Abstract
We sought to determine U.S. physicians' knowledge and perspectives regarding the 2004 American College of Cardiology/American Heart Association guidelines for management of patients who have ST-segment–elevation myocardial infarction (STEMI). We invited 45,998 physicians from the American Medical Association's roster to take an Internet survey of U.S. cardiologists and emergency physicians who were hospital-based or who had hospital-admitting privileges. To represent individual and combined populations, data were weighted on the basis of years in practice, sex, and geographic region. Of 505 cardiologists and 509 emergency physicians who completed the survey, 90% worked in an urban or suburban setting and 82% at hospitals with a cardiac catheterization laboratory. Sampling error was ±3.4%. Most respondents (61%) believed that overall myocardial infarction treatment needed a “great deal” or “fair amount” of improvement; 24% were “somewhat” or “not at all” familiar with the guidelines. Although 84% knew the recommended STEMI treatments for a patient who presents within 3 hours of symptom onset without contraindications to reperfusion or delay to invasive treatment, only 11% knew that there is no preferred approach. If percutaneous coronary intervention proved impossible within 90 minutes of presentation, 21% reported that eligible patients—assuming early presentation, confirmed STEMI diagnosis, and no high-risk STEMI or contraindications to fibrinolysis—would “rarely” or “never” receive guideline-recommended fibrinolysis.
Many cardiologists and emergency physicians are unfamiliar with the guidelines and with the uncertainty that surrounds therapeutic approaches, which suggests the need for increased education on effective treatments to expedite myocardial reperfusion in STEMI.
Key words: Angioplasty, transluminal, percutaneous coronary/standards/utilization; cardiovascular diseases/epidemiology/mortality; chronology as topic; delivery of health care/standards; fibrinolysis; guideline adherence; hospitals/standards; practice guidelines as topic; quality assurance/health care; randomized controlled studies as topic; statistics & numerical data; statistics as topic; time factors; treatment outcome
Acute coronary syndromes are the most common cause of death in the United States.1 The 2001 American Heart Association/American College of Cardiology (AHA/ACC) data on 1.68 million unique U.S. hospital discharges for acute coronary syndromes (myocardial infarction [MI] or unstable angina),2 with application of an estimated 30% rate of ST-segment–elevation MI (STEMI),2,3 suggest that approximately 500,000 cases of STEMI occur in the U.S. annually.2
Reducing a patient's risk of death after acute STEMI depends on minimizing the time from symptom onset to coronary reperfusion.4–7 Reperfusion may be accomplished by either administering fibrinolytic agents or performing primary percutaneous coronary intervention (PCI).2,8 Within the first 3 hours after symptom onset, the method of reperfusion is less important than the speed with which reperfusion is accomplished.2,9 Therefore, the therapeutic focus in patients with STEMI is on the need to decrease the time required for reperfusion.10–12
Evidence-based clinical guidelines exist for STEMI management. These include the jointly issued AHA/ACC guidelines,2 and those from the European Society of Cardiology (ESC).13 According to the guidelines for treatment of STEMI, both PCI and fibrinolysis are class IA recommendations—the highest level.
Percutaneous coronary intervention is generally the preferred reperfusion approach if it can be performed quickly—defined as a door-to-balloon time of less than 90 minutes—and expertly, at a high-volume PCI hospital.2,13 Fibrinolysis is preferred if PCI is not an option (is unavailable for any reason) or cannot be performed quickly.2,7,13 Within 3 hours of symptom onset—absent delays in performing an invasive procedure—there is no preference for either method.2
The importance of guideline adherence with respect to outcomes in STEMI has been described in several U.S. studies. According to the National Registry of Myocardial Infarction (NRMI)-3 and -4 databases, hospital death rates were lower in patients who underwent PCI within 90 minutes, compared with patients who experienced a longer door-to-balloon time.14 Other investigators have shown that door-to-balloon times exceeding 2 hours are associated with more late deaths, despite an initial presentation within 3 hours of symptoms.15 Accordingly, a clear understanding of the guidelines and their optimal application are crucial when a patient presents with STEMI.
Little has been known, however, about clinicians' un-derstanding of the guidelines surrounding STEMI management. Our purpose was to survey U.S. cardiologists and emergency physicians to determine their self-reported knowledge of and adherence to the ACC/AHA guidelines for the management of acute STEMI.
Methods
The survey was conducted by the independent research organization Harris Interactive® and was supported by a grant from PDL BioPharma, Inc. Respondents completed surveys from December 8 through 16, 2005. By use of the American Medical Association's (AMA's) master roster of all U.S. doctors, we identified 45,998 emergency physicians and cardiologists and invited them to participate. The response rate was low (see Results) to a postal letter that contained the survey's website address, individual identification, and a password. A monetary incentive was provided to all qualified respondents who completed the survey ($50 for the primary survey and $10 for a follow-on survey that was conducted in order to correct for a programming error that affected a question in the original survey).
