability of a structured design for a massage therapy clinical trial that included a treatment arm designed to control for the non-specific effects of a massage-therapy intervention.
Design
Pilot randomized controlled clinical trial
Setting
University integrated medicine research clinic
Interventions
Participants were randomized to a structured Swedish-style massage therapy intervention, a light-touch bodywork control intervention, or usual medical care. Details of the interventions are provided.
Main Outcome Measures
The primary outcome measures were the adherence of the participants to the study protocol and the perception of the intervention experience.
Results
Forty-four participants were randomized. Participants often found adherence to the twice-weekly outpatient bodywork interventions to be somewhat difficult; while, overall, 84% of participants completed the study, only 76% of those in an intervention arm successfully completed the trial. Participants randomized to the massage arm expressed uniformly positive attitudes both before and after the intervention. While some participants randomized to the light-touch bodywork arm initially expressed some reservations about their randomization assignment, all participants available for interview were pleased with their experience after the intervention period.
Conclusions
The proposed design was found to be relatively straightforward to implement and acceptable to participants. Early disappointment with not receiving massage therapy expressed by the light-touch intervention participants dissipated quickly. Twice-weekly outpatient intervention appointments were found to be highly burdensome for many patients actively undergoing chemotherapy, thus reducing adherence.
Introduction
Massage therapy is a promising modality that currently lacks a solid evidence base to better understand its benefits and risks. While there are many different forms of massage and bodywork, Swedish-style massage is the most widely practiced and studied massage therapy style in the United States. It is a system of long strokes, kneading and friction techniques on the more superficial layers of the muscles, combined with active and passive movements of the joints. Swedish-style massage focuses on muscle relaxation and is often used for stress reduction or after strenuous physical activity.
There have been several small studies examining massage therapy for a variety of health conditions. The main documented physiological benefits attributed to Swedish-style massage include a reduction in cortisol levels (1, 2) and creatine kinase (2), as well as increases in immune function, most notably neutrophil and natural killer cell count (1, 2). Numerous psychological benefits have also been reported, including stress reduction (3, 4), improved quality of life (4), and improvement in wake-sleep cycles (3, 4). The combination of these physical and psychological effects makes massage a promising therapy for multi-dimensional health conditions.
One of the most difficult challenges in bodywork studies has been the lack of an adequate control group. Control conditions for clinical trials of bodywork therapy are necessary to isolate the specific effects of massage therapy from the non-specific effects of the environment in which it is practiced. Before initiating our clinical trial, we conducted a Medline search for prior randomized clinical trials using Swedish-style massage therapy modalities as treatment alone. Of the 21 studies identified (2, 5–22) (17 of which reported a significant improvement with massage (2, 5, 7–13, 15, 16, 18–20, 22)), none used a sham bodywork therapy regimen as a control. The control arms used in these studies varied widely but included usual care or other treatments such as rest, spinal manipulation, and relaxation therapy. Because of their study designs, none sufficiently addressed the question of whether the act of massage (the manipulation of muscle tissue) was responsible for the observed outcomes, or whether these responses could be attributed, at least in part, to the nonspecific effects of the additional time and personal contact between the provider and patient. Other forms of bodywork, such as Feldenkrais (23), reflexology (24), and Reiki (25, 26), have been studied using sham control arms. Since completion of our trial, we have again searched the literature and found no Swedish-type massage trials that used a sham bodywork therapy regimen as a control. However, a light-touch massage (similar to our sham bodywork control protocol) was used in an observational study of massage therapy at a major cancer center (27). The development and testing of a sham bodywork control would represent an important advance in the development of clinical-trial methods that examine the specific effects of massage and other bodywork therapies.
In this paper, we describe the development of a pilot randomized clinical trial of massage therapy, incorporating a “sham bodywork control” intervention, an evaluation of its implementation in the pilot study, and the evolution of our assessment about its value as a strict control condition.
Description of CRAFT Study
Overview
The CRAFT (Chemotherapy Regimen And Fatigue: Touch-Therapy) study was a randomized, three-arm, parallel-comparison pilot clinical trial comparing the effects of a Swedish-style massage regimen to a sham-bodywork control and a usual-care group for fatigue reduction in patients with cancer who were either undergoing chemotherapy or had completed chemotherapy within the previous six months. Participants in the two bodywork arms were assigned to twice-weekly sessions over a six-week period. The primary outcomes assessed were levels of fatigue symptoms and quality-of-life; a qualitative study of outcomes was also included. Outcome assessments occurred at the midpoint and end of the intervention period, one week following the last intervention visit, and six weeks later; overall, participants remained under observation for three months. All procedures were approved by the institutional review boards of the University of California, San Francisco and the Kaiser Foundation Research Institute, Oakland, California.
