Abstract
During coronary artery bypass grafting, the length of the graft to the circumflex coronary artery or its end branches can be underestimated because of the posterior location of the circumflex. Herein, we describe a new bypass route—which we consider the shortest—to the ascending aorta.
In 2 patients, during proximal anastomosis of the saphenous vein bypass graft (via a route either anterior to the pulmonary artery or the transverse sinus) from the circumflex to the ascending aorta, the vein graft (approximately 5–6 cm in length) proved too short. We performed bypass in a new direction—from the circumflex coronary artery to the right side of the ascending aorta, under the inferior and superior venae cavae and along the interatrial groove—without the need for graft lengthening.
To our knowledge, the bypass route to the circumflex system described herein is new. This new route can be successfully used when the bypass conduit is too short to follow the conventional route. Our 2 patients benefited from this approach and were in Canadian Cardiovascular Society Class l two years after the surgical procedure.
Key words: Anastomosis, surgical/methods; cardiac surgical procedures/methods; cardiopulmonary bypass/methods; coronary artery bypass/methods; coronary artery disease/surgery; coronary vessels/surgery; treatment outcome
Because of the posterior location of the circumflex coronary artery (Cx) and the angles of its marginal branches,1 reaching the Cx with a graft from the ascending aorta is more difficult than reaching the right and anterior descending coronary arteries. Sometimes, graft lengthening is necessary. Herein, we describe a new route to the Cx, whereby graft lengthening via interposition or other methods is no longer required.
Surgical Technique
In early 2004, 2 male patients, one 57 years old and one 68 years old, presented with 3-vessel coronary artery disease in left-dominant coronary systems (Fig. 1). Patient 1 had ankylosing spondylitis; Patient 2 had immune thrombocytopenic purpura.
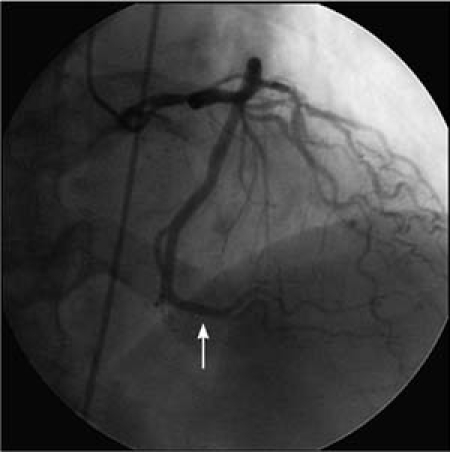
Fig. 1 Patient 1. Preoperative coronary angiogram shows a left-dominant coronary artery system with a dominant circumflex coronary artery (arrow).
Patient 1 underwent quadruple coronary artery bypass grafting. The autologous great saphenous vein was grafted to the Cx and to the posterior descending coronary artery via the single-graft technique, and an autologous Y-graft was performed with great saphenous vein to the left anterior descending coronary artery and to the diagonal branch. The left internal thoracic artery was not used as a bypass conduit in this patient to avoid disturbing thoracic wall stability and injuring the phrenic nerve, in view of the need for extrapulmonary respiratory support.
Patient 2 received 3 coronary artery bypass grafts: the left internal thoracic artery to the left anterior descending coronary artery, and an autologous Y-graft of the great saphenous vein to the Cx and to the left posterolateral artery.
In both patients, the distal coronary artery bypass anastomoses were performed in the cross-clamped ascending aorta with the use of myocardial protection and warm-blood cardioplegia. After the distal anastomoses were complete, the cross-clamps were removed. Preparations began for the proximal anastomosis of the blood-distended Cx bypass graft to the ascending aorta, via a route anterior to the pulmonary artery and through the transverse sinus. In both patients, the graft (approximately 5–6 cm in length) was too short. Therefore, we directed the conduit to the ascending aorta along a new passage.
We mobilized the inferior and superior venae cavae. The adipose tissue and posterior interatrial sulci in the interatrial grooves were then dissected in accordance with the length of the available graft and using the interatrial approach to the mitral valve as described by Carpentier and colleagues.2 In each patient, the vein graft from the Cx was directed along the posterior aspect of the left ventricle and under the inferior vena cava, along the posterior interatrial sulcus and then under the superior vena cava to the right posterior wall of the ascending aorta (Fig. 2).

Fig. 2 Patient 1. Schematic drawing shows the new route of the bypass from the circumflex coronary artery to the right side of the ascending aorta under the venae cavae, along the interatrial groove.
Results
In both patients, the grafts ran in a curve under both venae cavae and in the interatrial groove from the right posterior wall of the ascending aorta to the Cx system, without kinking or banding. This anatomic route was appropriate to the curved shape of the heart. If the graft length is sufficient, the graft will not be compressed by either of the venae cavae or by the posterior interatrial sulci because of the comparatively low blood pressure in these vessels and in the atria. The patency of the bypass grafts to the Cx was shown by transit-time flow measurements: 92 mL/min in the patient who received the vein graft to the Cx in single-graft technique, and 115 mL/min in the patient who had the original Y graft of the great saphenous vein to the Cx and to the left posterolateral artery.