Screening questions were used to identify physicians who were fully qualified to participate: cardiologists or emergency-department physicians who either were practicing primarily in a hospital setting or had admitting privileges at a hospital. Qualified respondents answered up to 40 questions, depending on their answers to previous questions. The survey used multiple-choice answers or Likert scales. Questions involved respondents' views regarding the diagnosis and management of acute MI (AMI), including their knowledge of AMI signs and symptoms and of ways to educate the public on these; their knowledge of time lapses in seeking treatment for AMI, and of whether AMI treatment in the U.S. needs improvement; their familiarity with and opinions of the ACC/AHA guidelines for the management of STEMI, including the recommended hospital protocols for the treatment of STEMI; and reperfusion treatment, including their opinions regarding the time that elapses until the administration of reperfusion therapy, the preferred reperfusion approaches, and the advantages and disadvantages of PCI and fibrinolysis.
Statistics
We calculated the initial number of invitation letters to send to physicians by referring to standard response rates that Harris Interactive® had experienced from use of the AMA master roster in previous studies. Data were weighted on the basis of physicians' sex, geographic region, and years of practice, to be representative of the total combined population of cardiologists and emergency physicians, and of the individual populations of cardiologists and emergency physicians.
Rim weighting was used to ensure that the participant population reflected the total U.S. physician population; weighting targets were determined from the AMA master roster. Cardiologists and emergency physicians were weighted separately, and then the 2 groups were postweighted together to maintain their correct proportions. Only qualified physicians from each group were weighted. Weighting variables were geographic region (East, South, Midwest, and West) and sex by years in practice (men 0–10, 11–20, 21–30, and >30 years in practice, respectively). Women were weighted similarly, except that the last category comprised women who had more than 20 years in practice.
In accordance with a standard formula (1/square root of [weighting efficiency × sample size]), sampling error was ±3.4% for the total sample of cardiologists and emergency-medicine physicians; ±5.1% for the sample of cardiologists; and ±4.6% for the sample of emergency physicians. A standard t test (confidence interval, 95%) was used to evaluate the statistical significance of differences between groups. Data are presented as percentages based on the weighted base, or as mean ± SD. A level of P <0.05 was considered statistically significant.
Results
Of 45,998 invitation letters sent to physicians throughout the United States, 1,059 were returned as undeliverable (incorrect address or no forwarding address), leaving 44,939 valid records. A total of 2,501 physicians entered the survey. The survey was suspended or terminated for 1,487 physicians who were not qualified to participate on the basis of their answers to the screening questions, or who did not complete the full survey; demographic data were not collected on this cohort. Therefore, the final response rate was low: 1,014 physicians (505 cardiologists and 509 emergency physicians) qualified for and completed the survey. Completion took 15 minutes, on average. Data on areas of practice within specialties were not collected (for example, interventional cardiologist vs noninterventional cardiologist).
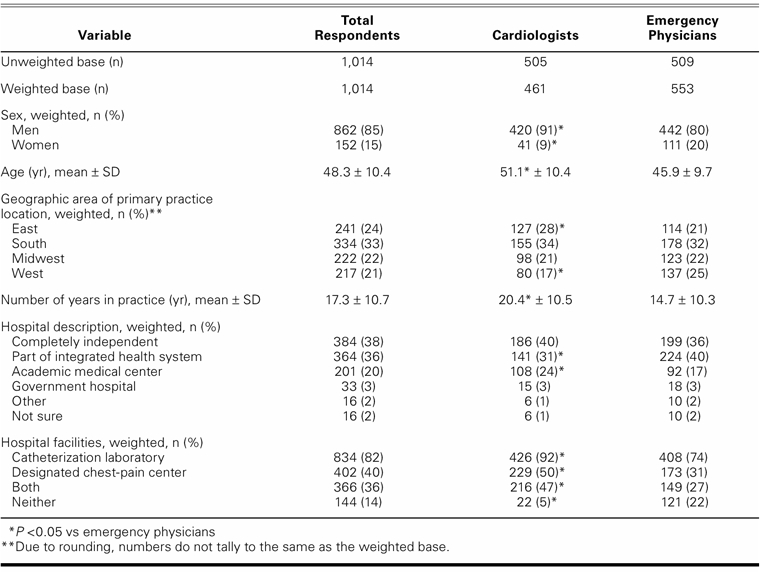
The demographic characteristics of the respondents are shown in Table I. Most were men (85%). The mean age of all respondents was 48.3 years, and they had been in practice for an average of 17.3 years. They were clinically active: on average, most saw more than 30 patients per week (95% overall; 93% of cardiologists, 97% of emergency physicians), and 24% overall saw more than 100 patients per week (23% of cardiologists, 24% of emergency physicians). Respondents were from 49 states, with good geographic distribution. Most worked at hospitals, or had hospital admitting privileges, in an urban (45%) or suburban (45%) setting; the remainder were rural. In addition, 82% of all respondents worked or had admitting privileges at a hospital that had a cardiac catheterization laboratory.