Participants
Participants were adults with a diagnosis of breast, ovarian, colon, or prostate cancer currently undergoing chemotherapy or who had completed chemotherapy within the prior 6 months. We allowed a variety of cancer types to both increase recruitment and to also examine response across different cancers. Since fatigue is a universal symptom across chemotherapy regimens, we felt it appropriate to include all chemotherapies administered for these cancers. Eligible patients had a Karnofsky performance status ≥70 and scored at least 14 on the Modified Schwartz Cancer Fatigue Scale (28).
Exclusion criteria included open dermal lesions, history of venous thrombosis, hematocrit <25%, elevated thyroid stimulating hormone, or previous use of oral steroids for more than 3 consecutive months in the prior five years. Patients who had been receiving regular bodywork (at least twice monthly over the prior six months) were also excluded.
Outcome measurements
The primary outcome measurement was the Revised Piper Fatigue Scale (29), selected because it had undergone a careful development process (29, 30), its psychometric properties had been studied and found to be acceptable, it was specifically targeted to the oncology population, was of acceptable length, and addressed the domains that the investigators felt important.
In addition to the Revised Piper Fatigue Scale, the Modified Schwartz Cancer Fatigue Scale (28) was used as a secondary measure. This scale, also developed specifically for patients with cancer, was a much shorter instrument and was well-suited to telephone screening (hence, its use as an eligibility screening criterion) and for rapid fatigue assessments at each intervention visit.
Additional information collected included a visual analogue scale for overall perceived levels of fatigue, the European Organization for Research and Treatment of Cancer (EORTC) QLQ-C30 (a cancer-specific quality-of-life measure) (31), the Center for Epidemiologic Studies Depression Scale (CES-D) (32), the Sleep Impairment Index (33), and a symptomatic side-effect profile. Covariate information collected included regular checks of the participants’ hematocrits to rule out the potential confounding effects of anemia.
Interventions
Participants were randomized in equal proportions to one of three intervention conditions: an active Swedish-style massage intervention (referred to as the “Medium-Intensity Bodywork” (MIB) arm to the participants), a sham-bodywork intervention (referred to as the “Low-Intensity Bodywork” (LIB) arm), and usual care. Participants in the two bodywork arms were asked to attend two sessions per week (and were strongly encouraged to attend at least once weekly). Prior to each bodywork session, the massage therapist assessed the participant for the presence of a deep venous thrombosis, following a structured exam that included calf circumference measurements (34).
We chose a standardized intervention for both treatment arms of the study. These interventions involved a full-body treatment that was completed in approximately 50 minutes; by design, each participant received massages from both male and female massage therapists. Both interventions addressed the same body regions, in the same order, for a specified amount of time. The massage therapists were instructed in both the massage procedure and the sham-touch procedure by the massage therapist co-investigator of the study (MP). Emphasis was placed on consistency in depth of touch and length of time spent on body regions. Because patients receiving massage may report a “hang-over effect” of the positive feelings a massage generates for one-to-two days after the intervention, a twice-weekly protocol (separated by at least one day) seemed most appropriate to maximize a beneficial effect. A six-week duration was chosen because the intervention could be completed before the end of most chemotherapy regimens and we assumed multiple weeks would intensify any positive effects. Moderate and low-intensity procedures were used (as opposed to deeper tissue techniques) because we wished to minimize discomfort and potential bruising of these patients undergoing chemotherapy.
We chose a standardized approach for several reasons. First, a standardized protocol minimized differences among practitioners administering the protocol and ensured that all the participants received as identical an intervention as possible. Importantly, it also limited the comparison between the two intervention groups to one factor (muscle manipulation vs. no muscle manipulation).
The massage protocol was pre-specified and deviations were permitted only for the inability of the participant to tolerate the massage (e.g., participants who were unable to lie supine received massage lying on their side). The intervention was delivered by licensed massage therapists who underwent specific training and who were assessed at regular intervals. Each intervention session was conducted in a private clinical treatment room at the Osher Center for Integrative Medicine Clinic at the University of California, San Francisco.
Because no studies to date had examined whether the effect of massage therapy is specifically from the manipulation of the muscle tissue or from the prolonged touch and contact from a massage therapist, we designed the LIB to control for the environmental conditions and physical contact of the massage arm. The LIB protocol was designed to touch the areas around the major muscle groups without manipulating the muscle tissue directly. Practitioners were instructed to lightly touch an area around a joint or bone region, hold that touch for a period of time, release their hands for a short period of time, adjust to a new position around that same region, and then reapply a light touch. This touch-release-touch method was devised to approximate the amount of time a massage therapist touches a participant during the MIB intervention. By protocol, the practitioners actively touched/massaged the patient during approximately 80% of the intervention time in both bodywork arms of the study.
