Abstract
Noncardiac components of genetic disorders can complicate the operative and postoperative courses of pediatric cardiac surgery patients. Prolonged hospital stay, increased treatment cost, morbidity, and death are more likely in this subgroup of patients.
Ventricular septal defect, which is a component of various genetic disorders, has a 22.3% incidence in VACTERL syndrome—a rare, nonrandom pattern of birth defects. Herein, we discuss the impact of ventricular septal defect closure in a 4-month-old girl who was diagnosed after birth with Vacterl syndrome.
Key words: Abnormalities, multiple/epidemiology; chromosome breakage; esophageal atresia/complications/epidemiology/etiology/genetics/surgery; fetal growth retardation/epidemiology; fetal heart; heart defects, congenital/chemically induced/classification/epidemiology; infant, newborn; progesterone/adverse effects; respiration disorders/etiology; tracheoesophageal fistula/complications/surgery
Cardiac defects may be observed in patients who have various genetic disorders. When the cardiac defects are surgically corrected, accompanying noncardiac anomalies can negatively influence the operative and postoperative courses of these patients.
The rare, nonrandom pattern of birth defects called VACTERL syndrome comprises vertebral column anomalies (V), anal atresia (A), congenital heart defects (C), tracheoesophageal defects (TE), renal and distal urinary tract anomalies (R), and limb abnormalities (L).1 The simultaneous presence of at least 3 of these anomalies constitutes a diagnosis of Vacterl syndrome.
Ventricular septal defect is the most common cardiac component of the syndrome (incidence, 22.3% of VACTERL cases). Herein, we report and discuss the operative and postoperative impact of Vacterl syndrome on the surgical closure of a ventricular septal defect (VSD) in a 4-month-old infant.
Case Report
In August 2005, a 4-month-old, 2.7-kg infant with no parental consanguinity was admitted to our institution with cyanosis, tachypnea, and growth retardation. At birth, she had weighed 1.74 kg. A prenatal medical history revealed a threat of spontaneous abortion in the 6th gestational week, for which the mother had received progesterone treatment until the 4th month of pregnancy. Fetal ultrasonography had then shown growth retardation and polyhydroamniosis. After periodic ultrasonographic examinations, the neonate was delivered by cesarean section in the mother's 36th week of pregnancy.
Esophageal atresia and tracheoesophageal fistula (EA/TEF) were diagnosed on the neonate's 1st day of life; at the institution where she was born, she underwent emergency end-to-end anastomosis to correct the atresia, and the fistula was also closed. Vertebral segmentation defect was an accompanying anomaly (Fig. 1). A 2-dimensional transthoracic echocardiogram revealed a large perimembranous VSD, apical Swiss-cheese VSDs, a patent ductus arteriosus (PDA), a persistent left superior vena cava, and pulmonary hypertension. Chromosome-breakage studies for Fanconi anemia (FA) were negative (nitrogen mustard, 0.21%; diepoxybutane, no breakage). Accordingly, the diagnosis of VACTERL syndrome was confirmed soon after birth. The infant was discharged from that hospital and was referred to ours for the repair of her cardiac defects.
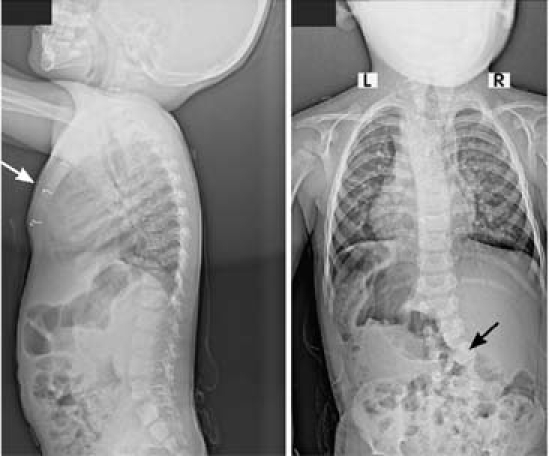
Fig. 1 Radiographs show sternal wire sutures (white arrow) and scoliosis (black arrow).
At 4 months of age, the infant underwent VSD closure (with a pericardial patch) and PDA ligation. Cardiac edema ensued. Dopamine (10 μg/[kg·mn]) and adrenaline (0.05 mg/[kg·mn]) were administered, and mechanical ventilation was instituted (1.9-L tidal volume and 40 breaths/min at 40% fraction of inspired oxygen). She was transferred with an open chest to the cardiovascular intensive care unit (ICU), where she was placed on teicoplanin and amicacine therapy.
The patient's chest was closed on the 2nd postoperative day. Excessive systemic inflammation caused increased capillary leakage syndrome, which was treated by means of isotonic peritoneal dialysis. On the 3rd postoperative day, endotracheal sputum tested positive for Pseudomonas aeruginosa, and the antibiotic regimen was changed to piperacillin/tazobactam. The period of intubation was prolonged due to Pseudomonas bronchopneumonia and pulmonary hypertension. Nine hours after initial extubation, the patient was reintubated because of insufficient respiratory efforts. When blood cultures proved positive for Stenotrophomonas maltophilia and Candida albicans, the antibiotic therapy was changed to fluconazole and cefoperazone. After white-blood-cell count and C-reactive protein readings indicated normal levels, the patient was successfully extubated. She was intubated for 18 of her 55 days in the cardiovascular ICU.
On the 20th postoperative day, the patient aspirated after feeding and developed grave bronchopneumonia. Antibiotic therapy was reinstituted after culture antibiograms were positive. The patient could not tolerate oral feeding, so a nasogastric catheter was placed and supportive parenteral nutrition was started.