TABLE I. Demographic and Practice Information on the U.S. Cardiologists and Emergency Physicians Who Participated in the Survey
Knowledge of Acute Myocardial Infarction Symptoms among U.S. Adults
Most respondents believed that most U.S. adults lack knowledge of MI symptoms (Fig. 1). Among those physicians who believed that at least some of their patients delay treatment for a heart attack, most thought that lack of knowledge was the chief reason: 86% indicated that patients think that MI symptoms will resolve spontaneously; 70%, that patients fail to recognize signs and symptoms; 64%, that patients do not understand the importance of early presentation; and 5%, that patients do not know where to receive treatment. Most physicians (71% overall; cardiologists, 77%; emergency physicians, 66%) responded that more than 25% of the patients whom they had treated for AMI had waited longer than they should have to seek treatment.
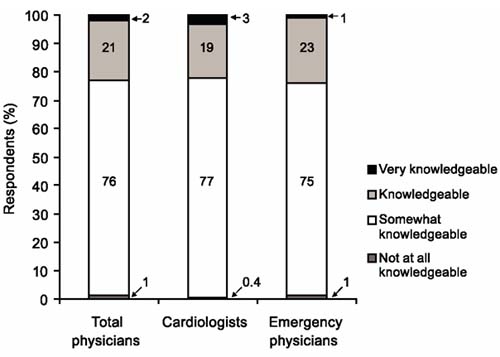
Fig. 1 Level of knowledge of acute myocardial infarction symptoms among U.S. adults, as rated by cardiologists and emergency physicians who participated in the survey.
The most effective ways suggested to help educate patients were discussing symptoms as part of screening for MI risk (50% overall; cardiologists, 48%; emergency physicians, 52%) and participating in television or radio public-service announcements with celebrity patients (36% overall; cardiologists, 37%; emergency physicians, 36%).
Opinions about Acute Myocardial Infarction Treatment in the United States
Most respondents (61%) thought that the treatment of AMI required either “a great deal” or “a fair amount” of improvement, although the belief was significantly less common among emergency physicians than cardiologists (53% vs 69%; P <0.05) (Fig. 2). When respondents who noted that the treatment of MI needed at least some improvement were asked to identify the 3 most effective ways by which to improve overall AMI therapy, the most commonly cited were providing more patient education on how to detect MI symptoms (82% overall; cardiologists, 84%; emergency physicians, 80%); reducing time to reperfusion once medical contact has been established (78% overall; cardiologists, 81%; emergency physicians, 76%); and offering opportunities for emergency departments, cardiologists, and emergency physicians to be trained together in responding to AMI (39% overall; cardiologists, 38%; emergency physicians, 39%).
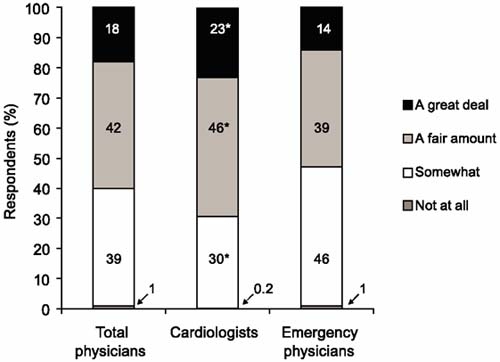
Fig. 2 Degree of improvement required in the treatment of acute myocardial infarction in the U.S., as rated by cardiologists and emergency physicians who participated in the survey.
Note: Percentages may differ from those for the combined categories, due to rounding.
P <0.05 vs emergency physicians
Awareness and Implementation of ACC/AHA STEMI Guidelines
Approximately one fourth (24%) of all respondents were “not at all familiar” or were “only somewhat familiar” with the STEMI guidelines (Fig. 3). Although lower among cardiologists than emergency physicians (19% vs 28%; P <0.05), these proportions were consistent between these physician groups at hospitals that had catheterization laboratories (cardiologists, 19%; emergency physicians, 29%) or designated chest-pain centers (16% and 27%), but not at hospitals that had neither (33% and 28%). However, due to the small number of cardiologists at hospitals that had neither a catheterization laboratory nor a designated chest-pain center, caution should be used when interpreting this last result. Of respondents who were at least “somewhat aware” of the guidelines, 84% overall considered the guidelines “effective” or “very effective” in determining how to treat AMI, while only 16% (cardiologists, 14%; emergency physicians, 17%) considered the guidelines only “somewhat effective.”
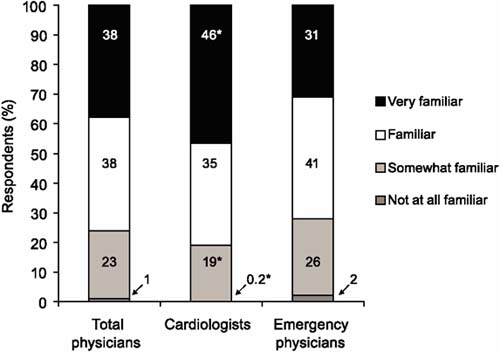
Fig. 3 Their own familiarity with current American Heart Association/American College of Cardiology guidelines on the management of ST-segment–elevation myocardial infarction, self-rated by cardiologists and emergency physicians who participated in the survey.