Participants randomized to the usual-care control arm came to the clinic for their baseline assessment and follow-up interviews but otherwise completed all outcome assessment instruments via mail. Participants in this arm were asked not to receive massage therapy outside of the study during the three-month follow-up period. Participants in the control group were offered compensation for completing their study procedures of either three free massages or monetary compensation at the end of the three-month follow-up period (no compensation was offered to participants in the two bodywork arms).
The detailed protocol descriptions are contained in the Appendix.
Recruitment of Therapists
The original intent was to have the massage therapy intervention provided by trained massage therapists and the light-touch control condition performed by oncology nurses. The reasoning for this choice was an attempt to avoid the potential bias that could result from the massage therapists (who could have a vested interest in the outcome of the study) unconsciously doing a better job performing the massage therapy than the control intervention. However, the schedules for the oncology nurses proved too restrictive for this study; the same massage therapists, therefore, performed both the active massage and the control sham-bodywork procedures.
Massage therapists were recruited from local massage-therapy schools and the university-affiliated wellness center. Their training and experience credentials were reviewed by the study investigators and their massage technique was observed prior to appointing them to the study-practitioner positions.
Recruitment of Patients
Recruitment to the trial was carried out at the University of California, San Francisco and the San Francisco facility of the Northern California Kaiser Permanente Health Plan. In addition to passive recruitment, such as posters and fliers, we were also assisted by clinical staff at both institutions who notified potentially eligible patients of the study and the way to access enrollment. The intended sample size for this study was 45 participants.
Qualitative Component
We also performed a series of in-depth, semi-structured, qualitative interviews at three time points: at the initial randomization visit (during which participants were informed of their randomization assignment), after the final intervention visit (or at six weeks for those participants randomized to the usual-care group), and six weeks after the second interview. Domains assessed in the qualitative interview included physical, social, emotional, and spiritual well-being, definitions and viewpoints regarding participants’ fatigue, and questions regarding their overall study experience.
These interviews were taped, transcribed verbatim, and coded by two researchers (SM and MP). Two of the questions focused on how participants viewed their assigned study intervention. The first question inquired about participants’ feelings regarding their randomization assignment and was asked immediately after participants were told of the study arm to which they were assigned. The second question was asked at the end of the intervention period and assessed the participants’ views regarding the intervention they received during the study. The coded responses were then divided into positive responses, negative responses, or no information available (the question was not asked, the participant didn’t respond, or the participant did not complete that interview).
Experience of Study Participants
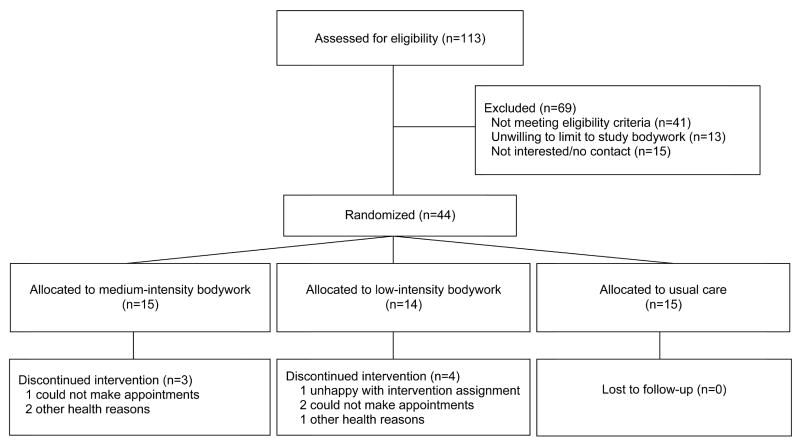
One hundred thirteen patients were screened for eligibility and forty-four were randomized over a two-year period. A flowchart of the enrollment of participants is shown in Figure 1.
Figure.
Participant flow of CRAFT Study
*One participant randomized to the low-intensity bodywork intervention received the mediumintensity bodywork intervention because of administrative scheduling problems.
Participants’ baseline characteristics are shown in Table 1. The mean age of the participants was 51 years; the study sample was overwhelmingly female and predominantly white.
Table 1.