The postoperative courses of these patients were uneventful, with no sign of myocardial ischemia or infarction. At their 2-year follow-up examinations, both patients underwent exercise electrocardiography, which revealed no ischemia during exercise or at rest. Both were in Canadian Cardiovascular Society Class 1; accordingly, no postoperative coronary angiography was performed.
Discussion
Even experienced cardiac surgeons can sometimes underestimate what length of graft from the Cx is adequate in the decompressed heart, because the Cx is so far from the ascending aorta. In such instances, the standard approach has been to lengthen the graft by interposing an additional segment. The route of our graft obviates the need for additional surgical intervention, such as another end-to-end interpositional anastomosis.
Another standard approach has been end-to-side anastomosis of the too-short vein graft into a neighboring vein graft, thus completing the proximal Cx graft anastomosis as a Y graft. However, this is not as safe for the dominant Cx, as can be inferred from Figure 1: the patency of either the Cx coronary vein graft or the other graft is endangered by completion of this anastomosis as a Y graft. The patency of our graft is not jeopardized either by a new end-to-end interpositional anastomosis or by another neighboring vein graft through end-to-side anastomosis to complete the Y graft. Furthermore, our approach enables direct proximal anastomosis on the right side of the ascending aorta.
There is a limitation to our graft approach: if the patient is known to require a later mitral valve operation in which the use of the interatrial approach or classic left atriotomy is necessary, our graft should not be performed, due to the risk of injury to the bypass conduit. We recommend the use of this new passage only if the original graft length is too short, because an additional surgical procedure—mobilization of the inferior and superior venae cavae and posterior interatrial dissection—will be necessary. However, performing this additional procedure takes only 1 or 2 minutes—less time than an interposition.
Rastan and Amir-Jahed3 first described the aorta–Cx coronary artery bypass through the transverse sinus. In practice, however, the most frequent route of the graft to the Cx system is anterior to the pulmonary artery; this is the approach that we routinely use. In contrast, Hudspeth1 and Grondin and Limet4 favored following the transverse sinus to the anterior right aspect or the posterior of the ascending aorta. They stated that, because the graft is much shorter, there is less chance that it will kink. Bonacchi and colleagues5 have even passed the right internal thoracic artery under the superior vena cava, past the transverse sinus, to the Cx coronary artery system, with excellent results. In our patients, however, the original graft segments to the Cx system were too short to take the route via the transverse sinus.
The graft from the Cx to the ascending aorta via a route either to the anterior pulmonary artery or to the transverse sinus can be directed along the left ventricle, left atrial appendage, and pulmonary artery. This is a longer route than if the bypass is directed along the basal left ventricle and interatrial groove to the ascending aorta. This route can be shortened by means of dissection as far as the posterior interatrial septum, as is described by Carpentier and associates2: the graft in this instance is directed chiefly along the interatrial groove from the Cx. By following this route, we were able to ensure that the vessel length would be sufficient to reach the ascending aorta without tension. Proper length and patency of the vein graft can be observed after completing the bypass by filling the heart via extracorporeal circulation.
The original Y graft from an autologous great saphenous vein and its branch can be used to reduce the number of proximal anastomoses and to increase runoff, due to the more-distal coronary anastomoses.
To our knowledge, the graft route from the ascending aorta to the Cx system described here is new. It can be successfully used if the length of the intended bypass conduit is insufficient.
Acknowledgment
We thank Barbara Junghaehnel from St.-Johannes-Hospital-Dortmund for her drawing.
Footnotes
Address for reprints: Niyazi Cebi, MD, Schondellestraße 19B, 44229 Dortmund, Germany E-mail: niyazicebi@hotmail.com
Dr. Cebi is currently with the Department for Cardiovascular Surgery, Istanbul Medicine Hospital; Barbaros Mah. Hoca Ahmet Yesevi, Cad. Nr. 19, 34203 Bagcilar, Istanbul, Turkey
References
- 1.Hudspeth AS. Circumflex coronary artery bypass grafting via transverse sinus. Ann Surg 1976;183(6):691–3. [DOI] [PMC free article] [PubMed]
- 2.Carpentier AF, Lessana A, Relland JY, Belli E, Mihaileanu S, Berrebi AJ, et al. The “physio-ring”: an advanced concept in mitral valve annuloplasty. Ann Thorac Surg 1995;60(5): 1177–86. [DOI] [PubMed]
- 3.Rastan H, Amir-Jahed AK. Aorta-circumflex coronary artery bypass through the transverse sinus. A new technique. Pahlavi Med J 1976;7(1):127–32. [PubMed]
- 4.Grondin CM, Limet R. Vein grafts to left-sided coronary arteries: passage through the transverse sinus. Ann Thorac Surg 1976;21(4):348–9. [DOI] [PubMed]
- 5.Bonacchi M, Prifti E, Battaglia F, Frati G, Sani G, Popoff G. In situ retrocaval skeletonized right internal thoracic artery anastomosed to the circumflex system via transverse sinus: technical aspects and postoperative outcome. J Thorac Cardiovasc Surg 2003;126(5):1302–13. [DOI] [PubMed]