P <0.05 vs emergency physicians
Most respondents (84% overall; cardiologists, 89%; emergency physicians, 79%) stated that they knew the preferred guideline-recommended treatment approach when a patient presented within 3 hours of symptom onset and had no contraindications for reperfusion therapy or reason to delay an invasive strategy. Overall, 2% (no difference by specialty) stated that they did not know the preferred approach in this situation. Fifteen percent were unsure of the preferred approach (cardiologists, 10%; emergency physicians, 19%); the corresponding proportions were 13% among doctors at hospitals that had catheterization laboratories, 11% among those at hospitals that had designated chest-pain centers, and 19% when hospitals had neither.
Among respondents who stated that they knew the preferred approach to the above situation according to the STEMI guidelines, 82% (cardiologists, 76%; emergency physicians, 88%) incorrectly indicated that it was PCI, and 6% (cardiologists, 9%; emergency physicians, 4%) indicated fibrinolysis. Only 11% (cardiologists, 15%; emergency physicians, 8%) correctly said that there is no preferred approach.
Most (78% overall; cardiologists, 77%; emergency physicians, 78%) indicated that their hospital had a written MI treatment protocol. Of the 91% of respondents whose hospital protocol reflected the ACC/AHA guidelines, more cardiologists (95%) than emergency physicians (88%) replied affirmatively (P <0.05). Only 1% (cardiologists, 0.3%; emergency physicians, 2%; P <0.05) said that their hospital's protocol did not reflect the guidelines, and 8% (cardiologists, 5%; emergency physicians, 10%; P <0.05) were unsure. However, among respondents whose hospital has a written protocol, about a quarter (23% overall; cardiologists, 22%; emergency physicians, 24%) deemed the protocol ineffective in helping providers determine treatment for AMI, and 50% (cardiologists, 50%; emergency physicians, 51%) indicated that the protocol was followed only sometimes or rarely.
Of the doctors surveyed, 40% (cardiologists, 44%; emergency physicians, 36%) believed that their hospital could improve reperfusion therapy times once medical contact occurred, in accordance with the door-to-needle or door-to-balloon timelines specified in the STEMI guidelines, by either a “great deal” or a “fair amount.” However, 69% (cardiologists, 67%; emergency physicians, 71%) indicated that performance of PCI within 90 minutes of initial medical contact was only “somewhat” or “not at all” realistic in patients who were transferred from a non-PCI-capable hospital to a PCI-capable hospital. Furthermore, 20% (cardiologists, 19%; emergency physicians, 20%) stated that performing PCI in less than 90 minutes was somewhat or not at all realistic, even if a patient were to present directly or be promptly transported to a hospital that had a catheterization laboratory.
Choice of Reperfusion Therapy
Fewer than half of the respondents (44% overall; cardiologists, 42%; emergency physicians, 46%) indicated that at their hospital eligible patients would “always” receive fibrinolysis for reperfusion if they could not undergo PCI within 90 minutes of initial medical contact (assuming early presentation, confirmed STEMI diagnosis, and no high-risk STEMI or contraindications to fibrinolysis). One third (33% overall; cardiologists, 34%; emergency physicians, 31%) said that eligible patients would “sometimes” receive fibrinolysis in this situation, while 21% (cardiologists, 21%; emergency physicians, 21%) indicated that eligible patients would “rarely” or “never” receive fibrinolysis in this situation.
Statistically significant differences existed between the subgroups of emergency physicians at hospitals that had different treatment facilities. Among emergency physicians at hospitals that had a catheterization laboratory or a designated chest-pain center, compared with emergency physicians at hospitals that had neither, significantly fewer reported that eligible patients would “always” receive fibrinolysis if they could not undergo PCI within 90 minutes of initial medical contact (catheterization laboratory, 38%; designated pain center, 34%; neither, 71%; P <0.05 for both comparisons). Significantly more emergency physicians reported that patients would “sometimes” receive fibrinolysis (catheterization laboratory 33% and designated pain center 40% vs neither, 21%; P <0.05 for both comparisons with the “neither” group and for catheterization laboratory vs designated pain center) or “rarely/never” receive fibrinolysis (catheterization laboratory 25% and designated pain center 25% vs neither, 7%; P <0.05 for both comparisons).
Most respondents (61% overall; cardiologists, 62%; emergency physicians, 60%) agreed that a patient with AMI who presented within 3 hours of symptom onset could benefit from fibrinolysis, even if the patient were eligible to undergo PCI within 90 minutes of initial medical contact (assuming early presentation, confirmed STEMI diagnosis, and no high-risk STEMI or contraindications to fibrinolysis).