Demographic characteristics of CRAFT study participants at randomization.
| Characteristic | All Groups (N=44) | MIB (N=15) | LIB (N=14) | UC (N=15) |
|---|---|---|---|---|
| Age (years); mean (SD) | 51.3 (9.9) | 49.1 (11.4) | 53.6 ( 11.0) | 51.2 (6.9) |
| Gender (n (%) female) | 42 (95%) | 14 (93%) | 13 (93%) | 15 (100%) |
| Race/Ethnicity (n (%)) | ||||
| African-American | 3 (7%) | 0 (0%) | 1 (7%) | 2 (13%) |
| Asian | 5 (11%) | 0 (0%) | 3 (21%) | 2 (13%) |
| Hispanic | 1 (2%) | 0 (0%) | 1 (7%) | 0 (0%) |
| Non-Hispanic white | 34 (77%) | 15 (100%) | 8 (57%) | 10 (67%) |
| Other | 2 (4%) | 0 (0%) | 1 (7%) | 1(7%) |
Abbreviations:
LIB = Low-Intensity Bodywork
MIB = Medium-Intensity Bodywork
SD = Standard Deviation
UC = Usual Care
The study participants’ adherence experience is summarized in Table 2. One LIB participant disliked her randomization choice and never appeared for an appointment. Two other LIB-allocated participants withdrew because of the difficulty in keeping twice-weekly appointments. The lone MIB dropout had spotty attendance and did not complete the required number of interview sessions.
Table 2.
Adherence experience in the CRAFT Pilot Study
| Study Arm | Enrolled | Completed Intervention | Did Not Complete Intervention | Withdrew for Health Reasons |
|---|---|---|---|---|
| MIB | 15 | 12 (80%) | 1 (7%) | 2 (13%) |
| LIB | 14 | 10 (71%) | 3 (21%) | 1 (7%) |
| UC | 15 | 15 (100%) | 0 (0%) | 0 (0%) |
| Totals | 44 | 37 (84%) | 4 (9%) | 3 (7%) |
Abbreviations:
LIB = Low-Intensity Bodywork
MIB = Moderate-Intensity Bodywork
UC = Usual Care
Three participants (two MIB, one LIB) withdrew for health reasons due to their cancer or chemotherapy regimen. The usual-care control group had the best adherence due to the fact that most of their data collection occurred at home via the mail.
As expected, all of the individuals allocated to the massage intervention had positive responses at the time of randomization; similarly, no negative responses were recorded after the intervention concluded (Table 3).
Table 3.
Qualitative analysis of participants’ views of study arm assignment
| Group | At-Randomization Responses | After Intervention Responses | ||||
|---|---|---|---|---|---|---|
| Pos | Neg | No Info | Pos | Neg | No Info | |
| MIB (n=15) | 15 | 0 | 0 | 12 | 0 | 3 |
| LIB (n=14) | 8 | 5 | 1 | 9 | 0 | 5 |
| UC (n=15) | 5 | 10 | 0 | 10 | 5 | 0 |
Abbreviations:
LIB = Low-Intensity Bodywork
MIB = Moderate-Intensity Bodywork
Neg = Negative response to randomization assignment
No Info = No information available to assess response to randomization assignment
Pos = Positive response to randomization assignment
UC = Usual Care
The LIB group reported mixed reactions to their randomization assignments initially, with some individuals satisfied receiving any intervention, while others were clearly disappointed they did not receive massage (Table 3). Thirty-six percent of participants in this arm had a negative viewpoint of being randomized to the LIB group. However, by the end of the intervention, we recorded no negative responses about their participation (although some follow-up data were missing).
The control arm was much more negatively viewed by participants, with 67% showing displeasure at the time of randomization. However this distribution of responses reversed after participation in the study, with 67% of respondents expressing a positive view of the control arm at study closeout. Many participants reported that they enjoyed filling out the questionnaires, stating that it kept them aware of their physical, mental, and emotional states during their chemotherapy treatment.
In summary, the qualitative interviews suggested that, despite some initial negativity regarding the LIB arm, those participants who completed the study viewed both intervention arms positively after the conclusion of the intervention.
Discussion
The CRAFT Pilot Study provided an important opportunity to inform the study of bodywork therapy for patients with cancer by testing several aspects of clinical-trial study design.
Perhaps the most important and unique element of the study was the development and testing of a novel control condition for massage therapy. Up to the time of study initiation, no study had reported the use of a comparison intervention that controlled for the experience of the massage-therapy encounter without providing the muscle manipulation that is at the core of massage. The inability to control for the non-specific aspects of massage therapy has been a serious impediment to more rigorous study of this aspect of bodywork therapy.
We found that we were able to successfully develop and implement a light-touch control intervention for this massage-therapy trial. Massage therapists could be trained to deliver the intervention and participants who were randomized to receive this intervention accepted it and adhered to the regimen nearly as well as those randomized to the Swedish-style massage therapy. In fact, it became clear during the study that, rather than a simple control condition, the light-touch intervention may have clinical benefits in its own right. The responses of the participants receiving the intervention were generally positive and many participants commented on the pleasant aspects of the quiet time alone with a caring bodywork therapist who crossed the “touch boundary.” Whether either intervention resulted in a suggestion of a clinically meaningful benefit awaits the results of the quantitative and qualitative analyses, but the ability to implement this type of control condition is clearly feasible.