The patient was transferred to the Department of Pediatrics' Division of Metabolism and Nutrition on the 55th postoperative day with severe growth deficiency. Bronchoscopy and thoracic spiral computed tomography revealed tracheomalacia and bilateral apical atelectasia with no need for specific treatment. For a total of 40 postoperative days, the infant was fed via nasogastric catheter. When she approximated normal weight and length curves for her age, she was discharged from the pediatric unit.
At the age of 3 years, the child underwent elective surgery for repair of scoliosis. At her last cardiac follow-up examination, in February 2008, she was doing very well.
Discussion
Our patient experienced several postoperative sequelae related to noncardiac components of VACTERL syndrome. Investigators2,3 have implicated early fetal exogenous hormone exposure, fetal physical stress (manifested by polyhydroamniosis), and the threat and treatment of spontaneous abortion as probable risk factors in the development of Vacterl syndrome. Our patient's prenatal medical history included all 3 of these.
Numerous studies have explored the long-term outcomes of VACTERL syndrome patients who have undergone EA/TEF repair. Respiratory complications are common. Delius and colleagues4 reported apnea and bradycardia, respiratory arrest, aspiration, and recurrent pneumonia in 46% of this population. The causes were gastroesophageal reflux disease in 74% of the patients, tracheomalacia in 13%, recurrent TEF in 13%, and esophageal stricture in 10%. Multiple causes were found in many patients.
Of patients with VACTERL syndrome who undergo surgery at an early age, 75% experience tracheomalacia. Remarkably, only 10% to 20% of these patients show clinically significant symptoms, such as biphasic stridor, stridor at rest, dyspnea during feeding, or expiratory wheezing. On the other hand, sputum retention due to impaired secretion clearance and ineffective cough can lead to tracheal mucosal metaplasia, cilia reduction, atelectasis, and recurrent pneumonia. Aspiration of secretions from the blind pouch of the former TEF site can also lead to infection. In our patient, prolonged intubation, aspiration pneumonia, feeding problems, and failure to thrive complicated the postoperative course. All of these possible factors, which are not expected to accompany routine VSD closure—became our chief concerns during the postoperative course of VSD that was part of a genetic disease.
A 2003 report5 implicated simple, isolated EA/TEF as a cause of growth retardation. In patients such as ours, in whom EA/TEF is an accompanying anomaly, the repair of this anomaly alone may not enable the patient to attain a normal growth curve. We consider it more likely that these patients will approximate a normal growth curve, especially when VSD closure accompanies EA/TEF repair.
Recent studies6,7 into the relationship between FA and VACTERL have induced physicians to investigate the incidence of FA in patients who have Vacterl syndrome. The Vacterl with hydrocephaly (Vacterl-H) phenotype is recognized as a severe manifestation of autosomal recessive FA. Although Vacterl-H has clearly been associated with FA (that is, there is chromosome breakage), the presence of chromosome-breakage in Vacterl without hydrocephaly is unclear. Faivre and colleagues6 reported finding 3 unrelated patients who had the Vacterl-without-hydrocephaly phenotype and (as determined from chromosome-breakage studies) a confirmed diagnosis of FA. Giampietro and co-authors7 noted a 10% incidence of the Vacterl phenotype in patients who were listed in the international FA registry. We had another patient, who had Vacterl and tetralogy of Fallot, whose chromosome-breakage test was negative. On the basis of these data, we concluded—as did Faivre and colleagues—that a chromosome-breakage test is not a requirement, but neither is it completely unnecessary. Accordingly, we performed a chromosome-breakage test for FA in our 4-month-old patient, and no abnormality was found.
Noncardiac components of genetic disorders can complicate the operative and postoperative courses of pediatric cardiac surgery patients and can incur prolonged hospital stays, increased treatment costs, and increased risk of morbidity and death. Especially in the subgroup of patients who have VACTERL syndrome, surgical and ICU teams should anticipate and investigate all sequelae in order to achieve better outcomes.
Footnotes
Address for reprints: Ali Can Hatemi, MD, PhD, Abdi Ipekci Cad. Polat Saray Apt. 79/17, Macka, Sisli, Istanbul 34367, Turkey. E-mail: hatemi@superonline.com
References
- 1.Keckler SJ, St Peter SD, Valusek PA, Tsao K, Snyder CL, Holcomb GW 3rd, Ostlie DJ. VACTERL anomalies in patients with esophageal atresia: an updated delineation of the spectrum and review of the literature. Pediatr Surg Int 2007;23(4): 309–13. [DOI] [PubMed]
- 2.Szendrey T, Danyi G, Czeizel A. Etiological study on isolated esophageal atresia. Hum Genet 1985;70(1):51–8. [DOI] [PubMed]
- 3.Hook EB. Cardiovascular birth defects and prenatal exposure to female sex hormones: a reevaluation of data reanalysis from a large prospective study. Teratology 1994;49(3):162–6. [DOI] [PubMed]
- 4.Delius RE, Wheatley MJ, Coran AG. Etiology and management of respiratory complications after repair of esophageal atresia with tracheoesophageal fistula. Surgery 1992;112(3): 527–32. [PubMed]
- 5.Little DC, Rescorla FJ, Grosfeld JL, West KW, Scherer LR, Engum SA. Long-term analysis of children with esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 2003;38 (6):852–6. [DOI] [PubMed]
- 6.Faivre L, Portnoi MF, Pals G, Stoppa-Lyonnet D, Le Merrer M, Thauvin-Robinet C, et al. Should chromosome breakage studies be performed in patients with VACTERL association? Am J Med Genet A 2005;137(1):55–8. [DOI] [PubMed]
- 7.Giampietro PF, Raggio CL, Reynolds C, Ghebranious N, Burmester JK, Glurich I, et al. DLL3 as a candidate gene for vertebral malformations. Am J Med Genet A 2006;140(22): 2447–53. [DOI] [PubMed]