To determine factors related to therapeutic preference, we asked respondents to select from a list of options as many as 2 factors that would cause either PCI or fibrinolysis to be the preferred reperfusion approach at their hospital. The most common choice for both PCI and fibrinolysis was related to catheterization capabilities—for PCI, most commonly cited was the presence of a catheterization laboratory (73%); for fibrinolysis, it was that the hospital lacked such a laboratory and the patient could not be transferred to a PCI-capable hospital in a timely fashion (44%) (Table II).
TABLE II. Chief Factors that Would Cause PCI or Fibrinolysis to Be the Preferred Reperfusion Approach at the Respondent's Hospital, by Respondent Specialty (%)*
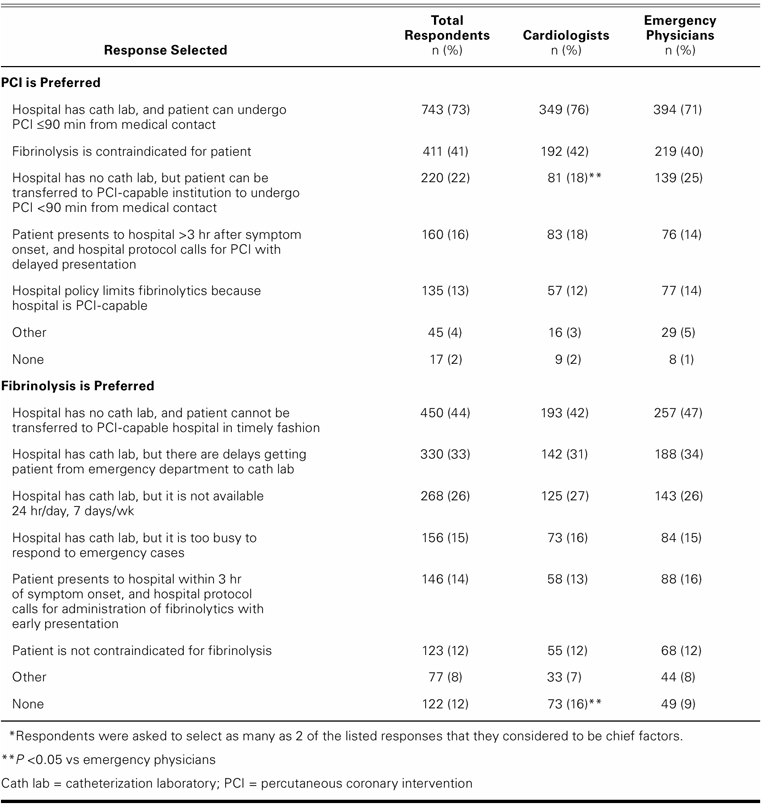
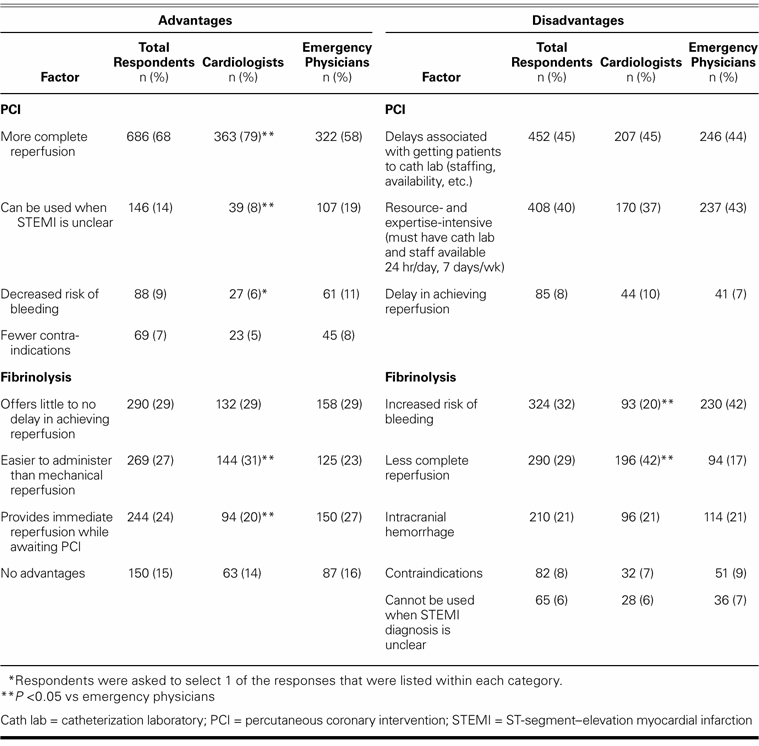
Table III shows what all respondents considered to be the advantages and disadvantages of reperfusion therapies. Overall, more complete reperfusion was listed as the primary advantage of PCI, whereas delay in getting the patient to the catheterization laboratory and the resource- and expertise-intensive nature of PCI were the foremost disadvantages. The chief advantages of fibrinolysis were speed to reperfusion and greater ease of administration than mechanical reperfusion; the disadvantages were increased risk of bleeding and less complete reperfusion. Cardiologists and emergency physicians responded similarly regarding the chief disadvantages of PCI, but statistically significant differences existed in regard to the advantages of PCI and the advantages and disadvantages of fibrinolysis.