In addition to the demonstrated viability of the control condition, several other aspects of the study design proved informative for future trials of massage therapy for patients with cancer. First, we found that a complex, intensive outpatient clinic-based protocol of bodywork therapy proved difficult for many of our participants to maintain full adherence. Patients with cancer have numerous stresses and many demands on their time; a twice-weekly intervention protocol proved burdensome for many patients. This burden was heightened by the fact that the interventions were delivered on an outpatient basis at the medical center (as opposed to an outcall method that would not require traveling); parking and transportation time in the San Francisco Bay Area caused additional problems for patients. We also realized that although participants were either currently receiving chemotherapy or they had completed chemotherapy within the past six months, these two groups have very different physical and psychological stressors placed upon them. We anecdotally noticed that those in active chemotherapy treatment had more difficulty with adherence than those who had complete chemotherapy but were still fatigued.
Second, we found that massage therapists were able to follow a structured massage protocol and to deliver the light-touch intervention well. Depending on the study design and research questions, it may or may not be preferable to deliver a highly structured massage intervention. Standardizing a bodywork intervention allows for better isolation of the various components of massage therapy relative to a non-structured protocol. However, a highly structured intervention may be quite different from the usual experience of both practitioners and clients in a non-research setting. The choice of the approach will depend on the nature of the research issues and specific questions under study.
Finally, we found, somewhat surprisingly, that recruitment proved problematic for this study. Several factors were identified as contributing to this difficulty. Many patients are already receiving massage therapy and declined to be randomized in a study that included a no-treatment arm. Other patients found the complexity and burden of the protocol to be a disincentive to enroll and travel issues also figured prominently among those who declined.
In summary, despite the many problems identified and lessons learned, we found that we were able to successfully develop and deliver a structured and controlled bodywork therapy intervention for use in clinical trials. The further development and refinement of these and other innovative methods will help generate greater understanding of the benefits, risks, and mechanisms of massage therapy for a wide range of medical conditions.
Acknowledgments
The authors gratefully acknowledge the assistance and support of Yvette Coulter; Carolyn Jacobs; Lori Ross, RN; Wolf Mehling, MD; Bradly Jacobs, MD; Amy Padula, MS; and the UCSF Cancer Research Center staff
We are grateful to the massage therapists whose expertise was vital to the successful completion of this trial: Matthew Christen, LMT; Timothy Cowen, LMT; Paula Koepke, LMT; Mindy Zlotnick, LMT; and Michael McNamara, LMT.
The authors are particularly indebted to the research participants, without whose contributions this study could not have taken place.
Supported by a grant from the National Center for Complementary and Alternative Medicine of the National Institutes of Health (#R21 AT000348)
Appendix
Bodywork Protocols Used in CRAFT Study
For both intervention groups, during the treatment sessions, the patient is draped with only those areas exposed that are receiving treatment. In the massage therapy arm, massage lotion is applied as needed by the therapist to ensure appropriate friction; in the bodywork arm, a minimal amount of lotion is put on the bodyworker’s hands for consistency across groups. The massage lotion used is Biotone Advanced Therapy Massage Crème (hypoallergenic and fragrance-free).
Massage Intervention Group (Moderate-Intensity Bodywork)
Certified Massage therapists specializing in Swedish-style massage perform the massages for this group. They are trained to follow the study protocol by the investigators and pre-study trial sessions are performed under supervision to ensure compliance with the regimen. The massage therapy session is structured in the following manner:
A patient enters the room led by the bodyworker who instructs the patient to disrobe, lie face down on the massage table, and put the draping sheet over their body. The bodyworker leaves the room while this occurs.
The bodyworker returns and begins the 50-minute session:
Upper and middle back are worked bilaterally, including the trapezius, erector spinae, and rhomboids for a total of 5 minutes efflurage strokes followed by 5 minutes of light petrissage. (10 minutes total)
Low back and upper buttocks are worked bilaterally including the latissimus dorsi, erector spinae, gluteus minimus, gluteus maximus, gluteus medius for a total of 3 minutes efflurage strokes, 2 minutes light petrissage. (5 minutes total)
The left posterior leg is worked including 2 minutes efflurage on the calf muscles (gastrocnemius and soleus) and 3 minutes efflurage on the hamstring muscles (seminmembranosus, semitendinosus and biceps femoris). This is repeated on the right posterior leg. (10 minutes total)
The patient turns over so they are now facing up. The bodyworker readjusts table/bolsters/sheets/blankets as needed.
The left anterior leg is worked including 2 minutes efflurage on the foot (abductor hallucis, abductor digiti minimi and flexor digitor brevis) and extensor muscles, as well as 3 minutes on the quadreceps femorus. This is repeated on the right anterior leg. (10 minutes total)
The left arm is worked including the deltoid, biceps brachii, triceps brachii brachioradialis, and the hand flexors and extensors for a total of 2 minutes of efflurage and 3 minutes of light petrissage. This is repeated on the right arm. (10 minutes total)
The muscles of the neck and shoulders are worked including the trapezius, levator scapulae, splenius, semispinalis, suboccipital muscles and sternocleidomastoid for a total of 2 minutes of efflurage and 3 minutes of light petrissage. (5 minutes total)
When completed, the patient is told that the massage is finished, is encouraged to drink water to prevent dehydration, and is instructed on how to get up from the table. The patient dresses, exits the therapy room, and meets with the research assistant before leaving to confirm their next appointment.
Bodywork Control Group (Light-Intensity Bodywork)
This control group is included in the study design to control for the amount of time that participants interact with a therapist as well as the physical contact that they receive. Massage Therapists are trained to perform the bodywork control sessions. They are instructed to follow the study protocol by the investigators and pre-study trial sessions will be performed under supervision to ensure compliance with the regimen. The control bodywork therapy session is structured in the following manner:
The patient enters the room led by the bodyworker who instructs the patient to disrobe, lie face down on the massage table, and put the provided draping sheet over their body. The bodyworker leaves the room while this occurs.
The bodyworker returns and begins the 50-minute session:
Both hands of the bodyworker are placed on the right shoulder blade. Pressure will be light and consistent for approximately 40 seconds. The bodyworker lifts their hands off the patient for approximately 10 seconds. The bodyworker repositions the hands slightly (rotating the position in a counter-clockwise manner around the shoulder blade) and repeats the touch. This is done a total of six times. (5 minutes)
Both hands of the bodyworker are placed on the left shoulder blade. The same protocol is performed (except that the rotation is clockwise). (5 minutes).
Both hands of the bodyworker are placed on the low back/sacrum area. The same protocol is performed (rotating the position in a clockwise manner completely around the sacrum). (5 minutes).
Both hands of the bodyworker are placed on the right heel. The same protocol is performed (rotating the position in a counter-clockwise manner around the heel). (5 minutes).
Both hands of the bodyworker are placed on the left heel. The same protocol is performed (rotating the position in a clockwise manner around the heel). (5 minutes).
The patient turns over so they are now facing up. The bodyworker readjusts table/bolsters/sheets/blankets as needed.
Both hands of the bodyworker are placed on the right patella. The same protocol is performed (rotating the position in a clockwise manner). (5 minutes)
Both hands of the bodyworker are placed on the left patella. The same protocol is performed (rotating the position in a counter-clockwise manner). (5 minutes)
Both hands of the bodyworker are placed on the right elbow joint. The same protocol is performed (rotating the position in a clockwise manner). (5 minutes)
Both hands of the bodyworker are placed on the left elbow joint. The same protocol is performed (rotating the position in a counter-clockwise manner). (5 minutes)
Both hands of the bodyworker are placed on the occipital ridge area of neck. The same protocol is performed (rotating the position in a clockwise manner). (5 minutes)
When completed, the patient is told that the treatment is finished, is encouraged to drink water to prevent dehydration, and is instructed on how to get up from the table. The patient dresses, exits the therapy room, and meets with the research assistant before leaving to confirm their next appointment.
Usual-Care Control Group
This group does not receive any bodywork treatments, only usual care from their oncology treatment team. Patients follow all other aspects of the study schema, including filling out forms, undergoing a physical exam, participating in interviews and having their blood drawn. On weeks that they are not in clinic for a blood draw or interview, the data collection forms are mailed to patients’ homes’ with instructions on how and when to fill them out. This control group is being used in this study to determine whether there is a non-specific effect on patient’s fatigue because of the human contact and extended time patients spend with a provider.
Footnotes
Conflict of Interest Statement
No author has any financial or personal relationships that might constitute a conflict of interest with this research.
Role of the Funding Source
The funding agency (The National Center for Complementary and Alternative Medicine at the National Institutes of Health) had no role in the study design, data collection, data analysis, writing of the manuscript, or the decision to submit this manuscript for publication.
Registration of Clinical Trial
This trial was registered with clinicaltrials.gov, #NCT00039793.