TABLE III. Most Common Responses (≥5% of Total Respondents) Regarding the Chief Advantages and Disadvantages of PCI and Fibrinolysis as Preferred Reperfusion Approaches, by Respondent Specialty (%)*
Discussion
Due to a lower-than-optimal response rate, the results of this survey may be considered exploratory; however, the study findings provoke thought and highlight an area for further investigation. Our results suggest both a need and an opportunity to improve clinicians' understanding of optimal treatment of acute STEMI. Respondents indicated that effective avenues toward achieving this goal include better educating patients to recognize the symptoms of MI, thus potentially reducing the time from symptom onset to medical contact (82%); and decreasing the time to reperfusion therapy after medical contact (78%). Unfortunately, in large, randomized STEMI clinical trials, the mean time to hospital presentation typically exceeds 3.5 hours after symptom onset. This is consistent with our survey findings that 71% of physicians believed that more than 25% of their AMI patients waited too long before seeking medical attention. Of our respondents who believed that at least some of their patients delayed treatment for MI, 86% attributed delays in seeking medical care to patients' expectations that symptoms would abate on their own; 70%, to patients' failure to recognize signs or symptoms of MI; 64%, to patients' lack of understanding of the importance of rapid hospital presentation; and 5%, to patients' lack of awareness of where to receive treatment.
Our respondents identified several methods by which physicians could educate patients about symptoms of possible MI. Chief among these were discussing symptoms as part of screening for MI risk (50%), and participating in television or radio public-service announcements with celebrity patients (36%). Unfortunately, other investigators have reported that large-scale public education has a limited effect on decreasing time from symptom onset to hospital presentation,16 although appropriate use of emergency medical services does increase. Accordingly, novel educational approaches may be needed to achieve further reductions in patient presentation times.
Many patients initially present to a non-PCI-capable hospital. If transfer to a different hospital for PCI is needed, achieving guideline-recommended door-to-balloon times becomes a substantial challenge.12,17 Although other studies have indicated that transfer for PCI can occur within a very short time, this may not reflect the contemporary U.S. medical experience: 69% of our respondents considered it unrealistic that PCI could be performed within 90 minutes of initial medical contact when a patient is transferred from a non-PCI-capable hospital to a PCI-capable hospital—and 20% also deemed PCI unrealistic within the recommended 90 minutes even if initial presentation was at a PCI-capable facility. Although the opinions defined in our survey are of concern, they are consistent with other reports. In analyses from the NRMI-3 and -4 registries, only 4.2% of transfer patients12 and 37% of patients who did not require transfer11 for PCI had door-to-balloon times of less than 90 minutes. As might be expected, a substantial minority (40%) of physicians from our survey believed that their hospital could improve reperfusion time by either a great deal or a fair amount.
Recent U.S. and European reports9,14,18 show that increased implementation of guideline-compliant therapy can result in improved outcomes. From our survey, we found what we consider widespread unfamiliarity with the STEMI guidelines among cardiologists and emergency physicians alike. The need for familiarity may be even more important among noncardiologists, because fewer emergency physicians than cardiologists were familiar with the STEMI guidelines. More collaboration between physician-specialty organizations could reduce this differential.
When our respondents compared the strengths and weaknesses of PCI and thrombolysis, the most common answers were broadly similar, regardless of specialty. However, the most common chief disadvantage of fibrinolysis differed by specialty: cardiologists cited less-complete reperfusion (42%), whereas emergency physicians cited an increased risk of bleeding (42%). We hypothesize that this divergence is the result of “practice bias”—emergency physicians transfer incompletely reperfused patients for invasive procedures but personally witness the complications of post-thrombolytic bleeding.
Overall, both physician groups supported the importance of time to reperfusion. Most (93% overall and in both groups) agreed that delayed time to reperfusion leads to worse outcomes in STEMI patients. However, a bias toward PCI appears to exist, perhaps due to data that support PCI's superiority over lysis.19 The implications of a PCI bias are notable between practices: 55% of cardiologists reported that their patients would receive fibrinolysis for reperfusion only “sometimes,” “rarely,” or “never” if PCI could not be performed within 90 minutes. The cardiologists indicated this even though 62% agreed that eligible patients who present within 3 hours of symptom onset benefit from fibrinolysis even if the patient can undergo PCI within 90 minutes of medical contact. It appears that the current therapeutic preference is for PCI in all circumstances, without recognition that with early presentation, rapid fibrinolysis is preferable to delayed PCI. Other investigators have reported similar findings. Kalla and colleagues9 noted that interventional cardiologists frequently prefer PCI over fibrinolysis, irrespective of the time to balloon inflation.