References
- 1.Ironson G, Field T, Scafidi F, Hashimoto M, Kumar M, Kumar A, et al. Massage therapy is associated with enhancement of the immune system’s cytotoxic capacity. Int J Neurosci. 1996 Feb;84(1–4):205–17. doi: 10.3109/00207459608987266. [DOI] [PubMed] [Google Scholar]
- 2.Smith LL, Keating MN, Holbert D, Spratt DJ, McCammon MR, Smith SS, et al. The effects of athletic massage on delayed onset muscle soreness, creatine kinase, and neutrophil count: a preliminary report. J Orthop Sports Phys Ther. 1994 Feb;19(2):93–9. doi: 10.2519/jospt.1994.19.2.93. [DOI] [PubMed] [Google Scholar]
- 3.Field T, Sunshine W, Hernandez-Reif M, Quintino O, Schanberg S, Kuhn C, et al. Massage therapy effects on depression and somatic symptoms in chronic fatigue syndrome. J of Chronic Fatigue Syndrome. 1997;3:43–51. [Google Scholar]
- 4.Sunshine W, Field T, Schanberg S, Quintino O, Fierro K, Kuhn C, et al. Fibromyalgia benefits from massage therapy and transcutaneous electrical stimulation. J Clin Rheumatology. 1996;2:18–22. doi: 10.1097/00124743-199602000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Chen ML, Lin LC, Wu SC, Lin JG. The effectiveness of acupressure in improving the quality of sleep of institutionalized residents. J Gerontol A Biol Sci Med Sci. 1999 Aug;54(8):M389–94. doi: 10.1093/gerona/54.8.m389. [DOI] [PubMed] [Google Scholar]
- 6.Dunn C, Sleep J, Collett D. Sensing an improvement: an experimental study to evaluate the use of aromatherapy, massage and periods of rest in an intensive care unit. J Adv Nurs. 1995 Jan;21(1):34–40. doi: 10.1046/j.1365-2648.1995.21010034.x. [DOI] [PubMed] [Google Scholar]
- 7.Field T, Grizzle N, Scafidi F, Schanberg S. Massage and relaxation therapies’ effects on depressed adolescent mothers. Adolescence. 1996 Winter;31(124):903–11. [PubMed] [Google Scholar]
- 8.Field T, Henteleff T, Hernandez-Reif M, Martinez E, Mavunda K, Kuhn C, et al. Children with asthma have improved pulmonary functions after massage therapy. J Pediatr. 1998 May;132(5):854–8. doi: 10.1016/s0022-3476(98)70317-8. [DOI] [PubMed] [Google Scholar]
- 9.Field T, Hernandez-Reif M, Hart S, Theakston H, Schanberg S, Kuhn C. Pregnant women benefit from massage therapy. J Psychosom Obstet Gynaecol. 1999 Mar;20(1):31–8. doi: 10.3109/01674829909075574. [DOI] [PubMed] [Google Scholar]
- 10.Field T, Hernandez-Reif M, Seligman S, Krasnegor J, Sunshine W, Rivas-Chacon R, et al. Juvenile rheumatoid arthritis: benefits from massage therapy. J Pediatr Psychol. 1997 Oct;22(5):607–17. doi: 10.1093/jpepsy/22.5.607. [DOI] [PubMed] [Google Scholar]
- 11.Field T, Hernandez-Reif M, Taylor S, Quintino O, Burman I. Labor pain is reduced by massage therapy. J Psychosom Obstet Gynaecol. 1997 Dec;18(4):286–91. doi: 10.3109/01674829709080701. [DOI] [PubMed] [Google Scholar]
- 12.Field T, Peck M, Krugman S, Tuchel T, Schanberg S, Kuhn C, et al. Burn injuries benefit from massage therapy. J Burn Care Rehabil. 1998 May-Jun;19(3):241–4. doi: 10.1097/00004630-199805000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Field TM, Quintino O, Hernandez-Reif M, Koslovsky G. Adolescents with attention deficit hyperactivity disorder benefit from massage therapy. Adolescence. 1998 Spring;33(129):103–8. [PubMed] [Google Scholar]
- 14.Hsieh CY, Phillips RB, Adams AH, Pope MH. Functional outcomes of low back pain: comparison of four treatment groups in a randomized controlled trial. J Manipulative Physiol Ther. 1992 Jan;15(1):4–9. [PubMed] [Google Scholar]
- 15.Nixon M, Teschendorff J, Finney J, Karnilowicz W. Expanding the nursing repertoire: the effect of massage on post-operative pain. Aust J Adv Nurs. 1997 Mar–May;14(3):21–6. [PubMed] [Google Scholar]
- 16.Patino O, Novick C, Merlo A, Benaim F. Massage in hypertrophic scars. J Burn Care Rehabil. 1999 May–Jun;20(3):268–71. discussion 7. [PubMed] [Google Scholar]