An analysis of data from the Enhanced Feedback for Effective Cardiac Treatment (EFFECT) project in Ontario, Canada, reported on factors that led to underuse of reperfusion therapy (mainly fibrinolysis, when PCI availability was limited).20 It was found that appropriate determinants for withholding reperfusion therapy were a patient's increasing time to hospital presentation, increasing risk of intracerebral hemorrhage, increasing Thrombolysis in Myocardial Infarction (TIMI) mortality risk index, and greater number of comorbid conditions. Some physicians consider the risk of intracerebral hemorrhage an “entirely rational” reason for forgoing particular treatments in specific patients.21 It has been suggested that if the potential benefits of treatment are marginal, a decision analysis may be a valuable means by which to assist physicians in balancing benefits and risks.21 Such an analysis might also aid in more effective implementation of guidelines or use of therapeutic options. Furthermore, decision analysis may assist physicians in taking into account various patient characteristics that can influence treatment decisions. A recent analysis of data from the NRMI-2, -3, and -4 databases indicated that factors such as age, time from symptom onset to presentation, and infarct location affected the length of PCI-related delay, after which any survival advantage of primary PCI over fibrinolysis was lost.22
Limitations of the Study
There are several limitations to this study. Our results could reflect physicians' disagreement with the 2004 ACC/AHA guidelines. However, this is inconsistent with our finding that 84% of respondents considered the guidelines “effective” or “very effective” in determining the treatment of AMI. Alternatively, our findings may simply be the result of incorrect recollection of guideline recommendations.
Another limitation is that the online survey format required that all respondents have Internet access. This is the medium often used by Harris Interactive® for conducting healthcare surveys and interviewing healthcare professionals; however, the possibility of bias introduced from an Internet-based survey is unknown. Additional bias may also have been introduced because the format of the survey used the respondents' self-reporting to determine their familiarity with the guidelines; although a question asked respondents to identify guideline recommendations, it was not possible to fully test respondents' understanding of and ability to use the guidelines.
The broad application of our findings may be limited if the doctors surveyed are not representative of the total U.S. physician population. Because a relatively small number of invited physicians participated in the survey, it must be considered that those who responded might have had a particular interest in taking surveys on healthcare issues, atypical of all U.S. cardiologists or emergency physicians. A converse effect could occur if physicians who were unfamiliar with the guidelines disproportionately exited the survey without completing the questions, or if the survey respondents were excessively motivated to participate by the receipt of a monetary award.
Finally, practice location could have influenced our results. Most respondents worked in an urban or a suburban setting; very few were physicians in a rural environment with longer transport times. As such, most respondents worked at or had admitting privileges at hospitals that had a catheterization laboratory. These factors could have biased responses in favor of PCI.
Conclusions
Most cardiologists (69%) and emergency physicians (53%) believed that a “great deal” or “fair amount” of improvement is needed in the treatment of AMI. Most endorsed increased patient education as a way to enhance detection of symptoms of AMI.
In regard to physicians' knowledge, 24% of the respondents (19% of cardiologists and 28% of emergency physicians) claimed to be only “somewhat familiar” or “not at all familiar” with the ACC/AHA STEMI management guidelines.
In terms of clinical practice, 69% of the respondents indicated that guideline-recommended PCI within 90 minutes is “somewhat” or “not at all” realistic if a patient requires transfer to another facility, and 20% held the same view even when the patient directly presents to a PCI-capable institution.
Finally, 54% of our respondents indicated that if their PCI-eligible patient could not undergo PCI within 90 minutes of medical contact, he or she would still only “sometimes” (33%), “rarely” (19%), or “never” (2%) receive guideline-recommended fibrinolysis.
Acknowledgment
Manuscript preparation assistance was provided by Wolters Kluwer Health Medical Communications Group.
Footnotes
Address for reprints: W. Frank Peacock, MD, Vice-Chief, Emergency Medicine, Cleveland Clinic, 9500 Euclid Ave., Cleveland, OH 44195-0002. E-mail: Peacocw@ccf.org
Source of support: This survey was conducted by Harris Interactive® on behalf of PDL BioPharma, Inc.
Disclosures: Dr. Peacock has received honoraria from or participated in advisory boards for Biosite, Innovise, Inverness, Millennium, PDL BioPharma, Schering-Plough, Scios, and The Medicines Company. Dr. Bhatt has received honoraria from, or participated in advisory boards or acted as a consultant for, AstraZeneca, Bristol-Myers Squibb, Centocor, Eisai, Eli Lilly, GlaxoSmithKline, Millennium, Paringenix, PDL BioPharma, Sanofi-Aventis, Schering-Plough, and The Medicines Company. Dr. Diercks has received honoraria from, or participated in advisory boards or acted as a consultant for, Biosite, Bristol-Myers Squibb, Innovise, Sanofi-Aventis, and The Medicines Company. Dr. Brown has participated in a speaker's bureau for Schering-Plough. Dr. Januzzi has received honoraria from, or participated in advisory boards or acted as a consultant for, Biosite, Dade-Behring, Inverness Medical Innovations, Merck, Ortho Clinical Diagnostics, Roche Diagnostics, and Sanofi-Aventis.