- 17.Pope MH, Phillips RB, Haugh LD, Hsieh CY, MacDonald L, Haldeman S. A prospective randomized three-week trial of spinal manipulation, transcutaneous muscle stimulation, massage and corset in the treatment of subacute low back pain. Spine. 1994 Nov 15;19(22):2571–7. doi: 10.1097/00007632-199411001-00013. [DOI] [PubMed] [Google Scholar]
- 18.Scafidi F, Field T. Massage therapy improves behavior in neonates born to HIV-positive mothers. J Pediatr Psychol. 1996 Dec;21(6):889–97. doi: 10.1093/jpepsy/21.6.889. [DOI] [PubMed] [Google Scholar]
- 19.Scafidi FA, Field T, Schanberg SM. Factors that predict which preterm infants benefit most from massage therapy. J Dev Behav Pediatr. 1993 Jun;14(3):176–80. [PubMed] [Google Scholar]
- 20.Hulme J, Waterman H, Hillier VF. The effect of foot massage on patients’ perception of care following laparoscopic sterilization as day case patients. J Adv Nurs. 1999 Aug;30(2):460–8. doi: 10.1046/j.1365-2648.1999.01101.x. [DOI] [PubMed] [Google Scholar]
- 21.Weber MD, Servedio FJ, Woodall WR. The effects of three modalities on delayed onset muscle soreness. J Orthop Sports Phys Ther. 1994 Nov;20(5):236–42. doi: 10.2519/jospt.1994.20.5.236. [DOI] [PubMed] [Google Scholar]
- 22.Wheeden A, Scafidi FA, Field T, Ironson G, Valdeon C, Bandstra E. Massage effects on cocaine-exposed preterm neonates. J Dev Behav Pediatr. 1993 Oct;14(5):318–22. [PubMed] [Google Scholar]
- 23.Johnson SK, Frederick J, Kaufman M, Mountjoy B. A controlled investigation of bodywork in multiple sclerosis. J Altern Complement Med. 1999 Jun;5(3):237–43. doi: 10.1089/acm.1999.5.237. [DOI] [PubMed] [Google Scholar]
- 24.Siev-Ner I, Gamus D, Lerner-Geva L, Achiron A. Reflexology treatment relieves symptoms of multiple sclerosis: a randomized controlled study. Mult Scler. 2003 Aug;9(4):356–61. doi: 10.1191/1352458503ms925oa. [DOI] [PubMed] [Google Scholar]
- 25.Mansour AA, Beuche M, Laing G, Leis A, Nurse J. A study to test the effectiveness of placebo Reiki standardization procedures developed for a planned Reiki efficacy study. J Altern Complement Med. 1999 Apr;5(2):153–64. doi: 10.1089/acm.1999.5.153. [DOI] [PubMed] [Google Scholar]
- 26.Shiflett SC, Nayak S, Bid C, Miles P, Agostinelli S. Effect of Reiki treatments on functional recovery in patients in poststroke rehabilitation: a pilot study. J Altern Complement Med. 2002 Dec;8(6):755–63. doi: 10.1089/10755530260511766. [DOI] [PubMed] [Google Scholar]
- 27.Cassileth BR, Vickers AJ. Massage therapy for symptom control: outcome study at a major cancer center. J Pain Symptom Manage. 2004 Sep;28(3):244–9. doi: 10.1016/j.jpainsymman.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 28.Schwartz A, Meek P. Additional construct validity of the Schwartz Cancer Fatigue Scale. J Nurs Meas. 1999 Spring;7(1):35–45. [PubMed] [Google Scholar]
- 29.Piper BF, Dibble SL, Dodd MJ, Weiss MC, Slaughter RE, Paul SM. The revised Piper Fatigue Scale: psychometric evaluation in women with breast cancer. Oncol Nurs Forum. 1998 May;25(4):677–84. [PubMed] [Google Scholar]
- 30.Piper BF, Lindsey AM, Dodd MJ, Ferketich S, Paul SM, Weller S. The development of an instrument to measure the subjective dimension of fatigue. In: Funk SG, Tournquist MT, Champagne LA, Copp RA, Weise RA, editors. Key aspects of comfort: management of pain, fatigue and nausea. New York: Springer; 1989. [Google Scholar]
- 31.Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993 Mar 3;85(5):365–76. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 32.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 33.Morin CM. Insomnia: psychological assessment and management. New York, NY: Guilford Press; 1993. [Google Scholar]
- 34.Anand SS, Wells PS, Hunt D, Brill-Edwards P, Cook D, Ginsberg JS. Does this patient have deep vein thrombosis? Jama. 1998 Apr 8;279(14):1094–9. doi: 10.1001/jama.279.14.1094. [DOI] [PubMed] [Google Scholar]