References
- 1.Cavendish JJ, Fugit RV, Safani M. Role of antiplatelet therapy in cardiovascular disease I: Acute coronary syndromes. Curr Med Res Opin 2004;20(11):1839–43. [DOI] [PubMed]
- 2.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 guidelines for the management of patients with acute myocardial infarction). J Am Coll Cardiol 2004;44(3):E1-E211. [DOI] [PubMed]
- 3.Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, et al. Heart disease and stroke statistics–2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee [published errata appear in Circulation 2006;113(14):e696 and Circulation 2006;114(23):e630]. Circulation 2006;113(6):e85–151. [DOI] [PubMed]
- 4.Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet 1996;348(9030):771–5. [DOI] [PubMed]
- 5.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 2004;109(10):1223–5. [DOI] [PubMed]
- 6.Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists' (FTT) Collaborative Group [published erratum appears in Lancet 1994;343(8899):742]. Lancet 1994;343(8893):311–22. [PubMed]
- 7.Nallamothu BK, Bates ER. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: is timing (almost) everything? Am J Cardiol 2003;92(7): 824–6. [DOI] [PubMed]
- 8.Hahn SA, Chandler C. Diagnosis and management of ST elevation myocardial infarction: a review of the recent literature and practice guidelines. Mt Sinai J Med 2006;73(1):469–81. [PubMed]
- 9.Kalla K, Christ G, Karnik R, Malzer R, Norman G, Prachar H, et al.; Vienna STEMI Registry Group. Implementation of guidelines improves the standard of care: the Viennese registry on reperfusion strategies in ST-elevation myocardial infarction (Vienna STEMI registry). Circulation 2006;113(20): 2398–405. [DOI] [PubMed]
- 10.Magid DJ, Wang Y, Herrin J, McNamara RL, Bradley EH, Curtis JP, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA 2005;294(7):803–12. [DOI] [PubMed]
- 11.McNamara RL, Herrin J, Bradley EH, Portnay EL, Curtis JP, Wang Y, et al; NRMI Investigators. Hospital improvement in time to reperfusion in patients with acute myocardial infarction, 1999 to 2002. J Am Coll Cardiol 2006;47(1):45–51. [DOI] [PMC free article] [PubMed]
- 12.Nallamothu BK, Bates ER, Herrin J, Wang Y, Bradley EH, Krumholz HM; NRMI Investigators. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction (NRMI)-3/4 analysis. Circulation 2005; 111(6):761–7. [DOI] [PubMed]
- 13.Van de Werf F, Ardissino D, Betriu A, Cokkinos DV, Falk E, Fox KA, et al. Management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J 2003;24(1): 28–66. [DOI] [PubMed]
- 14.McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, et al.; NRMI Investigators. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 2006;47(11):2180–6. [DOI] [PubMed]
- 15.Brodie BR, Hansen C, Stuckey TD, Richter S, Versteeg DS, Gupta N, et al. Door-to-balloon time with primary percutaneous coronary intervention for acute myocardial infarction impacts late cardiac mortality in high-risk patients and patients presenting early after the onset of symptoms. J Am Coll Cardiol 2006;47(2):289–95. [DOI] [PubMed]
- 16.Luepker RV, Raczynski JM, Osganian S, Goldberg RJ, Finnegan JR Jr, Hedges JR, et al. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: The Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA 2000;284(1):60–7. [DOI] [PubMed]
- 17.Smalling RW. Role of fibrinolytic therapy in the current era of ST-segment elevation myocardial infarction management. Am Heart J 2006;151(6 Suppl):S17–23. [DOI] [PubMed]
- 18.Bhatt DL, Roe MT, Peterson ED, Li Y, Chen AY, Harrington RA, et al.; CRUSADE Investigators. Utilization of early invasive management strategies for high-risk patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE Quality Improvement Initiative. JAMA 2004; 292(17):2096–104. [DOI] [PubMed]
- 19.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003;361(9351):13–20. [DOI] [PubMed]
- 20.Alter DA, Ko DT, Newman A, Tu JV. Factors explaining the under-use of reperfusion therapy among ideal patients with ST-segment elevation myocardial infarction. Eur Heart J 2006;27(13):1539–49. [DOI] [PubMed]
- 21.Rajagopal V, Bhatt DL. Gaps in myocardial infarction care: how might we best EFFECT change? Eur Heart J 2006;27 (13):1513–4. [DOI] [PubMed]
- 22.Pinto DS, Kirtane AJ, Nallamothu BK, Murphy SA, Cohen DJ, Laham RJ, et al. Hospital delays in reperfusion for ST-elevation myocardial infarction: implications when selecting a reperfusion strategy. Circulation 2006;114(19):2019–25. [DOI] [PubMed]


